Abstract
Background:
The purpose of this study was to perform the Creating Opportunities for Parent Empowerment (COPE) program for Iranian mothers and evaluate its effectiveness on stress, anxiety, and participation of mothers who have premature infants hospitalized in neonatal intensive care units (NICUs).
Materials and Methods:
A randomized clinical trial was conducted with 90 mothers of premature infants hospitalized in the educational neonatal NICUs of state hospitals affiliated to Isfahan University of Medical Sciences. For measuring the variables, State-Trait Anxiety Inventory, the Parental Stressor Scale: Neonatal Intensive Care, and The Index of Parental Participation/Hospitalized Infant were used. Intervention group received two phases of COPE program. This program consisted of information and behavioral activities about the characteristics of premature infants. Sessions’ interval was from 2 to 4 days. Stress and anxiety were measured three times (before each phase and 2-4 days after the second phase). Mothers’ participation was evaluated 2-4 days after the second phase. The t-test, χ2, Mann-Whitney U test, and repeated measurement test were used for data analysis.
Results:
Mothers in the intervention group reported significantly less anxiety and less stress in the NICU after performing each phase of the COPE program (P < 0.001), whereas at this time, the level of stress in the comparison group increased. Also, COPE mothers participated in their infants’ care rather than the mothers in the comparison group (P < 0.001).
Conclusion:
COPE program was effective for Iranian mothers. This study shows that irrespective of any culture, giving early and comprehensible educational-behavioral information may have positive effect on maternal psychological condition and maternal–infant interaction.
Keywords: Anxiety, Creating Opportunities for Parent Empowerment, Iran, participation, premature infant, stress
INTRODUCTION
The birth of a premature infant has long been documented as a stressful event for parents. The premature birth of an infant and the following neonatal intensive care cause psychological distress and can have a traumatizing effect on parents.[1,2] The neonatal intensive care unit (NICU) environment has the potential to exacerbate stress for parents of infants admitted to the NICU.[3,4] Mothers have typically been found to have higher levels of distress than fathers[5] and they experience significant levels of stress and depression in the early postpartum period.[6] Maternal stress can have deleterious effects on mother-infant interaction, particularly on mothers’ abilities to form an attachment to their baby.[7,8] Maternal stress diminishes the mother's ability to be sensitive to the infant's cues and be responsive in interacting with the infant.[9] Participating in infant care influences the maternal feelings in a positive direction. Finding of a study has shown that a mother who is denied the opportunity comparing to a mother whose child is left feeling confused and anxious. When the mother is nearby, breastfeeds and takes care of her child's daily care she has a feeling of participation.[10] This situation creates a need for practices that support parents during the acute phase of their infant's hospitalization in neonatal intensive care.[11] The facilitation of maternal confidence and positive parenting in the NICU may be a key point in establishing and sustaining long-term healthy mother-infant interactions and positive child outcomes.[12]
NICUs have been established in Iran since about 1984, and today they are running in the state and private hospitals of 31 provinces under the supervision of a neonatologist. There are high-tech equipments for infants’ treatment in most of these wards and mothers can settle in specific rooms close to the ward, so that they can go to their infants to take care of them primarily based on their willing and abilities at the times. Fathers can also visit their infants in specific hours, but they cannot stay there and no health care is provided for them. The premature birth rate in the place of research, Esfahan, Isfahan, is about 12-13%, and due to the prepared facilities, especially in the state hospitals, many of these infants would be saved. In Iran, no organized goal-oriented effort has been taken to increase the parents’ information and confidence and to decrease the mothers’ stress and anxiety following giving birth to an immature infant and its being in NICU. This would cause distress in mother-infant interaction, and so, the absence of timely and effective mothers’ participation in taking care of the infant. On the other hand, the nursing workload in NICUs is too high and nurses do not have enough time to help parents. Regarding without to these points, researchers tend to conduct the Creating Opportunities for Parent Empowerment (COPE) program in this survey. As a result, researchers tend to conduct the Creating Opportunities for Parent Empowerment (COPE) program in this survey. Due to the fact that it is both a written and audiotaped program and the information is provided in a simple language, it is not a time-consuming work for the nurses to transfer the information to the parents.
