Abstract
Background:
The management of Duane retraction syndrome (DRS) is challenging and may become more difficult if an associated accommodative component due to high hyperopia is present. The purpose of this study is to review clinical features and outcomes in patients with partially accommodative esotropia and DRS.
Setting and Design:
Retrospective, non-comparative case series.
Materials and Methods:
Six cases of DRS with high hyperopia were reviewed.
Results:
Of the patients studied, the mean age of presentation was 1.3 years (range: 0.5-2.5 years). The mean amount of hyperopia was + 5D (range: 3.50-8.50) in both eyes. The mean follow up period was 7 years (range: 4 months-12 years). Five cases were unilateral while one was bilateral. Four cases underwent vertical rectus muscle transposition (VRT) and one had medial rectus recession prior to presentation; all were given optical correction. Two (50%) of the four patients who underwent vertical rectus transposition cases developed consecutive exotropia, one of whom did not have spectacles prescribed pre-operatively. All other cases (four) had minimal residual esotropia and face turn at the last follow-up with spectacle correction.
Conclusion:
Patients with Duane syndrome can have an accommodative component to their esotropia, which is crucial to detect and correct prior to surgery to decrease the risk of long-term over-correction. Occasionally, torticollis in Duane syndrome can be satisfactorily corrected with spectacles alone.
Keywords: Duane syndrome, esotropia, strabismus
Duane retraction syndrome (DRS) patients can be orthotropic, esotropic, or exotropic in the primary position. Indications for surgery include ocular misalignment in the primary position, noticeable abnormal head position, severe globe retraction in side gaze, and abnormal vertical movements.[1] Surgical management of esotropic DRS includes options such as medial rectus muscle recession[2] or vertical rectus transposition.[3]
DRS can be associated with refractive errors. In particular, hyperopia is present in 57-82% of patients.[4,5,6] High hyperopia, defined as a refractive error greater than 4 D is present in less than 25% of patients with DRS.[5] Hyperopia can be associated with accommodative esotropia. The management of accommodative esotropia is typically optical with spectacle correction of the full cycloplegic refraction. Surgery is indicated only for the non-accommodative component, which manifests after full cycloplegic correction. Although some authors suggest that by operating for a higher angle of esotropia than the non-accommodative component, the need for hyperopic correction may be reduced or eliminated.[7,8] Kushner reported that surgical overcorrection in patients with partly accommodative esotropia with hyperopia greater than 2.5 diopters may not be reversible by postoperative reduction in the hyperopic correction.[9] There has been no previous study evaluating esotropic DRS with co-existent partially accommodative esotropia, yet the management of accommodative esotropia is quite different than that of DRS, with optical management being the treatment of choice.[10]
Given the differences in suggested management of partially or fully accommodative esotropia and DRS, we present our experience of managing these patients. The purpose of our study is to analyze the clinical findings and outcome of alignment in this group of patients.
Materials and Methods
After approval from the Institutional Review Board at University of California, Los Angeles, eligible patients were identified from a computerized database including patients seen between 2000 and 2010. The chart review adhered to the Declaration of Helsinki and all relevant privacy laws. Inclusion criteria were (1) Diagnosed case of esotropic DRS; and (2) Hyperopia greater than + 3.50 D in each eye. For the diagnosis of DRS, patients had to demonstrate limitation of abduction and palpebral fissure narrowing with globe retraction on adduction. Patients were excluded if they had less than 4 months of follow up. All preoperative and postoperative data were obtained with prism alternate cover tests at 20-foot distance targets and 13 inches for near targets or Krimsky's method measurements. Voluntary versions were performed on all patients and recorded as a 6-point scale: 0 = full movement, −1 = restriction to 45° of abduction, −2 = limited movement to 30°, −3 = limited movement to 15°, −4 = unable to move the eye past the midline, −5 = unable to rotate the eye to midline. All surgical procedures were also recorded for each eye. Face turn was measured subjectively at the clinical discretion of the operating surgeon.
The surgical approach for VRT followed the previous description by Foster and Rosenbaum including the use of posterior fixation augmentation sutures.[3,11] Cycloplegic refraction and ocular motility evaluation were performed at regular intervals during the follow-up period.
