Abstract
Context:
Donor tissue scarcity, Eye Bank Specular Microscopy as yet not made mandatory and tissue utilization often based on clinical judgment only.
Aims:
Prospectively analyze alteration in clinical grading of donor corneas and hence utilization, based on Eye Bank Specular Microscopy (EBSM) and to infer if EBSM should be mandatory in all eye banks.
Materials and Methods:
200 consecutive otherwise ‘suitable for surgery’ donor eyes were graded clinically. On quantitative and qualitative analysis of endothelial cells by EBSM, final grading was adjusted. Impact on subsequent utilization for various surgeries was analyzed with regard to Age of Donor, Death to Enucleation Time, Death to Preservation Time and Lens Status of Donor Eye.
Results:
76 eyes (38%) (P < 0.05) had significant change in grading. 12/59 (20.30%) tissues from donors <=40 years showed Cell Density (CD) between 1801-2500. 19/76 (25%) tissues from donor >60 years showed CD >= 2500. From donor >=81 years, 2/13 (15.3%) eyes showed CD between 2501-3000 and 1 (7.6%) eye showed CD > 3000. Owing to better grading after EBSM, 13/14 (92.85%) tissues with DTET >6 hours and 5/5 (100%) tissues with DTPT > 16 hours were transplanted. Out of 45 (22.5%) pseudo-phakic tissues, 21 (46.67%) tissues were used for Therapeutic/Tectonic Penetrating Keratoplasty (PKP) while 24 (53.33%) tissues were used for Optical PKP.
Conclusions:
EBSM significantly alters final grading of tissues and its subsequent utilization. Acquiring huge importance in areas where adequate supply of corneas is lacking, EBSM becomes an indispensable tool for optimizing availability of qualified tissues for surgery. EBSM should be made a mandatory analysis.
Keywords: Clinical donor tissue grading, death to enucleation time, death to preservation time, eye bank specular microscopy, optimizing donor tissue utilization
Time and again, availability of enough number of quality donor tissues has been found lagging far behind the requirement to effectively combat corneal blindness. Making this problem worse is the widespread un-guided decision making for the available, relatively substantial pool of tissues. Eye Bank Specular Microscopy (EBSM) has not been made mandatory for Eye Bank licensing and currently many eye banks in India and other developing nations do not use EBSM for tissue analysis.
The purpose of the present study was to:
Objectively and accurately document how EBSM, with regard to the Age of the Donor, Death to Enucleation Time (DTET), Death to Preservation Time (DTPT) and Lens status of the Donor eye, will alter the final grading of donor cornea from the initial clinical grading and its subsequent utilization for various present day corneal transplant surgeries
Recommend on the basis of this outcome, whether it would be worth making EBSM evaluation of tissues mandatory in all eye banks globally.
Materials and Methods
From January 2010 to September 2011, 1067 donor eyes were received, processed and analyzed at the eye bank in our institute. Tissues without any of the following exclusion criteria were included in the study. The exclusion criteria were donors with systemic history not available, cause of death not known, blood sample not available, having history of transmissible diseases and positive serological test, tissues sent to other eye banks, tissues in which EBSM was not possible or with poor clinical grading where corneo-scleral button was not excised.
Two hundred eyeballs initially moist chamber preserved were prospectively assessed by Slit Lamp Bio-Microscopy (SLBM). Epithelial defects, exposure keratitis, arcus senilis, corneal scars, epithelial edema, stromal edema, stromal opacification, folds in Descemet's membrane (DM), quality of endothelium, condition of anterior chamber, iris and pupil and lens status were studied.[1] A clinical grade ranging from excellent to poor was assigned [Figs. 1–5].[1,2]
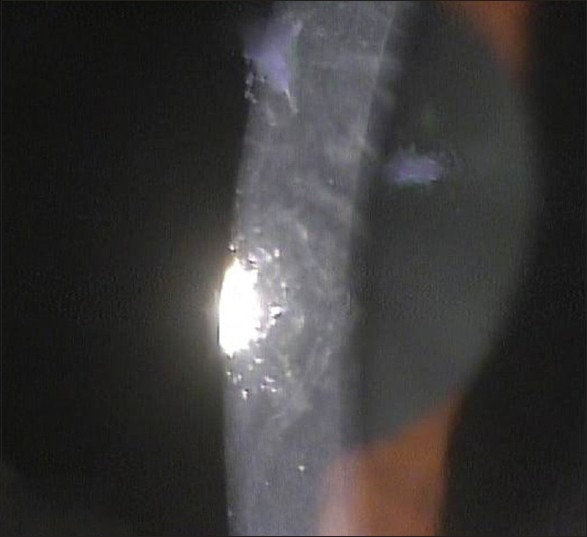
Figure 1.
