Abstract
We conducted a meta-analysis of randomized trials in which the effects of treatment with antidepressant medication were compared to the effects of combined pharmacotherapy and psychotherapy in adults with a diagnosed depressive or anxiety disorder. A total of 52 studies (with 3,623 patients) met inclusion criteria, 32 on depressive disorders and 21 on anxiety disorders (one on both depressive and anxiety disorders). The overall difference between pharmacotherapy and combined treatment was Hedges' g = 0.43 (95% CI: 0.31-0.56), indicating a moderately large effect and clinically meaningful difference in favor of combined treatment, which corresponds to a number needed to treat (NNT) of 4.20. There was sufficient evidence that combined treatment is superior for major depression, panic disorder, and obsessive-compulsive disorder (OCD). The effects of combined treatment compared with placebo only were about twice as large as those of pharmacotherapy compared with placebo only, underscoring the clinical advantage of combined treatment. The results also suggest that the effects of pharmacotherapy and those of psychotherapy are largely independent from each other, with both contributing about equally to the effects of combined treatment. We conclude that combined treatment appears to be more effective than treatment with antidepressant medication alone in major depression, panic disorder, and OCD. These effects remain strong and significant up to two years after treatment. Monotherapy with psychotropic medication may not constitute optimal care for common mental disorders.
Keywords: Combined treatment, psychotherapy, antidepressant medication, depressive disorders, anxiety disorders, dysthymia, obsessive-compulsive disorder, meta-analysis
Anxiety and depressive disorders are highly prevalent 1,2 and are associated with a substantial loss of quality of life for patients and their relatives 3,4, high levels of service use, substantial economic costs 5–7, and a considerable disease burden for public health 8. Effective treatments are available for these disorders, including several types of psychotherapy and antidepressant medication 9–11. Although psychotherapy and antidepressants are about equally effective for most anxiety and depressive disorders 12, there is some evidence that combined treatments may be more effective than each of these treatment alone 13–15. At the same time, however, an increasing proportion of patients with mental disorders in the past decade have received psychotropic medication without psychotherapy 16,17. It is important, therefore, to examine whether this has negative effects on the quality of care.
We conducted a meta-analysis of studies comparing pharmacotherapy alone with combined psychotherapy and pharmacotherapy. Although some earlier meta-analyses have examined this question, these were all aimed at one disorder, especially depression 13–15 and panic 18,19. For some other disorders – e.g., social anxiety disorder (SAD) and obsessive-compulsive disorder (OCD) – several primary studies have been conducted, but these have not yet been integrated into meta-analyses. The main goal of this paper, therefore, is to provide an overall meta-analysis of studies comparing antidepressant medication with combined treatment for anxiety and depressive disorders. We also examined whether differences between combined treatment and placebo only were larger than those between combined treatment and pharmacotherapy, in order to determine the relative contribution of psychotherapy and pharmacotherapy to the effects of combined treatments.
METHODS
Identification and selection of studies
We used several strategies to identify relevant studies. We searched four major bibliographical databases (PubMed, PsycInfo, Embase and the Cochrane database of randomized trials). We first developed a search string for psychotherapy with text and key words indicating the different types of psychotherapy and psychological treatments. This search string was combined with search strings indicating each of the disorders we included: major depression; dysthymia; generalized anxiety disorder (GAD); SAD; panic disorder; OCD; post-traumatic stress disorder (PTSD). We limited our search to randomized controlled trials. We also checked the references of 116 earlier meta-analyses of psychological treatments of the disorders (Figure 1).
Figure 1.
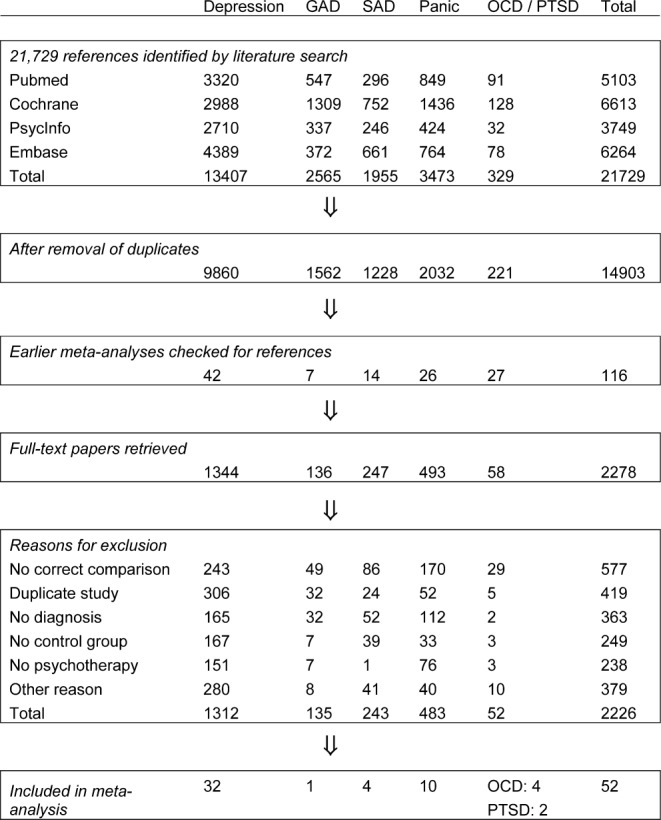
Selection and inclusion of studies. GAD – generalized anxiety disorder, OCD – obsessive-compulsive disorder, PTSD – post-traumatic stress disorder, SAD – social anxiety disorder
We included randomized trials in which the effects of treatment with antidepressant medication were compared to the effects of a combined antidepressant medication and psychological treatment in adults with a depressive disorder, panic with or without agoraphobia, GAD, SAD, OCD or PTSD. Only studies in which subjects met diagnostic criteria for the disorder according to a diagnostic interview – such as the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I), the Composite International Diagnostic Interview (CIDI), or the Mini-International Neuropsychiatric Interview (MINI) – were included. Studies on inpatients, adolescents and children (below 18 years of age) were excluded. We also excluded maintenance studies, aimed at people who had already recovered or partly recovered after an earlier treatment. Studies in English, German, Spanish, and Dutch were considered for inclusion.
Quality assessment and data extraction
We assessed the validity of included studies using the “Risk of bias” assessment tool, developed by the Cochrane Collaboration 20. This tool assesses possible sources of bias in randomized trials, including the adequate generation of allocation sequence; the concealment of allocation to conditions; the prevention of knowledge of the allocated intervention (masking of assessors); and dealing with incomplete outcome data (this was assessed as positive when intention-to-treat analyses were conducted, meaning that all randomized patients were included in the analyses). Assessment of the validity of included studies was conducted by two independent researchers, and disagreements were solved through discussion.
We also coded participant characteristics (disorder; recruitment method; target group); type of antidepressant that was used (selective serotonin reuptake inhibitor, SSRI; tricyclic antidepressant, TCA; serotonin-norepinephrine reuptake inhibitor, SNRI; monoamine oxidase inhibitor, MAOI; other or manualized treatment including several antidepressants); and characteristics of the psychotherapies (format; number of sessions; and type of psychotherapy). The types of psychotherapy we distinguished were cognitive behavior therapy (CBT), interpersonal psychotherapy (IPT), and others. Because most CBT therapies used a mix of different techniques, we clustered them together in one large family of CBT treatments. We rated a therapy as CBT when it included cognitive restructuring or a behavioral approach (such as exposure and response prevention). When a therapy used a mix of CBT and IPT, we rated it as “other”, along with other therapeutic approaches (such as psychodynamic therapies).
