Abstract
Objective:
Little is known about inpatient psychiatry settings and the services they provide for children and adolescents in Ontario. This paper provides the first broad description of unit characteristics, services provided, and patient characteristics in these settings.
Method:
Nominated representatives from Ontario hospitals with generic mental health beds (i.e., providing inpatient care across diagnostic groups) for children and adolescents were surveyed regarding data from April 2009 to March 2010. Response rate was 93%. Additional data were extracted from the Ontario Network of Child and Adolescent Inpatient Psychiatry Services (ONCAIPS) Directory and Ministry of Health and Long Term Care (MOHLTC) website.
Results:
Settings provided primarily crisis services with some planned elective admissions. Higher rates of involuntary admissions, briefer stays, lower interdisciplinary diversity, and lower occupancy were typical of settings with higher proportions of crisis admissions. Services most commonly provided included stabilization, assessment, pharmacotherapy, and mental health education. Bed numbers provincially, beds per staff, and prominence of suicide risk, mood disorders, and utilization of cognitive and behavioural approaches were comparable to trends internationally. Inter-setting disparities were observed in access to inpatient services for different age and diagnostic groups, and availability of psychiatry and different professions.
Conclusions:
Lack of consistent performance and outcome evaluation, common measures, availability of psychiatry and interdisciplinary supports, and dissimilar treatments provincially, suggest the need to consider potential improvements through systematic monitoring of setting performance and outcomes, and development of provincial best practice standards for staffing and treatment.
Keywords: psychiatric hospitalization, children, adolescents, benchmarking
Résumé
Objectif:
On sait très peu de choses des unités d’hospitalisation en psychiatrie et des services qu’elles prodiguent aux enfants et aux adolescents en Ontario. Cet article offre la première description générale des caractéristiques des unités, des services dispensés, et des caractéristiques des patients de ces unités.
Méthode:
Des représentants désignés des hôpitaux ontariens offrant des lits génériques de santé mentale, (c.-à-d., dispensant des soins aux patients hospitalisés de tous groupes diagnostiques) pour les enfants et les adolescents ont été interrogés sur les données d’avril 2009 à mars 2010. Le taux de réponse a été de 93%. Des données additionnelles ont été tirées du répertoire du Réseau d’unités de psychiatrie pour enfants et adolescents hospitalisés de l’Ontario (RUPEAHO) et du site Web du ministère de la Santé et des Soins de longue durée (MSSLD).
Résultats:
Les unités ont fourni des services principalement de crise et certaines hospitalisations non urgentes planifiées. Des taux plus élevés d’hospitalisations involontaires, de séjours abrégés, de diversité interdisciplinaire plus faible, et d’occupation plus faible étaient typiques des unités ayant des proportions plus élevées d’hospitalisations de crise. Les services les plus souvent dispensés étaient notamment la stabilisation, l’évaluation, la pharmacothérapie, et l’éducation en santé mentale. Le nombre des lits à l’échelle provinciale, les lits par employés, et la proéminence du risque de suicide, des troubles de l’humeur et le recours aux approches cognitives et comportementales étaient comparables aux tendances internationales. Des disparités ont été observées entre unités en ce qui concerne l’accès aux services d’hospitalisation pour différents groupes d’âge et diagnostiques, ainsi que la disponibilité de la psychiatrie et de différentes professions.
Conclusions:
L’absence de rendement constant et d’évaluation des résultats, les mesures communes, la disponibilité de la psychiatrie et de soutiens interdisciplinaires, et les traitements différents dans la province indiquent le besoin de songer à des améliorations possibles par la surveillance systématique du rendement et des résultats des unités, et par l’élaboration de normes de pratiques provinciales exemplaires en matière de dotation en personnel et de traitement.
Keywords: hospitalisation psychiatrique, enfants, adolescents, analyse comparative
Introduction
Child and adolescent inpatient psychiatry settings provide safety and care for youth with the most severe and complex mental health problems. In view of their importance, high costs, and widespread use, it is surprising how little is known about most aspects of inpatient care in Ontario and elsewhere (Barwick & Boydell, 2005). The present paper provides the first broad description of the state of Ontario’s settings to help reduce this information gap.