COPE program
The COPE program was developed by Dr. Bernadette Melnyk, Dean and Distinguished Foundation Professor in Nursing, Arizona State University College of Nursing and Healthcare Innovation. This program provides information in simple language in different media. During NICU stay, parents get printed materials and audiotapes. The goal is to teach parents the normal behaviors and characteristics of a preemie, and various activities help the parents to understand and appreciate their baby's special qualities. The content of the COPE program and skill-building activities is guided by self-regulation theory (Johnson, Fieler, Jones, Wlasowicz, and Mitchell, 1997) and control theory (Carver, 1979)[12] (as cited in Melnyk et al., 2001). On the basis of these theories, COPE intervention would strengthen parents’ knowledge and beliefs about their premature infants and their own parenting role and remove barriers that would inhibit them from participating in their infants’ care and interacting with them in a developmentally sensitive manner.[13]
The COPE program is a four-phase educational-behavioral intervention program. Phase I occurs 2-4 days after infants’ hospitalization, phase II occurs 2-4 days after phase I, phase III occurs 1-3 days before discharge to home, and the last one occurs 1 week after discharge from the NICU. In every phase, mothers get a pictorial booklet and related audiotaped information. Moreover, in order to implement the experimental information, parent is given a four-phase workbook and is supposed to do and record the related activities.
The content of these four phases is as follows. Phase I contains the tendered information about immature infant's physical and behavioral features, the differences between mature and immature infants, information about NICU's environment, and offers the strategies that help parents to participate in taking care of the infant. Workbook activities in this phase contain the activities to identify infant's features. Also, some milestones that the infant achieved while in the NICU are listed in the workbook and mothers are supposed to record the time that they occurred. In phase II, in addition to giving emphasis on the information in the first one, it renders new information about infant's behaviors, its growth and development, and gives further suggestions regarding increasing the mother's participation to take care of the infant and meeting its needs. The workbook of this phase contains activities that tend to identify the specific features of infant to understand infant's stress signs, or the signs of readiness for communication. In phase III, supplementary information about the details of infant's states and behavior, such as sleepiness, quiet alert state, or active alert state, and the best time to make communication with it is tendered. Also, related topics about parental role in the process of infant's smooth transition from hospital to home and continuance of mother-infant positive interaction are discussed. The activities of the workbook of this phase contain the items that help parents to identify specific behavioral signs in infant and providers the ability to calm it down at times of stress. Phase IV contains supplemental data about the behavior of immature infant and the parental role related to infant's growth and development, and also some suggestions to increase the mother-infant positive interaction. Workbook activities of this phase contain a series of specific techniques to improve the infant's cognitive development, such as songs and games, appropriate to its age.
MATERIALS AND METHODS
A randomized clinical trial was conducted. Data were collected from September 2009 to February 2010 in the educational NICUs of state hospitals affiliated to Isfahan University of Medical Sciences in Iran (20-bed NICU in Shaheed Beheshti Hospital and 14-bed NICU in Alzahra Hospital). Following the father's inability to stay long and take care of the infant in ward's environment, the study cases have been chosen among others. All mothers who were 18 years and older, could read and speak Persian, had no infant admitted to the NICU, and with infants with the following criteria participated in this study: (a) gestational age of 26-34 weeks, (b) birth weight of less than 2500 g and appropriate for gestational age, (c) anticipated survival, (d) singleton birth, (e) no severe handicapping conditions, and (f) born at the study sites. Mothers were excluded from the study if they did not visit their infants for more than 4 days and if their infants died or discharged before completing the COPE program.
