Abstract
Enhanced external counterpulsation (EECP) has been approved by the United States Food and Drug Administration (FDA) for management of refractory angina (Class IIb). EECP uses three sets of pneumatic cuffs that sequentially contract during diastole, increasing aortic diastolic pressure, augmenting coronary blood flow and central venous return. EECP improves anginal symptoms and exercise tolerance, and reduces nitroglycerin use in patients with chronic, stable angina. EECP has also been shown to be safe and beneficial in patients with symptomatic stable congestive heart failure. It has been postulated that cardiac benefits of EECP are mediated though vascular endothelial growth factor (VEGF) and nitric oxide mediated vasodilatation and angiogenesis. In June 2002, the FDA also approved EECP therapy for heart failure patients.
Keywords: Angina, Enhanced external counterpulsation (EECP), Heart failure, International EECP patient registry, Myocardial Infarction, Percutaneous Coronary Intervention
There is a high prevalence of symptomatic coronary artery disease (6.4 million patients) in the United States, with an annual incidence of about 400,000.1 In a subset of these patients: angina is not optimally controlled despite optimal medical management and coronary revascularization. This condition is termed refractory angina.2 The Scottish Intercollegiate Guidelines Network for management of refractory angina include: education, rehabilitation, cognitive behavioral therapy, spinal cord stimulation, transcutaneous electrical nerve stimulation, left stellate ganglion block, thoracoscopic sympathectomy, angiogenesis, and surgical transmyocardial revascularization, among others.3
In 1953, Kantrowitz demonstrated that coronary blood flow can be increased 20% to 40% by increasing diastolic blood pressure.4 Intra-aortic balloon pump (IABP) counterpulsation is an invasive method of increasing coronary blood flow, while enhanced external counterpulsation (EECP) is a non-invasive method. EECP therapy has been approved by the United States Food and Drug Administration (FDA) (Class IIb) for management of refractory angina and heart failure.
Methods
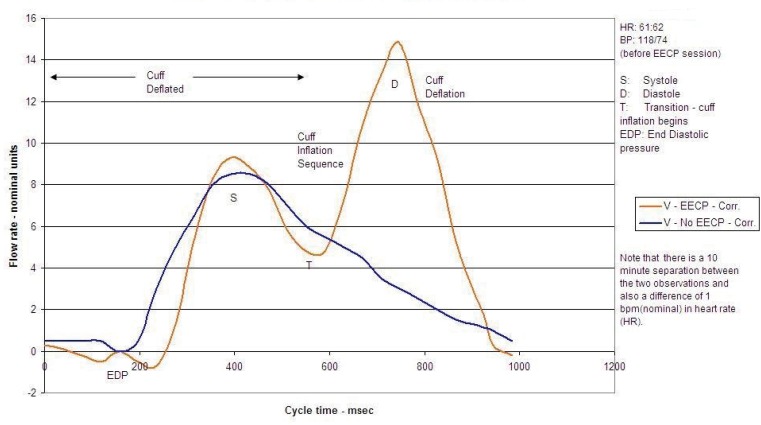
EECP is a registered trademark (timing mechanism of the machine) of Vasomedical, Inc., Westbury, New York, which manufactures EECP equipment in the United States. Most published studies have used Vasomedical EECP equipment. EECP therapy consists of three sets of pneumatic cuffs attached to each of the patient’s legs at the calf and lower and upper thigh. The inflation of the cuffs is triggered by a computer, and timing of the inflation is based on the R wave of the electrocardiogram. The EECP therapist adjusts the inflation and deflation timing to provide optimal blood movement per a finger plethysmogram waveform reading. This produces a retrograde flow of blood in the aorta (aortic counterpulsation), resulting in a diastolic augmentation of blood flow and also an increase in venous return, which leads to an improved coronary perfusion pressure during diastole. Shortly afterwards, the cuffs simultaneously deflate before the onset of systole, thereby decreasing vascular resistance, assisting with systolic unloading, and decreasing cardiac workload.2
Figure 1.
Schematic of the sequential diastolic and systolic deflations of leg cuffs during EECP therapy.
