Abstract
Background
Autism spectrum disorders (ASDs) are increasing in prevalence. Children with ASDs present with impairments in social interactions; communication; restricted, repetitive, and stereotyped patterns of behavior, interests, or activities; as well as motor delays. Hydrotherapy is used as a treatment for children with disabilities and motor delays. There have been no systematic reviews conducted on the effectiveness of hydrotherapy in children with ASDs.
Aim
We aimed to examine the effectiveness of hydrotherapy on social interactions and behaviors in the treatment of children with ASDs.
Methods
A systematic search of Cochrane, CINAHL, PsycINFO, Embase, MEDLINE®, and Academic Search Premier was conducted. Studies of participants, aged 3–18 years, with ASDs at a high-functioning level were included if they utilized outcome measures assessing social interactions and behaviors through questionnaire or observation. A critical appraisal, using the McMaster Critical Review Form for Quantitative Studies, was performed to assess methodological quality.
Results
Four studies of varying research design and quality met the inclusion criteria. The participants in these studies were aged between 3–12 years of age. The duration of the intervention ranged from 10–14 weeks, and each study used varied measures of outcome. Overall, all the studies showed some improvements in social interactions or behaviors following a Halliwick-based hydrotherapy intervention.
Interpretation
Few studies have investigated the effect of hydrotherapy on the social interactions and behaviors of children with ASDs. While there is an increasing body of evidence for hydrotherapy for children with ASDs, this is constrained by small sample size, lack of comparator, crude sampling methods, and the lack of standardized outcome measures. Hydrotherapy shows potential as a treatment method for social interactions and behaviors in children with ASDs.
Keywords: evidence-based practice, aquatic therapy, pediatrics, secondary research
Background
Autism spectrum disorders (ASDs), including Asperger’s syndrome and “atypical autism or pervasive developmental disorder – not otherwise specified,” are a group of neurodevelopment disorders “defined by compositions of impairments in three domains: reciprocal social interaction, neutral verbal and non-verbal communication alongside with inflexible behavior patterns, interests and activities (DSM-IV-TR/ICD-10 [Diagnostic and Statistical Manual of Mental Disorders-IV-Text Revision/International Classification of Disease]).”1 Historical prevalence reports are approximately four per 10,000 children;2 however, more recent data suggests an increasing prevalence of one in 88 US children, or 90 per 10,000.3,4
Whilst the diagnostic criteria for ASDs is based on social and behavioral impairments, children with ASDs may often present with motor skill difficulties and delays that may lead to decreased physical activity levels and social play.5–9 A range of treatment options are available, including behavioral therapy, sensory integration, dance and music therapies, diet modification, speech and language therapy, occupational and physical therapy, animal interaction, and pharmacological adjunct therapies.3,10–12
Hydrotherapy has been used for musculoskeletal and neuromuscular rehabilitation for over 100 years.11 It has been shown to improve motor performance in children with muscular dystrophy, cerebral palsy, cystic fibrosis, spina bifida, and Rett syndrome.11 Hydrotherapy is based on the principles of hydrodynamics (buoyancy, relative density, viscosity, resistance, hydrostatic pressure, turbulence, and flow) and is thought to provide multiple sensory stimuli through water temperature, weight relief, and vestibular input. The properties of water assist active movement, provide postural support, and promote relaxation of spastic muscles, improved circulation, and strengthening, allowing a variety of fundamental motor skills to be performed, relative to an individual’s skill level.6,13 Aquatic activities also provide opportunities for social interaction and play, which can facilitate language development and improve self-esteem, self-awareness, and sense of accomplishment.5
In recent years, there has been increased focus on specific hydrotherapy interventions for people with disabilities. For example, the Halliwick method14 was developed by James McMillan in the late 1940s, to introduce people with disabilities to the aquatic environment. Using the principles of hydrodynamics and body mechanics, the Halliwick method comprises four phases: adjustment to water, rotations, control of movement in water, and movement in water.15,16 Application of the Halliwick method follows a 10-point program.17
Anecdotally, in clinical practice, the Halliwick method is often the basis of many hydrotherapy programs, although it is adapted to meet the individual needs of patients/clients.
Research into the effects of a hydrotherapy program on children with increased needs is growing. Fragala-Pinkham et al18 found that a 14-week hydrotherapy exercise program improved cardiorespiratory endurance and fitness in children with disabilities, including ASDs. Pan7 found improvements of muscular strength and endurance in children with ASDs, following hydrotherapy. Motor performance was increased in children with ASDs, following a 12-week hydrotherapy program, in a study by Yanardag et al.5
Bumin et al19 found a decrease in stereotypical movements, in a child with stage III Rett Syndrome, after an 8-week, Halliwick-based hydrotherapy program: hand skills, balance, gait, and interaction with her environment improved, while her hyperactive behavior and anxiety was reduced. Pan7 found significant improvements in self-confidence, social performance, and relationships, in children with ASDs, as reported by parents.
A survey of 18 occupational therapists using hydrotherapy to treat young children with ASDs reported a substantial increase in attention, muscle strength, balance, toleration of touch, initiation and maintenance of eye contact, and social participation.11 Additionally, children with ASDs and their parents described aquatic therapy, water play skills, and swimming as enjoyable.5
The aim of our review was to investigate the effectiveness of hydrotherapy interventions in improving the social interaction and behaviors of children with ASDs. Improvements in these areas would extend the application of hydrotherapy beyond physical impairments, in children with ASDs.