Researchers screened 290 premature births and 135 of them met the eligibility criteria [Figure 1]. Among these 135 eligible births, 20 (14.8%) mothers refused participation, with the majority of them wanting to concentrate only on the new infant or they believed that participation would take time away from the other children at home. Researchers were unable to contact the mothers of 15 (11.1%) premature infants who met the eligibility criteria. Mothers who agreed to participate were randomly assigned to the study conditions by using RAND function in Excel 2007. The final sample after randomization comprised 100 mothers. After enrollment and randomization of the study groups, data for 10 mothers were eliminated from the study for analyses. Five mothers in the COPE program were eliminated from the study because of infant death (n = 2), transfer to another hospital (n = 1) or completion of baseline measures only (n = 2). Five comparison mothers also were eliminated from the analysis because of infant death (n = 2) or completion of baseline measures only (n = 3). Therefore, the final sample for data analyses included 90 mothers (45 in the COPE and 45 in the comparison group).
Figure 1.
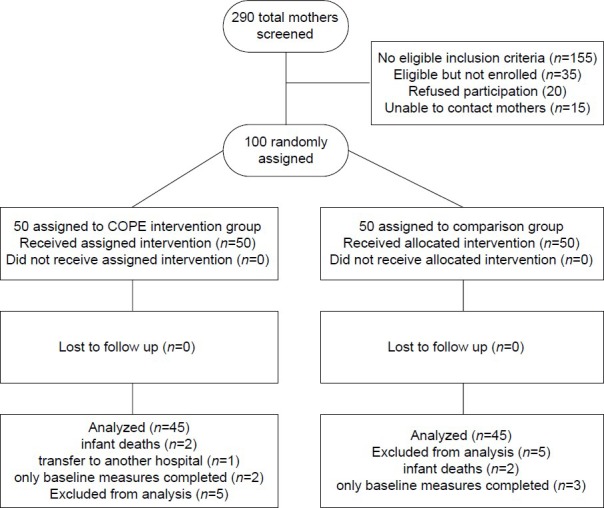
Study flowchart
The well-known State-Trait Anxiety Inventory (STAI)[14] was used to measure maternal state and trait anxiety. Current feelings of anxiety are measured with the A-State scale, while an individual's anxiety “proneness” is measured in the 20-item trait scale (A-Trait). A-State was used as the dependent variable to assess mothers’ current anxiety levels. Trait anxiety was assessed at one contact point only to measure anxiety proneness. Maternal trait anxiety and demographic measures are considered as important covariates in the study because findings from prior research have supported that these variables have potential effects on maternal state anxiety and mother-infant interaction.[13] The reliability was measured by Cronbach's alpha, and it was 0.93 for state anxiety and 0.87 for trait anxiety. Content Validity Index was measured as validity, and it was 0.97 for state anxiety and 0.99 for trait anxiety.
The Parental Stressor Scale: Neonatal Intensive Care (PSS: NICU)[15] assessed parental stress in the NICU arising from four dimensions: (a) sights and sounds, (b) infant behavior and appearance, (c) parental role alteration, and (d) staff behaviors and communication. Parents rate their perceptions of the stress level generated by each of the 46 items on a 5-point Likert scale ranging from 1 (=non-stressful) to 5 (=extremely stressful). Higher total scores indicate greater stress levels. Cronbach's alpha was 0.81 and Content Validity Index was 0.93.
The Index of Parental Participation/Hospitalized Infant (IPP-HI)[16] is an instrument that is designed for nurses and/or mothers to rate the range of care-related activities that mothers were observed or reported themselves to be involved in while there infant is hospitalized in an NICU. This instrument was used to measure maternal participation in her infant care. The IPP/HI is described as a 25-item dichotomous instrument that measures a range of previous 48-h time period activities of mothers, including items that pertain to routine infant care, basic illness-related care, emotional and developmental care, information seeking, and involvement in care by serving as an advocate and a decision-maker. Cronbach's alpha was 0.90 and Content Validity Index was 0.99.