The typical EECP course involves 35 one-hour sessions that the patient attends each week, Monday through Friday. However, two sessions can be completed per day if the patient so desires and is able to tolerate the sessions. The course of therapy can be extended for patients who do not start to develop improvement of their symptoms until late in the course of therapy. Additional treatment hours may be considered on a case-by-case basis for the patient to reach individual treatment objectives. Specifically, for patients who initially present with angina, a reduction of symptom frequency and/or intensity would be a measurement of progress. For patients with comorbidities or physical limiting factors, the therapy may be less effective and additional hours of treatment may be warranted.5,6 Repeat EECP may be required in about 20% of patients, especially if they failed to complete the initial 35-hours of EECP therapy.5
According to Vasomedical protocol, exclusion criteria for EECP include arrhythmias that interfere with machine triggering, bleeding diathesis, active thrombophlebitis, severe lower extremity vaso-occlusive disease, presence of a documented aortic aneurysm requiring surgical repair, and pregnancy. Precautions include decompensated heart failure, aortic insufficiency, severe mitral or aortic stenosis, uncontrolled hypertension, and heart rates greater than 120 beats per minute. Hypertension and elevated heart rates should be controlled before starting treatment, and heart failure patients should be stable before starting treatment. EECP is well tolerated, and the usual side effects are equipment-related, including leg and back pain, skin abrasion, bruising, blistering, edema, and paresthesias.2,5,6 The beneficial effects include reduced myocardial oxygen demand, increased venous return and cardiac output, improved endothelial function, prolonged time to exercise-induced ST depression on 12-lead electrocardiogram, and improvement or resolution of myocardial perfusion defects.6
Overall, EECP has been proven to be a safe therapy, as reported by the International EECP patient registry (IEPR) in 2000. Of 2511 patients treated, 0.3% died, 0.9% had a myocardial infarction, 0.2% had bypass grafting, and 0.8% had percutaneous coronary intervention (PCI) during the treatment period.7,8
Discussion
Role of EECP in Angina
The multicenter study-EECP (MUST-EECP)9 was the landmark prospective, blinded, multicenter study that randomly assigned 139 patients with chronic stable angina and positive exercise stress tests to full-dose EECP or a sham method with minimal pressures. The study showed significant increase in exercise time post-EECP from baseline (426 ± 20 to 470 ± 20s, P<0.001) versus the sham group (432 ± 22 to 464 ± 22s, P<0.03), and significant improved time to ≥ 1mm ST-segment depression in the EECP group (337±18 to 379±18s, P<0.002) compared with the sham group (326±21 to 330±20s, P<0.74). These results were maintained 12 months after EECP treatment.9,10
The IEPR demonstrated that 78% of patients had a reduction of ≥1 angina class, and 38% of patients had improvement of at least two classes. At least a 50% reduction in frequency of angina was experienced by 76% of patients as well as improvement in quality-of-life assessment that was sustained for at least 2-years.7,8 Loh et al11 conducted a follow-up review in 2008 that followed 1061 patients from the IEPR-1 (previously described) who maintained significant improvements in both weekly anginal events and quality of life at 3-years following completion of EECP therapy, compared with data obtained 1-week post-therapy.
A 5-year, single-center, non-randomized study in 33 patients with coronary artery disease, treated with EECP and grouped as responders vs non-responders found that major adverse cardiovascular events or mortality occured in 6 of 7 patients (86%) in the non-responder group and 6 of 26 patients (23%) in the responder group.12 The overall 5-year survival of EECP-treated patients was 88%, comparable to that seen with medical and revascularization therapies. At 5-years of follow-up, 64% of patients were alive without interim cardiovascular events or need for revascularization.12
The IEPR data also demonstrated an 83% reduction in hospitalization rates, compared to 6 months before EECP. About 86% of IEPR patients completed the 35-hour treatment.13 The EECP completion rate was a major indicator for benefit from EECP; there were significantly lower rates of myocardial infarction, coronary artery bypass grafting, and PCI mortality at 1-year among those who completed the 35-hour EECP therapy compared to those who did not.14 At 5-years, major adverse cardiovascular events (death, acute myocardial infarction, new coronary artery bypass grafting, new PCI, valve replacement, unstable angina) were significantly lower among EECP responders (23%) compared to non-responders (86%).12 EECP responders also have significant post-therapy improvements in perfusion defects on radionucleotide stress tests performed to the same cardiac work load and double product.12,15–17 EECP also has shown positive psychosocial effects amongst recipients.18
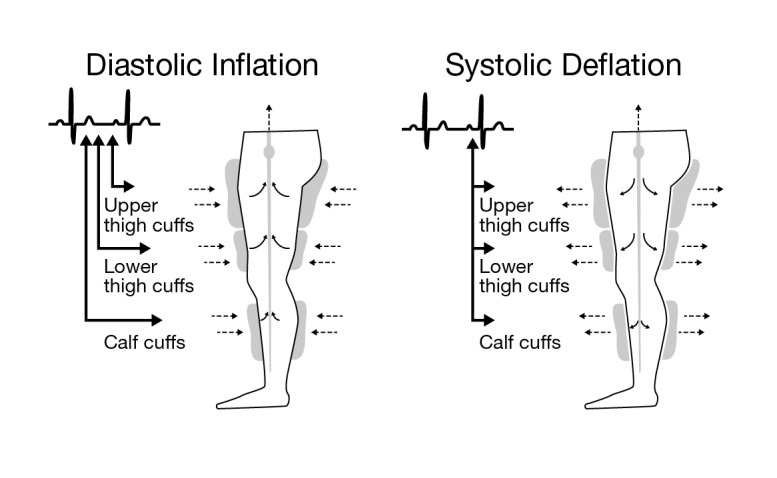
Figure 2.