Improved descriptions of services are important and timely in view of growing pressures from communities and emergency departments for admissions (Blader, 2011) and counter-pressures for bed reductions in favour of non-hospital alternatives (Barwick & Boydell, 2005). Inpatient proponents point to rapid, lasting improvements (Green et al., 2007) and high rates of satisfaction (Marriage, Petrie, & Worling, 2001). Others counter that similar outcomes and greater satisfaction are attainable through less expensive and intrusive community programs (Barwick & Boydell, 2005). But, until community programs better respond to pressures and prevent admissions, it is unlikely that inpatient settings will be displaced from their current prominent role within the mental health system (Blader, 2011).
In November 2006, the Ontario Centre of Excellence for Child and Youth Mental Health, recognizing the continuing importance of inpatient care, provided funding for the first meeting of child and adolescent inpatient psychiatry settings. Meeting participants formed the Ontario Network of Child and Adolescent Inpatient Psychiatry Services (ONCAIPS) for generic settings that admit across diagnostic groups. Network members committed to knowledge exchange and collaborative study of settings and services, and compiled the first provincial Directory of all settings in Ontario which is continually updated. Settings admitting single diagnostic groups such as eating disorders, infants (where the focus is on maternal mental health), families, and day treatment and non-hospital-based residential care settings were not included and are outside of the scope of the present study.
Internationally, generic inpatient settings that admit across diagnostic groups are linked by:
similar mental health legislation that permits involuntary admissions; and,
common practices including diagnosis following ICD (World Health Organization, 1992) or DSM criteria (American Psychiatric Association, 2000) and pharmacotherapy for stabilization and treatment (Dean, Scott, & McDermott, 2009; Warner, Fontanella, & Pottick, 2007).
All such settings also provide psychosocial interventions. These can involve non-specific “milieu therapy” (Delaney, 1997), family interventions, classroom-based education, and complete courses of evidence-supported therapy for specific problems such as behaviour therapy for aggression (Dean, Duke, George, & Scott, 2007), Dialectical Behavior Therapy for suicidal adolescents (Katz, Cox, Gunasekara, & Miller, 2004), and cognitive behavioural interventions for school refusal (Walter et al., 2010).
Accessibility, or the availability across the province of similar types and quality of inpatient care, setting characteristics, and services provided have not been described provincially. The goal of the present study is to provide an initial description of the state of Ontario’s settings and services with the intent of moving towards the establishment of a more permanent provincial information-base to facilitate cross-setting comparisons, and development of inpatient benchmarks and standards.
Method
Status as a Schedule 1 psychiatric facility under the Mental Health Act (i.e., a facility that is required to provide inpatient services where an individual can be detained or admitted involuntarily) and information about Ontario’s 14 Local Health Integration Networks (LHINs), which are jurisdictions responsible for planning and implementation of health care services in Ontario, were extracted in April 2010 from the Ministry of Health and Long Term Care (MOHLTC) website. Population per LHIN district was calculated from the 2006 census data available through Statistics Canada. Settings, number of beds, and age and exclusion criteria were extracted from the ONCAIPS (2010) Directory.
All 27 settings operating designated generic mental health beds for children and youth under age 18 in Ontario hospitals during April 1, 2009 to March 31, 2010 served as subjects. Surveys and SurveyMonkey links were e-mailed to each unit’s ONCAIPS representative (i.e., manager, director, or outcomes lead) in November 2010 asking for data collected for the preceding fiscal year. Settings were emailed reminders and contacted by telephone for completion and data verification when required. Twenty-five settings responded for a response rate of 93%.
Setting interdisciplinary diversity (e.g., O’Herlihy et al., 2001), was defined as the number of different disciplines from among: psychiatry, nursing (RN, RPNs, and nurse practitioners), child and youth counselling (typically as front-line staff providing daily programming in collaboration with nursing), social work, psychology (psychologists and psychological associates), teaching, occupational therapy, recreation therapy, pharmacy, pastoral counselling, physiotherapy, and speech/language pathology.
Number of responses is indicated per item where the response rate was less than 100%. Data were analysed using SPSS Version 19. Descriptive data and percentages were the principal modes of data presentation. Non-parametric tests and exact statistics were utilized as appropriate.