Concerning the point that it takes more time to implement phase III of the COPE program and that phase IV is conducted on the basis of home visit which is not common in Iran, these phases were omitted with the program designer's permission. Therefore, phases I and II of the program were translated by researchers. The issues of every phase consist of the scientific information in simple language, which almost coincided with NICUs conditions in Iran. The necessary reformation regarding the context's eloquence and fluency was done with the help of three faculty members of the School of Nursing and Midwifery, Shaheed Beheshti Medical University. Then, the information was prepared in the form of audiotape and a booklet (a separate booklet for every phase with related picture). Finally, in order to measure the booklet and audiotape fluency and clearness in mothers’ opinion, a pilot study was done on five mothers. In each hospital, there was a suitable room (without noise and shuttling) beside the NICU, which were useless in the evening. These rooms were used for performing the program. Mothers came to this place alone and one of the researchers gave instruments to them to complete. COPE mother received the booklet and listened to the tape there.
Intervention group
Two to four days post NICU admission, the mother completed demographic and infant variables questionnaire as well as State Anxiety Inventory and The Parental Stressor Scale. Then, the phase I booklet was given to the mother and she listened to its audiotape. Immediately following the audiotape, the mother answered the phase I manipulation check. Manipulation checks consisted of 10 true or false questions that the mother answered immediately after each intervention phase to assure they processed the audiotaped information. The first set of activity workbook was then given to the mother with specific instructions on how to complete. Four to eight days post NICU admission, the mother completed STAI and The Parental Stressor Scale. Next, the phase 2 booklet was given to the mother and she listened to its audiotape. Then, the mother answered the phase 2 manipulation check questions, and at the end, she received phase II of activity workbook with specific instructions on how to complete. Six to twelve days post NICU admission was the last visit of the research for each mother and she completed State Anxiety Inventory, The Parental Stressor Scale, and the (IPP-HI). Researcher requested the mother to complete the workbook activities and she monitored them throughout the study. Researcher prompted the mothers who had not completed the activities by the time of the next phase of the intervention to perform them by the next contact.
Comparison group
Mothers in the comparison group filled out all questionnaires at the same time as the intervention group (2-4, 4-8, and 6-12 days after infant hospitalization). They did not receive the COPE program, but using the content of each phase of the COPE program, one of the researchers answered all their questions. After ultimate assessment (6-12 days after infant hospitalization), this group also received a booklet which is a combination of phases I and II of the COPE program. Mothers also could listen to the audiotaped information of this booklet.
RESULTS
Data were analyzed using SPSS 16 for Windows. A P value of ≤0.05 was set for statistical significance. Kolmogorov-Smirnov test showed that the distribution of data was normal. Descriptive statistics were conducted at baseline to summarize demographic and clinical variables. In addition, t-tests for continuous variables, χ2 analyses for categorical variables, and Mann-Whitney U test for qualitative variables were performed to determine if the two study groups differed in these baseline factors. Spearman correlation test and repeated measurements test were also performed.
Among the 90 mothers, 45 were in the intervention group and 45 in the comparison group. No significant group differences were found at baseline in maternal demographic and infant variables [Tables 1 and 2]. In addition, no baseline differences between groups were found for stress and anxiety [Table 3]. Effects of the intervention program on maternal outcomes are presented in Table 3.
Table 1.
Comparability of the COPE intervention and comparison groups’ conditions
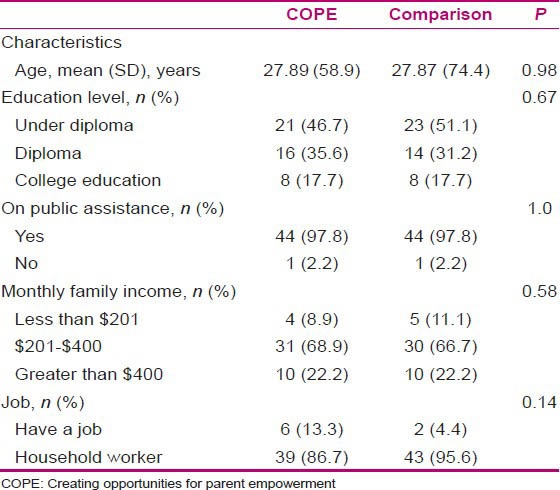
Table 2.