Finger pleythysmogram showing the changes in vascular flow rate during EECP therapy; Blue curve indicates blood pressure without EECP; brown curve shows augmentation of blood flow as EECP cuff is inflated. [S: systole, D: diastole, T: transition (cuff inflation begins), EDP: end-diastolic pressure.]
Role of EECP in Congestive Heart Failure
Earlier studies have indicated a higher incidence of heart failure in patients with left ventricular dysfunction based on EECP increasing venous return and preload, hence precipitating pulmonary edema.19 The Prospective Evaluation of Enhanced External Counterpulsation in Congestive Heart failure (PEECH)20 trial of 187 subjects with stable, symptomatic, mild-to-moderate heart failure (left ventricular ejection fraction [LVEF] ≤35 %) on optimal medical management demonstrated a significant increase in exercise time of at least 60 seconds in the EECP group (35%) compared to control group (25%), with a significant improvement of the Minnesota Living with Heart Failure score at 1 week and 3 months after treatment. There was no significant difference in the peak VO2 between the groups. A subgroup analysis of patients over age 65 from the PEECH trial (EECP n=41, control n=44) demonstrated a 6-month higher response rate in the peak VO2 group compared to the control group (29.7% vs 11.4%, P=0.017).20
The PEECH20 trial further demonstrated that 33.3% of patients showed improvement of at least one class of New York Heart Association (NYHA) classification 1-week post-EECP therapy, with 31.3% of patients reporting improvement in classification 6-months post-therapy. Of note, 11.4% and 14.3% of placebo patients reported the same results, respectively.21
Improvements in quality-of-life assessments without any major complications have also been demonstrated at 1 week and 6 months after EECP. In a study of 450 patients with refractory angina and left ventricular dysfunction (ejection fraction [EF]< 30 ± 8%) EECP significantly reduced 6-month emergency room visits by 78% and hospitalizations by 73%.22
EECP Mechanism in Congestive Heart Failure
Significant improvements in B-type natriuretic peptide, uric acid, free-T3/free-T4 ratio, and mitral annular E velocity have been observed in a prospective cohort study post-EECP therapy compared to baseline.23 EECP therapy has been shown to significantly increase LVEF and significantly reduce resting heart rate.24 EECP therapy has also been shown to be of benefit for patients with ischemic and non-ischemic cardiomyopathy, systolic or diastolic dysfunction.25 A study of 26 patients with heart failure (class II/III NYHA and average EF of 23%) showed clinical benefit without any major adverse cardiac effect.26
Role of EECP in Hypertension
A study of 108 consecutive patients receiving EECP demonstrated a significant (6.4 ± 16.2 mm Hg) reduction in systolic blood pressure at the end of therapy with no statistically significant effect on diastolic blood pressure or heart rate. Systolic blood pressure increased in the two lowest strata (<100 mmHg and 101–110 mmHg) and decreased in the remaining strata (111–120 mmHg, 121–130 mmHg, 131–140 mmHg, and ≥141 mmHg) (P< 0.001). These stratified differences were sustained after each EECP session as well as the immediate end and at 6 weeks of the EECP course.27 A recent study by Gurovich and Braith28 demonstrated that even a single session of EECP-related blood flow patterns improved flow-mediated dilation in femoral and brachial arteries in healthy subjects.
