Abstract
In 2008, the National Institute of Mental Health (NIMH) included in its new Strategic Plan the following aim: “Develop, for research purposes, new ways of classifying mental disorders based on dimensions of observable behavior and neurobiological measures”. The implementation of this aim was named the Research Domain Criteria project, or RDoC. RDoC is a programmatic initiative that will fund grants, contracts, early-phase trials, and similar activities for the purpose of generating studies to build a research literature that can inform future versions of psychiatric nosologies based upon neuroscience and behavioral science rather than descriptive phenomenology. RDoC departs markedly from the DSM and ICD processes, in which extensive workgroup meetings generate final and finely-honed sets of diagnoses that are modified in field tests only if problems with clinical utility arise. Rather, in keeping with its provenance as an experimental system, the RDoC provides a framework for conducting research in terms of fundamental circuit-based behavioral dimensions that cut across traditional diagnostic categories. While an important aim of the project is to validate particular dimensions as useful for eventual clinical work, an equally important goal is to provide information and experience about how to conceive and implement such an alternative approach to future diagnostic practices that can harness genetics and neuroscience in the service of more effective treatment and prevention. This paper summarizes the rationale for the RDoC project, its essential features, and potential methods of transitioning from DSM/ICD categories to dimensionally-oriented designs in research studies.
Keywords: Psychiatric diagnosis, Research Domain Criteria, RDoC, NIMH, DSM-5, translational research
A spirited debate about psychiatric diagnosis broke out on the eve of the DSM-5 release following a blog post by the Director of the National Institute of Mental Health (NIMH), Dr. Thomas Insel, entitled Transforming Diagnosis (1). In the post, Dr. Insel reviewed the common consensus in the research community regarding the problems with the DSM system, i.e., diagnoses based upon presenting signs and symptoms that have acceptable reliability but have increasingly been shown not to represent valid disease entities. Instead, he stated that the NIMH would “re-orient” its research away from the DSM-5 toward the NIMH's Research Domain Criteria (RDoC) project, developed to explore ways of incorporating such methods as genetics, neuroimaging, and cognitive science into future diagnostic schemes based upon behavioral dimensions and neural systems. The ensuing online discussion was unfortunately misguided, in that the post was addressed to the research community (and in particular, to potential peer reviewers of RDoC research grant applications) rather than to observers of the DSM-5, and the debate subsided following a joint press release by the NIMH and the American Psychiatric Association that reaffirmed the agencies' shared interests in psychiatric diagnosis and the important role played by the DSM in clinical use (2).
The scientific significance of the discussions, however, remained: the DSM-5 shows almost no influence of the remarkable advances in new technologies and substantive knowledge in neuroscience and behavioral science since the DSM-IV release in 1994, in spite of a decade-long literature review by committees of experts for the new revision. Dr. David Kupfer, the respected head of the DSM-5 process, was essentially correct in stating: “The problem that we've had in dealing with the data that we've had over the five to 10 years since we began the revision process of DSM-5 is a failure of our neuroscience and biology to give us the level of diagnostic criteria, a level of sensitivity and specificity that we would be able to introduce into the diagnostic manual” (3). His comment raises the obvious question: how does the field go about changing directions to remedy this pressing problem?
Students of nosology have considered at some length the kinds of research that need to be conducted in order to move toward more scientifically-informed conceptions of diagnosis and etiology. Considering the impressive range of disciplines that such commentaries represent, there is a remarkable consensus, as shown in the following small sample of quotations: “the DSM's descriptive criteria are designed to be transitional until research reveals etiologically distinct disorders among current syndromes” (4, p. 27); “empirical data have been quite consistent with the possibility that terms that are routinely used in clinical inquiry, from neuroticism and extraversion to depression and posttraumatic stress disorder, do not in fact represent meaningful, cohesive psychological constructs; rather, they represent combinations of constructs” (5, p. 281); “a more powerful approach is to move beyond simply rearranging symptom constellations, and to configure how known facts across the genomic, enviromic, endophenomic and phenomic domains may be reassembled to identify clusters of etiopathologically meaningful and empirically testable entities while remaining agnostic to traditional, phenotypic boundaries” (6, p. 11); “the field will have to collect data across the current diagnostic categories, focus on comparing across disorders as much as comparing across normal controls and will need to collect and curate data, so that it can be widely shared and collated” (7, p. 4). As a national funding agency charged with envisioning and implementing the future, the NIMH's goals are very much in harmony with such visions.