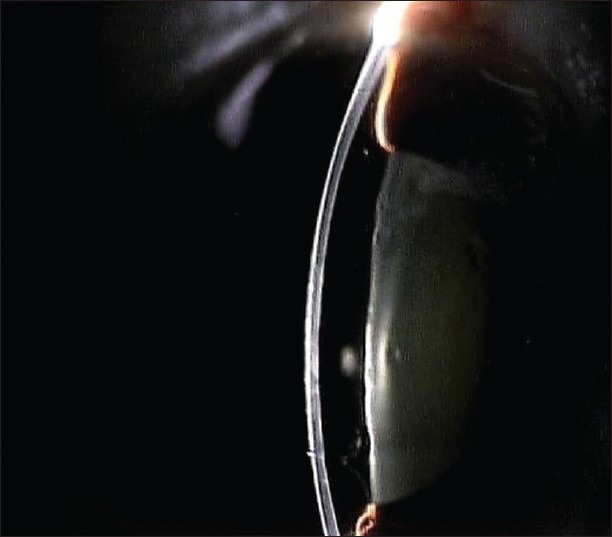
Excellent tissue with clear and compact stroma and no folds in Descemet's membrane
Figure 5.
Poor quality tissue with concave cornea and DM folds due to hypotony of eyeball
Figure 2.
Very good tissue with clear stroma, few faint DM folds
Figure 3.
Good tissue with stromal cloudiness and numerous but shallow DM folds
Figure 4.
Fair tissue with moderate epithelial haze, moderate stromal edema and heavy DM folds
With aseptic precautions, full thickness corneo-scleral button was excised from the eyeball which was preserved in McCarey-Kaufman (M-K) medium (Ramayamma International Eye Bank, LV Prasad Eye Institute, Hyderabad, India). The qualitative and quantitative endothelial cell analysis by Konan eye bank kerato analyzer (specular microscope) (Konan Medical Inc. Nishinomiya, Japan) was performed by an appropriately trained person. Center method was used for morphometric analysis.[3] On the basis of Mean CD and Standard Deviation of the mean cell area (SD), indicative of quantitative analysis, an adjusted grading was assigned to the tissue using the criteria in Table 1 [Figs. 6–9].[1,4] Cell morphology was understood by co-efficient of variation (CV) and percentage of hexagonal cells (6A).[3] As even in routine Indian patients corneas tend to be thinner and donor cornea with CD >2500 are not many,[4] as supply of tissues lags and as cut-offs are as such arbitrary, we had modified ranges of cell density as opposed to those in literature.[1] The final grading was altered accordingly as tissues having higher CD may still not have a good CV and 6A. Tissues with CV > 30% and 6A < 50% were not upgraded.[5] Also, tissues with good specular values in some area but with moderate to heavy DM folds were not upgraded.
Table 1.
Criteria for final grading of tissue post-EBSM
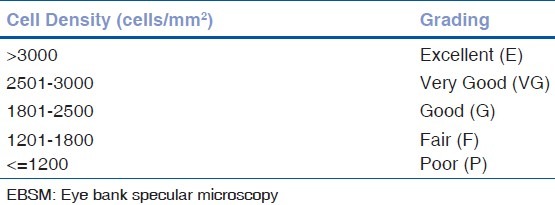
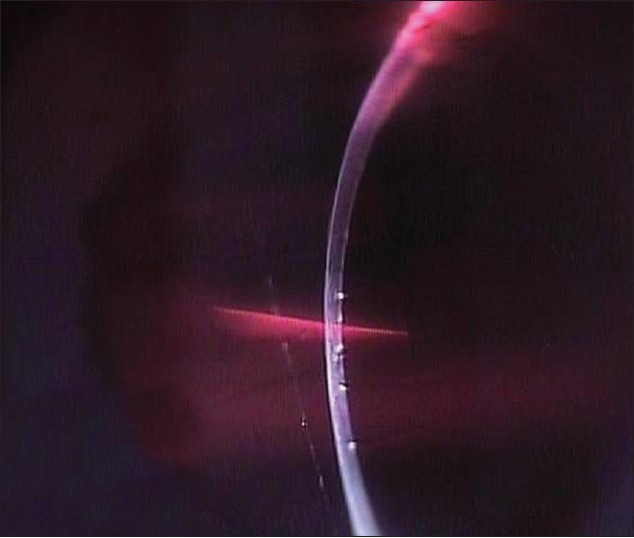
Figure 6.
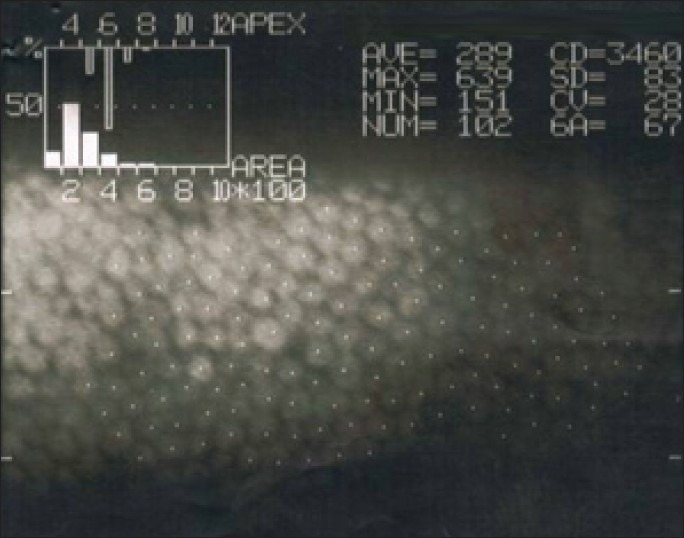
Excellent tissue with CD -3460 cells/mm2, CV 28% and 6A 67%
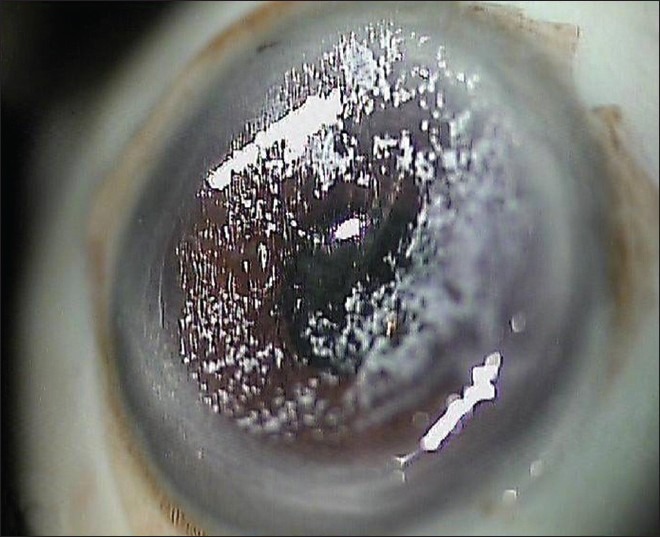
Figure 9.