Data collected included age, sex, laterality, cycloplegic refraction reading, amount of tropia, face turn, type and amount of surgery, and pre-operative and post-operative ocular alignment and torticollis measurements. Results are reported as mean ±1 SD.
Results
A total of 59 records of patients diagnosed with esotropic DRS were available for review. Of these, six patients met the study inclusion criteria. Patient characteristics for the six patients are summarized in Table 1. The age at presentation of the patients ranged between 0.5-2.5 years (mean 1.3 years). Five cases were unilateral (left) and one was bilateral. All had hyperopia ranging from +3.50 to +8.50 (mean 5) D. Mean preoperative esotropia in forced primary position was 19 ± 7 prism diopters. Mean face turn was 14 ± 8°.
Table 1.
Demographic and surgical details of patients with accommodative esotropia and duane retraction syndrome
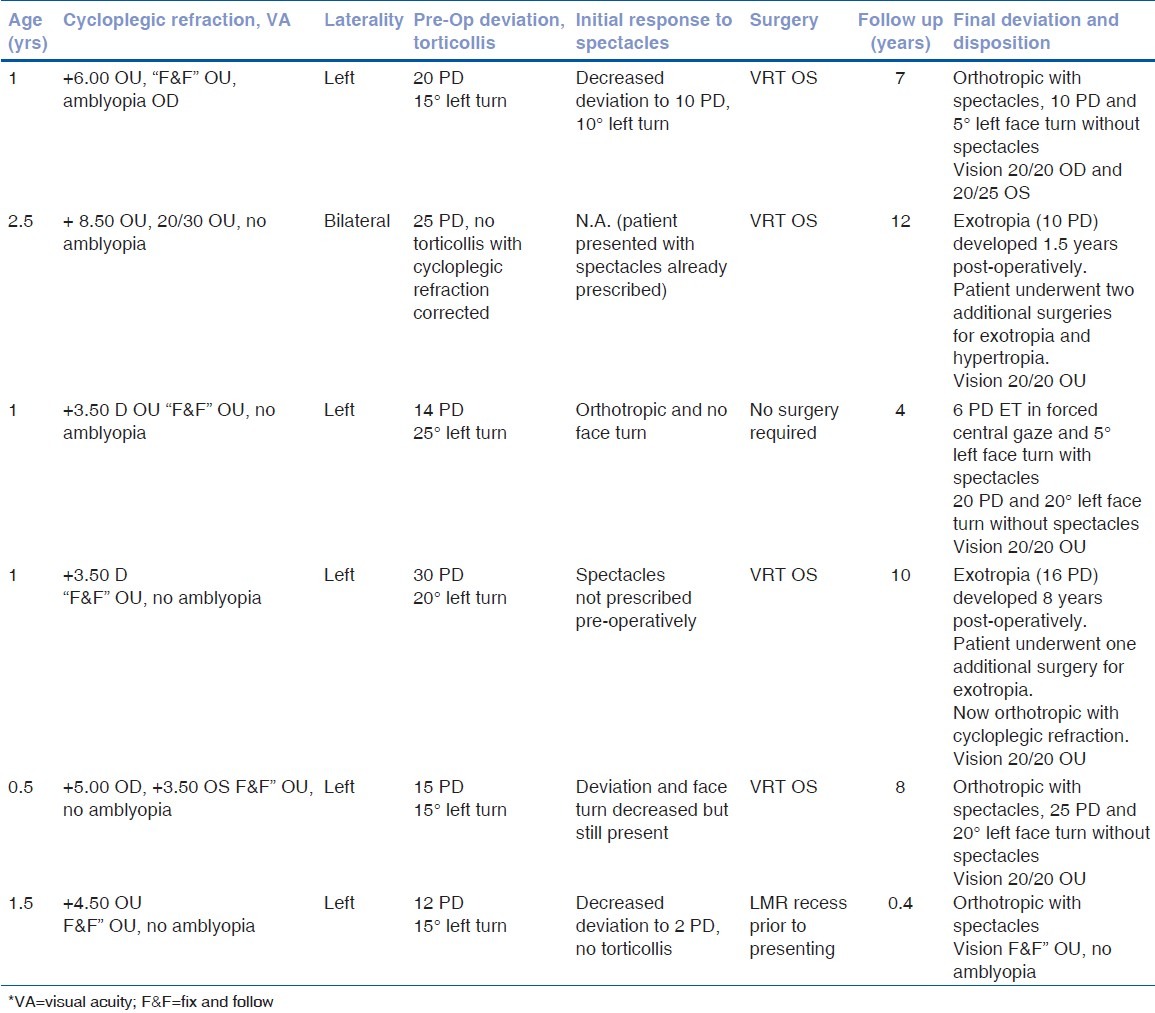
VRT was performed in four cases and one had unilateral medial rectus recession. Face turn and esotropia in primary position was eliminated with just spectacles in one case, glasses and left medial rectus recession in one case (surgery performed prior to presenting at our institution), and VRT and glasses in two cases Fig. 1. Of these four cases, all patients continued to demonstrate an esotropia and face turn without their hyperopic spectacles during the follow-up period. Out of four cases that had VRT two cases developed consecutive exotropia and required further surgical correction. The exotropia was not present immediately post-operatively and was first detected 1.5 and 8 years post-operatively. Both patients initially were not exotropic for at least the first post-operative year. One of these cases were not prescribed hyperopic spectacles pre-operatively and one had very high hyperopia (+8.50). Mean follow-up period for all patients was 7 ± 4 years.
Figure 1.

Patient in preferred head posture without (Left Panel) and with (Right Panel) hyperopic spectacle correction. Resolution of torticollis is seen with the use of spectacles.
Discussion
Esotropic DRS is managed by one of several surgical procedures. These include recession of the ipsilateral medial rectus muscle with or without a posterior fixation suture on the contralateral medial rectus muscle, bilateral medial rectus muscle recession and augmented VRT with or without medial rectus muscle recession.[3,12,13,14,15] However, the coexistence of an accommodative esotropia makes the management of DRS more challenging as a failure to detect and treat it may lead to long-term post-operative overcorrection or other difficulties associated with overcorrection in accommodative esotropia.