Meta-analyses
For each comparison between a pharmacotherapy and the combined treatment group, the effect size indicating the difference between the two groups at post-test was calculated (Hedges' g). Effect sizes were calculated by subtracting (at post-test) the average score of the pharmacotherapy group from the average score of the combined treatment group, and dividing the result by the pooled standard deviation. Because some studies had relatively small sample sizes, we corrected the effect size for small sample bias 21.
In the calculations of effect sizes in studies aimed at patients with depressive disorders, we used only those instruments that explicitly measured symptoms of depression. In studies examining anxiety disorders, we used only instruments that explicitly measured symptoms of anxiety. If more than one measure was used, the mean of the effect sizes was calculated, so that each study provided only one effect size. If means and standard deviations were not reported, we used the procedures of the Comprehensive Meta-Analysis software (version 2.2.021) to calculate the effect size using dichotomous outcomes; and if these were not available either, we used other statistics (such a t-value or p-value). To calculate pooled mean effect sizes, we used the above-mentioned software. Because we expected considerable heterogeneity among the studies, we employed a random effects pooling model.
Because the standardized mean difference (Hedges' g) is not easy to interpret from a clinical perspective, we transformed these values into the number needed to treat (NNT), using the formulae provided by Kraemer and Kupfer 22. The NNT indicates the number of patients that have to be treated in order to generate one additional positive outcome 23.
We also calculated the relative risk (RR) of dropping out from treatment in pharmacotherapy compared with combined treatment. To compare the long-term effects of the two treatments, we calculated the RR of having a positive outcome at follow-up.
As a test of homogeneity of effect sizes, we calculated the I2 statistic, which is an indicator of heterogeneity in percentages. A value of 0% indicates no observed heterogeneity, and larger values indicate increasing heterogeneity, with 25% as low, 50% as moderate, and 75% as high heterogeneity 24. We calculated 95% confidence intervals around I2 25, using the non-central chi-squared-based approach within the Heterogi module for Stata 26.
We conducted subgroup analyses according to the mixed effects model, in which studies within subgroups are pooled with the random effects model, while tests for significant differences between subgroups are conducted with the fixed effects model. For continuous variables, we used meta-regression analyses to test whether there was a significant relationship between the continuous variable and the effect size, as indicated by a Z-value and an associated p-value.
We tested publication bias by inspecting the funnel plot on primary outcome measures and by Duval and Tweedie's trim and fill procedure 27, which yields an estimate of the effect size after the publication bias has been taken into account. We also conducted Egger's test of the intercept to quantify the bias captured by the funnel plot and test whether it was significant.
RESULTS
Selection and inclusion of studies
After examining a total of 21,729 abstracts (14,903 after removal of duplicates), we retrieved 2,278 full-text papers for further consideration. We excluded 2,226 of the retrieved papers. The flow chart describing the inclusion process, including the reasons for exclusion, is presented in Figure 1. A total of 52 studies met inclusion criteria for this meta-analysis 28–79. Selected characteristics of the included studies are reported in Table1.
Table 1.
Selected characteristics of studies comparing treatment with antidepressant medication to combined treatment with psychotherapy and medication
| Study | Disorder | Psychotherapy | Medication | Ncom | Nmed | Quality* | Country |
|---|---|---|---|---|---|---|---|
| Azhar 28 | PAN | CBT | SSRI | 17 | 17 | − − − − | Other |
| Barlow et al 29 | PAN | CBT | TCA | 65 | 83 | − − + + | USA |
| Bellack et al 30 | Mood | Other | TCA | 17 | 18 | − − + − | USA |
| Bellino et al 31 | MDD | IPT | SSRI | 16 | 16 | − − + − | Europe |
| Berger et al 32 | PAN | Other | SSRI | 35 | 38 | − − − − | Europe |
| Blackburn et al 33 | MDD | CBT | TCA | 22 | 20 | − − − − | USA |
| Blanco et al 34 | SAD | CBT | MAOI | 32 | 35 | + + + + | USA |
| Blom et al 35 | MDD | IPT | SNRI | 33 | 30 | − − + + | Europe |
| Blomhoff et al 36 | SAD | BT | SSRI | 98 | 95 | + + + + | Europe |
| Browne et al 37 | DYS | IPT | SSRI | 122 | 117 | + + + − | Canada |
| Burnand et al 38 | MDD | DYN | TCA | 33 | 38 | − − + − | Europe |
| Crits-Christoph et al 39 | GAD | CBT | SNRI | 17 | 24 | − − + − | USA |
| Davidson et al 40 | SAD | CBT | SSRI | 42 | 39 | + + + + | USA |
| De Jonghe et al 41 | MDD | DYN | Prot/Other | 83 | 84 | − − + + | Europe |
| De Mello et al 42 | DYS | IPT | MAOI | 11 | 13 | − − + − | Other |
| Dozois et al 43 | MDD | CBT | Prot/Other | 21 | 21 | − + − − | Canada |
| Finkenzeller et al 44 | MDD | IPT | SSRI | 23 | 24 | + − + + | Europe |
| Foa et al 45 | OCD | BT | TCA | 19 | 27 | − − + − | USA |
| Hautzinger et al 46 | Mood | CBT | TCA | 32 | 24 | − − + + | Europe |
| Hellerstein et al 47 | DYS | Other | SSRI | 18 | 17 | − − − + | USA |
| Hollon et al 48 | MDD | CBT | TCA | 25 | 57 | − − + + | USA |
| Hsiao et al 49 | MDD | Other | Prot/Other | 24 | 26 | + − + + | Other |
| Keller et al 50 | MDD | Other | SNRI | 226 | 220 | + + + + | USA |
| King et al 51 | PAN | CBT | Prot/Other | 25 | 25 | − + + − | Other |
| Koszycki et al 52 | PAN | CBT | SSRI | 59 | 62 | + + + + | Canada |
| Lesperance et al 53 | MDD | IPT | SSRI | 67 | 75 | + + + + | Canada |
| Loerch et al 54 | PAN | CBT | MAOI | 14 | 16 | − − + + | Europe |
| Lynch et al 55 | MDD | Other | Prot/Other | 15 | 16 | − − − − | USA |
| Macaskill & Macaskill 56 | MDD | CBT | TCA | 9 | 9 | − − − − | Europe |
| Maina et al 57 | MDD, OCD | DYN | SSRI | 25 | 29 | + + + + | Europe |
| Markowitz et al 58 | DYS | IPT | SSRI | 21 | 24 | + + + + | USA |
| Misri et al 59 | Mood | CBT | SSRI | 19 | 16 | + − + + | Canada |
| Mitchell et al 60 | Mood | Other | Prot/Other | 45 | 53 | + + + + | USA |
| Murphy et al 61 | MDD | CBT | TCA | 22 | 24 | + + − + | USA |
| Mynors-Wallis et al 62 | MDD | PST | SSRI | 35 | 36 | + + + + | Europe |
| Naeem et al 63 | MDD | CBT | SSRI | 17 | 17 | + + + + | Other |
| Otto et al 64 | PTSD | CBT | SSRI | 5 | 5 | − − − − | USA |
| Prasko et al 65 | SAD | CBT | MAOI | 22 | 20 | − − + − | Europe |
| Ravindran et al 66 | DYS | CBT | SSRI | 24 | 22 | + + + − | Canada |
| Reynolds et al 67 | MDD | IPT | TCA | 16 | 25 | − − + + | USA |
| Rothbaum et al 68 | PTSD | BT | SSRI | 34 | 31 | − − + + | USA |
| Shamsaei et al 69 | MDD | CBT | SSRI | 40 | 40 | + − + − | Other |
| Shareh et al 70 | OCD | CBT | SSRI | 6 | 6 | − − − − | Other |
| Sharp et al 71 | PAN | CBT | SSRI | 29 | 29 | − − − − | Europe |