These insightful commentaries unfortunately omit one very inconvenient fact in the well-reasoned calls for new research directions: the DSM/ICD system has become the international de facto standard for submitting research grant applications to both private and public funding agencies, and conservative review processes are typically quite unforgiving of any deviations from orthodoxy. Further, the system has served so well for clinical, services, administrative, and legal purposes that any changes are now fraught due to the ripple effects that even the smallest changes in categories or criteria may have upon eligibility for mental health services, insurance payments, secular trends in prevalence rates, health care costs, research using the categories, and so on. Thus, the system's own success has become one of the largest barriers to change. In this light, the research enterprise is presented with a paradox. In order to attain groundbreaking nosological approaches in the future that are based upon genetics, other aspects of neurobiology, and behavioral science, a requisite literature is required that can inform these innovations in classification and measurement. However, such a research literature cannot be created as long as studies are conducted solely within the constraints of ICD/DSM categories. This is the rationale for the development of the RDoC project.
THE RDoC PROJECT
What does RDoC involve? The official statement of the RDoC goal – “Develop, for research purposes, new ways of classifying mental disorders…” – could be inferred to mean that NIMH has created a fully-fledged new nosology that is now ready for field trials. This is misleading. In fact, the goal of RDoC is to foster research to validate dimensions defined by neurobiology and behavioral measures that cut across current disorder categories, and that can inform future revisions of our diagnostic systems. In other words, RDoC is intended to support research toward a new classification system, but does not claim to be a completed system at the current time. To the contrary, RDoC represents a framework for conducting research on psychopathology in ways that diverge markedly from current standards. The ultimate goal is to build a research literature that reflects advances in genetics, other areas of neuroscience, and behavioral science to provide a foundation for precision diagnosis and treatment of mental disorders.
Research applications for the RDoC project are evaluated in the usual NIMH manner – through committees that conduct peer review and give high scores to the applications deemed most meritorious. To date, NIMH has relied upon a combination of funding set-asides and investigator-initiated applications to support RDoC research.
The development and overall organization of the RDoC project has been reviewed thoroughly elsewhere (8,9) and will not be covered in detail here. In brief, an NIMH workgroup was convened in early 2009 to devise an approach for the new system. The workgroup determined that five major domains of functioning would serve as an organizing rubric for subsuming the various dimensions. The five domains are: negative valence systems (i.e., those that respond to aversive situations), positive valence systems, cognitive systems, systems for social processes, and arousal/regulatory systems. A workshop was held for each of these five domains with representative experts from basic and translational areas. Each workshop accomplished three tasks on the basis of available basic and clinical literatures: a) determine the dimensions to be included in the domain, starting with a list of candidates nominated by the NIMH workgroup; b) provide a definition for each dimension; and c) for each dimension, specify various elements (as supported by relevant data) that could be used to characterize the dimension at each of several Units of Analysis (see below). Dimensions were included in the matrix if the workshop members deemed that they met two stringent criteria: a) there had to be evidence for the dimension as a validated behavioral function, and b) there had to be evidence for a neural circuit or system that plays a preponderant role in implementing the function.
STRUCTURE OF THE RDoC MATRIX
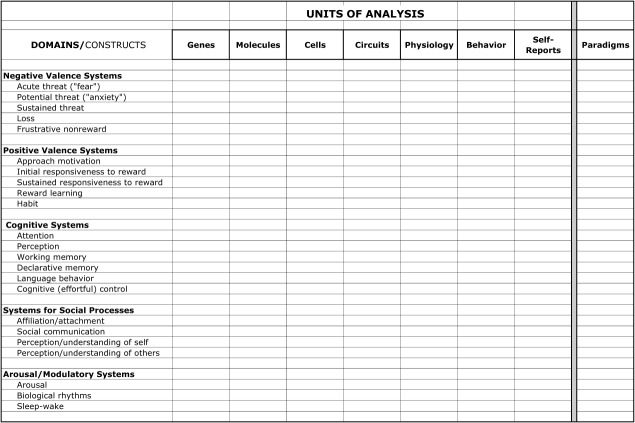
The major elements of this organizational scheme can be represented as a two-dimensional matrix (Figure 1, see also http://www.nimh.nih.gov/research-priorities/rdoc/index.shtml). The various dimensions referred to above appear in the rows of this matrix. They are formally termed “constructs” to denote their status as non-computable concepts based on convergent sets of data, whose precise functional significance changes as increasing amounts of data are compiled to inform our understanding (see 5). The constructs are grouped within the superordinate domains (the “Research Domains”) as noted above, reflecting significant relationships among constructs within each domain besides providing a heuristic organizing scheme.
Figure 1.
Research Domain Criteria matrix
The seven columns of the matrix represent various classes of measurement that could be used to assess each construct, and are termed “Units of Analysis” (there is also a column to represent various paradigms used to assess the construct). As noted above, entries for each cell – as defined by the intersection of a row (dimension) and a column (Unit of Analysis) – were nominated and vetted by the workshop participants. The center column refers to measurement of particular brain circuits; the three columns to its left denote respectively the genes, molecules, and cells that comprise circuits, while the columns to the right can be thought of as various circuit outputs (behavior, physiological responses, and verbal reports or clinician-completed instruments). The latter three columns include measures that could be used to assess signs and symptoms from various self-report or interviewer-based instruments.