Results
There were 183 beds across 27 settings according to Directory data (see Table 1 for characteristics of inpatient settings). Calculations utilizing census information indicated a prevalence of 5.9 beds per 100,000 youth under age 19. Beds by LHIN district varied from none to 15 per 100,000. Of the two districts without designated mental health beds that were within a hospital setting, one admitted children and adolescents to an out-of-hospital setting and the other utilized the inpatient setting of a nearby LHIN. According to the MOHLTC (2010) website, 26 of the 27 settings were Schedule 1 facilities capable of admitting involuntary patients. Eight settings excluded youth presenting with one or more of the following: developmental disability; forensic problems; eating disorders; substance abuse; conduct; and, pervasive developmental disorders. Directory data indicated that 18 of the 27 settings admitted children and adolescents, eight admitted adolescents, and one admitted children. Although youth typically are transitioned to adult services at age 18, directory data indicated that several in-patient settings serve youth up to age 19 or 20.
Table 1.
Characteristics of the “typical” inpatient setting in Ontario: April 1, 2009-March 31, 2010
| Characteristic per setting | Median | Range | na |
|---|---|---|---|
| Number of beds | 7 | 2 – 15 | 27b |
| Yearly admissionsc | 200 | 14 – 396 | 19 |
| Yearly admissions per bed | 23 | 2 – 50 | 19 |
| Crisis admissions (percent of total)d | 90% | 0 – 100% | 24 |
| Involuntary admissions | |||
| Form 1 (percent of total) | 40% | 0 – 80% | 21 |
| Form 3 (percent of total) | 5% | 0 – 40% | 15 |
| Length of stay in days | 22 | 2 – 137 | 20 |
| Annual occupancy (percent) | 73% | 38 – 106% | 20 |
| Alternate level of care (percent)e | 1% | 0 – 27% | 22 |
| Number of different disciplines | 6 | 3 – 11 | 25 |
| Average beds per nurse/CYC per shift | |||
| Day | 2.6 | 0.88 – 5 | 20 |
| Evening | 2.9 | 1 – 10 | 19 |
| Night | 4.1 | 1 – 10 | 18 |
Represents the total number of inpatient units responding to the survey item.
ONCAIPS Directory (not survey) data were utilized for this item, therefore n = 27 not 25.
An admission refers to all formal hospital admissions to a designated mental health bed.
A crisis admission refers to an unplanned emergent admission (as opposed to a planned elective admission).
Alternate level of care refers to patients awaiting transfer who no longer require the level of intensity of services provided by the current acute hospital setting.
Adolescents aged 14 and over (Mdn=81%) were significantly more likely to be admitted than children aged 13 and under (Mdn=19%), (Wilcoxon signed-ranks=122, n=16, z=2.80, df=1, p < .05, r = .70). For children, there was a higher percentage of male (Mdn=56%) relative to female (Mdn = 44%) admissions across settings; however, this difference did not reach statistical significance. Conversely, for adolescents, the percentage of female (Mdn = 59%) relative to male (Mdn = 41%) admissions across settings was higher but did not reach statistical significance. Six settings also reported small rates of admission for individuals aged 18 or over.
Admissions were significantly more likely to be unplanned crisis than planned elective (Wilcoxon signed-ranks = 40, n=24, z=−2.99, df=1, p < .05, r = .61). Two settings reported admitting solely crisis; one, solely elective; and the remaining 21 admitting both. Rates of involuntary detention for psychiatric assessment (i.e., Form 1) or of involuntary admission for treatment (i.e., Form 3) accounted for nearly half of all admissions on average (see Table 1). Accordingly, respondents (n = 22) identified suicide risk as the most prevalent problem precipitating admission. Higher proportion of crisis admissions predicted greater numbers of Form 1 detentions, (Spearman Rho = .54, p < .05, n=20), lower average length of stay (LOS) (Spearman Rho =− .54, p < .05, n=22), lower occupancy (Spearman Rho = −.55, p < .05, n=19), and lower interdisciplinary diversity (Spearman Rho = −.52, p < .05, n=19).
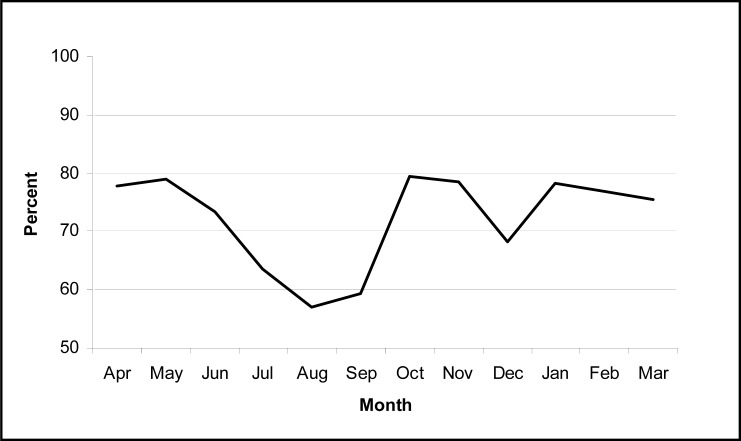
Median monthly occupancies (n=17) indicated peaks in the spring and fall and valleys in the summer and mid-winter (see Figure 1). Front-line staff in higher occupancy settings were responsible for fewer beds per day (Spearman Rho = −.67, p < .05, n=16), evening (Spearman Rho = −.49, p < .05, n=15), and night shifts (Spearman Rho = −.62, p < .05, n=14).