| Sirey et al 72 | MDD | Other | Prot/Other | 21 | 24 | − − + + | USA |
| Spinhoven et al 73 | PAN | CBT | SSRI | 20 | 19 | − − − + | Europe |
| Tenneij et al 74 | OCD | BT | Prot/Other | 34 | 46 | − − + + | Europe |
| Thompson et al 75 | MDD | CBT | TCA | 36 | 33 | − − − + | USA |
| van Apeldoorn et al 76 | PAN | CBT | Prot/Other | 36 | 37 | + + + + | Europe |
| Weissman et al 77 | MDD | IPT | TCA | 23 | 20 | − − + − | USA |
| Wiborg & Dahl 78 | PAN | DYN | TCA | 20 | 20 | + + + + | Europe |
| Wiles et al 79 | Mood | CBT | Prot/Other | 14 | 11 | + + + + | Europe |
A positive or negative sign is given for four quality criteria: allocation sequence, concealment of allocation to conditions, blinding of assessors, and intention-to-treat analysis
BT – behavior therapy, CBT – cognitive behavior therapy, DYN – psychodynamic therapy, DYS – dysthymic disorder, GAD – generalized anxiety disorder, IPT – interpersonal psychotherapy, MAOI – monoamine oxidase inhibitor, MDD – major depressive disorder, Mood – mixed mood disorder, Ncom – number of patients in the combined treatment condition, Nmed – number of patients in the pharmacotherapy condition, OCD – obsessive-compulsive disorder, PAN – panic disorder with or without agoraphobia, Prot/Other – other antidepressant or protocolized treatment with antidepressants, PST – problem-solving therapy, PTSD – post-traumatic stress disorder, SAD – social anxiety disorder, SNRI – serotonin-norepinephrine reuptake inhibitor, SSRI – selective serotonin reuptake inhibitor, TCA – tricyclic antidepressant
Characteristics of included studies
In the 52 studies, 3,623 patients participated (1,767 in the combined treatment conditions and 1,856 in the pharmacotherapy only conditions). Thirty-two studies were aimed at depressive disorders (22 on major depression, including one that was aimed at patients with both major depression and OCD; 5 on dysthymia; and 5 on mixed mood disorders) and 21 at anxiety disorders (10 on panic disorder with or without agoraphobia; 4 on OCD; 4 on SAD; 2 on PTSD, and one on GAD). Most studies (n = 32) recruited patients exclusively from clinical samples, and were aimed at adults in general instead of a more specific population (such as older adults or patients with a comorbid somatic disorder).
Most psychotherapies belonged to the family of cognitive and behavioral therapies, while nine studies examined IPT, and the remaining 10 examined other therapies (including psychodynamic therapies). The number of treatment sessions ranged from 5 to 56, with most therapies (n = 36) having between 10 and 20 sessions. The antidepressants that were examined in the studies included SSRIs (n = 22), TCAs (n = 13), SNRIs (n = 3), MAOIs (n = 4), and treatment protocols with different types of antidepressant medication (n = 10).
Most studies were conducted in the US (n = 20), or Europe (n = 19). Two papers were published in German, the rest in English.
Quality assessment
The quality of the studies varied (Table1). Twenty-one studies reported an adequate sequence generation, while the other 31 did not. Nineteen studies reported allocation to conditions by an independent (third) party. Thirty-nine studies reported blinding of outcome assessors or used only self-report outcomes, whereas 13 did not report blinding. Thirty-one studies conducted intention-to-treat analyses (a post-treatment score was analyzed for every patient even if the last observation prior to attrition had to be carried forward or that score was estimated from earlier response trajectories). Thirteen studies met all four quality criteria, another six studies met 3 criteria, while the remaining 33 studies met two criteria or less.
Effects of combined treatment versus antidepressants only
The overall mean effect size indicating the difference between pharmacotherapy only and combined treatment of pharmacotherapy and psychotherapy at post-test for all 52 studies was 0.43 (95% CI: 0.31-0.56) in favor of the combined treatment. This corresponds to a NNT of 4.20. Heterogeneity was moderate to high (I2 = 64; 95% CI: 52-73). After exclusion of three possible outliers with extremely large effect sizes (g > 1.5; Table2), the effect size was somewhat smaller (g = 0.37; 95% CI: 0.27-0.47; NNT = 4.85), but heterogeneity was reduced to a moderate level (I2 = 48). The results of these analyses are reported in Table2. A forest plot of the studies and their effect sizes is given in Figure 2.
Table 2.
Effects of combined therapy for adult depressive and anxiety disorders compared with antidepressant medication only
| Ncomp | g | 95% CI | I2 | 95% CI | p | NNT | ||
|---|---|---|---|---|---|---|---|---|
| Depressive and anxiety disorders | 52 | 0.43 | 0.31-0.56 | 64 | 52-73 | 0.81 | 4.20 | |
| Possible outliers excluded (g > 1.5) | 49 | 0.37 | 0.27-0.47 | 48 | 28-63 | 4.85 | ||
| Depressive disorders | 32 | 0.41 | 0.28-0.54 | 50 | 25-67 | 0.17 | 4.39 | |
| Major depression | 23 | 0.43 | 0.29-0.57 | 30 | 0-58 | 4.20 | ||
| Dysthymia | 5 | 0.20 | −0.21-0.60 | 0 | 0-79 | 8.93 | ||
| Mixed depressive disorders | 5 | 0.56 | 0.12-0.99 | 73 | 32-89 | 3.25 | ||
| Anxiety disorders | 21 | 0.47 | 0.23-0.71 | 75 | 61-84 | 0.66 | 3.85 | |
| Panic disorder | 10 | 0.54 | 0.25-0.82 | 82 | 68-90 | 3.36 | ||
| OCD | 4 | 0.70 | 0.14-1.25 | 67 | 5-89 | 2.63 | ||
| SAD | 4 | 0.32 | −0.01-0.71 | 65 | 0-88 | 5.56 | ||
| PTSD | 2 | 0.31 | −0.39-1.00 | 0 | - | 5.75 | ||
| GAD | 1 | −0.51 | −1.42-0.40 | - | - | (3.55) | ||
| Subgroup analyses | ||||||||
| Medication | SSRI | 22 | 0.34 | 0.15-0.53 | 76 | 63-84 | 0.45 | 5.26 |
| TCA | 13 | 0.46 | 0.22-0.71 | 9 | 0-47 | 3.91 | ||
| Other/protocol | 17 | 0.51 | 0.31-0.72 | 41 | 0-67 | 3.55 | ||
| Recruitment | Clinical samples | 32 | 0.49 | 0.34-0.64 | 63 | 46-75 | 0.09 | 3.68 |
| Community | 16 | 0.28 | 0.08-0.47 | 45 | 2-70 | 6.41 | ||
| Target group | Adult in general | 43 | 0.44 | 0.30-0.57 | 65 | 51-74 | 0.89 | 4.10 |
| Specific group | 9 | 0.41 | 0.12-0.71 | 64 | 27-83 | 4.39 | ||
| Type of therapy | CBT | 33 | 0.51 | 0.35-0.66 | 70 | 58-79 | 0.20 | 3.55 |
| IPT | 9 | 0.24 | −0.05-0.53 | 32 | 0-69 | 7.46 | ||
| Other | 10 | 0.37 | 0.09-0.64 | 10 | 0-50 | 4.85 | ||
| Number of sessions | 5-9 | 11 | 0.67 | 0.40-0.93 | 86 | 76-91 | 0.10 | 2.75 |
| 10-12 | 16 | 0.24 | 0.03-0.46 | 48 | 8-71 | 7.46 | ||
| 13-18 | 18 | 0.47 | 0.26-0.67 | 4 | 0-52 | 3.85 | ||
| >19 | 7 | 0.41 | 0.06-0.76 | 33 | 0-72 | 4.39 | ||
| Treatment format | Individual | 42 | 0.46 | 0.32-0.59 | 68 | 55-76 | 0.35 | 3.91 |
| Group | 9 | 0.29 | −0.02-0.60 | 40 | 0-73 | 6.17 | ||
| Quality score | <3 | 32 | 0.49 | 0.33-0.66 | 62 | 44-74 | 0.23 | 3.68 |
| 3 or 4 | 20 | 0.35 | 0.16-0.54 | 67 | 47-79 | 5.10 | ||
CBT – cognitive behavior therapy, GAD – generalized anxiety disorder, IPT – interpersonal psychotherapy, Ncomp – number of comparisons, NNT – number needed to treat, OCD – obsessive-compulsive disorder, PTSD – post-traumatic stress disorder, SAD – social anxiety disorder, SNRI – serotonin-norepinephrine reuptake inhibitor, SSRI – selective serotonin reuptake inhibitor, TCA – tricyclic antidepressant
Figure 2.