The matrix includes two other dimensions that are critical to the RDoC goal, and should be considered integral parts of the structure. These two dimensions, often interacting strongly, comprise developmental trajectories and environmental effects (broadly considered). Most mental illnesses are now viewed as neurodevelopmental disorders, and maturation of the nervous system interacts with a wide variety of external influences beginning at conception. There has been considerable research on multiple risk factors, in such disparate areas as prenatal infections and early life abuse/neglect, that can constitute risk for later disorders. However, the current diagnostic systems do not necessarily promote an integrative account of developmental patterns that may differentially lead to resilience or to disorders, nor a precise understanding of why a particular insult may lead to different disorders (e.g., that early life stress represents a risk variously for depression, post-traumatic stress disorder (PTSD), or borderline personality disorder). A major goal of RDoC is to focus research on relevant systems to document the unfolding of trajectories as they interact with various events – not only in childhood, but across the life span.
Some writers have commented that RDoC embodies a reductionistic approach that is exclusively focused on genetics and biomarkers to the exclusion of social influences (e.g., 10). In fact, as some astute commentators have observed (e.g., 11), this is not the case. There is a strong emphasis on developing a more mechanistic understanding of how such factors as life events and the social environment interact with development to produce a range of observed outcomes.
As mentioned above, RDoC is a framework that is designed and intended to both foster and accommodate new research findings on a continual basis. How is this envisioned, given the current structure of the matrix? The constructs should be regarded as particularly promising dimensions that could be studied within the overall experimental scheme, as vetted by workshop participants for their potential applicability to various clinical problems. So, the current constructs serve both as particularly good candidates for investigators wishing to conduct RDoC-themed research, and as examples for researchers interested in conducting studies to validate a new construct. The RDoC workgroup is committed to updating the matrix periodically, but this is not actually necessary, because investigators are always free to submit grant applications for new constructs (or revisions of the current constructs). As always, the merit of these new ideas is evaluated through the NIMH/National Institutes of Health (NIH) peer review system.
MAJOR POSTULATES OF RDoC
RDoC adopts very different perspectives compared to traditional systems in considering psychopathology. As some of the implications are nuanced and subtle, additional elaboration will be useful regarding its workings.
One of the controversies surrounding the DSM-5 has revolved around the issue of whether disorders may be considered as qualitatively different from normality (e.g., 12) or fall along a continuum with no sharp distinction between normal functioning and disorder (e.g., 13). Resolution of this ongoing debate would obviously be informed by data regarding the overall distribution of “normal” with respect to adaptive, mildly impaired, and severely impaired functioning. Unfortunately, historically there has been little consensus about the domains of normal functioning in cognitive and emotional spheres, or how to measure them. However, over the last few decades, as a result of increasingly advanced technologies for structural and functional analyses of brain circuits, and equally increasing sophistication of behavioral measurements, the major systems of the brain have been delineated and related to their functional outputs. Comparative research has implicitly mitigated the views of human exceptionalism that supported problematic mind-brain dichotomies, and demonstrated the surprising conservation of genes, neurotransmitters, and behavioral functions across evolution – even in model animals such as fruit flies and zebrafish, let alone mammalian species such as rodents and primates (14).
To give just three examples: a) the crude “reward system” identified by Olds and Milner (15) has given way to the increasingly sophisticated explication of dorsal and ventral striatum and the associated differentiation of functions for experiencing reward, seeking reward, learning contingencies for reward, and developing habits (e.g., 16,17); b) responses to acute threat and potential threat have been distinguished behaviorally and related to distinguishable circuits along with components that dynamically regulate these responses (18,19); and c) systems that implement the cognitive operations of working memory first posited on the basis of behavioral studies in the late 1960s and 1970s have been reliably characterized (20,21). Importantly, many paradigms have been developed that can provide measures both of behavioral performance and of related functional brain activity in a large population, thus providing some sense of the normal distribution of behavior; obviously, this capability, in turn, permits a quantitative specification of the extent to which various aspects of functioning deviate from normality. Importantly, these new developments are not confined only to laboratory tasks, but also to psychometrically-derived inventories that relate strongly to real-world functioning (e.g., 22).