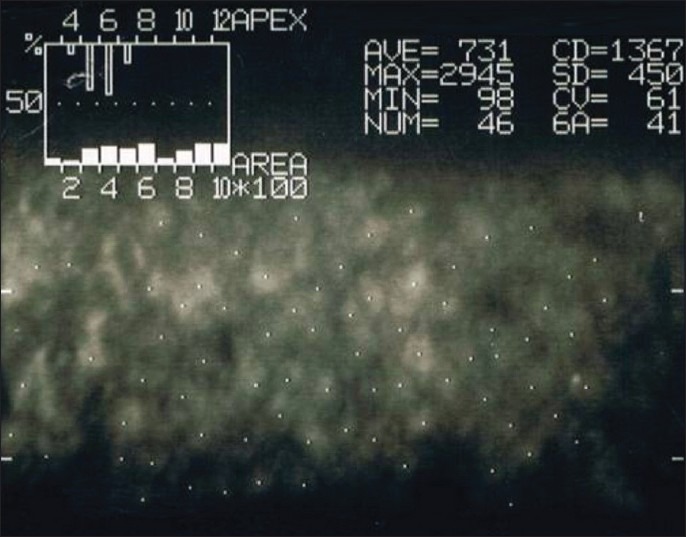
Fair tissue with CD -1367 cells/mm2, CV 61% and 6A 41%
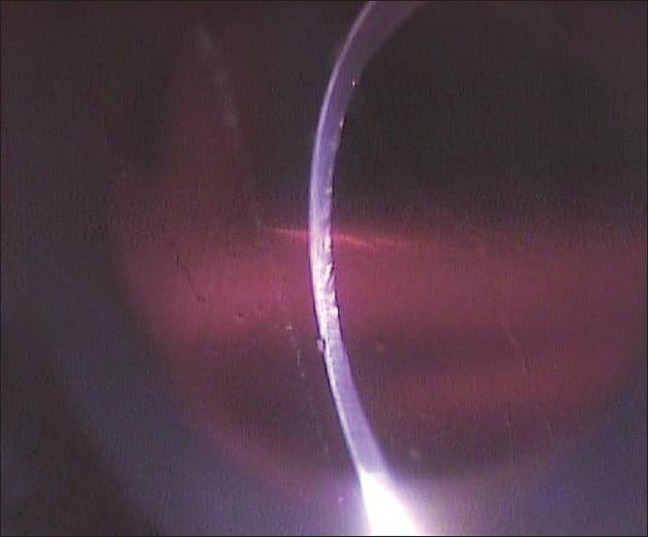
Figure 7.
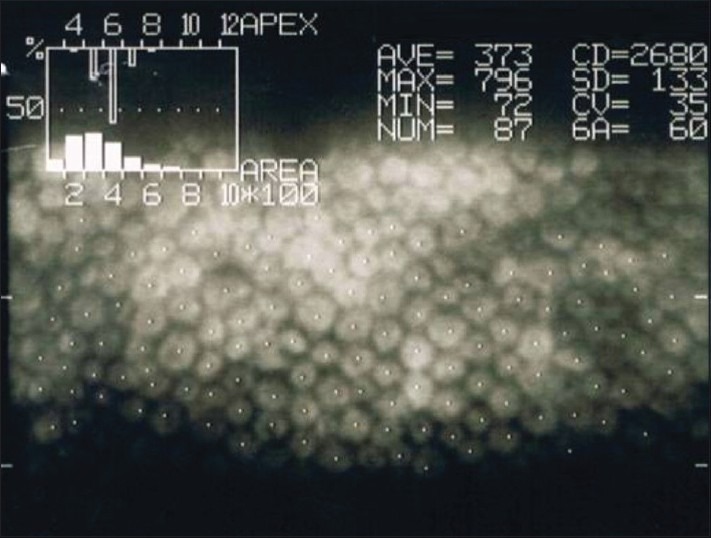
Very good tissue with CD -2680 cells/mm2, CV 35% and 6A 60%
Figure 8.