EECP in Acute Coronary Syndrome with Cardiogenic Shock
A single-center, prospective study of ten patients with acute coronary syndrome and/or cardiogenic shock, ineligible for IABP counterpulsation, and received two to four 1-hour bedside treatments by portable EECP demonstrated a lack of portable EECP-related adverse effects like bleeding complications, heart failure exacerbation, skin breakdown, or interference with nursing care.29 EECP treatment resulted in significant increase in 30-minute mean arterial pressure compared to baseline (P=0.0002) and dyspnea severity (P=0.036) without significant changes in heart rate, pulse oximetry, or urine output. This study also suggests improved cardiovascular performance and possibly clinical outcomes with acute inpatient EECP in patients with acute coronary syndrome and cardiogenic shock.29
Role of EECP in Non-cardiac Conditions
EECP has been tried in treatment of restless leg syndrome,30 erectile dysfunction,31 hepatorenal syndrome,32 Syndrome X,33 and retinal artery occlusion,34 although it is not FDA-approved for management of these conditions. EECP has been shown to improve transdermal oxygen concentration and concentration of moving red blood cells and significantly reduced transdermal carbon dioxide pressure and velocity of blood cells in healthy subjects probably due to peripheral vasodilatation.35
Mechanism of Action
Endothelium
EECP responders have significant immediate increase in the reactive hyperemia-peripheral arterial tonometry (a non-invasive method of measuring peripheral endothelial function) index after each treatment and at 1-month.36 Endothelium plays an integral part in vascular homeostasis, and its dysfunction leads to imbalance between nitric oxide—a potent vasodilator, anti-proliferative, anti-inflammatory molecule—and endothelin-1—a potent vasoconstrictor, mitogen, and pro-inflammatory molecule.37 A prospective study of 25 patients by Barsheshet et al38 demonstrated EECP-related increase in median number of endothelial progenitor cells (10.2 to 17.8 cells, P<0.001) and colony forming units (3.5 to 11, P=0.01). EECP leads to improved coronary blood flow derived from increased shear stress,39 which leads to increased endothelial nitric oxide release and resultant vasodilatation.40 Patients with coronary artery disease have been noted to have a significant increase in levels of plasma nitric oxide levels and a significant decrease in plasma endothelin-1 levels, 1 month after a course of EECP.41,42 In a prospective study by Shechter et al43 in 2003 of 20 patients with coronary artery disease, EECP resulted in significant improvement in flow-mediated dilatation of the brachial artery (8.2 ± 2.2%, P=0.01) compared to controls (3.1± 2.2%, P= 0.78).
A randomized controlled study of 42 patients with symptomatic coronary artery disease (35 one-hour EECP [n=28] and sham-EECP [n=14]) by Braith et al44 showed significant increase in flow-mediated dilatation of brachial arteries (51% vs 2%) and femoral arteries (31% vs 5%), while reducing endothelin-1 (−25% vs +5%) and nitric oxide synthase inhibitor asymmetric dimethyl arginine (−28% vs +0.2%).
Oxidative stress
Oxidative stress is associated with various cardiovascular risk factors and plays a key role in the etiology of atherogenesis and endothelial dysfunction.45 Furthermore, Braith et al44 showed EECP-mediated reduction in pro-inflammatory cytokines (tumor necrosis-α [−16% vs +12.1%], monocyte chemoattractant protein-1 [−13% vs +0.2%], vascular cell adhesion molecule-1 [−6% vs +1%], hs C-reactive protein [−32% vs +5%], and lipid peroxidation marker 8-isoprostane platelet growth factor 2α [−21% vs +1.3%]) with treatment vs sham.
Angiogenesis
Shear stress is a known stimulus for coronary collateral development and recruitment.46 Vascular endothelial growth factors (VEGF) and platelet-derived growth factors that are crucial in angiogenesis are upregulated by vascular shear stress.47,48 A course of EECP has shown to increase plasma levels of VEGF, basic fibroblast growth factor, and hepatocyte growth factor in a study of 11 patients with stable angina.49 VEGF is known to induce nitric oxide synthase expression and activity. Endothelial nitric oxide stimulates the effect of VEGF on endothelial cells and their organization in networklike structures.50 In a study of 6-week EECP on 12 beagle dogs, Wu et al48 demonstrated a significant increase in the microvessels density per mm(2) in the infarcted regions (vWF, 15.2 +/− 6.3 vs 4.9 +/− 2.1, P < 0.05; alpha-actin, 11.8 +/− 5.3 versus 3.4 +/− 1.2, P< 0.05) of EECP group compared to control group, respectively. There was also a significant increase in VEGF expression, and they demonstrated that an increase in capillary density corresponded to improved myocardial perfusion by 99mTc-sestamibi single-photon emission computed tomography.51
A 2013 prospective interventional study of 50 patients by Eslamian et al52 demonstrated significant difference between perfusion scan ischemia severity before and 1-month post-EECP completion (P=0.04). A prospective study by Buschmann et al53 showed significant improvement in coronary flow index (from 0.08 ± 0.01 to 0.15 ± 0.02; P< 0.001) and fractional flow reserve (from 0.68 ± 0.03 to 0.79 ± 0.03; P= 0.001) in EECP-treated patients (n=16) compared to none in the control group (n=7), indicating the stimulation of coronary arteriogenesis via EECP in patients with stable coronary artery disease.53
Exercise capacity
EECP may promote improvement in exercise duration with no change in peak double product by reduction in peripheral vascular resistance.54
Controversies
Limited data from well-designed, multicenter, randomized, prospective data are available on the efficacy and efficiency of EECP. Both randomized-controlled trials (MUST-EECP9 and PEECH20) received sponsorship from Vasomedical, the EECP manufacturer. These studies included patients with chronic stable angina, and refractoriness to standard anginal treatment was not a mandatory requirement. Also, patients with class IV angina, overt heart failure, unstable angina, and myocardial infarction within 3 months were excluded. The MUST-EECP9 intervention group had longer duration of angina and higher incidence of prior myocardial infarction, and personnel administering the EECP were not blinded.