In terms of the RDoC system, several consequences ensue from these developments. First, RDoC adopts a translational approach to disorders, construing (for these experimental purposes) pathology in terms of deviations in fundamental functional systems. While translational research has become almost a cliché in contemporary research, RDoC marks a subtle but significant shift in direction for psychiatry. The standard approach to psychiatric illness has been to define a mental disorder (on the basis of signs and symptoms) and then seek a pathophysiology relating to those symptoms. In contrast, RDoC asks the following questions: “What is the normal distribution for a certain trait or characteristic; what is the brain system that primarily implements this function; and, how can we understand, at various levels of mechanism (23), what accounts for the development of dysregulation or dysfunction in these systems along normal-to-abnormal dimensions?”. This strategy has obvious advantages in terms of applying basic research at all levels of analysis to clinical problems, as the translation is relatively straightforward. On the other hand, it may be more difficult for clinical researchers, since the symptoms that they are accustomed to study literally do not appear in the RDoC matrix. A further implication of the translational approach is that RDoC is agnostic to current disorder categories. There is no claim to “understand” or “explain” DSM/ICD disorders in terms of these functions; rather, the aim is more simply to seek an understanding of how these various systems may become dysregulated to various extents and to relate such dysregulation to relevant symptoms.
On a related point, RDoC incorporates a dimensional approach to psychopathology, inherently examining, to quote the NIMH Strategic Plan for RDoC, “the full range of variation, from normal to abnormal, among the fundamental components [dimensions] to improve understanding of what is typical versus pathological”. In fact, the framework intentionally omits any disease definitions, disorder thresholds, or cutpoints for various levels of psychopathology. Because such boundaries can bias the way research is conducted (particularly given the inertia of ICD/DSM-determined disorder categories), the aim is simply to gather data about the dimensions that will support future decisions in this regard, made on the basis of quantitative data rather than clinical consensus. Further, the availability of reliable and valid quantitative measurements could permit adjustments over time consequent to epidemiological studies of risk and outcome, as has happened frequently over the years in such areas as hypertension (24).
One important point in this regard is that there is no assumption that the relationships between various measures of a particular construct are linear, as might be presumed under a simple severity model. Indeed, the search for points of disjunction and non-linear functions is a major reason for a purely empirical approach. One instance of this phenomenon is the classic inverted U-shaped curve relating arousal and performance (25). In another intriguing study, Tucker et al (26) recorded a cortical event-related potential termed the error-related negativity (ERN), which in this case demonstrated a larger response when the subject was given feedback regarding task-related errors. As predicted, patients with depression showed larger ERNs than controls; however, the unexpected finding was a quadratic relationship with depression severity, such that the large ERNs were seen only in patients with moderate (but not mild or severe) depression scores.
Some observers might object that this translational emphasis over-simplifies the richness of psychopathology, or that complex psychiatric symptoms are not yet ready to be explained in such a direct translational manner. For instance, one hears informal comments at conferences that psychosis is a “black box” in RDoC. The rejoinder to this view holds that, if the field is ever to establish a diagnostic system based upon neuroscience, sooner or later it will be essential to explain complex symptoms in terms of dysregulation in basic brain operations (as exemplified in the quotations above). For instance, hallucinations might be broached in part via a consideration of systems that represent the integration of perceptual information (27), while networks that mediate functions involved with language, working memory, declarative memory, and learning would appear to be promising avenues for the study of delusions (28). The growing realization that some degrees of psychotic phenomena are present in the normal population (29), and also in broad ranges of psychiatric outpatients (30), is consistent with a view of these symptoms as dimensionally arrayed in the population and not simply a manifestation of qualitatively distinct severe pathology. Thus, an essential component of an experimental classification system involves challenging investigators to depart from traditional ways of thinking about disorders in order to seek promising new experimental ideas.
Another issue concerns the relationship of the various RDoC measures to presenting signs and symptoms, since of course the latter are the actual clinical phenomena that bring patients to the clinic. Establishing mechanistic relationships by which disruptions in the functioning of one or more constructs (as assessed by various Units of Analysis) result in specified symptoms or impairments is considered as a central task for the RDoC project, and a major component of the grant funding program. Notwithstanding the translational research approach, the RDoC project is very much directed toward an understanding of the impairments that patients experience in their lives, and this desideratum was emphasized by the RDoC workgroup in nominating constructs.
The concern about the current diagnostic environment has not been so much with the symptoms themselves, as with the way in which they are clustered into disorders in the polythetic DSM system. Particularly in research and in treatment development (where the diagnostic category is pre-eminent as an independent variable or treatment indication, respectively), the polythetic algorithms serve to de-emphasize individual symptoms because they are important only insofar as they contribute to diagnosis. Thus, a strong RDoC research project will focus upon a specific clinical problem that can be better explicated through a research design that combines appropriate Units of Analysis to illuminate the mechanisms of dysfunction.