Methods
Search strategy
This review was conducted and reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.20 In March 2013, a search of six electronic databases was conducted collaboratively by the two reviewers. The searched databases included: Cochrane (all available dates), Cumulative Index to Nursing and Allied Health Literature (CINAHL) (January 1982–March 2013), PsycINFO (January 1840–March 2013), Embase (January 1980–March 2013), MEDLINE® (January 1966–March 2013), and Academic Search Premier (January 1975–March 2013). Only studies published in English were included. No date restrictions were applied as there were no known published systematic reviews. Table S1 outlines the search question and keywords used in the search strategy. The reference lists of all the included studies were reviewed to elicit any relevant studies that were not located by the electronic search.
Study design
All forms of primary and secondary evidence were searched for, including systematic reviews, retrospective studies, randomized control trials (RCTs), controlled clinical trials (CCTs), and case studies.
Population
Studies were included for consideration if the participants were aged 3–18 years, of either sex, and diagnosed with ASDs (including Asperger’s syndrome and pervasive developmental disorders), irrespective of the diagnostic criteria used. Participants had to be at a high-functioning level to participate in a hydrotherapy intervention. Exposure to prior aquatic experience or other prior interventions did not result in any exclusion of participants.
Intervention
Studies were included if the intervention described a hydrotherapy program, such as the Halliwick method.14 Studies describing interventions of swimming and other water sports, water play, and land-based aquatic play were not considered.
Outcome measures
Studies were included if they utilized outcome measures that assessed social interaction and behavior through questionnaire or observation, such as the School Social Behavior Scales (SSBS-2), observational stereotypical movement analysis, or Computerized Evaluation Protocol of Interactions in Physical Education (CEPI-PE). Possible adverse effects from hydrotherapy interventions include fatigue due to increased physical activity and regression of social or motor behaviors, due to change in routine or environment. Such adverse effects would have ethical and clinical considerations. The adverse effects were considered.
Search of literature
A review protocol was established and the databases searched. The results of the searches were pooled, and duplicates removed. Potential studies were identified by evaluating the title and abstract to determine their appropriateness, following the Population, Intervention, Comparator and Outcome (PICO) criteria (as described in Table 1). The relevant studies were independently reviewed in full by the two reviewers to determine their inclusion, based on the predetermined criteria and the evidence hierarchy. Any disagreement was resolved with discussion or, when needed, through consultation with a third party.
Table 1.
Search strategy (PICO criteria)
| Definition | |
|---|---|
| Population | Children aged 3–8 years diagnosed with ASDs |
| Intervention | Hydrotherapy program, such as the “Halliwick method”14 |
| Comparator | N/A |
| Outcome | Assessing social interaction and behavior through questionnaire or observation |
Abbreviations: ASDs, autism spectrum disorders; N/A, not available; PICO, Population, Intervention, Comparator and Outcome.
Quality assessment
The methodological quality of the included studies was independently assessed by the two reviewers. The hierarchy of evidence for all the studies was assessed according to the National Health and Medical Research Council (NHMRC) designation of levels of evidence.21 The McMaster Critical Review Form for Quantitative Studies22 was used for all RCTs, CCTs, and single case study designs.
Data extraction and analysis
The data was extracted by the two reviewers and collated into excel spread sheets, including information related to: study design; participants’ information (age, sex, and diagnosis); intervention components; intervention duration; dose and frequency of the intervention; experimental design and method randomization; outcome measures; statistical analyses; and the results of pre- and postanalysis or other appropriate analysis. Any disagreement was resolved through discussion and consultation with a third party, where needed.
The collected data were compared, but due to the small number of studies and variability in the outcome measures, a meta-analysis was not appropriate. Therefore, a narrative analysis was performed by the two reviewers.
Body of evidence framework
The NHMRC body of evidence framework was used in the interpretation of findings and the implications for clinical practice. The framework evaluated the included studies along five dimensions of evidence. The five components of the framework assessed: 1) the quantity, quality, and level of evidence; 2) consistency; 3) clinical impact; 4) generalizability; and 5) applicability to the Australian health care setting – this latter was not included in this review as the intervention may be implemented in an international population. Based on this framework, evidence-based recommendations for practice and research could be made.
Results
Search results
The search strategy returned 61 total “hits,” 43 of these were potentially relevant studies. After removal of the duplicates and review of the full-text versions, a total of four studies were identified as being eligible for review. The search strategy is outlined in Figure 1. Potentially relevant articles that fulfilled initial inclusion criteria were subsequently excluded for the following reasons:
Figure 1.
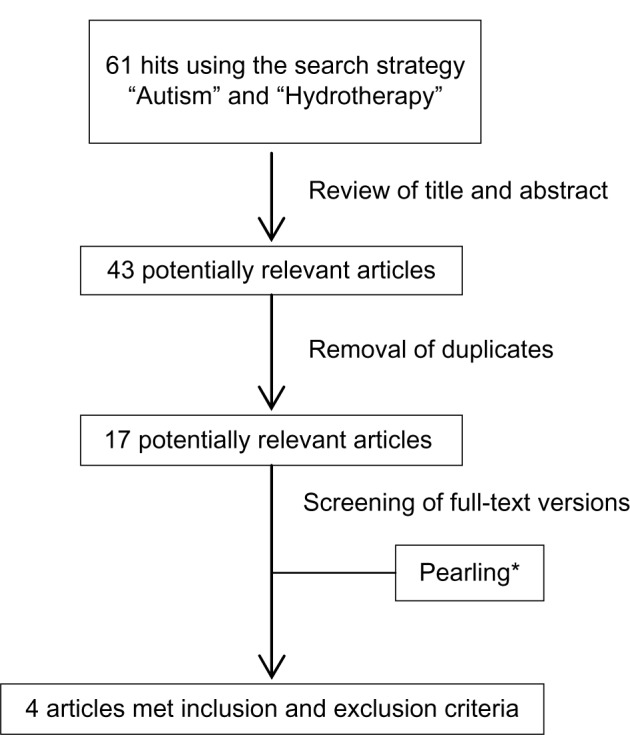
Consort diagram.