Most available studies have critical limitations such as conclusions based on subjective assessment, failure to complete the entire 35 one-hour EECP course, and lack of comparison group. The PEECH20 trial failed to maintain a statistically significant improvement in Quality of Life after 6 months. The EECP group had a higher attrition rate (23.7%) compared to control group (13.85) due to adverse events.2
A prospective study by Dockery et al55 did not show significant change in arterial stiffness parameters as measured by carotid-radial pulse wave velocity and aortic augmentation index, despite a significant improvement in treadmill exercise time and blood pressure reduction after a 7-week EECP therapy. Hence, the study suggests that factors besides change in arterial wall mechanics could be contributing to the sustained clinical benefit seen by EECP.55 Available data are unclear on whether EECP in non-responders contributed to a higher incidence of adverse cardiac events than responders. A small subgroup analysis of the PEECH trial showed that the EECP benefit seen in patients with ischemic cardiomyopathy was not seen in patients with non-ischemic cardiomyopathy. This may have been attributed to low patient numbers and non-blinding of patients to therapy, hence leading to a placebo effect.21
Some data from IEPR reveal that in patients with EF ≤ 35% there is a significant increase in adverse cardiac events, death, congestive heart failure, and hospitalization after 6 months.19 Non-randomized trials conducted with limited patients and at a limited number of institutions usually run the risk of selection bias and placebo effect influencing the outcome of the trial. Data on longterm cardiac mortality are unavailable; hence symptomatic improvement with EECP does not guarantee improved survival or reduced cardiovascular mortality.
In 2010, Braith et al’s44 randomized controlled trial of 42 patients demonstrated significant EECP-mediated dilation of brachial and femoral arteries and release of vasoactive agents reduction of pro-inflamatory markers. However, the small patient number affects the power and generalizabilty of the study. Also, the clinical significance of peripheral flow dynamics and endovascular chemicals is largely unknown.44
Conclusion
EECP has been used in the treatment of angina for the past two decades with a record of safety and, more recently, several publications which support its efficacy. It is approved by the FDA for the treatment of chronic or unstable angina and in patients with congestive heart failure. Treatment has been associated with improved exercise tolerance and myocardial perfusion, as evidenced by nuclear imaging and positron emission tomography. More research will hopefully shed additional light on the mechanism of action and verify the longterm attenuation of symptoms in patients with unstable angina pectoris and in those with congestive heart failure.
References
- 1.American Heart Association 2002 Heart and Stroke Statistical Update. Dallas, TX: American Heart Association; 2001 [Google Scholar]
- 2.Braverman D. EECP Clinical Studies. Health Technology Assessment 2009;13:1–13 [Google Scholar]
- 3.Scottish Intercollegiate Guidelines Network Management of stable angina a national clinical guideline. SIGN guideline 96. Edinburgh: SIGN; 2007 [Google Scholar]
- 4.Kantrowitz A. Experimental augmentation of coronary flow by retardation of arterial pulse pressure. Surgery 1953;34: 678–687 [PubMed] [Google Scholar]
- 5.Braverman DL. Enhanced external counterpulsation: an innovative physical therapy for refractory angina. PM R.2009;1: 68–276 [DOI] [PubMed] [Google Scholar]
- 6.Bonetti PO, Holmes DR, Jr, Lerman A, Barsness GW. Enhanced external counterpulsation for ischemic heart disease: what’s behind the curtain? J Am Coll Cardiol 2003;41:1918–1925 [DOI] [PubMed] [Google Scholar]
- 7.Soran O, Kennard ED, Kfoury AG, Kelsey SF, IEPR Investigators Two-year outcomes after enhanced external counterpulsation (EECP) therapy in patients with refractory angina pectoris and left ventricular dysfunction (report from the International EECP Patient Registry). Am J Cardiol 2006;97:17–20 [DOI] [PubMed] [Google Scholar]