TRANSITIONING FROM ICD/DSM TO RDoC
What would a prototypical RDoC design look like? Such an experiment would include subjects with a wide range of normal-to-impaired functioning with respect to the dimensional construct(s) of interest. While many studies would employ enriched sampling of subjects who evince levels of impairment consistent with current diagnostic criteria, the focus would be exclusively on the RDoC constructs without recourse to ICD/DSM diagnoses in the design. (It is acknowledged that, for the foreseeable future, these diagnoses will be needed for medical records and insurance purposes). At the extreme, for example, samples for a study of reward circuit activity (as relevant to anhedonia and/or mania) might be drawn from virtually the entire population of treatment-seeking adults – mood/anxiety spectrum, psychotic spectrum, eating disorders, personality disorders; for appropriate exploration of dimensionality, the sample would also include relatively minor psychopathology such as an adjustment reaction diagnosis as well as those individuals who do not meet criteria for any diagnosis. A similar approach might be used to study executive function in children across a range of autism spectrum, attention-deficit/hyperactivity disorder, and mood/anxiety disorders (and once again, those who do not meet criteria for any disorder).
There are two highly important caveats that are necessary to place this sort of design in context. First, there are the obvious considerations for appropriate inclusion and exclusion criteria. The usual exclusions for neurological conditions or injuries, intellectual disability, extensive substance abuse in adults, etc. would still apply; on the other hand, one tactic for exploring dimensionality is to broaden the inclusion criteria for control subjects by permitting more prior or current psychopathology. For both adults and children, it is also critical to account for normative developmental stages (e.g., cognitive and physical development in children, cognitive slowing in later life), given the emphasis on normative measurement. Second, studies of this type may be more informative when they build upon a prior basis of research with the relevant constructs and research designs; for example, studies that have established consistent results for an anhedonia dimension across the mood/anxiety spectrum will have a much firmer foundation for extension to psychotic and other disorders.
Designs such as those above (vastly oversimplified here for brevity) may be considered the “gold standard” in terms of RDoC's instantiation of the corresponding goal in the NIMH Strategic Plan. Accordingly, a critical aspect of the RDoC program is helping researchers make the transition – both conceptually and practically – from the ICD/DSM to a dimensional outlook. This has been a matter of ongoing concern for the NIMH workgroup, as the DSM/ICD system has been used for so long in research and clinical practice that some transition is needed to consider psychopathology from other perspectives. These issues would depend not only on becoming accustomed to the significance of new scale values (e.g., for anhedonia or working memory), but also on achieving a “mental model” for patients seen through the RDoC lens. The same psychopathology would be present, of course, but conceived and measured in distinct ways.
The general approach to this transition would incorporate various combinations of RDoC constructs and DSM/ICD disorder categories in experiments. While these steps may be useful in transition, there are potential drawbacks as well. One problem is the temptation for the disorder categories to remain privileged with respect to the dimensions: investigators might continue to regard the diagnostic thresholds as demarcation points for ill versus well, and also continue viewing pathology through the DSM/ICD lens rather than acclimating to the idea of neural systems-based functional constructs. There is also the obvious potential bias in sampling mostly patients who meet current diagnostic criteria, in treatment-seeking samples or with other recruiting strategies, thus short-circuiting dimensional exploration. In short, these transitional steps pose the risk that investigators will continue to regard their patients – both clinically and in terms of research designs – in familiar DSM terms, failing to grow a sufficient appreciation of the precision-medicine zeitgeist that RDoC is intended to facilitate. For these reasons, transitional research designs are best regarded as temporary heuristics for a limited number of studies if the full potential of the RDoC framework is to be reached.
With these caveats in mind, there are two broad approaches that investigators might use for transitional designs. The first would be studies that explore RDoC dimensions within multiple diagnostic groups. The simplest form of this type would specify in the design two or three distinct DSM disorders, each recruited for a sufficient N to achieve acceptable statistical power. The analysis could then be conducted in terms of the DSM factor, the RDoC dimension, and the interaction. Where the N's are too small to permit an interaction design, the numbers might at least be large enough to conduct tests of the separate main effects of the DSM factor and the RDoC dimension(s). Important additions to these designs would include subjects that contribute to exploring a broad range of the dimensions under study. As mentioned above, control groups with liberal inclusion criteria would be important; others could include treatment-seeking individuals who just fail to meet criteria for a DSM diagnosis (as by coming up one symptom short in the polythetic list, or forme fruste), or patients with not otherwise specified (NOS) diagnoses. As with all DSM-based studies, this type of design suffers from the problem of how to accommodate and analyze varying numbers and patterns of co-morbid DSM diagnoses – a continuing obstacle that has been a major rationale for the RDoC approach.
