Abstract
Yellow phosphorus, a component of certain pesticide pastes and fireworks, is well known to cause hepatotoxicity. Poisoning with yellow phosphorus classically manifests with acute hepatitis leading to acute liver failure which may need liver transplantation. We present a case of yellow phosphorus poisoning in which a patient presented with florid clinical features of cholestasis highlighting the fact that cholestasis can rarely be a presenting feature of yellow phosphorus hepatotoxicity.
Keywords: Cholestasis, poisoning, yellow phosphorus
INTRODUCTION
Yellow phosphorus (YP) is a well-known hepatotoxic agent commonly used in fireworks and pesticide pastes.[1] Literature about YP poisoning is limited to case series, which supports acute hepatitis with or without acute liver failure as the most common form of clinical presentation.[2,3,4,5] Even though one report has described biochemical evidence of cholestasis in cases of YP toxicity[6] clinical cholestasis has not been documented so far. This report demonstrates a case of YP poisoning presenting with predominant features of clinical and biochemical cholestasis.
CASE REPORT
A forty three-year-old gentleman presented to us after eight days of suicidal ingestion of one tube (35 g) of rodenticide paste (Ratol, containing 3% YP). He had history of daily alcohol intake of about 50-60 grams for the past 5 years without any history suggestive of underlying chronic liver disease or cirrhosis. He had no past history of jaundice. He denied history of ingesting any other drugs or toxins in the recent past.
After self-limiting nausea and vomiting on the day of ingestion, he remained asymptomatic for 4 days. He observed dark-coloured urine and generalized itching on day 5 after ingestion. Pruritus was severe and disturbing his sleep. After being detected to have jaundice, by his local physician, he was referred to our institute on day 8 for further investigation.
Examination revealed clinical jaundice with excoriation marks all over the body secondary to severe pruritus. His liver was palpable 4 cm below the costal margin and was firm in consistency. Detailed examination failed to show any stigma of underlying chronic liver disease, splenomegaly, or ascites. Cardiovascular and nervous system examination was observed normal and there were no bleeding diathesis. He was not in hepatic encephalopathy as assessed by normal mini-mental state examination score (MMSE). He reported the pruritus as 8 on a visual analogue score of 0 to 10.[7]
Evaluation showed a normal hemogram, with bilirubin of 22 mg/dL (0.2-2.0 mg/dL) with a direct fraction of 18 mg/dL, serum alanine amino transferase (ALT) of 58 IU/L (0-40 IU/L), aspartate amino transferase (AST) level of 100 IU/L (0-40 IU/L), alkaline phosphatase (AP) value of 277 IU/L (50-150 IU/L), and gamma glutamyl transferase (GGT) of 140 IU/L (20-40 IU/L). Prothrombin time was prolonged by 4 seconds, which normalized after vitamin K injection. Electrocardiogram and renal functions were normal.
Other causes of liver disease were ruled out by negative HbsAg, anti-HCV, IgM anti-HEV, and IgM anti-HAV serology. His serum ceruloplasmin and ferritin levels were normal. Ultrasound scan of the abdomen was unremarkable, except for a fatty liver. Upper Gastrointestinal (GI) endoscopy showed no varices. After normalization of prothrombin time, liver biopsy was done on day 14 of ingestion, which showed enlarged hepatocytes, giant cell transformation, intrahepatic cholestasis and spotty hepatocyte necrosis with infiltration by lymphocytes and few eosinophils [Figure 1]. Histopathology has not shown any evidence of architectural distortion of hepatic lobule, fibrosis, cirrhosis, or regenerating nodules.
Figure 1.
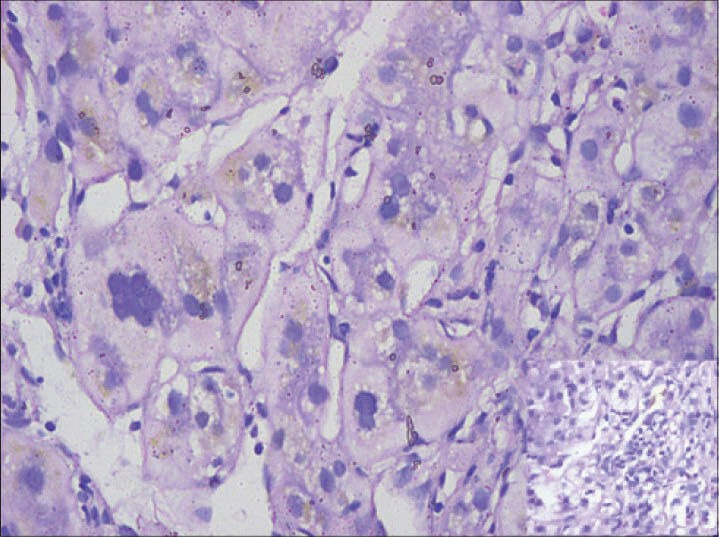
Liver biopsy showing enlarged hepatocytes, giant cell transformation and intrahepatic cholestasis. Inset shows inflammatory cell infiltration (H and E, ×400)
The patient never developed any clinical signs of acute liver failure. Pruritus was controlled with emollients, ursodeoxycholic acid, cholestyramine and sertraline. Liver function tests normalized and pruritus also improved over the next 3 weeks. Patient is currently asymptomatic after 4-months of follow-up.