[9] The management of partially accommodative esotropia without DRS involves titrating the amount of medial rectus muscle recession according to the amount of esotropia present with hyperopic correction. Although some authors recommend overcorrection,[9] the prevailing recommendation is to avoid overcorrection of the accommodative component of the esotropia to minimize the risk of long-term consecutive exotropia. However, the role that coexistent accommodative esotropia has in DRS patients with high hyperopia has not been well described and although the accommodative component is not directly linked to the underlying pathophysiology of DRS, it is important to recognize their coexistence in certain cases.
Earlier, Molarte et al. reported series of VRT surgery in 13 patients with DRS. Six of thirteen patients required additional medial rectus muscle recession.[3] None of the patients developed consecutive exotropia. We performed VRT in four cases in this study. Among the VRT cases, two developed overcorrection that needed further corrective surgery - given that these exotropias presented late, it is likely that they may have been related to a decrease in the accommodative component with a decreasing amount of hyperopia. We do not know whether these overcorrections could have been avoided by prescribing spectacles in the case that did not have pre-operative spectacles prescribed and detecting more latent hyperopia in the case that was treated pre-operatively with spectacles; however, theoretically if the pre-operative esotropia was smaller (due to more correction of an accommodative component), then perhaps a less aggressive surgical procedure may have been considered such as a small medial rectus recession or a VRT without posterior fixation suture. The consecutive exotropia that developed in these cases after the VRT did not respond to undercorrection of hyperopia as is often the case in partially accommodative esotropia, and both patients required lateral rectus muscle recession thereby underscoring the importance of detecting and treating esotropic DRS with co-existent partially accommodative esotropia.
Our study should be understood within the context of its limitations. First, it is a retrospective study that may have some selection bias based on our location as a tertiary referral center. Second, the sample size is small due to the relative rarity of this disorder. Finally, follow-up is variable and ranges from four months to 12 years thereby presenting the possibility of follow-up bias.