Notes: *Pearling refers to a review of the reference lists of identified studies in search of any additional studies that might not have been sourced through the literature search. It is also termed secondary searching.
Intervention was a swimming program not hydrotherapy
Diagnosis of Rett syndrome
Outcome measures did not assess social interactions and behaviors (ie, only assessed physical fitness or motor skill performance)
No valid outcome measure used
Not an experimental research design
Full-text article not published in English.
Methodological quality
The included studies were assessed for methodological quality using the NHMRC designation of levels of evidence and the McMaster Critical Review Form for Quantitative Studies. The results of the critical appraisal are outlined in Table 2. Two studies were rated as NHMRC level III and two were rated as level IV. Two of the studies received moderate McMaster scores23,25 whereas the two others received low scores.15,24
Table 2.
Levels of evidence and methodological quality of included studies
| Study | NHMRC designation of levels of evidence | McMaster critical appraisal tool score |
|---|---|---|
| Yilmaz et al15 | IV | 6/13 (46%) |
| Pan24 | III-3 | 10/14 (71%) |
| Ennis25 | IV | 6/14 (43%) |
| Chu and Pan26 | III-2 | 11/14 (79%) |
Abbreviation: NHMRC, National Health and Medical Research Council.
Studies received lowered McMaster scores because they were deficient with respect to random allocation of subjects, concealed allocation, homogeneity of sample, blinding of subjects and therapists, reporting of dropouts, justification of sample size, and addressing contamination and cointervention. Two of the studies did not address the analysis method appropriately, and one study did not report dropouts. Only one study included blinding of measurers. One study did not describe the intervention in detail, and two did not give details on the validity and reliability of outcome measures. Table 2 provides an overview of the NHMRC designation of levels of evidence and the critical appraisal scores for the individual studies.
Study characteristics
The included studies were published from 2004–2012. They comprised one single-subject case study with pre- and postmeasurements;15 one controlled, single-blinded, within-participant repeated measures crossover study with 10 weeks of follow up;23 one (pre- and postmeasure) case series;24 and one study that included three intervention arms (trained peer assistance, trained sibling assistance, or untrained assistance [the controls]).25 One study was conducted in Turkey,15 two in Taiwan,23,25 and one in the US.24
Participant characteristics
Table 3 outlines the characteristics of each study. The number of participants in the studies was one, eleven, 16, and 42. The participants’ age ranged from 3–12 years. Ethnicity was not reported by any of the studies. The diagnoses included high-functioning autism and Asperger’s syndrome. The diagnostic criteria were not specified for two of the articles;15,24 the other two23,25 sought independent diagnosis according to the DSM-IV criteria. One study excluded individuals with intellectual disability as a concurrent condition, another excluded participants with a history of previous or current psychiatric or neurological disorder aside from ASD, and one study included participants with comorbidities such as spina bifida and cerebral palsy.
Table 3.
Study characteristics
| Study | Research design | Age (yrs) | N | Diagnosis | Intervention | Outcome measure | Results |
|---|---|---|---|---|---|---|---|
| Yilmaz et al15 | Case study | 9 | 1 | Not specified | Hydrotherapy program using Halliwick method14 10 wks, 3 times/wk, 60 min |
Video analysis of behaviors before and after intervention | Decrease in stereotypical movements Increase response to stimuli |
| Pan24 | CCT | 6–9 | 16 | DSM-IV criteria High-functioning autism (n=8) Asperger’s syndrome (n=8) |
Water exercise swimming program based on HAAR, according to Halliwick 10 wks, 2 times/wk, 90 min 21 wks total: 10 wks WESP, 10 wks control, 1 wk transition |
SSBS-2 | Improvements in social interactions and behavior Maintained after 10 weeks of follow up |
| Ennis25 | Case series | 3–9 | 11 5 dropouts |
ASD, including Asperger’s syndrome and PDD–NOS Secondary diagnoses included spina bifida and cerebral palsy |
Aquatic program 10 wks, 2 times/wk, 60 min |
Peds-QL | Improvement in Peds-QL total scores Individual improvements in social skills, school functioning, and emotional functioning |
| Chu and Pan26 | CCT | 7–12 | 42 21 ASD |
DSM-IV criteria High-functioning autism (n=14) Asperger’s syndrome (n=7) |
Aquatic program based on HAAR according to Halliwick 16 wks, 2 times/wk, 60 min |
CEPI-PE | All children with ASD showed improvements in physical and social behaviors (higher with trained peer/sibling assistance) Decrease in physical interactions with teachers and some physical interactions with peers/siblings |
Abbreviations: ASD, autism spectrum disorder; CCT, controlled clinical trial; CEPI-PE, Computerized Evaluation Protocol of Interactions in Physical Education; DSM, Diagnostic and Statistical Manual of Mental Disorders; HAAR, Humphries’ Assessment of Aquatic Readiness; PDD-NOS, pervasive developmental disorder – not otherwise specified; Peds-QL, Pediatric Quality of Life Inventory™; SSBS-2, School Social Behavior Scales; WESP, water exercise swimming program.
Types of intervention
All four studies based their hydrotherapy intervention on the Halliwick method. Two of the studies used the Humphries’ Assessment of Aquatic Readiness assessment instruction, which was developed in accordance with the foundations of the Halliwick method. The protocol used by Ennis24 included specific skill performance and free time. Table 3 specifies the duration of each program. The hydrotherapy programs consisted of two to three sessions per week, over 10–16 weeks; the individual sessions ranged from 60–90 minutes. Progression of the aquatic activities was paced individually, over the course of the program.