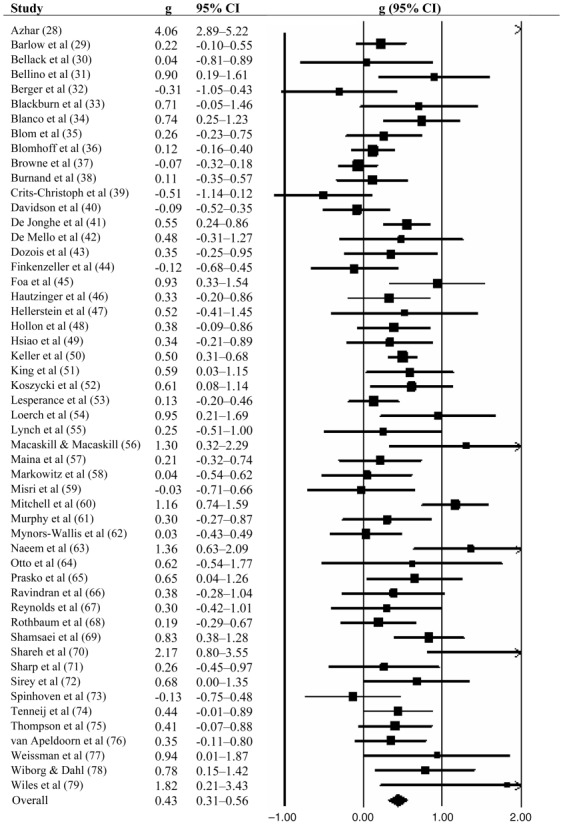
Effects of pharmacotherapy compared to combined treatment with pharmacotherapy and psychotherapy (Hedges' g)
For specific disorders, we found evidence that combined treatment was more effective than pharmacotherapy alone in major depression (g = 0.43; 95% CI: 0.29-0.57; NNT = 4.20), panic disorder (g = 0.54; 95% CI: 0.25-0.82; NNT = 3.36), and OCD (g = 0.70; 95% CI: 0.14-1.25; NNT = 2.63). We also found some indication that combined treatment may be more effective than pharmacotherapy in SAD (g = 0.32; 95% CI: −0.01-0.71; NNT = 5.56), although this was not significant (p<0.1). Insufficient evidence was found for dysthymia, PTSD, and GAD.
Inspection of the funnel plot and Duval and Tweedie's trim and fill procedure pointed at some risk of publication bias. After adjustment for possible publication bias, the overall mean effect size was reduced from g = 0.43 (NNT = 4.20) to g = 0.29 (95% CI: 0.15-0.43; NNT = 6.17; number of imputed studies: 10). Egger's test of the intercept also indicated significant publication bias (intercept: 1.33; 95% CI: 0.24-2.42; p<0.01).
We found no indication that combined treatment resulted in lower dropout from treatment than pharmacotherapy alone. The RR of dropping out of treatment, in the 35 studies in which dropout was reported, was RR = 0.99 (95% CI: 0.95-1.03; I2 = 24; 95% CI: 0-50).
Subgroup analyses indicated no significant differences between the effects sizes of depressive and anxiety disorders, between the different depressive disorders (while excluding anxiety disorders), and between the different anxiety disorders (while excluding depressive disorders) (Table2). We also found no indication that the effect sizes differed according to the type of medication (SSRI; TCA; other or protocolized), target group (adults in general or more specific target group), psychotherapy treatment format (individual or group), type of therapy (CBT; IPT; other), number of treatment sessions (5-9; 10-12; 13-18; >19); and quality of the studies (meeting 3 or 4 criteria versus less than 3 criteria). We did find a trend (p<0.1) indicating that the effect size may be higher in clinical samples (g = 0.49) compared with samples that included patients recruited from the community (g = 0.27).
We examined whether baseline severity was associated with outcome in the 20 studies examining depressive disorders. Mean baseline severity according to the Hamilton Depression Rating Scale (HAM-D) was moderate in 16 of the 20 studies (score 18-24), severe in three studies (score >24), and mild in one study (score <18) 80. In a meta-regression analysis, we did not find any indication that the effect size of difference between pharmacotherapy and combined treatment was associated with baseline severity of depression (slope: 0.007; 95% CI: −0.022-0.038; p = 0.63).
Combined treatment versus placebo
In 11 of the 53 studies, the combined treatment could be compared to a pill placebo control group. All of these studies also included a psychotherapy-only condition (with or without a pill placebo), as well as a pharmacotherapy-only condition. This allowed us to calculate the effect sizes indicating the difference between pharmacotherapy and placebo, psychotherapy (with or without a pill placebo) and placebo, as well as between combined treatment and placebo. With these effect sizes we could estimate the contribution of pharmacotherapy and psychotherapy to the effects of combined treatment.
The results of the analyses are presented in Table3. The effects of combined treatment compared with placebo are large (g = 0.74; 95% CI: 0.48-1.01; NNT = 2.50), with moderate to high heterogeneity (I2 = 65; 95% CI: 33-82). In these 11 studies, the effect size of pharmacotherapy compared with placebo was g = 0.35 (95% CI:0.21-0.49) and that of psychotherapy compared with placebo was g = 0.37 (95% CI: 0.11-0.64). This suggests that the effects of psychotherapy and those of pharmacotherapy are largely independent of each other, and each add about 50% to the overall effects of combined treatment. The independence of the effects of the two kinds of treatments is further supported by the effect sizes of pharmacotherapy versus combined treatment (g = 0.37 in this sample), and those of psychotherapy versus combined treatment (g = 0.38).
Table 3.
