Abstract
Introduction: Necrobiosis lipoidica (NL) is a rare chronic granulomatous dermatitis that usually appears in the lower extremities. It affects about 0.3–1.2% of diabetic patients, the majority of whom have type 1 diabetes. The etiology and pathogenesis of this disorder are still unclear. NL is characterized by skin rash that usually affects the shins. The average onset is 30 years, with females being affected more commonly. There are very few reported cases of necrobiosis lipoidica in children.
Case report: We report a case of a 16 year old girl affected by type 1 diabetes mellitus (15 years disease duration) who developed an erythematous nodular rash on the lower extremities and interscapular area. In the suspect of necrobiosis lipoidica, a skin biopsy was performed (lower extremities and interscapular area). The microscopic evaluation of the pretibial lesions was suggestive of necrobiosis lipoidica. The smaller lesions in the interscapular area showed signs of perivascular dermatitis which could be consistent with early stages of necrobiosis lipoidica. Local treatment with tacrolimus determined a progressive improvement of the lesions.
Conclusion: In patients with T1DM, diagnosis of NL of the lower legs is usually unequivocal. However, diagnosis may be more challenging in the presence of lesions with recent onset and/or atypical clinical presentation and unusual site. In these cases, NL must always be taken in consideration in order to avoid misdiagnosis, wrong/late treatment decisions and progression to ulceration.
Keywords: diabetes, necrobiosis lipoidica, T1DM, skin lesion, type 1 diabetes, granulomatous dermatitis, children
Introduction
Necrobiosis lipoidica (NL) is a rare chronic granulomatous dermatitis first described in 1929 by Oppenheim that usually appears in the lower extremities that affects about 0.3–1.2% of diabetic patients, the majority of whom have type 1 diabetes.1 The etiology and pathogenesis of this disorder are still unclear. NL is characterized by a skin rash that usually affects the shins. The average onset is 30 y, with females being affected more commonly. There are very few reported cases of necrobiosis lipoidica in children. We report a case of a 16 y old girl who developed lesions on the lower extremities and in the interscapular area, which is an unusual location.
Case report
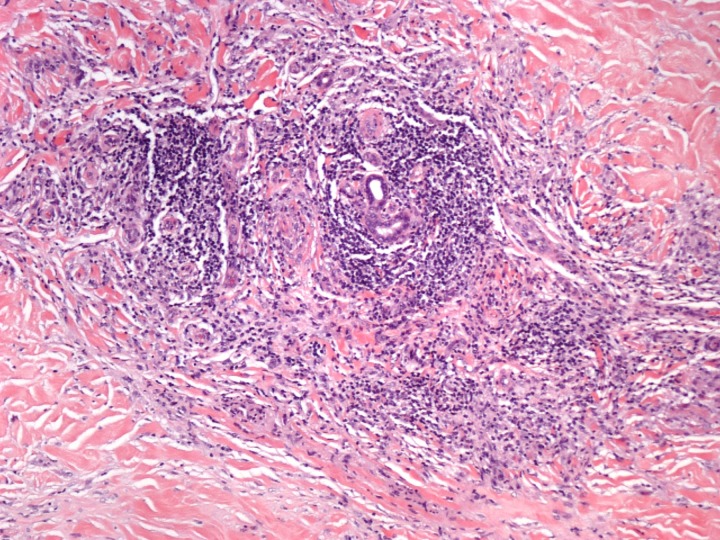
The patient, a Caucasian 16-y-old girl, was born at term by non-consanguineous, healthy parents. Type 1 diabetes (T1DM) had been diagnosed at one year of age. Our patient’s medical history was otherwise unremarkable. Until the age of 12 she maintained an adequate glucose control with HbA1c < 34 mmol/mol. Thereafter her glucose control progressively worsened with a HbA1c of 86 mmol/mol. At the age of 16, during a routine diabetes follow-up visit, the patient presented with erythematous subcutaneous nodular lesions which had appeared 4 mo earlier, initially in the pretibial area and subsequently in the interscapular area. Her HbA1c was 64 mmol/mol and daily insulin requirements were 0.95 U/kg/day. In the suspect of necrobiosis lipoidica, a skin biopsy was performed (lower extremities and interscapular area) (Figs. 1 and 2). The microscopic evaluation of the pretibial lesions was suggestive of necrobiosis lipoidica. The smaller lesions in the interscapular area showed signs of perivascular dermatitis which could be consistent with early stages of necrobiosis lipoidica (Fig. 3). Local treatment with tacrolimus determined a progressive improvement of the lesions. Diabetes self-management education was reinforced and her HbA1c showed a gradual reduction.
Figure 1. Erythematous and subcutaneous nodular lesions at the lower limbs
Figure 2. Erythematous and subcutaneous nodular lesions at the intrascapular region
Figure 3. Focal collagen necrosis with surrounding histiocytes that palisade in a radial pattern. Mononuclear and plasmacellular interstitial infiltrate.
Discussion
NL in the pediatric population has been described in 2.3% of cases.2 It usually consists of a rash involving the lower extremities. It may initially be represented by erythematous circular papules which may gradually progress to yellowish-brown, telangectatic plaques with central atrophy and raised violaceous border. It rarely involves hands, fingers, face and scalp.3 The etiology of NL is still currently elusive and few data exist regarding the pediatric population. However, due to the significant relationship with diabetes (75–90% of patients with NL have or will develop T1DM), many studies have proposed microangiopathy as leading etiological suspect. Immune-complex vasculitis and collagen abnormalities may also represent potential underlying causes.4 Previous studies have shown that glucose control does not appear to be correlated with NL onset and severity. However, a study by Cohen concluded on the contrary, that NL is usually associated with poor glucose control and that a tighter glucose control, as currently practiced, might improve or prevent this disorder.5
Diagnosis of NL is mainly clinical, but a bioptic evaluation may be useful especially in the early stages of disease. Differential diagnosis include erythema nodosum, lupus panniculitis, granuloma annulare, sarcoidosis and amyloidosis.