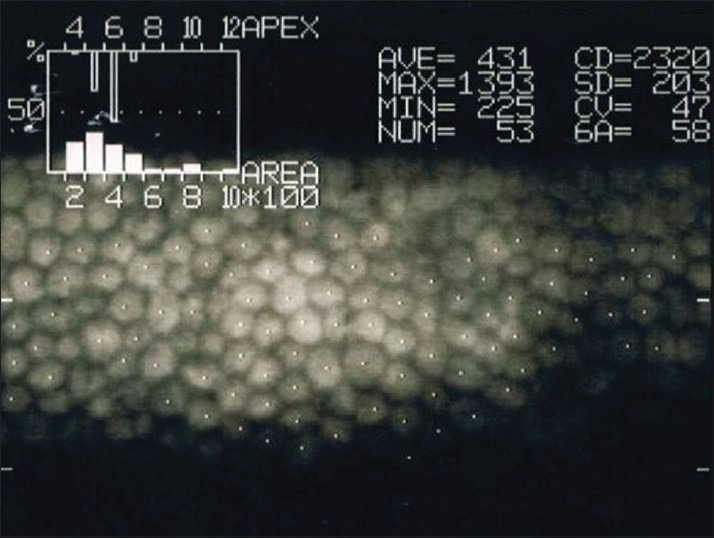
Good tissue with CD -2320 cells/mm2, CV 47% and 6A 58%
Final grading and subsequent utilization of tissues for various transplant surgeries was then analyzed with regard to the age of donor, DTET, DTPT and lens status of donor eye.
Results
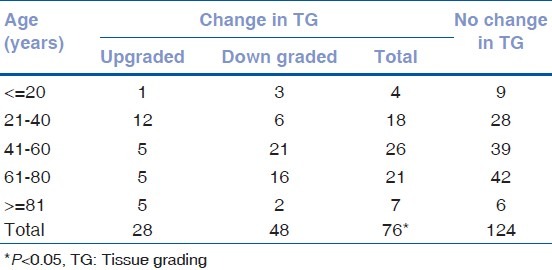
From the 200 eyes that were studied, 128 (64%) eyes belonged to donor age group 41-80 years demonstrating that the largest proportion of donors belonged to this age group [Table 2]. Out of 13 tissues with <=20 years of age, two (15.38%) tissues showed CD 1801-2500. Eight (61.54%) tissues had CV > 30% and two (15.36%) had 6A<=50% [Table 3]. Thus, even younger donor corneas may demonstrate a lower endothelial count with poor quality. Towards higher age groups, out of 63 eyes of 61-80 years of age, 16 (25.39%) eyes had CD 2501-3000 and only 12 (19.05%) eyes had CD 1201-1800. Out of 13 eyes from donor age >=81 years, two (15.39%) eyes had CD 2501-3000, one (7.69%) eye showed CD > 3000 and seven (53.85%) showed good morphology with 6A > 50%. Applying the modified criteria for grading, out of 200 eyes, there was statistically significant change in tissue grading in 76 (38%) eyes (P < 0.05) [Table 4]. 28 (36.84%) were upgraded and 48 (63.16%) were downgraded. Highest number of eyes [12 (26.09%)] were upgraded in the 21-40 years age group and out of them, one was used for Descemet's Stripping with Endothelial Keratoplasty (DSEK), two for Triple Surgery (PK with Cataract), seven for Optical Penetrating Keratoplasty (PKP) and only two for Therapeutic Penetrating Keratoplasty (TPK). Even in eyes with age 81 years or more, five (38.4%) tissues were upgraded with two tissues used for PKP and three for TPK and only two (15.3%) tissues were downgraded.
Table 2.
Endothelial CD and TG in different age groups
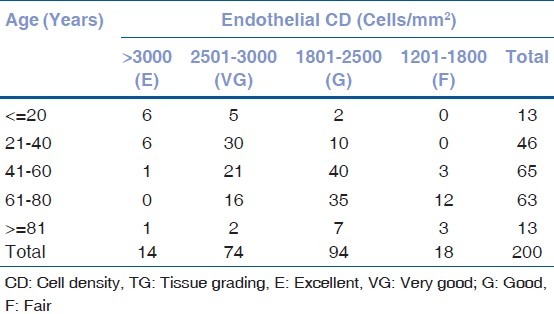
Table 3.
Endothelial cell morphology criteria in different age groups
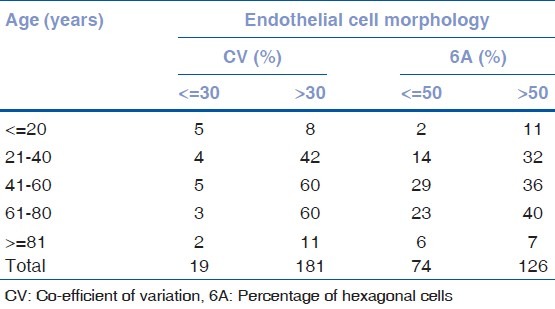
Table 4.