The study by Chu and Pan25 had three intervention arms: a peer-assisted group (PG), a sibling-assisted group (SG), and a control group (CG) participating in the intervention concurrently. Pan23 had two intervention groups participating in a cross-over design: during the first 10 weeks group A received hydrotherapy while group B participated in their usual activities, this was followed by a 1-week transition, then another 10 weeks in which group B received hydrotherapy and group A participated in their usual activities. When not receiving hydrotherapy, each group participated in their regular treatment and activities. Ennis24 conducted two consecutive 10-week interventions. In that study, six children completed one 10-week intervention, and three completed the two 10-week interventions.
Measures
The outcome measures used in each study are identified in Table 3. One study15 assessed participants’ behaviors, including: stereotypical movement analysis (spinning, swinging, and delayed echolalia) and no or late (within 5 seconds) reaction to stimulus. The assessment was based on an analysis of 45-minute-long video camera footage. Another study23 used the SSBS-2 to assess social behaviors. The SSBS-2 is a classroom teacher-rated, norm-referenced standardized instrument that assesses social competencies, such as peer relations, self-management/compliance, and academic behavior, as well as antisocial behavior, such as hostile/irritable, antisocial/aggressive, and defiant/disruptive behaviors. The third study24 used the Pediatric Quality of Life Inventory™ (Peds-QL) parent survey to assess quality of life issues; the results of the Peds-QL were reported as total scores and as physical functioning, emotional functioning, social functioning, and school functioning subscale scores. The fourth study25 used the CEPI-PE to assess physical and social interaction behaviors. This assessment was focused on four subcategories of interactions: between the child with ASD and the instructor; between the child with ASD and their designated peer/sibling; between the child with ASD and the other children with ASD; and between the child with ASD and the other typically developing peers/siblings in the group. The social interaction behaviors could be voluntary or spontaneous, or verbal or nonverbal. The physical interaction behaviors consisted of active engagement in individual or group aquatic activities. Each 50-minute observation session was recorded on videotape and analyzed.
All the studies measured participants before and after the hydrotherapy interventions. One arm of the Pan23 study was measured after a 10-week follow-up period, due to its crossover design. Two studies15,24 did not identify the validity or reliability of the outcome measure. The other two23,25 reported a high degree of validity and reliability of their respective outcome measures.
Outcome
Table 4 provides a summary of results from the included studies. The summarized findings indicate that hydrotherapy had a positive impact on the social interactions and behaviors in children with ASD.
Table 4.
Summary of results
| Study | Summarized findings on the effect of hydrotherapy on social interactions and behaviors
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Stereotypical movements | Response to stimuli | Social interactions | Antisocial behaviors | Physical interactions – peers/siblings | Physical interactions – teachers | School behavior and academic performance | Emotional functioning | |
| Yilmaz et al15 | ↓ (+) | ↑ (+) | ||||||
| Pan24 | ↑ (+) | ↓ (+) | ↑ (+) | |||||
| Ennis25 | (+) | (+) | (+) | (+) | ||||
| Chu and Pan26 | ↑ (+) | Mixed | ↓ (±) | |||||
Notes: ↑ = increased, ↓ = decreased, (+) = positive change/improvement, (±) = could be interpreted as positive or negative change.
Yilmaz et al15 reported a reduction in participants’ stereotypical movements following the 10-week hydrotherapy intervention. The duration of three stereotypical movements was measured before and after the hydrotherapy intervention (and was decreased for all three): the duration of swinging was 7 minutes and 5 minutes, respectively; the duration of spinning was 2 minutes and 0 minutes, respectively; and the duration of delayed echolalia was 4 minutes and 2 minutes, respectively. The researchers also found an increase in the participants’ reaction to stimuli. The number of nonreactions to stimuli decreased, from 12 to 6, at the pre and postintervention 45-minute behavioral analyses, respectively.
Pan23 reported significant improvements (P<0.01) in the participants’ social interactions and behaviors following each group’s hydrotherapy intervention. Both groups had significant improvements (P<0.01) in hostile/irritable and antisocial behavior. Further improvement (P<0.01) in hostile/irritable behavior was seen at the 10 week follow-up assessment of Group A (no follow-up was done for Group B). Group A also demonstrated significant improvements (P<0.01) in academic behavior, aggressive behavior, and defiant/disruptive behavior, while group B showed significant improvement (P<0.01) in social competence. There was no overall between-group difference in outcomes.
In the study by Ennis,24 there was a decrease in the Peds-QL score in 67% of children, indicating positive changes across the areas of social, emotional, school, and physical function. These positive changes were seen in most of the Peds-QL subscores, although this was to varying degrees: 83% of children showed an increase in social functioning, 50% showed an increase in school functioning, 67% showed an increase in physical functioning, and 50% showed an increase in emotional functioning. In addition, in one participant, there was no change in either the emotional or school subscale over the 10-week intervention.
In addition to these results, the three participants who completed both of the 10-week interventions showed continued improvements in most subscales: 67% showed improved total Peds-QL scores (one showed no change), 67% showed improvement in physical functioning, 100% showed an improvement in emotional functioning, 33% showed improvement in social functioning (one showed no change), and 100% showed an improvement in school functioning.
Chu and Pan25 showed improved social interactions with peers/siblings and teachers and reduced physical interactions with teachers, in all groups, during the group activity time. The untrained CG group showed improved physical interactions with peers/siblings, whereas the PG- and SG-assisted groups showed a decrease. Additionally, the PG- and SG-assisted groups showed improvement in social interactions with other peers/siblings and other children with ASD during this time.