Direct comparisons between psychotherapy, pharmacotherapy, combined psychotherapy and pharmacotherapy, and placebo in anxiety and depressive disorders (Hedges' g)
| Ncomp | g | 95% CI | I2 | 95% CI | NNT | |
|---|---|---|---|---|---|---|
| Combined vs. placebo | 11 | 0.74 | 0.48-1.01 | 65 | 33-82 | 2.50 |
| Pharmacotherapy vs. combined | 11 | 0.37 | 0.12-0.63 | 43 | 0-72 | 4.85 |
| Pharmacotherapy vs. placebo | 11 | 0.35 | 0.21-0.49 | 0 | 0-60 | 5.10 |
| Psychotherapy vs. combined | 11 | 0.38 | 0.16-0.59 | 53 | 8-76 | 4.72 |
| Psychotherapy vs. placebo | 11 | 0.37 | 0.11-0.64 | 68 | 41-83 | 4.85 |
Ncomp - number of comparisons, NNT – number needed to treat
Long-term differences between pharmacotherapy and combined treatment
Long-term differences between pharmacotherapy and combined treatment were reported in 19 studies, with follow-up periods varying from 3 to 24 months. Because the way positive outcomes were defined differed from study to study, we have reported the definition of a positive outcome at each of the follow-up points in Table4.
Table 4.
Long-term follow-up effects in included studies: definitions of positive outcome and relative risk associated with each outcome
| Study | Outcome | Follow-up (months) | RR | 95% CI |
|---|---|---|---|---|
| Barlow et al 29 | CGI response | 6-8 | 1.52 | 1.07-2.16 |
| Barlow et al 29 | CGI response | 9-12 | 1.39 | 0.75-2.58 |
| Barlow et al 29 | PDSS response | 6-8 | 1.52 | 1.07-2.16 |
| Barlow et al 29 | PDSS response | 9-12 | 1.31 | 0.69-2.45 |
| Bellack et al 30 | <10 on BDI + HAMD | 6-8 | 1.30 | 0.53-3.16 |
| Blanco et al 34 | remission | 3-5 | 2.07 | 1.08-3.96 |
| Blanco et al 34 | response | 3-5 | 1.61 | 1.09-2.37 |
| Hautzinger et al 46 | response | 9-12 | 1.91 | 1.07-3.39 |
| Hellerstein et al 47 | remission | 3-5 | 0.62 | 0.23-1.66 |
| Hellerstein et al 47 | response | 3-5 | 1.53 | 0.74-3.14 |
| Hollon et al 48 | no relapse | 9-12 | 1.87 | 0.99-3.52 |
| Hollon et al 48 | no relapse | 13-24 | 1.73 | 0.90-3.32 |
| Keller et al 50 | no relapse | 3-5 | 1.01 | 0.95-1.08 |
| Loerch et al 54 | FQ<10 | 6-8 | 1.17 | 0.79-1.74 |
| Loerch et al 54 | FQ>50% improvement | 6-8 | 1.17 | 0.79-1.74 |
| Lynch et al 55 | BDI<9 | 6-8 | 1.29 | 0.43-3.88 |
| Lynch et al 55 | HAMD<7 | 6-8 | 2.35 | 1.07-5.16 |
| Maina et al 57 | CGI success | 6-8 | 1.55 | 0.62-3.86 |
| Maina et al 57 | HAMD response | 6-8 | 1.16 | 0.47-2.86 |
| Maina et al 57 | YBOCS response | 6-8 | 0.77 | 0.38-1.58 |
| Mitchell et al 60 | HAMD<9 | 3-5 | 2.08 | 1.13-3.82 |
| Mitchell et al 60 | HAMD<9 | 9-12 | 1.76 | 1.01-3.08 |
| Mitchell et al 60 | HAMD<9 | 13-24 | 1.42 | 0.91-2.23 |
| Murphy et al 61 | no relapse | 9-12 | 1.71 | 0.61-4.80 |
| Mynors-Wallis et al 62 | recovered | 9-12 | 1.18 | 0.81-1.73 |
| Prasko et al 65 | no relapse | 3-5 | 1.62 | 0.89-2.95 |
| Prasko et al 65 | no relapse | 9-12 | 2.16 | 0.81-5.77 |
| Prasko et al 65 | no relapse | 13-24 | 1.94 | 0.71-5.31 |
| Reynolds et al 67 | no relapse | 3-5 | 9.58 | 2.09-43.94 |
| Sharp et al 71 | FQ-AG: clinically significant change | 6-8 | 1.60 | 0.88-2.91 |
| Sharp et al 71 | HAMA: clinically significant change | 6-8 | 1.64 | 0.95-2.82 |
| Sharp et al 71 | SRT: clinically significant change | 6-8 | 2.50 | 0.88-7.07 |
| van Apeldoorn et al 76 | remission | 6-8 | 1.48 | 0.63-3.47 |
| van Apeldoorn et al 76 | remission | 9-12 | 1.93 | 0.87-4.27 |
| Wiborg & Dahl 78 | no DSM relapse | 9-12 | 3.20 | 1.45-7.05 |
| Wiborg & Dahl 78 | remission | 9-12 | 3.20 | 1.45-7.05 |
BDI – Beck Depression Inventory, CGI – Clinical Global Impression, FQ – Fear Questionnaire, FQ-AG – Fear Questionnaire, Agoraphobia Subscale, HAMA – Hamilton Anxiety Rating Scale, HAMD – Hamilton Depression Rating Scale, PDSS – Postpartum Depression Screening Scale, RR – relative risk, SRT – Kellner and Sheffield Symptom Rating Scale, YBOCS – Yale-Brown Obsessive Compulsive Scale
The RR of having a positive outcome for all follow-up periods together was 1.48 (95% CI: 1.23-1.78; NNT = 4.29), and ranged from RR = 1.40 to 1.51 (NNTs: 3.41 to 6.90) for the four follow-up periods we distinguished. In each of the four follow-up periods, combined treatment was significantly more effective than pharmacotherapy alone (Table5).
Table 5.
Long-term effects of combined therapy for anxiety and depressive disorders compared with antidepressive medication only: relative risk of having a positive outcome
| Ncomp | RR | 95% CI | I2 | 95% CI | NNT | |
|---|---|---|---|---|---|---|
| 3-5 months after end of treatment | 6 | 1.60 | 1.03-2.48 | 75 | 43-89 | 3.41 |
| 6-8 months after end of treatment | 7 | 1.40 | 1.13-1.73 | 0 | 0-71 | 6.90 |
| 9-12 months after end of treatment | 10 | 1.51 | 1.25-1.84 | 13 | 0-56 | 4.52 |
| 13-24 months after end of treatment | 4 | 1.49 | 1.12-1.98 | 0 | 0-85 | 4.35 |
| All long-term outcomes pooled | 19 | 1.48 | 1.23-1.78 | 55 | 25-73 | 4.29 |
Ncomp – number of comparisons, NNT – Number needed to treat, RR – relative risk
DISCUSSION
In this meta-analysis, we found clear evidence that combined treatment with psychotherapy and antidepressant medication is more effective than treatment with antidepressant medication alone. This difference was significant for major depression, panic disorder, and OCD. A trend indicated possible superior effects in SAD. We did not find sufficient evidence for a significant difference in dysthymia, PTSD and GAD, but this could be due to the small number of studies and associated lack of statistical power for these disorders. The superior effects of combined treatment remained significant at one to two-year follow-up.
We found that the superior effects of combined treatment may have been overestimated by publication bias, which is in line with earlier research on pharmacotherapy 81 as well as psychotherapy 82, showing evidence of publication bias in both fields. However, even after adjusting for publication bias, the superiority of combined treatment was still statistically significant.