Comparability of the COPE intervention and comparison groups’ infant conditions
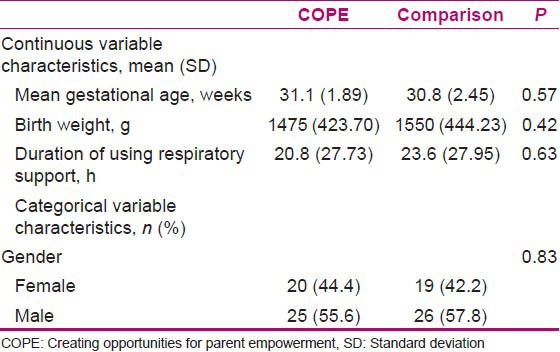
Table 3.
Maternal outcomes
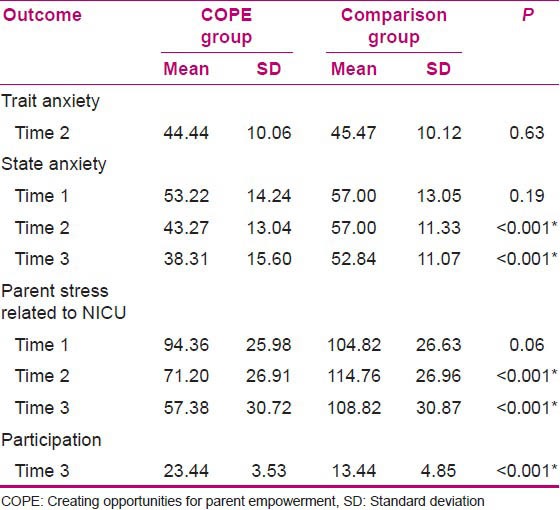
During the NICU hospitalization, mothers in the COPE program reported significantly less overall parental stress in the NICU than did mothers in the comparison group [Figure 2]. Mothers’ state anxiety decreased over time, with significant COPE and comparison-group differences identified [Figure 3]. Mothers in the COPE program were also more involved in their infants’ care in the NICU than the comparison mothers [Figure 4].
Figure 2.
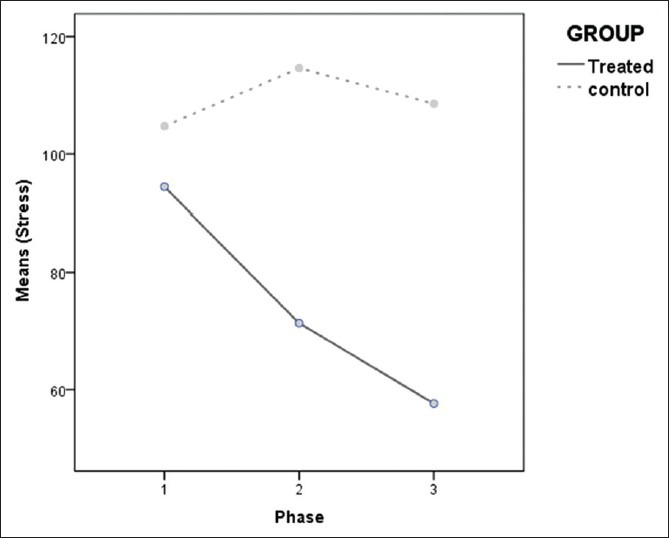
Maternal stress over time
Figure 3.