An alternative approach, somewhat more compatible with an RDoC design, would be to include subjects from all diagnostic groups in one of the chapters of the new “metastructure” crafted largely in common between DSM-5 and the upcoming ICD-11, without targeting a specific N for each category. These chapters generally include a number of disorders varying in severity – for instance, the Schizophrenia Spectrum chapter contains schizotypal disorder, schizophreniform disorder, brief delusional disorder, etc. As above, inclusion of subjects with subsyndromal pathology or unaffected relatives, in addition to control groups as described above, would contribute to the dimensional objectives. As an added benefit, inclusion of these more varied groups represents potentially a significant contribution to public health, in that these are patients with palpable impairments who are typically excluded from most pathophysiology and treatment studies due to their failure to fit one of the modal diagnoses. To our knowledge, there are no good estimates of the percentage of patients in these shadow groups, nor estimates of the magnitude of the public health significance posed by their symptoms and impairment. Finally, a number of studies have demonstrated palpable impairments on various laboratory tasks in clinically unaffected relatives of probands (e.g., 31). While such studies have been used to demonstrate heritable risk, there has been insufficient attention to date on how such results could inform the actual pathophysiological differences that (as quoted above) “improve understanding of what is typical versus pathological”.
A broader version of this alternative sampling strategy would involve subjects with primary diagnoses from different chapters of the ICD/DSM metastructure, again without constraining the subjects to two or three specified categories. Such groups might initially include disorders of somewhat comparable psychopathology, e.g., schizophrenia spectrum/bipolar spectrum or unipolar mood/anxiety disorders. The goal, however, would not be to distinguish particular groups as is typically done, but rather to explore the underlying dimension(s) so as to gain a more comprehensive understanding of the pathological mechanisms. In this regard, for instance, Craddock and Owen (32) posited a gradient of neurodevelopmental pathology, ranging in a continuous fashion that begins with intellectual disability and progresses through autism, schizophrenia, schizoaffective disorder, bipolar disorder, and unipolar depression. Each disorder is seen not as a unitary disease entity, but rather as a particular range within the overall gradient. (It is worth noting that, if one selects subjects from two adjacent ranges of a larger gradient, a statistically significant result is virtually guaranteed; it is clearly highly misleading, at best, to conclude that these represent two qualitatively distinct disease entities).
The second broad type of transitional designs might simply employ a single ICD/DSM group in the usual fashion. However, the investigators would propose analyses of various dimensions within the group that might provide more information about subtypes or ranges along relevant dimensions than data from symptom-based efforts (e.g., the modest success for understanding or treating vegetative signs or atypical depression within the overall category of unipolar depression). In most cases, this type of design will have less potential relative to the ultimate goals of the RDoC scheme, because it cannot contribute to an understanding of specified constructs or mechanisms that could represent cross-cutting diagnostic criteria in future nosologies. However, this approach may represent a useful way for investigators with research programs directed toward a single ICD/DSM disorder to initiate the transition toward studying RDoC dimensions. To repeat a point made earlier, one component of such studies (as with any RDoC design) might profitably explore developmental trajectories so as to understand how individual differences in neuroplasticity over time contribute to heterogeneity in presenting symptomatology and activity in relevant systems.
RDoC AND TREATMENT DEVELOPMENT
While the above steps have been oriented toward psychopathology, there are relatively near-term possibilities for using RDoC concepts in treatment as well. The common element for any treatment trial in RDoC will require the development of a valid set of measures that can reliably distinguish a particular subtype, or critical location along a dimension, to predict successful treatment outcomes. As one example, given the well-known heterogeneity of ICD/DSM categories, establishing mechanistically-based subtypes of current disorders may enhance matching of patients to treatments. For instance, PTSD is often regarded as a prototypical “fear circuit” disorder. However, many patients with PTSD show a blunted affective response to affective challenges (33), which may relate to multiple traumas and/or a chronic course (34). Accordingly, classic exposure therapies for PTSD might be predicted to be effective only for highly fear-reactive patients (where the fear can be extinguished), while different therapies may be indicated for those with a blunted response pattern. Appropriate assessments for measuring the fear response in a reliable, idiographic manner, for which there are multiple potential candidates but no validated methods, would permit a test of this hypothesis – which appears to hold for other anxiety disorders as well (34).
Similarly, development of new treatments may be facilitated by the identification of more homogeneous subgroups of patients. As a group of industry scientists noted, “by increasing the mechanistic understanding of disease and matching the right treatments to the right patients, one could move from one-size-fits-all to targeted therapy and increase the benefit-risk ratio for patients” (35). In other words, new treatments that target a mechanism associated with one particular symptom may have a low probability of success in a trial for a DSM/ICD indication, because the particular symptom is not shared by all patients with the diagnosis. By contrast, an exemplary research topic in RDoC might involve an enhanced understanding of how various aspects of reward-related systems relate to clinical anhedonia (a symptom of depression which itself may be a multi-faceted clinical construct). If a new anhedonia treatment were developed that targets a novel mechanism based upon such research advances, the prediction would be that the treatment has therapeutic effects only for those depressed patients with anhedonia, but should be efficacious for patients with other diagnoses who have measurable anhedonia. Once again, “measurable anhedonia” is a key phrase that necessitates prior validation of widely-accepted procedures for this type of trial.