- 8.Michaels AD, Linnemeier G, Soran O, Kelsey SF, Kennard ED. Two-year outcomes after Enhanced External Counterpulsation for stable angina pectoris (from the International EECP patient registry [IEPR]). Am J Cardiol 2004;93:461–464 [DOI] [PubMed] [Google Scholar]
- 9.Arora RR, Chou TM, Jain D, Fleishman B, Crawford L, McKiernan T, Nesto RW. The multicenter study of enhanced external counterpulsation (MUST-EECP): effect of EECP on exercise-induced myocardial ischemia and anginal episodes. J Am Coll Cardiol 1999;33:1833–1840 [DOI] [PubMed] [Google Scholar]
- 10.Cohn PF. Enhanced external counterpulsation for treatment of angina pectoris. Prog Cardiovasc Dis 2006;49:88–97 [DOI] [PubMed] [Google Scholar]
- 11.Loh PH, Cleland JG, Louis AA, Kennard ED, Cook JF, Caplin JL, Barness GW, Lawson WE, Soran OZ, Michaels AD. Enhanced external counterpulsation in the treatment of chronic refractory angina: a long-term follow-up outcome from the International Enhanced External Counterpulsation Patient Registry. Clin Cardiol 31: 59–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawson WE, Hui JC, Cohn PF. Long-term prognosis of patients with angina treated with enhanced external counterpulsation: five-year follow-up study. Clin Cardiol 2000;23:254–258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawson WE, Linnemeier G, et al. Predictor of hospitalization in end stage coronary disease: The effect of enhanced external counterpulsation. AHA quality of care and outcome. Research in Cardiovascular Disease and Stroke Conference; Washington DC April 2325, 2009 [Google Scholar]
- 14.Lawson WE, Hui JC, Kennard ED, Barsness G, Kelsey SF, IEPR Investigators Predictors of benefit in angina patients one year after completion of enhanced external counterpulsation: initial responders to treatment versus non responders. Cardiology 2005;103:201–206 [DOI] [PubMed] [Google Scholar]
- 15.Lawson WE, Hui JC, Soroff HS, Zheng ZS, Kayden DS, Sasvary D, Atkins H, Cohn PF. Efficacy of enhanced external counterpulsation in treatment of angina pectoris. Am J Cardiol 1992;70:859–862 [DOI] [PubMed] [Google Scholar]
- 16.Lawson WE, Hui JC, Zheng ZS, Burgen L, Jiang L, Lillis O, Oster Z, Soroff H, Cohn P. Improved exercise tolerance following enhanced external counterpulsation: cardiac of peripheral effect? Cardiology 1996;87:271–275 [DOI] [PubMed] [Google Scholar]
- 17.Lawson WE, Hui JC, Guo T, Burger L, Cohn PF. Prior revascularization increases the effectiveness of enhanced external counterpulsation. Clin Cardiol 1998;21:841–844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Springer S, Fife A, Lawson W, Hui JC, Jandorf L, Cohn PF, Fricchione G. Psychosocial effects of enhanced external counterpulsation in the angina patient: a second study. Psychosomatics 2001;42:124–132 [DOI] [PubMed] [Google Scholar]
- 19.Lawson WE, Kennard EE, Holubkov R, Kelsey SF, Strobeck JE, Soran O, Feldman AM, IEPR Investivators Benefit and safety of enhanced external counterpulsation in treating coronary artery disease patients with a history of congestive heart failure. Cardiology 2001;96:78–84 [DOI] [PubMed] [Google Scholar]
- 20.Abbotsmith CW, Chung ES, Varricchione T, de Lame PA, Silver MA, Francis GS, Feldman AM, Prospective Evaluation of EECP in Congestive Heart Failure Investigators Enhanced external counterpulsation improves exercise duration and peak oxygen consumption in older patients with heart failure: a subgroup of the PEECH trial. Congest Heart Fail 2006;12:307–311 [DOI] [PubMed] [Google Scholar]
- 21.Feldman AA, Silver MA, Francis GS, Abbottsmith CW, Fleishman BL, Soran O, de Lame PA, Varricchione T, PEECH Investigators Enhanced external counterpulsation improves exercise tolerance in patients with chronic heart failure. J Am Coll Cardiol 2006;48:1198–1205 [DOI] [PubMed] [Google Scholar]
- 22.Soran O, Kennard ED, Bart BA, Kelsey SF, IEPR Investigators Impact of external counterpulsation treatment on emergency department visits and hospitalization in refractory angina patients with left ventricular dysfunction. Congest Heart Fail 2007;13:36–40 [DOI] [PubMed] [Google Scholar]