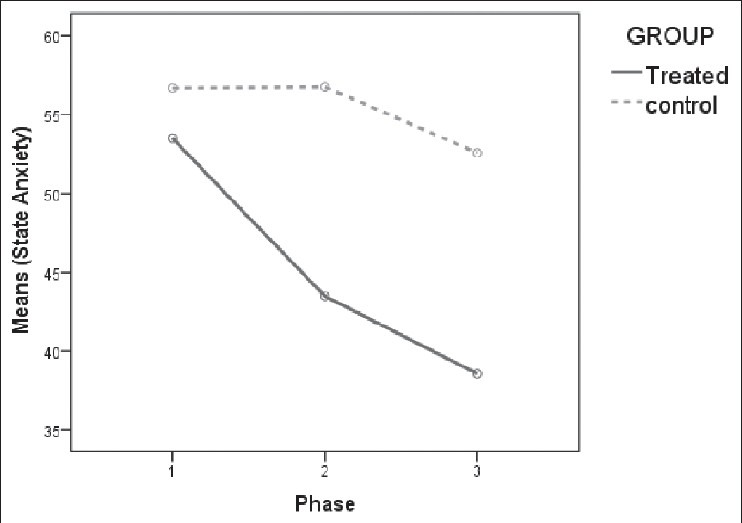
Maternal state anxiety over time
Figure 4.
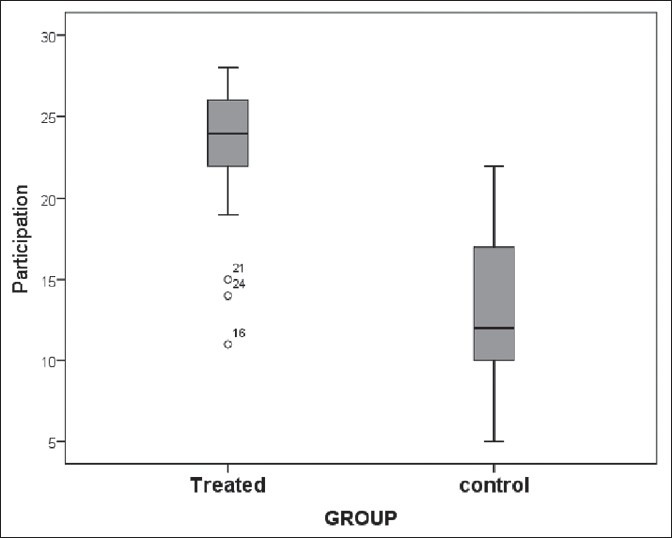
Maternal participation
COPE mothers had also significantly high total scores on the questions in manipulation checks dealing with the COPE-program content, indicating that mothers processed the content of the program from all two phases of the interventions.
DISCUSSION
The purpose of this study was to perform the COPE program for Iranian mothers and evaluate its effectiveness on the level of stress, anxiety, and participation of mothers who have premature infants hospitalized in NICUs. Findings of this study provide additional support for earlier studies that proved instructing parents in premature behavior and involving them in the care of their infant may facilitate bonding, increase parents’ confidence in care giving, and possibly improve the parent-child relationship.[11,17]
After performing just the first stage of the program, the state anxiety level of the mothers reduced, and after performing phase II of the program, the state anxiety level of the mothers further reduced. Since most mothers’ education was less than diploma, it can be said that the information in phases I and II could the level of education in most of the mothers was less than diploma (high school), it can be said that the information in phases I and II could provide Iranian mothers’ information needs. Clear information of the infant's condition provided for parents on a regular basis facilitates accurate perception of the infant's morbidity, with subsequent alterations in distress levels.[8] After performing two phases of COPE program, mothers’ stress reduced in the experimental group, while assessments conducted at the same time in the control group indicated that stress in the second assessment was more than in the first one. This finding indicates that parents of premature infants experience heightened anxiety and stress during and following their infants’ NICU stay.[5,9,18] COPE mothers were significantly less stressed related to NICU because they were given concrete information regarding the NICU environment and what to expect of their premature infants.[12]
The results of this study showed that the mothers’ participation in the experimental group was more than that in the control group. Through the parental role information in the COPE program, mothers learned how best to interact with their infants during hospitalization and were encouraged to be involved in their infants’ care.[13] Nursing support reduces parental stress and anxiety during infants’ NICU hospitalization and, therefore, fosters the parents’ abilities to cope with the difficulties they are facing.[19] Giving understandable information is critical for optimal parental involvement in their infant's care.[20]
In the study of Melnyk et al. (2006), all four phases of the COPE program were conducted in the USA. The results of this study demonstrate the following: Mothers in the COPE program reported significantly less overall parental stress in the NICU than did mothers in the comparison group, the level of mothers’ anxiety reduced at the end of program (after performing phase IV), and the mother's participation in taking care of the infant did not have significant statistical differences between the two groups. Contrasting this study with the study of Melnyk et al. (2006), the findings of the two studies are the same in the effect of program on the mothers’ stress related to NICU. However, the results of anxiety and participation are different. Also, there are differences in the socioeconomic status of samples in the two studies. Most