Figure 1.
Percent of total child and adolescent inpatient psychiatry beds that were occupied per month averaged across settings for the fiscal year April 1, 2009 to March 31 2010.
Interdisciplinary diversity was significantly associated with longer stay (Spearman Rho = .66, p < .05, n=22) and more beds (Spearman Rho = .46, p < .05, n=25). Nurses were the most prevalent group seeing all patients in 96% of settings (n=25), followed by child and youth counsellors (CYCs) in 86% of settings. Social workers and teachers were represented in a majority of settings and psychological service providers and occupational therapists in about half. Other disciplines were less frequent. Although 88% of settings employed full-time psychiatrists, one setting retained a psychiatrist who saw only some patients. Two had no psychiatrist, with this role being filled by paediatricians with off-site consultative psychiatric support. Median responsibility per psychiatrist was six beds (range 2–20, n=25). Front-line staff on larger units were responsible for more beds across day (Spearman Rho = .81, p < .05, n=20), evening (Spearman Rho = .71, p < .05, n=19) and night shifts (Spearman Rho = .71, p < .05, n=18).
Median percentages for primary discharge diagnoses (n=20) were: mood (39.4%); adjustment (13.8%); anxiety (7.5%); behaviour (6.5%); psychosis (5.4%); substance abuse (2.8%); and, ADHD (2.2%). Others disorders were infrequent. Mood, anxiety, and psychosis were the only diagnoses represented across all settings. Shortest LOS were for adjustment (Mdn=5.3, n=16) and behaviour disorders (Mdn=6.4, n=8); longest LOS were for developmental delay/intellectual disability (Mdn=17.8, n=8), psychosis (Mdn=17.7, n=16), and eating disorders (Mdn=17.5, n=11). DSM-IV guidelines (60%) were in slightly more common use than ICD-10 (45%), with a number of settings utilizing both.
All settings reported providing stabilization, family assessments, diagnosis, and mental health education. All settings, with one exception, provided risk assessment and pharmacology. About half provided psychoeducational assessment for school purposes some of the time. The psychosocial therapy (n=25) in most frequent use was cognitive behavioural (88%), followed by solution focused (76%), interpersonal (60%), and dialectical behaviour (44%), and to a lesser extent behaviour, occupational, and recreation therapies. No setting utilized psychoanalytic approaches.
Although a number of settings reported symptom-specific measures of change for certain patients, less than half reported measuring outcomes (e.g., pre- and post- comparisons) routinely for every patient. Symptom change was the outcome most frequently measured (46% of settings), followed by risk reduction (33%), stabilization (29%) and functional improvement (25%). Specific measures in more common use were the Childhood Acuity of Psychiatric Illness scale (Lyons, 1998), the Child and Adolescent Needs and Strengths – Mental Health (Lyons, Sokol, & Lee, 1999) and global functioning scales.
Discussion
Findings indicate that child and adolescent inpatient psychiatry settings in Ontario generally resemble settings internationally in terms of numbers of beds per population, size of settings, prominence of suicide risk and mood disorders, services such as diagnosis and pharmacotherapy, and utilization of cognitive and behavioural approaches (Ellilä, 2007; O’Herlihy et al., 2001). Like other descriptive studies internationally, Ontario’s survey also revealed concerning inter-setting disparities in access for different age and diagnostic groups, availability of psychiatry and different professions, and many aspects of service provision. If one of the goals of the system of care is to provide children and adolescents in the province with similar access to inpatient care and high service quality, the survey results suggest that this is yet to be well realized provincially. Access to beds differed significantly across the province and certain diagnostic groups were found to be able to access inpatient care in some geographic areas but not others. There was significant lack of access to psychiatry, inequity in availability of interdisciplinary supports, inconsistency in types of treatments provided, and insufficient tracking of outcomes across settings.