Microscopic evaluation usually shows degeneration of collagen, granulomatous inflammation of subcutaneous tissues and of blood vessels, capillary basement membrane thickening and obliteration of vessel lumen. Spontaneous remission of NL may present in less than 20% of cases. Ulceration is the most frequent complication and appears in 25–33% of cases. Rarely, squamous cell carcinoma may develop in areas of NL.6 Several therapeutic options for NL can be proposed. However its treatment still remains a challenge. Initial therapy includes topical, intralesional or systemic corticosteroids. Some authors have reported a beneficial effect from smoking cessation and blood glucose control. Other therapeutic options are antiplatelet agents, cyclosporine, thalidomide, clofazimine, anti-TNF agents, fumaric acid esters, PUVA, photodynamic therapy, hydroxychloroquine, and tacrolimus.7-13
Conclusions
In patients with T1DM, diagnosis of NL of the lower legs is usually unequivocal. However, diagnosis may be more challenging in the presence of lesions with recent onset and/or atypical clinical presentation and unusual site. In these cases, NL must always be taken in consideration in order to avoid misdiagnosis, wrong/late treatment decisions and progression to ulceration.
Consent
Written informed consent was obtained from the patient and parents for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Glossary
Abbreviations:
- NL
Necrobiosis lipoidica, T1DM, Type 1 diabetes
Footnotes
Previously published online: www.landesbioscience.com/journals/dermatoendocrinology/article/27790
References
- 1.Ahmed I, Goldstein B. Diabetes mellitus. Clin Dermatol. 2006;24:237–46. doi: 10.1016/j.clindermatol.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Pavlović MD, Milenković T, Dinić M, Misović M, Daković D, Todorović S, Daković Z, Zecevi RD, Doder R. The prevalence of cutaneous manifestations in young patients with type 1 diabetes. Diabetes Care. 2007;30:1964–7. doi: 10.2337/dc07-0267. [DOI] [PubMed] [Google Scholar]
- 3.Dissemond J. Images in clinical medicine. Necrobiosis lipoidica diabeticorum. N Engl J Med. 2012;366:2502. doi: 10.1056/NEJMicm1109700. [DOI] [PubMed] [Google Scholar]
- 4.Scaramuzza A, Macedoni M, Tadini GL, De Angelis L, Redaelli F, Gazzarri A, Comaschi V, Giani E, Zuccotti GV. Necrobiosis lipoidica diabeticorum. Case Rep Pediatr. 2012;2012:152602. doi: 10.1155/2012/152602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gottrup F, Karlsmark T. Leg ulcers: uncommon presentations. Clin Dermatol. 2005;23:601–11. doi: 10.1016/j.clindermatol.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 6.Hammami H, Youssef S, Jaber K, Dhaoui MR, Doss N. Perforating necrobiosis lipoidica in a girl with type 1 diabetes mellitus: a new case reported. Dermatol Online J. 2008;14:11. [PubMed] [Google Scholar]
- 7.Patsatsi A, Kyriakou A, Sotiriadis D. Necrobiosis lipoidica: early diagnosis and treatment with tacrolimus. Case Rep Dermatol. 2011;3:89–93. doi: 10.1159/000327936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eberle FC, Ghoreschi K, Hertl M. Fumaric acid esters in severe ulcerative necrobiosis lipoidica: a case report and evaluation of current therapies. Acta Derm Venereol. 2010;90:104–6. doi: 10.2340/00015555-0757. [DOI] [PubMed] [Google Scholar]
- 9.Berking C, Hegyi J, Arenberger P, Ruzicka T, Jemec GB. Photodynamic therapy of necrobiosis lipoidica--a multicenter study of 18 patients. Dermatology. 2009;218:136–9. doi: 10.1159/000182259. [DOI] [PubMed] [Google Scholar]
- 10.Peyrí J, Moreno A, Marcoval J. Necrobiosis lipoidica. Semin Cutan Med Surg. 2007;26:87–9. doi: 10.1016/j.sder.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Kavala M, Sudogan S, Zindanci I, Kocaturk E, Can B, Turkoglu Z, Altintas S. Significant improvement in ulcerative necrobiosis lipoidica with hydroxychloroquine. Int J Dermatol. 2010;49:467–9. doi: 10.1111/j.1365-4632.2010.04149.x. [DOI] [PubMed] [Google Scholar]
- 12.Clayton TH, Harrison PV. Successful treatment of chronic ulcerated necrobiosis lipoidica with 0.1% topical tacrolimus ointment. Br J Dermatol. 2005;152:581–2. doi: 10.1111/j.1365-2133.2005.06388.x. [DOI] [PubMed] [Google Scholar]
- 13.Narbutt J, Torzecka JD, Sysa-Jedrzejowska A, Zalewska A. Long-term results of topical PUVA in necrobiosis lipoidica. Clin Exp Dermatol. 2006;31:65–7. doi: 10.1111/j.1365-2230.2005.01962.x. [DOI] [PubMed] [Google Scholar]