of the mothers’ education was less than a diploma in the present study, while most of the mothers had an education level of more than a diploma in the study of Melnyk et al. (2006). Also, the income of most of the families in this study was less than $4000, but the families in Melnyk et al.'s (2006) study had more than $40,000 as income. According to the above analysis, further and earlier effect of program in this study can be due to economical and cultural differences between samples. On the other hand, welfare and educational facilities and psychological support are not the same in these two countries. This is the supportive finding for this claim that higher SES socioeconomic status mothers have stricter and more demanding cognitive schemas for their own beliefs/confidence in how they should parent their premature infants, while lower socioeconomic status mothers may have schemas that are less rigid.[13]
One of the limitations of this study is that it was conducted in only the state hospitals. Potential differences in practice may exist in private institutions that may influence generalizability of the findings. Another limitation that should be noted is that the samples were only mothers. It also would be possible to determine if the intervention program may have positive effect on fathers’ psychological condition in the situation that they could not participate in their infants’ care during hospitalization in the NICU.
CONCLUSION
Analyzing the results of the present study specified that psychological status and participation of Iranian mothers who had premature infants improved by presenting COPE intervention in the NICUs. During this program, mothers knew about the differences between their infants and mature infants, and they learned how to play their maternal role in the NICU and how to interact suitably with their infants. Therefore, the results of this study confirm the findings of previous studies regarding theory-based intervention with parents of premature infants that begins early in the NICU stay and results in (1) less parental stress in the NICU, (2) more positive parent-infant interactions in the NICU, and (3) less parental anxiety after hospitalization.[21] This study shows that these results can be the same in completely different countries.
ACKNOWLEDGMENTS
The authors acknowledge all mothers and their preterm babies who participated in this study. They also acknowledge Dr. Melnyke for her great help and guidance.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Jotzo M, Poets CF. Helping parents cope with the trauma of Premature Birth: An Evaluation of a trauma-preventive psychological intervention. Pediatrics. 2005;115:915–9. doi: 10.1542/peds.2004-0370. [DOI] [PubMed] [Google Scholar]
- 2.Kaaresen PI, Rønning JA, Ulvund SE, Dahl LB. A randomized controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics. 2006;118:9–19. doi: 10.1542/peds.2005-1491. [DOI] [PubMed] [Google Scholar]
- 3.Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005;49:608–15. doi: 10.1111/j.1365-2648.2004.03336.x. [DOI] [PubMed] [Google Scholar]
- 4.Nagata M, Nagai Y, Sobajima H, Ando T, Honjo S. Depression in the early postpartum period and attachment to children-in mothers of NICU infants. Infant Child Dev. 2004;13:93–110. [Google Scholar]
- 5.Carter JD, Mulder RT, Darlow BA. Parental stress in the NICU: The influence of personality, psychological, pregnancy and family factors. Pers Mental Health. 2007;1:40–50. [Google Scholar]
- 6.Younger JB, Kendell MJ, Pickler RH. Mastery of stress in mothers of premature infants. J Spec Pediatr Nurs. 1997;2:29–35. doi: 10.1111/j.1744-6155.1997.tb00197.x. [DOI] [PubMed] [Google Scholar]