Change in final TG in different age groups
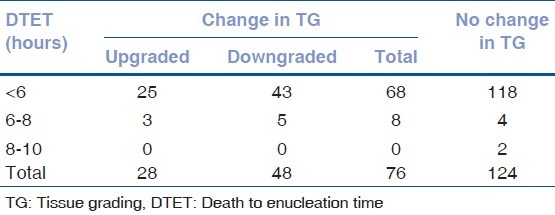
Out of 186 (93%) eyes enucleated as early as < 6 hours after death [Table 5], 85 (45.70%) tissues showed CD 1801-2500 and 23 (12.3%) tissues showed CD 1201-1800. From 12 (6%) eyes that were enucleated within 6-8 hours from death, none showed CD < 1800. Amongst this group, though nine of these tissues had CV > 30%, six tissues had good morphology with 6A > 50% [Table 6]. Out of these 12 tissues, three (25%) tissues were upgraded and five (41.68%) were downgraded [Table 7]. Out of three tissues that were upgraded, two were utilized for Triple surgery and one for Optical PKP. Thus, after performing EBSM and assessing endothelial cell morphology, some tissues which were obtained even at longer time after death (>6 hours) were found to remain good.
Table 5.
Endothelial CD and TG with different DTET
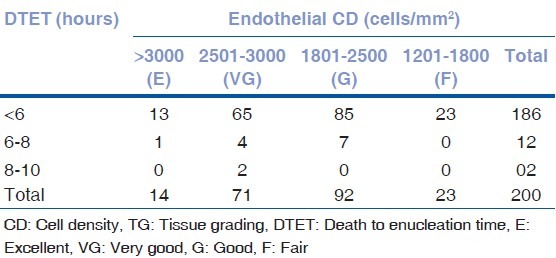
Table 6.
Endothelial cell morphology criteria with different DTET
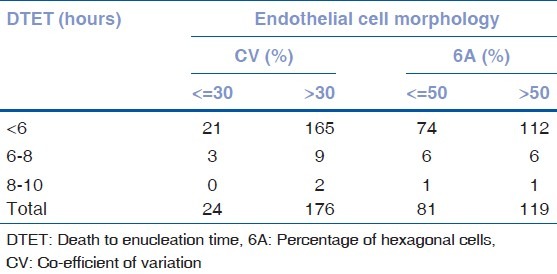
Table 7.
Change in final TG in relation to different DTET
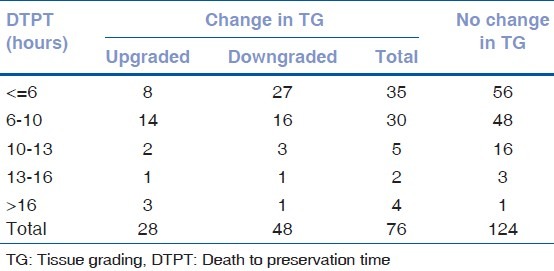
Out of 91 (45.5%) tissues with DTPT as short as <=6 hours [Table 8], 16 (17.58%) tissues showed CD 1201-1800. Out of 78 (39%) tissues with a longer DTPT of 7-10 hours, 31 (39.74%) showed CD > 2500. Out of five tissues with DTPT of 14-16 hours, all five tissues showed CD > 1800 and all tissues were used for Optical PKP. From the tissues with more than 16 hours of DTPT, two showed CD > 3000, one showed CD 2501-3000 while only two showed CD 1801-2500 and there was no tissue with CD < 1800. From this group, only one tissue was used for TPK and the rest were used for Optical PKP. Five tissues with DTPT of 7-10 hours and four tissues with DTPT > 16 hours had 6A > 50% [Table 9]. Significantly, three (60%) tissues with DTPT > 16 hours were upgraded [Table 10]. It shows that without the use of EBSM there may be wastage of reasonable pool of good quality tissues if they were utilized only on the basis of an assumption regarding DTPT and the clinical grading.
Table 8.
Endothelial CD and TG with different DTPT
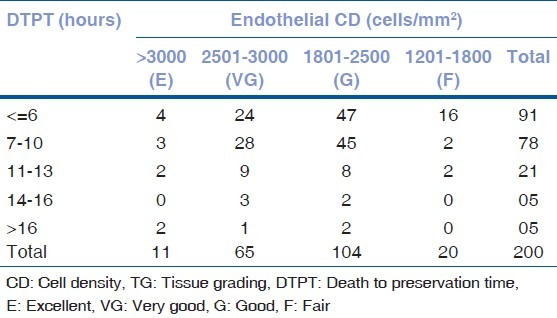
Table 9.
Endothelial cell morphology criteria with different DTPT
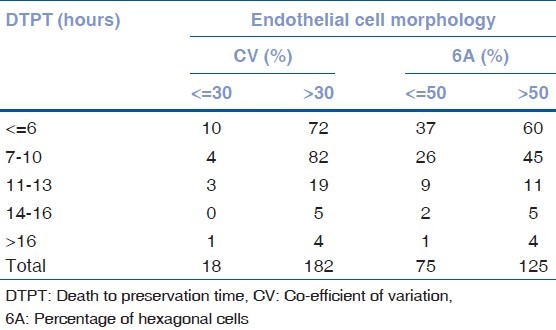
Table 10.