We also found some indications that the difference between pharmacotherapy and combined treatment was especially high in clinical samples compared with samples that were (in part) recruited from the community. Although this difference was only marginally significant (p<0.1), it does suggest that patients actively seeking treatment may benefit more from combined treatment than people who are recruited from the community.
Research up to now has not been able to answer the question of how large the effects of combined treatment are compared with pill placebo only. We found indications that the effects of combined treatment compared with placebo only were about twice as large as those of pharmacotherapy compared with placebo only.
Until now it has not been established well whether the effects of pharmacotherapy and those of psychotherapy are complementary to each other, whether they have effects independent from each other, or whether combined treatments lead to higher effects than the sum of the two treatments alone 83,84. The present study indicates that the effects of psychotherapy and pharmacotherapy may be largely independent from each other and additive, not interfering with each other, and both contribute about equally to the effects of combined treatment.
From a clinical point of view, this paper suggests that combined treatment should be used in more patients than is currently done in clinical practice. Most patients receive either pharmacotherapy or psychotherapy 16,17, and only a minority receives combined therapy. Combined treatment is especially given to more severe and chronic cases. Our data suggest that the superior effects of combined treatment are not associated with baseline severity, at least in depression. Because the effects of the two treatments seem to be largely independent from each other, combined treatment may also be beneficial in less severe cases.
This study has some limitations. First, it is not possible to blind comparisons of pharmacotherapy to combined treatment and this may have introduced a bias in the outcomes. Second, because patients refusing antidepressants may not have been willing to be enrolled in trials, there may have been a sampling bias that could limit the generalizability of these findings. Third, we found considerable levels of heterogeneity among the studies, which could not fully be explained by moderator analyses. Another limitation was the relatively small number of included studies for some disorders. A final limitation is that we considered psychotherapy and pharmacotherapy as monolithic treatments, while in fact several different treatments were used in the included studies.
In sum, the present study found superior effects of combined treatment over pharmacotherapy alone, which are significant and relevant up to two years after treatment. These results thus support the use of combined treatment for common mental disorders rather than monotherapy with psychotropic medication without psychotherapy.
References
- 1.Kessler RC, Berglund P, Demler O, et al. National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Ustun TB, Ayuso-Mateos JL, Chatterji S, et al. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386–92. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]
- 4.Saarni SI, Suvisaari J, Sintonen H, et al. Impact of psychiatric disorders on health-related quality of life: general population survey. Br J Psychiatry. 2007;190:326–32. doi: 10.1192/bjp.bp.106.025106. [DOI] [PubMed] [Google Scholar]
- 5.Berto P, D'Ilario D, Ruffo P, et al. Depression: cost-of-illness studies in the international literature: a review. J Ment Health Policy Econ. 2000;3:3–10. doi: 10.1002/1099-176x(200003)3:1<3::aid-mhp68>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg PE, Birnbaum HG. The economic burden of depression in the US: societal and patient perspectives. Exp Opin Pharmacother. 2005;6:369–76. doi: 10.1517/14656566.6.3.369. [DOI] [PubMed] [Google Scholar]
- 7.Smit F, Cuijpers P, Oostenbrink J, et al. Excess costs of common mental disorders: population based cohort study. J Ment Health Policy Econ. 2006;9:193–200. [PubMed] [Google Scholar]
- 8.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute for Health and Clinical Excellence (NICE) Depression; the treatment and management of depression in adults. Holborn: NICE; 2009. [Google Scholar]
- 10.Bauer M, Bschor T, Pfennig A, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders in primary care. World J Biol Psychiatry. 2007;8:67–104. doi: 10.1080/15622970701227829. [DOI] [PubMed] [Google Scholar]
- 11.Bandelow B, Sher L, Bunevicius R, et al. Guidelines for the pharmacological treatment of anxiety disorders, obsessive-compulsive disorder and posttraumatic stress disorder in primary care. Int J Psychiatry Clin Pract. 2012;16:77–84. doi: 10.3109/13651501.2012.667114. [DOI] [PubMed] [Google Scholar]
- 12.Cuijpers P, Sijbrandij M, Koole SL, et al. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry. 2013;12:137–48. doi: 10.1002/wps.20038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cuijpers P, Dekker J, Hollon SD, et al. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis. J Clin Psychiatry. 2009;70:1219–29. doi: 10.4088/JCP.09r05021. [DOI] [PubMed] [Google Scholar]
- 14.Cuijpers P, Straten van A, Warmerdam L, et al. Psychological treatment versus combined treatment of depression: a meta-analysis. Depress Anx. 2009;26:279–88. doi: 10.1002/da.20519. [DOI] [PubMed] [Google Scholar]
- 15.Maat de SM, Dekker J, Schoevers RA, et al. Relative efficacy of psychotherapy and combined therapy in the treatment of depression: a meta-analysis. Eur Psychiatry. 2007;22:1–8. doi: 10.1016/j.eurpsy.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Olfson M, Marcus SC. National trends in outpatient psychotherapy. Am J Psychiatry. 2010;167:1456–63. doi: 10.1176/appi.ajp.2010.10040570. [DOI] [PubMed] [Google Scholar]
- 17.Marcus SC, Olfson M. National trends in the treatment for depression from 1998 to 2007. Arch Gen Psychiatry. 2010;67:1265–73. doi: 10.1001/archgenpsychiatry.2010.151. [DOI] [PubMed] [Google Scholar]
- 18.Furukawa TA, Watanabe N, Churchill R. Combined psychotherapy plus antidepressants for panic disorder with or without agoraphobia. Cochrane Database of Systematic Reviews. 2007;1:CD004364. doi: 10.1002/14651858.CD004364.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hofmann SG, Sawyer AT, Korte KJ, et al. Is it beneficial to add pharmacotherapy to cognitive-behavioral therapy when treating anxiety disorders? A meta-analytic review. Int J Cogn Ther. 2009;2:160–75. doi: 10.1521/ijct.2009.2.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.0.1. Oxford: Cochrane Collaboration; 2008. [Google Scholar]
- 21.Hedges LV, Olkin I. Statistical methods for meta-analysis. San Diego: Academic Press; 1985. [Google Scholar]