- 7.Garel M, Dardennes M, Blondel B. Mothers’ psychological distress 1 year after very preterm childbirth. Results of the epipage qualitative study. Child Care Hlth Dev. 2006;33:137–43. doi: 10.1111/j.1365-2214.2006.00663.x. [DOI] [PubMed] [Google Scholar]
- 8.Trombini E, Surcinelli P, Piccioni A, Alessandroni R, Faldella G. Environmental factors associated with stress in mothers of preterm newborns. Acta Paediatr. 2008;97:894–8. doi: 10.1111/j.1651-2227.2008.00849.x. [DOI] [PubMed] [Google Scholar]
- 9.Zelkowitz P, Papageorgiou A, Bardin C, Wang T. Persistent maternal anxiety affects the interaction between mothers and their very low birth weight children at 24 months. Early Hum Dev. 2009;85:51–8. doi: 10.1016/j.earlhumdev.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Wigert H, Johansson R, Berg M, Hellstrom H. Mothers’ experiences of having their newborn child in a neonatal intensive care unit. Scand J Caring Sci. 2006;20:35–41. doi: 10.1111/j.1471-6712.2006.00377.x. [DOI] [PubMed] [Google Scholar]
- 11.Sloan K, Rowe J, Jones L. Stress and coping in fathers following the birth of a preterm infant. J Neonatal Nurs. 2008;14:108–15. [Google Scholar]
- 12.Melnyk BM, Alpert-Gillis L, Feinstein NF, Fairbanks E, Schultz-Czarniak J, Hust D, et al. Improving cognitive development of low-birth-weight premature infants with the COPE program: A pilot study of the benefit of early NICU intervention with mothers. Res Nurs Health. 2001;24:373–89. doi: 10.1002/nur.1038. [DOI] [PubMed] [Google Scholar]
- 13.Melnyk BM, Crean HF, Fischbeck-Feinstein N, Fairbanks E. Maternal anxiety and depression following a premature infants’ discharge from the NICU: An integrative model of the COPE program. Nurs Res. 2007;57:383–94. doi: 10.1097/NNR.0b013e3181906f59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spielberger C, Gorsuch R, Lushene R. Palo Alto, CA: Consulting Psychologists; 1997. The STAI Manual. [Google Scholar]
- 15.Miles M. Parents of critically ill premature infants: Sources of stress. Crit Care Nurs Q. 1989;12:69–74. doi: 10.1097/00002727-198912000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Melnyk BM, Alpert-Gillis LJ, Hensel PB. Helping Mothers Cope with a Critically Ill Child: A Pilot Test of the COPE Intervention. Res Nurs Health. 1997;20:3–14. doi: 10.1002/(sici)1098-240x(199702)20:1<3::aid-nur2>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 17.Maguire CM, Bruil J, Wit JM, Walther FJ. Reading premature infants’ behavioral cues: An intervention study with parents of premature infants born b32 weeks. Early Hum Dev. 2007;83:419–24. doi: 10.1016/j.earlhumdev.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Browne JV, Talmi A. Family-based interventions to enhance infant-parent relationships in the neonatal intensive care unit. J Pediatr Psychol. 2005;30:667–77. doi: 10.1093/jpepsy/jsi053. [DOI] [PubMed] [Google Scholar]
- 19.Ichijima E, Kirk R, Hornblow A. Parental support in neonatal intensive care units: A cross-cultural comparison between New Zealand and Japan. J Pediatr Psychol. 2011;26:206–15. doi: 10.1016/j.pedn.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Cone S. The Impact of communication and the neonatal intensive care unit environment on parent involvement. Newborn Infant Nurs Rev. 2007;7:33–8. [Google Scholar]
- 21.Melnyk BM, Fischbeck-Feinstein N, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants ‘length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment neonatal intensive care unit program: A randomized controlled trial. Pediatrics. 2006;118:1414–37. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]