Change in final TG in relation to different DTPT
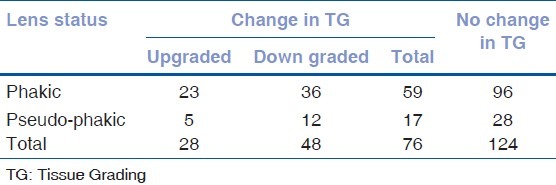
Out of 155 eyes in phakic group, 75 (48.39%) showed CD < 2500 [Table 11]. Out of 45 pseudo-phakic eyes, 32 (71.11%) showed CD > 1800 and only 13 (28.89%) showed CD 1201-1800. None of the pseudo-phakic eyes showed CD < 1200 which was noteworthy. Significantly, 24 (53.33%) tissues from this group were used for Optical PKP and 21 (46.67%) tissues were used for Therapeutic/Tectonic PKP (TePK). Significantly, 28 (62.22%) pseudo-phakic tissues showed a good morphology of 6A > 50% [Table 12]. Out of 76 eyes with change in tissue grading post EBSM, five (11.11%) pseudo-phakic eyes and 23 (14.84%) phakic eyes were upgraded and 12 (26.68%) pseudo-phakic eyes and 36 (23.27%) phakic eyes (three times the number of pseudo-phakic eyes) were downgraded [Table 13].
Table 11.
Endothelial CD and TG in relation to lens status
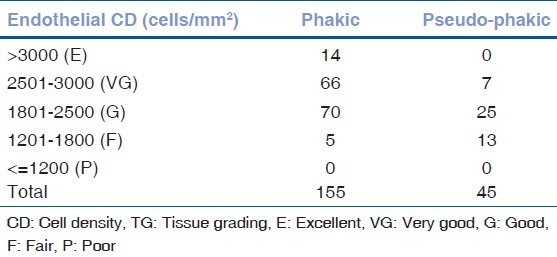
Table 12.
Endothelial cell morphology criteria in relation to Lens status
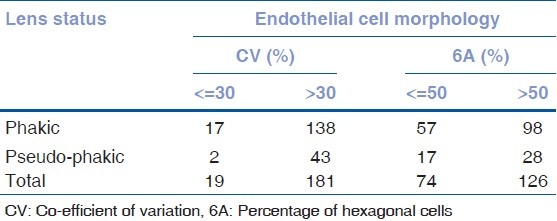
Table 13.
Change in final TG in relation to lens status of the donor
Thus, it can be seen that we can greatly and favorably influence the number of tissues which can be used for various transplant surgeries and make an objective and rationalized difference to the quality of donor tissues made available for transplantation by studying the endothelium of the donor tissue with the help of EBSM.
Discussion
Mattern et al.,[6] studied how frequently specular microscopy results affects the outcome of eye bank judgment as to the transplantability of donor corneas. For donors aged above 40, specular microscopy criteria was used to rule out unacceptable tissues. Corneas from donors more than 69 years were initially presumed to be unacceptable for transplant but routine specular microscopic examination helped to clear transplant of 31 of these. In our study, there were 65 tissues between 41-60 years, out of which only three (4.6%) showed CD 1201-1800. Out of them, one tissue with CD 1700 which was clinically graded as good had 6A-64% and CV-30% and could be utilized for PKP. Second tissue with CD 1742, CV-46% and 6A-36% clinically graded as very good was downgraded and utilized for Patch Graft. Third tissue with CD 1792 and clinically graded as very good had CV-50% and 6A-48% and was utilized for TePK. All tissues with CD 2501-3000 were used for Optical PKP. Five (7.6%) tissues showed upgrading from their clinical grade and out of these, three were used for Optical PKP and two were used for Triple surgery. Between 61-80 years, five (7.9%) tissues were up-graded. One was used for DSEK, three for Optical PKP and one for TePK. As in the study cited above from the West and as studied by Chuw et al.,[7] that large numbers of corneas from donors more than 65 years can be used successfully to restore vision by doing quantitative and qualitative assessment of cornea by specular microscopy, our study showed a similar finding for tissues from donors more than 60 years age. In addition, the age limit could be extended towards older age groups as five tissues from donors more than 80 years got upgraded post-EBSM.
Gain et al.,[8] studied the suitability of corneas from very old donors for graft after organ culture and their clinical and endothelial outcomes in recipients after PKP. No statistically significant difference was found in overall suitability for transplantation between two groups of donors with less than 85 years and more than 85 years, but elimination for low endothelial density was more frequent in donors with more than 85 years. In our study, EBSM was performed on tissues preserved in M-K medium. Contrasting with the above, seven (61.53%) tissues of age 81 years or more with CD 1801-2500 could be used for transplantation in relatively age matched patients. Three (23%) tissues had CD 1201-1800 but even they were fruitfully used for TPK or TePK, since in a country like ours, there are sizeable numbers of patients who require such surgeries.
Farias et al.,[9] had evaluated 203 corneas and showed that younger age donors had significantly better evaluation than older age donors. In our study, out of 59 tissues from younger age donors (<=40 years), 12 (20.30%) tissues showed CD 1801-2500 and out of 76 tissues from older age donors (>60 years), 19 (25%) tissues showed CD >=2500. In contrast to the study by Farias et al., we found that even younger age donors can have CD < 2500 and older age donors may show better values on evaluation. Only on the basis of SLBM (and at some places only on Torch-Light examination) and donor's age criteria, the tissues with higher age group have been considered by many eye banks as useful only for TPK and TePK. Significant number of such tissues which are not being subjected to EBSM may not be utilized for better prognosis transplantation due to lack of proper analysis. This shows that very meticulous application of quantitative and qualitative criteria of routine EBSM makes a difference to proper tissue utilization.