A majority of settings identified suicide risk as the most prevalent precipitant of admissions, consistent with findings and beliefs that inpatient units should be heavily involved in suicide risk management (Hanssen-Bauer et al., 2011). Although suicide prevention is clearly important, the extent to which inpatient units provide reassuring safety for concerned communities, as opposed to contributing to long term prevention of suicide, remains to be studied.
Prevalence of child admissions was found to be small in Ontario, similar to the United States, and smaller than Europe (Case, Olfson, Marcus, & Stegel, 2007; Ellilä, 2007). However, should there be increasing demands to admit children, as trends in the United States suggest (Case et al., 2007), it will become increasingly important to consider separate child and adolescent settings given the differing safety and social requirements of the two groups.
The Ontario blend of primarily crisis admissions with a small proportion of elective admissions for treatment falls between the very brief crisis focus, more common in the United States (Blader, 2011), and the longer planned treatment stays more typical of Europe (O’Herlihy et al., 2001). The findings support the view that both crisis and longer term inpatient treatments are important in Ontario. The crisis versus elective focus of units, however, impresses as locally determined rather than provincially planned. Settings with a greater proportion of crisis admissions had briefer LOS, more frequent involuntary detention for assessment, less diverse interdisciplinary staff, and lower occupancy. This is not an unexpected pattern given the large back up role inpatient units provide for emergency care settings, the emphasis upon rapid discharge to interdisciplinary community follow-up, and the waxing and waning of emergency care pressures.
About one in two admissions in Ontario is involuntary, which is significantly higher than rates in Finland (Kaltiala-Heino, 2004), the United Kingdom (Mears et al., 2003), and Norway (Hanssen-Bauer et al., 2011). The finding that involuntary detentions tend to be brief suggests the possibility that there may be significant numbers of youth misidentified or at low transient risk. If more timely access to psychiatric assessment and mental health programs were available to communities, emergency departments, initial crisis responders, parents and schools, it is possible that the use of involuntary admissions and admissions in general could be significantly reduced (Smith, 2004).
Findings that mood, anxiety, and psychosis were the only diagnoses present across all generic settings may reflect not only the prevalence of such disorders, but also beliefs about appropriateness of such diagnoses for inpatient care. Youth with mood disorders were the most common group admitted in Ontario, which is consistent with findings internationally (Case et al., 2007; O’Herlihy et al., 2001). Inter-setting variability in diagnoses has been noted in numerous studies and may be resulting from a number of factors including cross-setting inconsistencies in diagnostic practice and selective exclusion of certain diagnoses (e.g., Leon, Lyons, & Uziel-Miller, 2000). The present study found that certain diagnoses such as eating disorders and developmental disabilities are routinely excluded from certain settings in Ontario but not others, which affects the consistency of diagnoses reported across units.
The present findings noted a range in setting sizes from two to 15 beds. Small settings with few beds have certain significant disadvantages such as difficulty providing numbers-dependent patient activities (e.g., group work, classroom) and interdisciplinary care. Smaller settings, as the present study notes, also employ more staff per bed. On the other hand it could be argued that more staff per bed translates into more staff time per patient, thereby improving care. Smaller bed units can also be more easily dispersed to general hospitals “closer to home” than a single large centralized setting, thereby reducing travel time and improving access for many families.
Almost all inpatient settings were found to provide pharmacotherapy and psychosocial therapy. The most prevalent psychosocial therapies reported are cognitive behavioural, followed by solution focused, systemic, and interpersonal. This is consistent with international trends indicating movement away from psychoanalysis and towards cognitive and behavioural approaches (Ellilä, 2007; O’Herlihy et al., 2001). Although therapies reported by Ontario settings impress as evidence-based, it is not clear whether settings utilize protocols for pharmacotherapy and cognitive behavioural therapy, or approaches that are informed by the literature but not protocol-driven. As evidence-based interventions depend upon protocols and outcome measurement it is concerning that less than half of the settings surveyed reported evaluating outcomes in a systematic manner.