- 22.Kraemer HC, Kupfer DJ. Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry. 2006;59:990–6. doi: 10.1016/j.biopsych.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Laupacis A, Sackett DL, Roberts RS. An assessment of clinically useful measures of the consequences of treatment. N Engl J Med. 1988;318:1728–33. doi: 10.1056/NEJM198806303182605. [DOI] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ioannidis JPA, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–6. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Orsini N, Higgins J, Bottai M, et al. Heterogi: Stata module to quantify heterogeneity in a meta-analysis. Boston: Boston College Department of Economics; 2005. [Google Scholar]
- 27.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 28.Azhar MZ. Comparison of Fluvoxamine alone, Fluvoxamine and cognitive psychotherapy and psychotherapy alone in the treatment of panic disorder in Kelantan – implications for management by family doctors. Med J Malaysia. 2000;55:402–8. [PubMed] [Google Scholar]
- 29.Barlow DH, Gorman JM, Shear MK, et al. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. JAMA. 2000;283:2529–36. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- 30.Bellack AS, Hersen M, Himmelhoch J. Social skills training compared with pharmacotherapy and psychotherapy in the treatment of unipolar depression. Am J Psychiatry. 1981;138:1562–67. doi: 10.1176/ajp.138.12.1562. [DOI] [PubMed] [Google Scholar]
- 31.Bellino S, Zizza M, Camilla R, et al. Combined treatment of major depression in patients with borderline personality disorder: a comparison with pharmacotherapy. Can J Psychiatry. 2006;51:253–60. doi: 10.1177/070674370605100707. [DOI] [PubMed] [Google Scholar]
- 32.Berger P, Sachs G, Amering M, et al. Personality disorder and social anxiety predict delayed response in drug and behavioral treatment of panic disorder. J Affect Disord. 2004;80:75–8. doi: 10.1016/S0165-0327(03)00043-0. [DOI] [PubMed] [Google Scholar]
- 33.Blackburn IM, Bishop S, Glen AI, et al. The efficacy of cognitive therapy in depression: a treatment trial using cognitive therapy and pharmacotherapy, each alone and in combination. Br J Psychiatry. 1981;139:181–9. doi: 10.1192/bjp.139.3.181. [DOI] [PubMed] [Google Scholar]
- 34.Blanco C, Heimberg RG, Schneier FR, et al. A placebo-controlled trial of phenelzine, cognitive behavioral group therapy, and their combination for social anxiety disorder. Arch Gen Psychiatry. 2010;67:286–95. doi: 10.1001/archgenpsychiatry.2010.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blom MB, Spinhoven P, Hoffman T, et al. Severity and duration of depression, not personality factors, predict short term outcome in the treatment of major depression. J Affect Disord. 2007;104:119–26. doi: 10.1016/j.jad.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 36.Blomhoff S, Haug TT, Hellström K, et al. Randomised controlled general practice trial of sertraline, exposure therapy and combined treatment in generalised social phobia. Br J Psychiatry. 2001;179:23–30. doi: 10.1192/bjp.179.1.23. [DOI] [PubMed] [Google Scholar]
- 37.Browne G, Steiner M, Roberts J, et al. Sertraline and/or interpersonal psychotherapy for patients with dysthymic disorder in primary care: 6-month comparison with longitudinal 2-year follow-up of effectiveness and costs. J Affect Disord. 2002;68:317–30. doi: 10.1016/s0165-0327(01)00343-3. [DOI] [PubMed] [Google Scholar]
- 38.Burnand Y, Andreoli A, Kolatte E, et al. Psychodynamic psychotherapy and clomipramine in the treatment of major depression. Psychiatr Serv. 2002;53:585–90. doi: 10.1176/appi.ps.53.5.585. [DOI] [PubMed] [Google Scholar]
- 39.Crits-Christoph P, Newman MG, Rickels K, et al. Combined medication and cognitive therapy for generalized anxiety disorder. J Anxiety Disord. 2011;25:1087–94. doi: 10.1016/j.janxdis.2011.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davidson JRT, Foa EB, Huppert JD, et al. Fluoxetine, comprehensive cognitive behavioral therapy, and placebo in generalized social phobia. Arch Gen Psychiatry. 2004;61:1005–13. doi: 10.1001/archpsyc.61.10.1005. [DOI] [PubMed] [Google Scholar]
- 41.Jonghe de F, Kool S, Aalst van G, et al. Combining psychotherapy and antidepressants in the treatment of depression. J Affect Disord. 2001;64:217–29. doi: 10.1016/s0165-0327(00)00259-7. [DOI] [PubMed] [Google Scholar]
- 42.Mello de MF, Myczcowisk LM, Menezes PR. A randomized controlled trial comparing moclobemide and moclobemide plus interpersonal psychotherapy in the treatment of dysthymic disorder. J Psychother Pract Res. 2001;10:117–23. [PMC free article] [PubMed] [Google Scholar]
- 43.Dozois DJA, Bieling PJ, Patelis-Siotis I, et al. Changes in self-schema structure in cognitive therapy for major depressive disorder: a randomized clinical trial. J Consult Clin Psychol. 2009;77:1078–88. doi: 10.1037/a0016886. [DOI] [PubMed] [Google Scholar]
- 44.Finkenzeller W, Zobel I, Rietz S, et al. Interpersonal psychotherapy and pharmacotherapy for post-stroke depression. Feasibility and effectiveness. Nervenarzt. 2009;80:805–12. doi: 10.1007/s00115-008-2649-1. [DOI] [PubMed] [Google Scholar]
- 45.Foa EB, Liebowitz MR, Kozak MJ, et al. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 2005;162:151–61. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- 46.Hautzinger M, Jong-Meyer de R, Treiber R, et al. Wirksamkeit Kognitiever Verhaltenstherapie, Pharmacotherapie und deren Kombination bei nicht-endogenen, unipolaren Depressionen. Zeitschr Klin Psychol. 1996;25:130–45. [Google Scholar]
- 47.Hellerstein DJ, Little SAS, Samstag LW, et al. Adding group psychotherapy to medication treatment in dysthymia: a randomized prospective pilot study. J Psychother Pract Res. 2001;10:93–103. [PMC free article] [PubMed] [Google Scholar]
- 48.Hollon SD, DeRubeis RJ, Evans MD, et al. Cognitive therapy and pharmacotherapy for depression: singly and in combination. Arch Gen Psychiatry. 1992;49:774–81. doi: 10.1001/archpsyc.1992.01820100018004. [DOI] [PubMed] [Google Scholar]
- 49.Hsiao FH, Jow GM, Lai YM, et al. The long-term effects of psychotherapy added to pharmacotherapy on morning to evening diurnal cortisol patterns in outpatients with major depression. Psychother Psychosom. 2011;80:166–72. doi: 10.1159/000321558. [DOI] [PubMed] [Google Scholar]
- 50.Keller MB, McCullough JP, Klein DN, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–70. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- 51.King ALS, Valenca AM, Melo-Neto de VL, et al. Efficacy of a specific model for cognitive-behavioral therapy among panic disorder patients with agoraphobia: a randomized clinical trial. Sao Paulo Med J. 2011;129:325–34. doi: 10.1590/S1516-31802011000500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koszycki D, Taljaard M, Segal Z, et al. A randomized trial of sertraline, self-administered cognitive behavior therapy, and their combination for panic disorder. Psychol Med. 2011;41:373–83. doi: 10.1017/S0033291710000930. [DOI] [PubMed] [Google Scholar]
- 53.Lesperance F, Frasure-Smith N, Koszycki D, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. JAMA. 2007;297:367–79. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- 54.Loerch B, Graf-Morgenstern M, Hautzinger M, et al. Randomised placebo-controlled trial of moclobemide, cognitive-behavioural therapy and their combination in panic disorder with agoraphobia. Br J Psychiatry. 1999;174:205–12. doi: 10.1192/bjp.174.3.205. [DOI] [PubMed] [Google Scholar]