CONCLUSIONS
As noted at the outset, RDoC is a long-term funding project designed to inform future versions of classification systems. The goal is for research conducted under the aegis of RDoC to make a definitive contribution toward precision medicine in psychiatry, through identification of relationships among aberrations in fundamental neural systems and functional impairments – and notably including an emphasis upon neurodevelopmental trajectories and environmental factors.
Perhaps the most important point about RDoC is that its essence is to provide a broad framework for conducting research on mental disorders from a wholly new perspective. In this sense, what is most important about RDoC is not the list of constructs and the matrix per se – although thousands of person-hours have been devoted to crafting the overall organization and its specific elements – but the idea of freeing up investigators to pursue exciting translational research questions driven by neuroscience and behavioral science rather than by constraining sets of symptom clusters.
The main notion of the RDoC matrix is to provide guidance to investigators in how they might set about taking the first steps down the long and arduous road that must be traversed to reach a point when neuroscience-based nosologies are possible (and intermediate research designs such as the steps discussed above reflect the fact that some period of transition is to be expected). Perhaps the outcomes for RDoC might be assessed by the number of research programs that, freed from the strictures of current diagnostic guidelines, outstrip the RDoC matrix to move in entirely new directions that transcend the organization of the current system. Such a result would be a testament to the imagination and scientific prowess of the clinical research community, which will play the largest role in how research conducted in the spirit of the RDoC approach contributes to progress in understanding and treating mental disorders in the years ahead.
References
- 1.Insel TR. Transforming diagnosis http://www.nimh.nih.gov.
- 2.Insel TR, Lieberman JA. DSM-5 and RDoC: shared interests http://www.nimh.nih.gov.
- 3.Belluck P, Carey B. Psychiatry's guide is out of touch with science, experts say. New York: Times; 2013. May 6 http://www.nytimes.com. [Google Scholar]
- 4.Wakefield JC. Are you as smart as a 4th grader? Why the prototype-similarity approach to diagnosis is a step backward for a scientific psychiatry. World Psychiatry. 2012;11:27–8. doi: 10.1016/j.wpsyc.2012.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith GT, McCarthy DM, Zapolski TCB. On the value of homogeneous constructs for construct validation, theory testing, and the description of psychopathology. Psychol Assess. 2009;21:272–84. doi: 10.1037/a0016699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keshavan MS, Nasrallah HA, Tandon R. Schizophrenia, “Just the facts” 6. Moving ahead with the schizophrenia concept: from the elephant to the mouse. Schizophr Res. 2011;127:3–13. doi: 10.1016/j.schres.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kapur S, Phillips AG, Insel TR. Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it? Mol Psychiatry. 2012;17:1174–9. doi: 10.1038/mp.2012.105. [DOI] [PubMed] [Google Scholar]
- 8.Sanislow CA, Pine DS, Quinn KJ, et al. Developing constructs for psychopathology research: Research Domain Criteria. J Abnorm Psychol. 2010;119:631–9. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- 9.Morris SE, Cuthbert BN. Research Domain Criteria: cognitive systems, neural circuits, and dimensions of behavior. Dialogues Clin Neurosci. 2012;14:29–37. doi: 10.31887/DCNS.2012.14.1/smorris. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McLaren N. Cells, circuits, and syndromes: a critical commentary on the NIMH Research Domain Criteria project. Ethical Hum Psychol Psychiatry. 2011;13:229–36. [Google Scholar]
- 11.Bolton D. Should mental disorders be regarded as brain disorders? 21st century mental health sciences and implications for research and training. World Psychiatry. 2013;12:24–5. doi: 10.1002/wps.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wakefield JC. The perils of dimensionalization: challenges in distinguishing negative traits from personality disorders. Psychiatr Clin North Am. 2008;31:379–93. doi: 10.1016/j.psc.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Krueger RF, Eaton NR. Personality traits and the classification of mental disorders: toward a more complete integration in DSM-V and an empirical model of psychopathology. Pers Disord Theory Res Treat. 2010;1:97–118. doi: 10.1037/a0018990. [DOI] [PubMed] [Google Scholar]