DISCUSSION
Sporadic cases of suicidal or accidental ingestion of YP are common in developing countries and the usual sources are fireworks and rodenticide pastes. On ingestion, YP is rapidly absorbed through the intestinal tract, and few hours after the ingestion, 69% to 73% of the total ingested-dose concentrates into the liver, leads to predominant features of hepatotoxicity. Other reported toxic effects include gastrointestinal symptoms, renal failure, arrhythmias, seizures, coma, bone marrow suppression, and cardiovascular collapse.[8]
Clinical features of acute poisoning with YP have been classically divided into 3 stages.[9] The first is a gastrointestinal stage characterised by nausea, vomiting, and abdominal pain occurring within 24 hours, with normal laboratory tests. The second is an asymptomatic stage but laboratory investigations in this stage reveal a hepatitic picture. These changes may then progress to the third stage of acute liver failure which may even necessitate liver transplantation. Our patient had the typical features of stages 1 and 2 with a cholestatic presentation in stage 3. We made adequate efforts to exclude possibility of underlying alcohol related chronic liver disease with decompensation using ultrasound scan, upper GI endoscopy, and liver biopsy.
Liver histopathology in YP poisoning, usually obtained from post-mortem or explant livers, shows features of toxic hepatitis with extensive necrosis, ballooning degeneration, and steatosis.[2] Reports have suggested the presence of biochemical evidence of cholestasis,[6] but clinical presentation purely with florid features of cholestasis have not been described in literature so far.
Management of YP poisoning is usually supportive; studies have not shown any clear benefit from corticosteroids, N-acetyl cysteine or exchange transfusion.[10] Living donor liver transplantation has been shown to be beneficial in cases with acute liver failure.[2,3,11] In our case, our patient responded to usual anti-cholestatic modalities like cholestyramine, ursodeoxy cholic acid, and sertraline.
To conclude, we describe intrahepatic cholestasis with severe pruritus as a rare presenting feature of yellow phosphorus poisoning, with improvement in clinical and biochemical responses to supportive therapeutic management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Simon FA, Pickering LK. Acute yellow phosphorus poisoning. Smoking stool syndrome. JAMA. 1976;235:1343–4. [PubMed] [Google Scholar]
- 2.Ates M, Dirican A, Ozgor D, Aydin C, Isik B, Ara C, et al. Living donor liver transplantation for acute liver failure in pediatric patients caused by the ingestion of fireworks containing yellow phosphorus. Liver Transpl. 2011;17:1286–91. doi: 10.1002/lt.22384. [DOI] [PubMed] [Google Scholar]
- 3.Santos O, Restrepo JC, Velásquez L, Castaño J, Correa G, Sepúlveda E, et al. Acute liver failure due to white phosphorus ingestion. Ann Hepatol. 2009;8:162–5. [PubMed] [Google Scholar]
- 4.Mauskar A, Mehta K, Nagotkar L, Shanbag P. Acute hepatic failure due to yellow phosphorus ingestion. Indian J Pharmacol. 2011;43:355–6. doi: 10.4103/0253-7613.81500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Taskesen M, Adıguzel S. A rare cause of poisoning in childhood: Yellow phosphorus. J Emerg Med. 2012;43:270–2. doi: 10.1016/j.jemermed.2011.05.083. [DOI] [PubMed] [Google Scholar]
- 6.Fernandez OU, Canizares LL. Acute hepatotoxicity from ingestion of yellow phosphorus-containing fireworks. J Clin Gastroenterol. 1995;21:139–42. doi: 10.1097/00004836-199509000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Bellmann R, Graziadei IW, Feistritzer C, Schwaighofer H, Stellaard F, Sturm E, et al. Treatment of refractory cholestatic pruritus after liver transplantation with albumin dialysis. Liver Transpl. 2004;10:107–14. doi: 10.1002/lt.20001. [DOI] [PubMed] [Google Scholar]
- 8.Tafur AJ, Zapatier JA, Idrovo LA, Oliveros JW, Garces JC. Bone marrow toxicity after yellow phosphorus ingestion. Emerg Med J. 2004;21:259–60. doi: 10.1136/emj.2003.007880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCarron MM, Gaddis GP, Trotter AT. Acute yellow phosphorus poisoning from pesticide pastes. Clin Toxicol. 1981;18:693–712. doi: 10.3109/15563658108990295. [DOI] [PubMed] [Google Scholar]
- 10.Marin GA, Montoya CA, Sierra JL, Senior JR. Evaluation of corticosteroid and exchange-transfusion treatment of acute yellow-phosphorus intoxication. N Engl J Med. 1971;284:125–8. doi: 10.1056/NEJM197101212840303. [DOI] [PubMed] [Google Scholar]
- 11.Akman SA, Cakir M, Baran M, Arikan C, Yuksekkaya HA, Tumgor G, et al. Liver transplantation for acute liver failure due to toxic agent ingestion in children. Pediatr Transplant. 2009;13:1034–40. doi: 10.1111/j.1399-3046.2008.01119.x. [DOI] [PubMed] [Google Scholar]