- 23.Kozdağ G, Ertaş G, Aygün F, Emre E, Kirbaş A, Ural D, Soran O. Clinical effects of enhanced external counterpulsation treatment in patients with ischemic heart failure. Anadolu Kardiyol Derg 2012;12:214–221 [DOI] [PubMed] [Google Scholar]
- 24.Gorcsan J, III, Crawford L, Soran O, et al. Improvements in left ventricular performance by enhanced external counterpulsation in patients with heart failure. J Am Coll Cardiol 2000;35 Suppl:230A10636285 [Google Scholar]
- 25.Prasad GN, Ramasamy S, Thomas JM, Nayar PG, Sankar MN, Sivakadaksham N, Cherian KM. Enhanced external counterpulsation therapy: current evidence for clinical practice and who will benefit? Indian Heart J 2010;62:296–302 [PubMed] [Google Scholar]
- 26.Soran O, Fleishman B, Demarco T, Grossman W, Schneider VM, Manzo K, de Lame PA, Feldman AM. Enhanced external counterpulsation in patients with heart failure: a multicenter feasibility study. Congest Heart Fail 2002;8:204–208 [DOI] [PubMed] [Google Scholar]
- 27.Campbell AR, Satran D, Zenovich AG, Campbell KM, Espel JC, Arndt TL, Poulose AK, Boisjolie CR, Juusola K, Bart BA, Henry TD. Enhanced external counterpulsation improves systolic blood pressure in patients with refractory angina. Am Heart J. 2008;156:1217–1222 [DOI] [PubMed] [Google Scholar]
- 28.Gurovich AN, Braith RW. Enhanced external counterpulsation creates acute blood flow patterns responsible for improved flow-mediated dilation in humans. Hypertens Res 2013;36:297–305 [DOI] [PubMed] [Google Scholar]
- 29.Cohen J, Grossman W, Michaels AD. Portable enhanced external counterpulsation for acute coronary syndrome and cardiogenic shock: a pilot study. Clin Cardiol 2007;30:223–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rajaram SS, Shanahan J, Ash C, Walters AS, Weisfogel G. Enhanced external counterpulsation as a novel treatment for restless leg syndrome (RLS): a preliminary test of the vascular neurologic hypothesis for RLS. Sleep Med 2005;6:101–106 [DOI] [PubMed] [Google Scholar]
- 31.Froschermaier SE, Werner D, Leike S, Schneider M, Waltenberger J, Daniel WG, Wirth MP. Enhanced external counterpulsation as a new treatment modality for patients with erectile dysfunction. Urol Int 1998;61:168–171 [DOI] [PubMed] [Google Scholar]
- 32.Werner D, Tragner P, Wawer A, Porst H, Daniel WG, Gross P. Enhanced external counterpulsation: a new technique to augment renal function in liver cirrhosis. Nephrol Dial Transplant 2005;20:920–926 [DOI] [PubMed] [Google Scholar]
- 33.Kronhaus KD, Lawson WE. Enhanced external counterpulsation is an effective treatment for Syndrome X. Int J Cardiol 2009;135:256–257 [DOI] [PubMed] [Google Scholar]
- 34.Werner D, Michalk F, Harazny J, Hugo C, Daniel WG, Michelson G. Acclerated reperfusion of poorly perfused retinal areas in central retinal artery occlusion and branch retinal artery occlusion after a short treatment with enhanced external counterpulsation. Retina 2004;24:541–547 [DOI] [PubMed] [Google Scholar]
- 35.Hilz MJ, Werner D, Marthol H, Flachskampf FA, Daniel WG. Enhanced external counterpulsation improves skin oxygenation and perfusion. Eur J Clin Invest 2004;34:385–391 [DOI] [PubMed] [Google Scholar]
- 36.Bonetti PO, Barsness GW, Keelan PC, Schnell TI, Pumper GM, Kuvin JT, Schnall RP, Holmes DR, Higano ST, Lerman A. Enhanced external counterpulsation improves endothelial function in patients with symptomatic coronary artery disease. J Am Coll Cardiol 2003;41:1761–1768 [DOI] [PubMed] [Google Scholar]
- 37.Lerman A, Burnett JC., JrIntact and altered endothelium in regulation of vasomotion. Circulation 1992;86:12–19 [PubMed] [Google Scholar]
- 38.Barsheshet A, Hod H, Shechter M, Sharabani-Yosef O, Rosenthal E, Barbash IM, Matetzky S, Tal R, Bentancur AG, Sela BA, Nagler A, Leor J. The effects of external counterpulsation therapy on circulating endothelial progenitor cells in patients with angina pectoris. Cardiology. 2008;110:160–166 [DOI] [PubMed] [Google Scholar]
- 39.Kern MJ, Aguirre F, Bach R, Donohue T, Siegel R, Segal J. Augmentation of coronary blood flow by intra-aortic balloon pumping in patients after coronary angioplasty. Circulation 1993;87:500–511 [DOI] [PubMed] [Google Scholar]