Findings support the view that Ontario inpatient units are committed to interdisciplinary staffing, which is a common expectation internationally (e.g., Bacon, Thompson, & Solomon, 2009). Additionally, there are indications of commitments to adjustments in front-line workload as reflected by more staff per bed allocations for higher occupancy settings. The prominence of nurses and CYCs seems to reflect a belief in the importance of balancing medical and behavioural management needs. It was, however, concerning that several inpatient psychiatry settings did not employ psychiatrists as full time members of the core interdisciplinary team, and that full time psychiatrists in some settings were responsible for ten times as many beds as those in others. There was also significant cross-setting variability in interdisciplinary capacity. Given the findings that interdisciplinary diversity is higher for planned elective care than crisis, it may be important to further explore differences between these two settings in terms of their staffing needs.
High response rate, convergence of findings among information sources, and consistency with many findings internationally provides an acceptable level of confidence about what the results say about the state of child and adolescent psychiatric inpatient care in Ontario. However, the present study has noteworthy limitations which need to be acknowledged and better addressed in future studies. Limitations include small sample size, lack of experimental control (making causal interpretation difficult), and reliance upon retrospective reports of data that may not have been collected by settings in the same way. A few settings provided no data at all, and others incomplete data. The lack of provincial definitions for terms such as readmission rates and therapy further affected reliability.
The study provides reassuring information at the same time as it raises a number of additional questions. Findings suggesting seasonal differences in admission rates corresponding to school and other seasonal stresses have been found before (Hawton et al., 2003) and could have important implications for resourcing and prevention if verified by future studies. Future studies will also need to not only address the shortcomings in the present study, but also broaden the survey to include information about the origin of referrals, use of restraints and seclusion, medications in use, and post-discharge services. ONCAIPS will also need to review whether to include specialized settings for eating disorders, substance abuse, and forensics in its membership and surveys in order to provide a more complete picture of provincial inpatient psychiatric care.
Despite shortcomings, the present study nevertheless provides an important first broad-based description of the state of Ontario’s child and adolescent inpatient psychiatry services. Lack of access to beds in some geographic districts is concerning as insufficient access may result in extended stays in emergency settings and out-of-district services. Standards for inpatient care with ongoing monitoring may be required to improve access, service quality, and staffing consistency. It is the hope of the ONCAIPS membership that future surveys will continue the benchmarking collaboration and promote development of common standards and benchmarks. Such initiatives will help to improve service quality and outcomes, and help assure that all children and adolescents are able to access the most effective mental health care possible.
Acknowledgements/Conflicts of Interest
The authors thank the membership and steering committee of ONCAIPS for their participation and support. The authors are employed in inpatient settings and serve on the steering committee of ONCAIPS. Points of view presented may have been influenced by their professional experiences with inpatient care and loyalties to these settings. No external funding was received for this study.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 2000. [Google Scholar]
- Bacon S, Thompson P, Solomon J. Service Standards. 5th ed. London, UK: Inpatient CAMHS Royal College of Psychiatrists’ Centre for Quality Improvement London; 2009. [Google Scholar]
- Barwick M, Boydell K. A review of acute child and adolescent mental health services. Toronto, ON: Ministry of Children and Youth Services; 2005. [Google Scholar]
- Blader J. Acute inpatient care for psychiatric disorders in the Unites States 1996 to 2007. Archives of General Psychiatry. 2011;68:1276–1283. doi: 10.1001/archgenpsychiatry.2011.84. [DOI] [PubMed] [Google Scholar]
- Case B, Olfson M, Marcus S, Stegel C. Trends in the inpatient mental health treatment of children and adolescents in US community hospitals between 1990 and 2000. Archives of General Psychiatry. 2007;64:89–96. doi: 10.1001/archpsyc.64.1.89. [DOI] [PubMed] [Google Scholar]