During the individual activity time, the CG group (with untrained peers/siblings) showed no significant improvements, whereas both the PG- and SG-assisted groups (which had trained peers/siblings) showed improved physical interactions with peers, improved social interactions with peers and teachers, and reduced physical interactions with teachers.
Thus, the children with ASD who were assisted by trained peers or siblings had significantly greater improvement in social and physical interactions compared with those who had untrained peers or siblings assisting them.
NHMRC body of evidence framework
The analysis of the results, using the NHMRC body of evidence framework, is described in Table 5. Given that the overall body of evidence was limited in size and had methodological flaws, the results of this review should be applied with caution. Despite positive outcomes being reported in every study, there are several factors that were unclear or were inadequately addressed – the grade of evidence was lowered due to these inconsistencies in the current evidence base. Therefore, the implementation of recommendations should be made with caution.
Table 5.
NHMRC body of evidence framework
| Component | Grade | Comments |
|---|---|---|
| Evidence base | D – poor Level IV studies, or level I to III studies with high risk of bias |
Quantity: total of four studies Total participants: 49 children with ASD (5 dropouts) Level III: two studies Level IV: two studies Quality: low |
| Consistency | D – poor Evidence is inconsistent |
Multiple study designs While all participants were diagnosed with ASD, the prevalence of comorbidities was not addressed or was unclear Multiple and varied outcome measures Statistical analysis adequate in two of the four studies |
| Clinical impact | D – poor Slight or restricted |
One study reported effect size and for others, the effect size could not be calculated due to insufficient data While intervention protocol was adequately described, no justification for parameters or developmental process were outlined Consistent findings for only one outcome (social interaction), with varied outcomes for other measures Minimal reporting of outcomes relating to academic performance, behaviors, and physical and emotional functioning No adverse effects were reported but reasons for dropouts not addressed Only one study undertook follow-up (for up to 10 weeks) and other studies did not report any ongoing follow-up data |
| Generalizability | B – good Population(s) studied in body of evidence is/are similar to the target population |
Population studied in the evidence base is similar to the target population Age range 6–12 years Samples included in the studies were high functioning individuals The current evidence base lacks clarity in terms of reporting of comorbidities and cointerventions and its impact on outcomes, and small sample sizes that did not represent the autism spectrum and did not include any teenagers |
| Grade of recommendation | D – poor Body of evidence is weak, and recommendation should be applied with caution |
Limited number of studies were identified from the literature Overall, these studies were low level and were of low quality While some congruency in findings across all four studies, the current evidence base lacks clarity in terms of the prevalence of comorbidities, poor justification of parameters and developmental processes, differing outcome measures, and lack of long-term follow-up |
Abbreviations: ASD, autism spectrum disorder; NHMRC, National Health and Medical Research Council.
Discussion
The four studies included in the systematic review investigated the effect of a hydrotherapy program on the social interactions and behaviors of children aged 3–12 years who were diagnosed with high functioning autism or Asperger’s syndrome. In all four studies, the respective hydrotherapy intervention, each underpinned by the Halliwick method, resulted in improvements in social interactions and behaviors. Follow-up studies showed that at 10 weeks postintervention, there was a carryover effect, and further improvement after a second round of intervention was also observed.
The results of this review correspond with previous small-scale research evidence reporting the benefits of hydrotherapy programs on social interactions and behaviors, in children with ASDs.9,11,26–31 Chu and Pan25 have suggested these improvements may be due to enforced social interaction with peers or siblings through the constructs of the hydrotherapy program and guidance of the instructor. Children with ASDs benefit from receiving constant individual attention from the instructor and from observing the positive social interactions of others during hydrotherapy sessions.23,25 Lessons from clinical practice indicate that the potential benefits from hydrotherapy include: stimulation of vocalization and language; improved toleration of touch; encouragement of eye contact, and improved confidence.11,30 While not the focus of hydrotherapy sessions, these benefits may have holistic effects and hence translate to improved relationships with peers and siblings and increased social acceptance.25
Effect on social interactions and behaviors
The decreased physical interaction with teachers observed by Chu and Pan25 may not necessarily be a negative result. As discussed by Chu and Pan, this change may be interpreted as positive in that the child with ASD is less reliant on adult interaction and more willing to interact with his/her peers. Vonder Hulls et al11 discussed similar findings in their research, suggesting that a decrease in children with ASDs asking teachers for help could be interpreted positively as a sign that the child is gaining confidence and independence, rather than as diminishing interactions.
Effect of age, sex, ethnicity
The results from this review are likely to be applicable to the broader ASD population. However, the variable presentation of the ASD population in social, behavioral, and physical domains could affect outcome, as discussed in Vonder Hulls et al.11 Thus, the four reviewed studies included only high-functioning individuals, and the effectiveness at the lower-functioning end of the spectrum is unknown. Within the ASD population, age may not be a limiting factor as social, behavioral, and physical impairments can continue through life. There is also the possibility of extending these results to application in the management of other neurodevelopmental disorders involving social interaction and behavioral impairments.