- 55.Lynch TR, Morse JQ, Mendelson T, et al. Dialectical behavior therapy for depressed older adults: a randomized pilot study. Am J Geriatr. 2003;11:33–45. [PubMed] [Google Scholar]
- 56.Macaskill ND, Macaskill A. Rational-emotive therapy plus pharmacotherapy vs. pharmacotherapy alone in the treatment of high cognitive dysfunction depression. Cogn Ther Res. 1996;20:575–92. [Google Scholar]
- 57.Maina G, Rosso G, Rigardetto S, et al. No effect of adding brief dynamic therapy to pharmacotherapy in the treatment of obsessive-compulsive disorder with concurrent major depression. Psychother Psychosom. 2010;79:295–302. doi: 10.1159/000318296. [DOI] [PubMed] [Google Scholar]
- 58.Markowitz JC, Kocsis JH, Bleiberg KL, et al. A comparative trial of psychotherapy and pharmacotherapy for “pure” dysthymic patients. J Affect Disord. 2005;89:167–75. doi: 10.1016/j.jad.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 59.Misri S, Reebye P, Corral M, et al. The use of paroxetine and cognitive-behavioral therapy in postpartum depression and anxiety: a randomized controlled trial. J Clin Psychiatry. 2004;65:1236–41. doi: 10.4088/jcp.v65n0913. [DOI] [PubMed] [Google Scholar]
- 60.Mitchell PH, Veith RC, Becker KJ, et al. Brief psychosocial-behavioral intervention with antidepressant reduces poststroke depression significantly more than usual care with antidepressant: living well with stroke: randomized, controlled trial. Stroke. 2009;40:3073–8. doi: 10.1161/STROKEAHA.109.549808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Murphy GE, Simons AD, Wetzel RD, et al. Cognitive therapy and pharmacotherapy. Singly and together in the treatment of depression. Arch Gen Psychiatry. 1984;41:33–41. doi: 10.1001/archpsyc.1984.01790120037006. [DOI] [PubMed] [Google Scholar]
- 62.Mynors-Wallis LM, Gath DH, Day A, et al. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ. 2000;320:26–30. doi: 10.1136/bmj.320.7226.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Naeem F, Waheed W, Gobbi M, et al. Preliminary evaluation of culturally sensitive CBT for depression in Pakistan: findings from Developing Culturally-sensitive CBT Project (DCCP) Behav Cogn Psychother. 2011;39:165–73. doi: 10.1017/S1352465810000822. [DOI] [PubMed] [Google Scholar]
- 64.Otto MW, Hinton D, Korbly NB, et al. Treatment of pharmacotherapy-refractory posttraumatic stress disorder among Cambodian refugees: a pilot study of combination treatment with cognitive-behavior therapy vs sertraline alone. Behav Res Ther. 2003;41:1271–6. doi: 10.1016/s0005-7967(03)00032-9. [DOI] [PubMed] [Google Scholar]
- 65.Prasko J, Dockery C, Horacek J, et al. Moclobemide and cognitive behavioral therapy in the treatment of social phobia. A six-month controlled study and 24 months follow up. Neuroendocrinol Lett. 2006;27:473–81. [PubMed] [Google Scholar]
- 66.Ravindran AV, Anisman H, Merali Z, et al. Treatment of primary dysthymia with group cognitive therapy and pharmacotherapy: clinical symptoms and functional impairments. Am J Psychiatry. 1999;156:1608–17. doi: 10.1176/ajp.156.10.1608. [DOI] [PubMed] [Google Scholar]
- 67.Reynolds CF, 3rd, Miller MD, Pasternak RE, et al. Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry. 1999;156:202–8. doi: 10.1176/ajp.156.2.202. [DOI] [PubMed] [Google Scholar]
- 68.Rothbaum BO, Cahill SP, Foa EB, et al. Augmentation of sertraline with prolonged exposure in the treatment of posttraumatic stress disorder. J Trauma Stress. 2006;19:625–38. doi: 10.1002/jts.20170. [DOI] [PubMed] [Google Scholar]
- 69.Shamsaei F, Rahimi A, Zarabian MK, et al. Efficacy of pharmacotherapy and cognitive therapy, alone and in combination in major depressive disorder. Hong Kong J Psychiatry. 2008;18:76–80. [Google Scholar]
- 70.Shareh H, Gharraee B, Atef-Vahid MK, et al. Metacognitive Therapy (MCT), fluvoxamine, and combined treatment in improving obsessive-compulsive, depressive and anxiety symptoms in patients with Obsessive-Compulsive Disorder (OCD) Iran J Psychiatry Behav Sci. 2010;4:17–25. [Google Scholar]
- 71.Sharp DM, Power KG, Simpson RJ, et al. Fluvoxamine, placebo, and cognitive behaviour therapy used alone and in combination in the treatment of panic disorder and agoraphobia. J Anxiety Dis. 1996;10:219–42. [Google Scholar]
- 72.Sirey JA, Bruce ML, Alexopoulos GS. The Treatment Initiation Program: an intervention to improve depression outcomes in older adults. Am J Psychiatry. 2005;162:184–6. doi: 10.1176/appi.ajp.162.1.184. [DOI] [PubMed] [Google Scholar]
- 73.Spinhoven P, Onstein EJ, Klinkhamer RA, et al. Panic management, trazodone and a combination of both in the treatment of panic disorder. Clin Psychol Psychother. 1996;3:86–92. [Google Scholar]
- 74.Tenneij NH, Megen HJ, Denys DAJP, et al. Behavior therapy augments response of patients with obsessive-compulsive disorder responding to drug treatment. J Clin Psychiatry. 2005;66:1169–75. doi: 10.4088/jcp.v66n0913. [DOI] [PubMed] [Google Scholar]
- 75.Thompson LW, Coon DW, Gallagher-Thompson D, et al. Comparison of desipramine and cognitive/behavioral therapy in the treatment of elderly outpatients with mild-to-moderate depression. Am J Geriatr Psychiatry. 2001;9:225–40. [PubMed] [Google Scholar]
- 76.Apeldoorn van FJ, Hout van WJPJ, Huisman M, et al. Is a combined therapy more effective than either CBT or SSRI alone? Results of a multicenter trial on panic disorder with or without agoraphobia. Acta Psychiatr Scand. 2008;17:260–70. doi: 10.1111/j.1600-0447.2008.01157.x. [DOI] [PubMed] [Google Scholar]
- 77.Weissman MM, Prusoff BA, Dimascio A, et al. The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. Am J Psychiatry. 1979;136:555–8. [PubMed] [Google Scholar]
- 78.Wiborg IM, Dahl AA. Does brief dynamic psychotherapy reduce the relapse rate of panic disorder? Arch Gen Psychiatry. 1996;53:689–94. doi: 10.1001/archpsyc.1996.01830080041008. [DOI] [PubMed] [Google Scholar]
- 79.Wiles NJ, Hollinghurst S, Mason V, et al. A randomized controlled trial of cognitive behavioural therapy as an adjunct to pharmacotherapy in primary care based patients with treatment resistant depression: a pilot study. Behav Cogn Psychother. 2008;36:21–33. [Google Scholar]
- 80.Katz R, Shaw BF, Vallis TM. The assessment of severity and symptom patterns in depression. In: Beckham EE, Leber WR, et al., editors. Handbook of depression. 2. New York: Guilford; 1995. –61.pp. 85 [Google Scholar]
- 81.Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358:252–60. doi: 10.1056/NEJMsa065779. [DOI] [PubMed] [Google Scholar]
- 82.Cuijpers P, Smit F, Bohlmeijer, et al. Is the efficacy of cognitive behaviour therapy and other psychological treatments for adult depression overestimated? A meta-analytic study of publication bias. Br J Psychiatry. 2010;196:173–8. doi: 10.1192/bjp.bp.109.066001. [DOI] [PubMed] [Google Scholar]
- 83.Friedman MA, Detweiler-Bedell JB, Leventhal HE, et al. Combined psychotherapy and pharmacotherapy for the treatment of major depressive disorder. Clin Psychol Sci Pract. 2004;11:47–68. [Google Scholar]
- 84.Otto MW, Smits JAJ, Reese HE. Combined psychotherapy and pharmacotherapy for mood and anxiety disorders in adults: review and analysis. Clin Psychol Sci Pract. 2005;12:72–86. [Google Scholar]