- 14.Razafsha M, Behforuzi H, Harati H, et al. An updated overview of animal models in neuropsychiatry. Neuroscience. 2013;240:204–18. doi: 10.1016/j.neuroscience.2013.02.045. [DOI] [PubMed] [Google Scholar]
- 15.Olds J, Milner P. Positive reinforcement produced by electrical stimulation of septal area and other regions of rat brain. J Comp Physiol Psychol. 1954;47:419–27. doi: 10.1037/h0058775. [DOI] [PubMed] [Google Scholar]
- 16.Berridge KC. Food reward: brain substrates of wanting and liking. Neurosci Biobehav. 1995;20:1–25. doi: 10.1016/0149-7634(95)00033-b. [DOI] [PubMed] [Google Scholar]
- 17.Treadway MT, Zald DH. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev. 2011;35:537–55. doi: 10.1016/j.neubiorev.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davis M. Neural systems involved in fear and anxiety measured with fear-potentiated startle. Am Psychol. 2006;61:741–56. doi: 10.1037/0003-066X.61.8.741. [DOI] [PubMed] [Google Scholar]
- 19.Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: a synthetic review and evolving model of the cognitive control of emotion. Ann NY Acad Sci. 2012;1251:E1–24. doi: 10.1111/j.1749-6632.2012.06751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baddeley AD, Hitch G, Bower GH. Recent advances in learning and motivation. Vol. 8. New York: Academic Press; 1974. Working memory; pp. 47–89. Vol. [Google Scholar]
- 21.Barch DM, Smith E. The cognitive neuroscience of working memory: relevance to CNTRICS and schizophrenia. Biol Psychiatry. 2008;64:11–7. doi: 10.1016/j.biopsych.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patrick CJ, Venables NC, Yancey JR, et al. A construct-network approach to bridging diagnostic and physiological domains: application to assessment of externalizing psychopathology. J Abnorm Psychol. 2013;122:902–16. doi: 10.1037/a0032807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bechtel W, Schouton M, de Jong HL. The matter of mind: philosophical essays of psychology, neuroscience, and reduction. Malden: Blackwell; 2007. Reducing psychology while maintaining its autonomy via mechanistic explanations; pp. 172–98. [Google Scholar]
- 24.Kotchen TE. Historical trends and milestones in hypertension research: a model of the process of translational research. Hypertension. 2011;58:522–38. doi: 10.1161/HYPERTENSIONAHA.111.177766. [DOI] [PubMed] [Google Scholar]
- 25.Mattay VS, Goldberg TE, Fera F, et al. Catechol O-methyltransferase val158-met genotype and individual variation in the brain response to amphetamine. Proc Natl Acad Sci USA. 2003;100:6186–91. doi: 10.1073/pnas.0931309100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tucker DM, Luu P, Frishkoss G, et al. Frontolimbic response to negative feedback in clinical depression. J Abnorm Psychol. 2003;112:667–78. doi: 10.1037/0021-843X.112.4.667. [DOI] [PubMed] [Google Scholar]
- 27.Ford JM, Dierks T, Fisher DJ, et al. Neurophysiological studies of auditory verbal hallucinations. Schizophr Bull. 2012;38:715–23. doi: 10.1093/schbul/sbs009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tamminga CA, Stan AD, Wagner AD. The hippocampal formation in schizophrenia. Am J Psychiatry. 2010;167:1178–93. doi: 10.1176/appi.ajp.2010.09081187. [DOI] [PubMed] [Google Scholar]
- 29.Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res. 2002;54:59–65. doi: 10.1016/s0920-9964(01)00352-8. [DOI] [PubMed] [Google Scholar]
- 30.Gaudiano BA, Zimmerman M. Prevalence of attenuated psychotic symptoms and their relationship with DSM-IV diagnoses in a general psychiatric outpatient clinic. J Clin Psychiatry. 2013;74:149–57. doi: 10.4088/JCP.12m07788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Snitz BE, MacDonald AW, III, Carter CS. Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: a meta-analytic review of putative endophenotypes. Schizophr Bull. 2006;32:179–94. doi: 10.1093/schbul/sbi048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Craddock N, Owen MJ. The Kraepelinian dichotomy – going, going… but still not gone. Br J Psychiatry. 2010;196:92–5. doi: 10.1192/bjp.bp.109.073429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lanius R, Bluhm R. A review of neuroimaging studies in PTSD: heterogeneity of response to symptom provocation. J Psychiatr Res. 2006;40:709–29. doi: 10.1016/j.jpsychires.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 34.McTeague LM, Lang PJ. The anxiety spectrum and the reflex physiology of defense: from circumscribed fear to broad distress. Depress Anxiety. 2012;29:264–81. doi: 10.1002/da.21891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wong EH, Yocca F, Smith MA, et al. Challenges and opportunities for drug discovery in psychiatric disorders: the drug hunters' perspective. Int J Neuropsychopharmacol. 2010;13:1269–84. doi: 10.1017/S1461145710000866. [DOI] [PubMed] [Google Scholar]