Interventions
The structure of the hydrotherapy sessions was consistent across the four studies, and all the interventions were based on the principles of the Halliwick method. The intensity of the intervention was comparable between the studies: three of the four studies were of 60 minutes duration, one was 90 minutes; two of the four studies conducted sessions twice a week, and the third conducted sessions three times a week (the fourth was not defined); hydrotherapy interventions were held over 10–16 weeks. These designs are commonly employed in hydrotherapy interventions.5,7–9,11,18,31
One study25 implemented the assistance of trained or untrained typically developing peers and siblings in the hydrotherapy program. This was a unique concept, and greater improvements were seen in the children with ASDs who were assisted by a trained peer or sibling. Similar results have been found in land-based interventions utilizing trained typically developing peers or siblings.32–34
Limitations
As with any research, there are some limitations of this systematic review. Despite considerable searching of the literature, we were able to locate only four studies that met the inclusion criteria. The included studies had low-level research designs (level III or IV) and had some issues of methodological quality. The methodological concerns in areas such as sampling techniques, allocation of subjects to treatment groups, homogeneity of treatment groups, and blinding may be difficult to address due to the population of interest and the intervention administered (thus, for example, efforts were made to control for the variable presentation of ASDs rather than to randomly allocate the participants to treatment groups). The sample sizes were generally small and lacking justification, possibly due to the poor availability of children with ASDs to participate in the studies. The breadth of the social and behavioral impairments in children with ASDs impedes standardization of the scope and intent of outcome measures utilized in studies; given the diversity of the outcome measures used and heterogeneity in sampling and interventions, a direct comparison of results between studies was not possible.
There also exist possible limitations in implementing the intervention in question. Access to hydrotherapy services is likely to be influenced by a number of factors, such as local health care models of service delivery and funding arrangements. These factors need to be taken into account when considering hydrotherapy as an option.
Conclusion
Implications for clinical practice
There is an increasing body of evidence to support the widely held view that a hydrotherapy intervention, underpinned by the Halliwick approach, may be effective in improving the social interactions and behaviors of children with ASDs. Further, it has been identified that the improvements in social interactions and behaviors may be further enhanced by the use of trained peers or siblings to assist the child with ASDs during the hydrotherapy intervention. However, while hydrotherapy may be considered as an adjunct treatment for the problematic social interactions and behaviors in children with ASDs, it must be recognized that the current evidence base also suffers from important methodological issues.
Implications for future research
An emerging body of evidence has been identified to support the use of a hydrotherapy intervention for improving the social interactions and behaviors of children with ASDs. However, significant research limitations have also been recognized, highlighting the need for further research. Future studies could address the effect of age, the intensity of intervention, class size, and student-teacher ratio, and the feasibility of applying hydrotherapy for individuals at the lower-functioning end of the autism spectrum. Future studies may also improve on the current evidence by implementing a standardized outcome measure. Sampling methods could be improved, to increase the sample size derived from representative population, and long-term follow-up undertaken, to capture the sustainability and durability of outcomes. It would also be beneficial to determine the effect of hydrotherapy as a stand-alone intervention compared with other interventions or combination of interventions, and to determine the effect of the parameters underpinning the hydrotherapy program. Additionally, future research should integrate the recently released DSM-V diagnostic criteria into the sampling strategies and explore the impact of this approach to diagnosis on the selection of relevant interventions.
Supplementary materials
Table S1.
Search terms and relevant literature from the database search
| Database | Search terms | Mesh/Subject headings | Limiters | Hits | Relevant hits |
|---|---|---|---|---|---|
| Medline | Autis* or ASD or ASDs or “Autis* Spectrum Disorder*” or |
exp Child Development Disorders, Pervasive/or exp Autistic Disorder/or exp Asperger Syndrome/ exp Hydrotherapy |
English language and (“all child (0 to 18 years)”; or “preschool child (2 to 5 years)” or “child (6 to 12 years)” or “adolescent (13 to 18 years)”) | 5 | 4 |
| PsychINFO | “Pervasive Development* Disorder*” or PDD or PDDs or Asperger* Hydrotherapy OR Halliwick or |
DE “Autism” OR DE “Pervasive Developmental Disorders” OR DE “Aspergers Syndrome” OR DE “Autism” OR DE “Rett Syndrome” OR DE “Aspergers Syndrome” DE “Hydrotherapy” |
English; age groups: childhood (birth–12 yrs), preschool age (2–5 yrs), school age (6–12 yrs), adolescence (13–17 yrs) | 7 | 7 |
| EMBASE | hydro-therapy or “water therapy” or “water based” or “water exercise” or “aquatic exercise” or “aquatic based” or |
exp Asperger syndrome/or exp autism/or exp “pervasive developmental disorder not otherwise specified”/ exp Hydrotherapy/ |
English language and (child <unspecified age> or preschool child <1 to 6 years> or school child <7 to12 years> or adolescent <13 to 17 years>) | 10 | 9 |
| CINAHL | “aquatic therapy” or “pool based” or “pool therapy” or “pool exercise” or balneotherapy or aquatic |
“Child Development Disorders, Pervasive+” OR “Asperger Syndrome” OR “Autistic Disorder” OR “Pervasive Developmental Disorder-Not Otherwise Specified” “Hydrotherapy+” OR “Aquatic Exercises” OR “Water” OR “Balneology” |
Language: English; age groups: child, preschool: 2–5 years, child: 6–12 years, adolescent: 13–18 years, all child | 10 | 7 |
| COCHRANE | 3 | 3 | |||
| Academic Search Premier |
DE “AUTISM” OR DE “ASPERGER’S syndrome” OR DE “AUTISM in adolescence” OR DE “AUTISM in adults” OR DE “AUTISM in children” OR DE “AUTISM – Treatment” OR DE “AUTISM in adolescence” OR DE “ASPERGER’S syndrome in adolescence” OR DE “AUTISM in children” OR DE “AUTISM in children – Case studies” OR DE “AUTISM spectrum disorders” OR DE “ASPERGER’S syndrome” OR DE “AUTISM” OR DE “RETT syndrome” DE “HYDROTHERAPY” OR DE “BATHS, Moor & mud” OR DE “BATHS, Partial” OR DE “SPONDYLOTHERAPY” OR DE “HYDROTHERAPY for children” |
English language | 26 | 13 |
Abbreviations: ASD, autism spectrum disorder; Mesh, medical subject headings; PDD, pervasive developmental disorder.