Due to longer (more than 6 hours) DTET general perception remains that the tissue may not remain good enough for optical or good prognosis transplantation and may be used for TPK or Patch graft. So, it has been debated whether to perform enucleation or defer it if DTET is more than 6 hours or any other such stipulated time. Grabska-Liberek et al.,[10] showed that overall rating of the tissues which were obtained in a very short time after death (up to 5 hours) was higher as compared with corneas removed 8-12 hours after donor's death. In our study, out of 200 eyes, 14 (7%) eyes were enucleated more than 6 hours after death. Out of 12 tissues with DTET between 6-8 hours, one (8.3%) tissue showed CD > 3000, CV-36% and 6A-55% and was used for Triple surgery, four tissues showed CD 2501-3000 and all were used for Optical PKP. Out of seven tissues which showed CD 1801-2500, six were used for Optical PKP and one with CD 1800, CV-45% and 6A-35% was used for TePK. There were two (1%) eyes with DTET between 8-10 hours and yet both of them showed CD > 2500. Out of these, one was used for Triple surgery and one for Optical PKP. Contrasting the study by Grabska-Liberek et al., from a developed country, we found that tissues enucleated more than 6 hours after death also had better grading and endothelial count, and could be used for Optical transplant surgeries, if only EBSM is done.
Due to longer DTPT, it is presumed that the tissue may not remain good enough for Optical PKP though the DTET was short (less than 6 hours). So, such tissues may get used for TPK or Patch Graft and may not be used for Optical PKP if not analyzed on EBSM. Cernak M[11] studied the vitality of the endothelium in relation to the DTPT. His study showed that corneas with more than ten hours of DTPT require longer time at room temperature to get rid of edema and on specular microscopic evaluation it was very difficult to find a group of endothelial cells for evaluation and such tissues are less suitable or are unsuitable for transplantation. Contrasting this, in our study, from the five (2.5%) tissues with DTPT of 14-16 hours, three (60%) showed CD 2501-3000, out of which two were used for DSEK and one was used for Triple surgery. Two tissues with CD 1801-2500 were used for Optical PKP. Also, there were five (2.5%) tissues with DTPT > 16 hours, out of which, one was used for DSEK, three for Triple surgery and only one was used for TPK. We had no difficulty in endothelial cell analysis by EBSM in tissues with longer DTPT and it could be performed at same interval as that of tissues with shorter DTPT.
It is believed that the tissues from pseudo-phakic eyes may not have good endothelial morphology and density and should not be used for optical transplantation. This is still in vogue in certain centers despite considerable refinement in cataract management techniques over the years. An advance in micro-surgical techniques like use of viscosurgical devices protects the endothelium. The advantage of such advances can be carried forward into the utility of tissues by performing EBSM. Whereby, even pseudo-phakic eyes can be found to have good cell quantity and quality and could be used for good prognosis transplantation. The lens status of the eye is not a genuine clue to the status of the endothelium and it therefore needs to be objectively evaluated for any decision making. Probst et al.,[12] studied the quality of donor corneal tissues in more than 75 years age group which showed that 17 of 35 phakic eyes in that age group were suitable for transplantation and none of the 15 pseudo-phakic eyes was found suitable for transplantation. In contrast, out of 45 pseudo-phakic tissues analyzed in our study, 25 (55.55%) tissues showed CD 1801-2500 out of which six were used for Optical PKP, seven for Triple, two for DSEK, five for TePK and five for TPK. Five tissues used for TPK showed CD < 1900 and poor cell morphology with numerous DM folds. Out of seven pseudo-phakic eyes with CD 2501-3000, three were used for Triple surgery and four for Optical PKP. Out of 13 pseudo-phakic eyes with CD 1201-1800, four were used for TePK, seven for TPK and two tissues with CV < 30% and 6A > 50% were used for Optical PKP.
Age of donor, DTET, DTPT and the phakic/pseudo-phakic status of donor eyes and the clinical grading, which have been often used by many numerically well performing Eye Banks, are ‘by themselves’ not good guides for decision making regarding the quality of tissues and its utilization. The impact on donor tissue grading and its benefit, on the basis of corneal endothelial cells (Specular Microscopy) is well acceptable as seen from the studies from developed countries. Despite the very clear importance of endothelial cells and the advantage of ‘specular microscopic technique’ for clinically judging the corneal endothelial status, there is apathy towards the complete application of EBSM and rationalizing the distribution of tissue for different indications of corneal transplant surgeries based on it. As seen in our study, very meticulous application of the quantitative and the qualitative criteria of the donor corneal endothelial cells as analyzed by EBSM leads to significant change in final grading of the tissues [38% (P < 0.05)]. 28 (36.8%) tissues - upgraded, 48 (63.1%) - downgraded. There was a related significant change in their subsequent utilization for the different present day corneal transplant surgeries.