- 40.Davies PF. Flow-mediated endothelial mechanotransduction. Physiol Rev 1995;75:519–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Masuda D, Nohara R, Hirai T, Kataoka K, Chen LG, Hosokawa R, Inubushi M, Tadamura E, Fujita M, Sasayama S. Enhanced external counterpulsation improved myocardial perfusion and coronary flow reserve in patients with chronic stable angina: evaluation by (13)N-ammonia positron emission tomography. Eur Heart J 2001;22:1451–1458 [DOI] [PubMed] [Google Scholar]
- 42.Barsness GW. Enhanced External Counterpulsation in Unrevascularizable Patients. Curr Interv Cardiol Rep 2001;3:37–43 [PubMed] [Google Scholar]
- 43.Shechter M, Matetzky S, Feinberg MS, Chouraqui P, Rotstein Z, Hod H. External counterpulsation therapy improves endothelial function in patients with refractory angina pectoris. J Am Coll Cardiol 2003;42:2090–2095 [DOI] [PubMed] [Google Scholar]
- 44.Braith RW, Conti CR, Nichols WW, Choi CY, Khuddus MA, Beck DT, Casey DP. Enhanced external counterpulsation improves peripheral artery flow mediated dilatation in patients with chronic angina: a randomized sham-controlled study. Circulation 2010;122:1612–1620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cai H, Harrison DG. Endothelial dysfunction in cardiovascular diseases: the role of oxidant stress. Circ Res 2000;87:840–844 [DOI] [PubMed] [Google Scholar]
- 46.Kersten JR, Pagel PS, Chilian WM, Warltier DC. Multifactorial basis for coronary collateralization: a complex adaptive response to ischemia. Cardiovasc Res 1999;43:4457. [DOI] [PubMed] [Google Scholar]
- 47.Gan L, Miocic M, Daroudi R, Selin-Sjogren L, Jern S. Distinct regulation of vascular endothelial growth factor in intact human conduit vessels exposed to laminar fluid shear stress and pressure. Biochem Biophys Res Commun 2000;272:490–496 [DOI] [PubMed] [Google Scholar]
- 48.Wu G, Du Z, Hu C, Zheng Z, Zhan C, Ma H, Fang D, Ahmed KT, Laham RJ, Hui JC, Lawson WE. Angiogenic effects of long term enhanced external counterpulsation in a dog model of myocardial infarction. Am J Physiol Heart Circ Physiol 2006;290:H248H254. [DOI] [PubMed] [Google Scholar]
- 49.Resnick N, Collins T, Atkinson W, Bonthron DT, Dewey CF, Jr, Gimbrone MA., JRPlatelet-derived growth factor B chain promoter contains a cis-acting shear-stress-responsive element. Proc Natl Acad Sci USA 1993;90:4591–4595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Masuda D, Nahara K, Kataoka K, et al. Enhanced external counterpulsation promotes angiogenesis factors in patients with chronic stable angina (abstr). Circulation 2001;104:II445. [DOI] [PubMed] [Google Scholar]
- 51.Papapetropoulos A, Garcia-Cardena G, Madri JA, Sessa WC. Nitric oxide production contributes to the angiogenic properties of vascular endothelial growth factor in human endothelial cells. J Clin Invest 1997;100:3131–3139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eslamian F, Aslanabadi N, Mahmoudian B, Shakouri SK. Therapeutic effects of enhanced external counterpulsation on clinical sumptoms, echocardiographic measurements, perfusion scan parameters and exercise tolerance test in coronary artery disease patients with refractory angina. Int J Med Sci Public Health 2013;2:179–187 [Google Scholar]
- 53.Buschmann EE, Utz W, Pagonas N, Schuylz-Menger J, Busjahn A, Monti J, Maerz W, le Noble F, Thierfelder L, Dietz R, Klauss V, Gross M, Buschmann IR, Arteriogenesis Network (Art. Net.) Improvement of fractional flow reserve and collateral flow by treatment with external counterpulsation (Art.Net.-2 Trial). Eur J Clin Invest 2009;39:866–875 [DOI] [PubMed] [Google Scholar]
- 54.Stys TP, Lawson WE, Hui JC, Fleishman B, Manzo K, Srobeck JE, Tartaglia J, Ramasamy S, Suwita R, Zheng ZS, Liang H, Werner D. Effects of enhanced external counterpulsation on stress radionucleotide coronary perfusion and exercise capacity in chronic stable angina pectoris. Am J Cardiol 2002;89:822–824 [DOI] [PubMed] [Google Scholar]
- 55.Dockery F, Rajkumar C, Bulpitt CJ, Hall RJ, Bagger JP. Enhanced external counterpulsation does not alter arterial stiffness in patients with angina. Clin Cardiol. 2004;27:689–692 [DOI] [PMC free article] [PubMed] [Google Scholar]