Acknowledgments
We would like to thank Dr Lucylynn Lizarondo for her prompt and helpful guidance throughout the initial stages of this review.
Author contributions
RM and MP conceptualized the topic, developed the search strategy, carried out the search of literature and data extraction, and contributed equally to the development of the final draft. SK instituted the use of the NHMRC body of evidence framework and revised the draft. All the authors contributed toward data analysis, revision of the manuscript and are accountable for all aspects of the work.
Disclosure
The lead author (RM) is currently employed by a community-based children’s service organization that provides services to children living with disabilities and special needs, as well as support for their families and carers. The authors report no other conflicts of interest.
References
- 1.Bölte S, Westerwald E, Holtmann M, Freitag C, Poustka F. Autistic traits and autism spectrum disorders: the clinical validity of two measures presuming a continuum of social communication skills. J Autism Dev Disord. 2011;41(1):66–72. doi: 10.1007/s10803-010-1024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prior M. Is there an increase in the prevalence of autism spectrum disorders? J Paediatr Child Health. 2003;39(2):81–82. doi: 10.1046/j.1440-1754.2003.00097.x. [DOI] [PubMed] [Google Scholar]
- 3.Kong X, Chen L, Wang X. Future directions in autism treatment. N A J Med Sci. 2012;5(3):185–188. [Google Scholar]
- 4.Matson JL, Kozlowski AM. The increasing prevalence of autism spectrum disorders. Res Autism Spectr Disord. 2011;5(1):418–425. [Google Scholar]
- 5.Yanardag M, Akmanoglu N, Yilmaz I. The effectiveness of video prompting on teaching aquatic play skills for children with autism. Disabil Rehabil. 2013;35(1):47–56. doi: 10.3109/09638288.2012.687030. [DOI] [PubMed] [Google Scholar]
- 6.Lee J, Porretta DL. Enhancing the motor skills of children with autism spectrum disorders. JOPERD. 2013;84(1):41–45. [Google Scholar]
- 7.Pan CY. The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders. Res Autism Spectr Disord. 2011;5(1):657–665. [Google Scholar]
- 8.Fragala-Pinkham MA, Haley SM, O’Neil ME. Group swimming and aquatic exercise programme for children with autism spectrum disorders: a pilot study. Dev Neurorehabil. 2011;14(4):230–241. doi: 10.3109/17518423.2011.575438. [DOI] [PubMed] [Google Scholar]
- 9.Fragala-Pinkham M, O’Neil ME, Haley SM. Summative evaluation of a pilot aquatic exercise program for children with disabilities. Disabil Health J. 2010;3(3):162–170. doi: 10.1016/j.dhjo.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Reid G, O’Connor J. The autism spectrum disorders: activity selection, assessment, and programme organization. Palaestra. 2003;19(1):20–27. [Google Scholar]
- 11.Vonder Hulls DS, Walker LK, Powell JM. Clinicians’ perceptions of the benefits of aquatic therapy for young children with autism: a preliminary study. Phys Occup Ther Pediatr. 2006;26(1–2):13–22. doi: 10.1300/j006v26n01_03. [DOI] [PubMed] [Google Scholar]
- 12.Field T, Lasko D, Mundy P, et al. Brief report: autistic children’s attentiveness and responsivity improve after touch therapy. J Autism Dev Disord. 1997;27(3):333–338. doi: 10.1023/a:1025858600220. [DOI] [PubMed] [Google Scholar]
- 13.Dumas H, Francesconi S. Aquatic therapy in pediatrics: annotated bibliography. Phys Occup Ther Pediatr. 2001;20(4):63–78. [PubMed] [Google Scholar]
- 14.Martin J. The Halliwick Method. Physiotherapy. 1981;67(10):288–291. [PubMed] [Google Scholar]
- 15.Yilmaz I, Yanarda M, Birkan B, Bumin G. Effects of swimming training on physical fitness and water orientation in autism. Pediatr Int. 2004;46(5):624–626. doi: 10.1111/j.1442-200x.2004.01938.x. [DOI] [PubMed] [Google Scholar]
- 16.Yılmaz I, Konukman F, Birkan B, Yanardag M. Effects of most to least prompting on teaching simple progression swimming skill for children with autism. Educ Train Dev Disabil. 2010;45(3):440–448. [Google Scholar]
- 17.Skinner A, Thomson A. Aquatics therapy and the Halliwick concept. Exceptional Parent. 2008;38(7):76–77. [Google Scholar]
- 18.Fragala-Pinkham M, Haley SM, O’Neil ME. Group aquatic aerobic exercise for children with disabilities. Dev Med Child Neurol. 2008;50(11):822–827. doi: 10.1111/j.1469-8749.2008.03086.x. [DOI] [PubMed] [Google Scholar]
- 19.Bumin G, Uyanik M, Yilmaz I, Kayihan H, Topçu M. Hydrotherapy for Rett syndrome. J Rehabil Med. 2003;35(1):44–45. doi: 10.1080/16501970306107. [DOI] [PubMed] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 21.Merlin T, Weston A, Tooher R. Extending an evidence hierarchy to include topics other than treatment: revising the Australian ‘levels of evidence’. BMC Med Res Methodol. 2009;9:34. doi: 10.1186/1471-2288-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Law M, Stewart D, Pollock N, Letts L, Bosch J, Westmorland M. Critical Review Form—Quantitative Studies. Hamilton, ON: McMaster University; 1998. [Accessed December 23, 2013]. http://www.srs-mcmaster.ca/Portals/20/pdf/ebp/quanreview.pdf. [Google Scholar]