- Dean AJ, Duke SG, George M, Scott J. Behavioral management leads to reduction in aggression on a child and adolescent inpatient unit. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:711–720. doi: 10.1097/chi.0b013e3180465a1a. [DOI] [PubMed] [Google Scholar]
- Dean AJ, Scott J, McDermott BM. Changing utilization of pro re nata (‘as needed’) sedation in a child and adolescent psychiatric inpatient unit. Australian and New Zealand Journal of Psychiatry. 2009;43:360–365. doi: 10.1080/00048670902721095. [DOI] [PubMed] [Google Scholar]
- Delaney KR. Milieu therapy: A therapeutic loophole. Perspectives in Psychiatric Care. 1997;33:19–28. doi: 10.1111/j.1744-6163.1997.tb00537.x. [DOI] [PubMed] [Google Scholar]
- Ellilä H. Child and adolescent psychiatric inpatient care in Finland. From the Department of Child Psychiatry and Department of Nursing Science, University of Turku; Turku, Finland: 2007. [Google Scholar]
- Green J, Jacobs B, Beecham J, Dunn G, Kroll L, Tobias C, Briskman J. Inpatient treatment in child and adolescent psychiatry – a prospective study of health gain and costs. Journal of Child Psychology and Psychiatry. 2007;48:1259–1267. doi: 10.1111/j.1469-7610.2007.01802.x. [DOI] [PubMed] [Google Scholar]
- Hanssen-Bauer K, Heyerdahl S, Hatling T, Jensen G, Olstad PM, Stangeland T, Tinderholt T. Admissions to acute adolescent psychiatric units: A prospective study of clinical severity and outcome. International Journal of Mental Health Systems. 2011;5:1–11. doi: 10.1186/1752-4458-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawton K, Hall S, Sinkin S, Bale L, Bond Al, Codd S, Stewart A. Deliberate self-harm in adolescents: A study of characteristics and trends in Oxford, 1990–2000. Journal of Child Psychology and Psychiatry. 2003;44:1191–1198. doi: 10.1111/1469-7610.00200. [DOI] [PubMed] [Google Scholar]
- Kaltiala-Heino R. Increase in involuntary psychiatric admissions of minors. Social Psychiatry & Psychiatric Epidemiology. 2004;39:53–59. doi: 10.1007/s00127-004-0694-z. [DOI] [PubMed] [Google Scholar]
- Katz L, Cox B, Gunasekara S, Miller A. Feasibility of Dialectical Behavior Therapy for suicidal adolescent inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:276–282. doi: 10.1097/00004583-200403000-00008. [DOI] [PubMed] [Google Scholar]
- Leon SC, Lyons JS, Uziel-Miller ND. Variations in clinical presentations of children and adolescents at eight psychiatric hospitals. Psychiatric Services. 2000;51:786–790. doi: 10.1176/appi.ps.51.6.786. [DOI] [PubMed] [Google Scholar]
- Lyons JS. The Severity and Acuity of Psychiatric Illness scales: An outcome management and decision-support system. Child and adolescent version. Manual. San Antonio, TX: Psychological Corporation; 1998. [Google Scholar]
- Lyons JS, Sokol P, Lee M. The Child and Adolescent Needs and Strengths for Children and Adolescents with Mental Health Challenges (CANS-MH) manual. Winnetka, IL: Budding Praed Foundation; 1999. [Google Scholar]
- Marriage K, Petrie J, Worling D. Consumer satisfaction with an adolescent inpatient psychiatric unit. Canadian Journal of Psychiatry. 2001;46:969–975. doi: 10.1177/070674370104601011. [DOI] [PubMed] [Google Scholar]
- Mears A, White R, O’Herlihy A, Worrall A, Banerjee S, Jaffa T, Hill P, Lelliott P. Characteristics of the detained and informal child and adolescent psychiatric in-patient populations. Child and Adolescent Mental Health. 2003;8:131–134. doi: 10.1111/1475-3588.00059. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Long Term Care 2010. May 1, 2010. Downloaded. from http://www.health.gov.on.ca/english/public/contact/psych/designated.html.
- O’Herlihy A, Worrall A, Banerjee S, Jaffa T, Hill P, Mears A, Lelliott P. National In-patient Child and Adolescent Psychiatry Study. Final Report to the Department of Health. London: Royal College of Psychiatrists’ Research Unit; 2001. [Google Scholar]
- Smith WG. Young people admitted to a general hospital: A worrisome trend. Paediatric Child Health. 2004;9:228–233. doi: 10.1093/pch/9.4.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter D, Hautmann C, Rizk S, Petermann M, Minkus J, Sinzig J, Doepfner M. Short term effects of inpatient cognitive behavioral treatment of adolescents with anxious-depressed school absenteeism: An observational study. European Child & Adolescent Psychiatry. 2010;19:835–844. doi: 10.1007/s00787-010-0133-5. [DOI] [PubMed] [Google Scholar]
- Warner LA, Fontanella CA, Pottick KJ. Initiation and change of psychotropic medication change among adolescents in inpatient care. Journal of Child and Adolescent Psychopharmacology. 2007;17:701–712. doi: 10.1089/cap.2007.0120. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines (ICD-10) Geneva: World Health Organization; 1992. [Google Scholar]