Despite its limitations, we believe that this study demonstrates a crucial phenomenon in patients with DRS and high hyperopia. The overcorrection that occurred years after surgery in one patient who was not prescribed spectacles pre-operatively to detect an accommodative component points out the need for vigilance in performing cycloplegic refraction in all DRS patients prior to performing surgery and targeting surgery to the non-accommodative component. The remainder of the patients in this series demonstrate that results after VRT can be excellent in this sub-class of patients with coexistent accommodative esotropia and esotropic DRS if the hyperopia is adequately corrected. Finally, there are also likely patients who will obtain relief of torticollis and primary position esotropia in Duane syndrome simply with spectacle correction alone.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Jampolsky A. Duane Syndrome. In: Rosenbaum AL, Santiago AP, editors. Clinical Strabismus Management. Philadelphia: WB Saunders; 1999. pp. 325–46. [Google Scholar]
- 2.Farvardin M, Rad AH, Ashrafzadeh A. Results of bilateral medial rectus muscle recession in unilateral esotropic Duane syndrome. J AAPOS. 2009;13:339–42. doi: 10.1016/j.jaapos.2009.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Molarte AB, Rosenbaum AL. Vertical rectus muscle transposition surgery for Duane's syndrome. J Pediatr Ophthalmol Strabismus. 1990;27:171–7. doi: 10.3928/0191-3913-19900701-03. [DOI] [PubMed] [Google Scholar]
- 4.Anvari FE, Mohammadi SF, Eskandari A. Duane's retraction syndrome, a case series from Iran. Int Ophthalmol. 2008;28:275–80. doi: 10.1007/s10792-007-9125-y. [DOI] [PubMed] [Google Scholar]
- 5.Kirkham TH. Anisometropia and amblyopia in Duane's syndrome. Am J Ophthalmol. 1970;69:774–7. doi: 10.1016/0002-9394(70)93419-7. [DOI] [PubMed] [Google Scholar]
- 6.Tredici TD, Von Noorden GK. Are anisometropia and amblyopia common in Duane's syndrome? J Pediatr Ophthalmol Strabismus. 1985;22:23–5. doi: 10.3928/0191-3913-19850101-08. [DOI] [PubMed] [Google Scholar]
- 7.Wright KW, Bruce-Lyle L. Augmented surgery for esotropia associated with high hypermetropia. J Pediatr Ophthalmol Strabismus. 1993;30:167–70. doi: 10.3928/0191-3913-19930501-09. [DOI] [PubMed] [Google Scholar]
- 8.Gobin M. Should accommodative strabismus be operated on? J Fr Ophtalmol. 1992;15:483–91. [PubMed] [Google Scholar]
- 9.Kushner BJ. Partly accommodative esotropia. Should you overcorrect and cut the plus? Arch Ophthalmol. 1995;113:1530–4. doi: 10.1001/archopht.1995.01100120060010. [DOI] [PubMed] [Google Scholar]
- 10.Von Noorden GK. Binocular Vision and Oclular Motility. St Luis, MO: CV Mosby Co; 1985. pp. 282–3. [Google Scholar]
- 11.Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997;1:20–30. doi: 10.1016/s1091-8531(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 12.Puerto-Hernandez B, Lopez-Caballero C, Rodriguez-Sanchez JM, Gonzalez-Manrique M, Contreras I. Surgical treatment of Duane's syndrome type I by recession of the medial rectus of the affected eye and faden operation of the contralateral medial rectus. Arch Soc Esp Oftalmol. 2008;83:113–6. doi: 10.4321/s0365-66912008000200009. [DOI] [PubMed] [Google Scholar]
- 13.Kraft SP. A surgical approach for Duane syndrome. J Pediatr Ophthalmol Strabismus. 1988;25:119–30. doi: 10.3928/0191-3913-19880501-06. [DOI] [PubMed] [Google Scholar]
- 14.Barbe ME, Scott WE, Kutschke PJ. A simplified approach to the treatment of Duane's syndrome. Br J Ophthalmol. 2004;88:131–8. doi: 10.1136/bjo.88.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greenberg MF, Pollard ZF. Poor results after recession of both medial rectus muscles in unilateral small-angle Duane's syndrome, type I. J AAPOS. 2003;7:142–5. doi: 10.1016/mpa.2003.S1091853102420010. [DOI] [PubMed] [Google Scholar]