- 23.Pan CY. Effects of water exercise swimming program on aquatic skills and social behaviors in children with autism spectrum disorders. Autism. 2010;14(1):9–28. doi: 10.1177/1362361309339496. [DOI] [PubMed] [Google Scholar]
- 24.Ennis E. The effects of a physical therapy-directed aquatic program on children with autism pectrum disorders. Journal of Aquatic Physical Therapy. 2011;19(1):4–10. [Google Scholar]
- 25.Chu CH, Pan CY. The effect of peer- and sibling-assisted aquatic program on interaction behaviors and aquatic skills of children with autism spectrum disorders and their peers/siblings. Res Autism Spectr Disord. 2012;6(3):1211–1223. [Google Scholar]
- 26.Killian KJ, Joyce-Petrovich RA, Menna L, Arena SA. Measuring water orientation and beginner swim skills of autistic individuals. Adapt Phys Activ Q. 1984;1(4):287–295. [Google Scholar]
- 27.Huettig C, Darden-Melton B. Acquisition of aquatic skills by children with autism. Palaestra. 2004;20(2):20–46. [Google Scholar]
- 28.Harland K. A Will of His Own: Reflections on Parenting a Child with Autism. London: Jessica Kingsley Publishers; 2007. Revised edition. [Google Scholar]
- 29.Best JF, Jones JG. Movement therapy in the treatment of autistic children. Aust Occup Ther J. 1974;21(2):72–86. [Google Scholar]
- 30.Dulcy F. An integrated developmental aquatic program (IDAP) for children with autism. National Aquatics Journal. 1992;8(2):7–10. [Google Scholar]
- 31.Yilmaz İ, Birkan B, Konukman F, Erkan M. Using a constant time delay procedure to teach aquatic play skills to children with autism. Educ Train Dev Disabil. 2005;40(2):171–182. [Google Scholar]
- 32.Weiss MJ, Harris SL. Teaching social skills to people with autism. Behavior Modification. 2001;25(5):785–802. doi: 10.1177/0145445501255007. [DOI] [PubMed] [Google Scholar]
- 33.Tsao LL, Odom SL. Sibling-mediated social interaction intervention for young children with autism. Topics Early Child Spec Educ. 2006;26(2):106–123. [Google Scholar]
- 34.Bass JD, Mulick JA. Social play skill enhancement of children with autism using peers and siblings as therapists. Psychol Sch. 2007;44(7):727–735. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1.
Search terms and relevant literature from the database search
| Database | Search terms | Mesh/Subject headings | Limiters | Hits | Relevant hits |
|---|---|---|---|---|---|
| Medline | Autis* or ASD or ASDs or “Autis* Spectrum Disorder*” or |
exp Child Development Disorders, Pervasive/or exp Autistic Disorder/or exp Asperger Syndrome/ exp Hydrotherapy |
English language and (“all child (0 to 18 years)”; or “preschool child (2 to 5 years)” or “child (6 to 12 years)” or “adolescent (13 to 18 years)”) | 5 | 4 |
| PsychINFO | “Pervasive Development* Disorder*” or PDD or PDDs or Asperger* Hydrotherapy OR Halliwick or |
DE “Autism” OR DE “Pervasive Developmental Disorders” OR DE “Aspergers Syndrome” OR DE “Autism” OR DE “Rett Syndrome” OR DE “Aspergers Syndrome” DE “Hydrotherapy” |
English; age groups: childhood (birth–12 yrs), preschool age (2–5 yrs), school age (6–12 yrs), adolescence (13–17 yrs) | 7 | 7 |
| EMBASE | hydro-therapy or “water therapy” or “water based” or “water exercise” or “aquatic exercise” or “aquatic based” or |
exp Asperger syndrome/or exp autism/or exp “pervasive developmental disorder not otherwise specified”/ exp Hydrotherapy/ |
English language and (child <unspecified age> or preschool child <1 to 6 years> or school child <7 to12 years> or adolescent <13 to 17 years>) | 10 | 9 |
| CINAHL | “aquatic therapy” or “pool based” or “pool therapy” or “pool exercise” or balneotherapy or aquatic |
“Child Development Disorders, Pervasive+” OR “Asperger Syndrome” OR “Autistic Disorder” OR “Pervasive Developmental Disorder-Not Otherwise Specified” “Hydrotherapy+” OR “Aquatic Exercises” OR “Water” OR “Balneology” |
Language: English; age groups: child, preschool: 2–5 years, child: 6–12 years, adolescent: 13–18 years, all child | 10 | 7 |
| COCHRANE | 3 | 3 | |||
| Academic Search Premier |
DE “AUTISM” OR DE “ASPERGER’S syndrome” OR DE “AUTISM in adolescence” OR DE “AUTISM in adults” OR DE “AUTISM in children” OR DE “AUTISM – Treatment” OR DE “AUTISM in adolescence” OR DE “ASPERGER’S syndrome in adolescence” OR DE “AUTISM in children” OR DE “AUTISM in children – Case studies” OR DE “AUTISM spectrum disorders” OR DE “ASPERGER’S syndrome” OR DE “AUTISM” OR DE “RETT syndrome” DE “HYDROTHERAPY” OR DE “BATHS, Moor & mud” OR DE “BATHS, Partial” OR DE “SPONDYLOTHERAPY” OR DE “HYDROTHERAPY for children” |
English language | 26 | 13 |
Abbreviations: ASD, autism spectrum disorder; Mesh, medical subject headings; PDD, pervasive developmental disorder.