Shortage of tissues suitable for surgery is a constant concern. This is much more relevant for developing countries. Supplies of quality donor corneas continue to lag behind the demand despite proposed Hospital Cornea Retrieval Program, proposed networking of Eye Banks and elevated motivational work. This shortage appears to be partly due to the custom in many centers to use tissues only from younger donors, tissues with very short DTET and DTPT, tissues with phakic status of eyes and those with excellent to good Torch Light/Bio-microscopic grading. In reality, there exists a sizeable pool of good quality tissues amongst the available tissues and with improved evaluation techniques, as seen in our study, it is possible to identify these tissues and to add them to the supply of available corneas. Our study is trying to focus on how to utilize more tissues from the available pool of tissues, thus optimizing utilization against discarding them for reasons which may not be indicative of their actual grade. Currently, in developing countries, though desirable, making available better criteria for matching of tissue (like HLA matching) for every donor-recipient match is beyond reach. Many Eye Banks are far from even the minimum scientific standards necessary for having reasonable Eye Bank practice. And while a better method is awaited for, the known advantages should be made available by making it mandatory for Eye Banks to have the facility of EBSM. Our study is clearly indicating that by performing EBSM, there can be a definite statistically significant positive influence in optimized utilization of tissues from the available pool.
The findings of our study can be extended to apply to advancement in EBSM technology whereby it would allow the evaluation even in poor grade tissues (currently not possible) and make them fruitfully useful for the evolved component corneal surgeries. For future betterment of the Eye Banking system, EBSM is indispensable as it would help Eye Banks communicate in the same specific objective terms and efficient networking of Eye Banks can thus be established. Thus for an Eye Bank, the EBSM by providing valuable quantitative and qualitative data becomes an indispensable tool for optimizing the availability of tissues for surgery and its availability should be made mandatory in all Eye Banks and it should be employed as frequently and in as many tissues as possible. Hope this works as an eye-opener and no Eye Banks are granted license without incorporation of availability of this mandatory analysis, especially in our subcontinent where demand always exceeds supply.
Acknowledgment
Meena N Pataniya (MS), Assistant Professor of Ophthalmology, Cornea and External Diseases Unit.
The team at DE Ankleshwaria Eye Bank, M and J Institute of Ophthalmology, Ahmedabad, India.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Doughman DJ. Corneal Tissue Preservation. In: Leibowitz HM, Waring GO, editors. Corneal disorders: Clinical Diagnosis and Management. 2nd ed. Philadelphia, PA: WB Saunders Co; 1998. pp. 871–909. [Google Scholar]
- 2.Saini JS, Reddy MK, Jain A, Ravindra MS, Jhaveria S, Raghuram L, et al. Perspectives in eye banking. Indian J Ophthalmol. 1996;44:47–55. [PubMed] [Google Scholar]
- 3.Benetz BA, Yee R, Bidros M, Lass J. Specular Microscopy. In: Krachmer JH, Mannis MJ, Holland EJ, editors. Cornea: Fundamentals, Diagnosis and Management. 3rd ed. St. Louis, MO: Mosby Elsevier; 2011. pp. 177–203. [Google Scholar]
- 4.Basak SK. Descemet stripping and endothelial keratoplasty in endothelial dysfunctions: Three-month results in 75 eyes. Indian J Ophthalmol. 2008;56:291–6. doi: 10.4103/0301-4738.41412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srinivasan M. Specular Microscopy. In: Dutta LC, editor. Modern Ophthalmology. 3rd ed. New Delhi, India: Jaypee Brothers; 2005. pp. 147–53. [Google Scholar]
- 6.Mattern RM, Heck EL, Cavanagh HD. The impact on tissue utilization of screening donor corneas by specular microscopy at the University of Texas Southwestern Medical center. Cornea. 1995;14:562–7. [PubMed] [Google Scholar]
- 7.Chu W, Dahl P, O’Neill MJ. Benefits of specular microscopy in evaluating eye donors aged 66 and older. Cornea. 1995;14:568–70. [PubMed] [Google Scholar]
- 8.Gain P, Rizzi P, Thuret G, Chiquet C, Michel-Valanconny C, Pugniet JL, et al. Corneal harvesting from donors over 85 years of age: Cornea outcome after banking and grafting. J Fr Ophtalmol. 2002;25:274–89. [PubMed] [Google Scholar]
- 9.Farias RJ, Kubokawa KM, Schirmer M, Sousa LB. Evaluation of corneal tissue by slit lamp and specular microscopy during the preservation period. Arq Bras Oftalmol. 2007;70:79–83. doi: 10.1590/s0004-27492007000100015. [DOI] [PubMed] [Google Scholar]
- 10.Grabska-Liberek I, Szaflik J, Brix-Warzecha M. The importance of various factors relating to the morphological quality of corneas used for PKP by the Warsaw Eye Bank from 1996 to 2002. Ann Transplant. 2003;8:26–31. [PubMed] [Google Scholar]
- 11.Cernak M. Evaluation of the quality of a donor cornea before transplantation. Cesk Slov Oftalmol. 2002;58:319, 323–5. [PubMed] [Google Scholar]
- 12.Probst LE, Halfaker BA, Holland EJ. Quality of corneal donor tissue in the greater-than-75-year age group. Cornea. 1997;16:507–11. [PubMed] [Google Scholar]


