Abstract
This study explored the prevalence of risk behaviors (excessive alcohol use, illegal drug use, heavy smoking, reduced sleep, overweight, underweight, sedentary behavior, high use of Internet/TV/videogames for reasons not related to school or work, and truancy), and their association with psychopathology and self-destructive behaviors, in a sample of 12,395 adolescents recruited in randomly selected schools across 11 European countries. Latent class analysis identified three groups of adolescents: a low-risk group (57.8%) including pupils with low or very low frequency of risk behaviors; a high-risk group (13.2%) including pupils who scored high on all risk behaviors, and a third group (“invisible” risk, 29%) including pupils who were positive for high use of Internet/TV/videogames for reasons not related to school or work, sedentary behavior and reduced sleep. Pupils in the “invisible” risk group, compared with the high-risk group, had a similar prevalence of suicidal thoughts (42.2% vs. 44%), anxiety (8% vs. 9.2%), subthreshold depression (33.2% vs. 34%) and depression (13.4% vs. 14.7%). The prevalence of suicide attempts was 5.9% in the “invisible” group, 10.1% in the high-risk group and 1.7% in the low-risk group. The prevalence of all risk behaviors increased with age and most of them were significantly more frequent among boys. Girls were significantly more likely to experience internalizing (emotional) psychiatric symptoms. The “invisible” group may represent an important new intervention target group for potentially reducing psychopathology and other untoward outcomes in adolescence, including suicidal behavior.
Keywords: Risk behaviors, adolescents, media consumption, sedentary behavior, reduced sleep, psychiatric symptoms, suicidal behavior, SEYLE
Risk behaviors 1,2 and psychiatric symptoms 3,4 among youth are a major public health concern. Adolescents establish patterns of behavior and make lifestyle choices that affect both their current and future health and well-being 5–8. It has been shown that some of these choices have a strong association with mental disorders in adulthood 9,10. Given the importance of this transitional period and the acute need for targeted preventive efforts, it is essential to gather information regarding the prevalence of both healthy and risk behaviors, as well as psychiatric symptoms, based on a robust methodology 6,11–14.
Detailed information regarding adolescent risk behaviors is regularly collected in the United States through the Youth Risk Behavior Surveillance System (YRBSS) for the purpose of helping to shape policy and to identify areas for further research. Data from the YRBSS indicate that many pupils engage in behaviors that place them at risk for the leading causes of morbidity and mortality 15,16. These include tobacco, alcohol and substance use 17–19, underweight 20, obesity 21, sedentary behavior 22, unhealthy sleep patterns 23, and truancy 24. Many of these behaviors and conditions frequently co-occur in the same individuals 25. Similar information is not systematically collected and available for other regions of the world, including Europe.
The European School Survey Project on Alcohol and Other Drugs (ESPAD, 26) and the European Monitoring Centre for Drugs and Drug Addiction 27 regularly provide European Union Member States with an overview of alcohol and drug problems in the continent. However, these projects focus primarily on substance abuse, with limited attention to other risk behaviors and lifestyles. Studies that provide a comprehensive picture of adolescent risk behaviors, therefore, are critically needed in Europe 25. There is also recent evidence of an association in adolescents between mental health status, risk behaviors and lifestyles 28–32. To date, no comprehensive cross-national study has been conducted to test associations between risk behaviors, lifestyles and psychiatric symptoms in European adolescents.
The Saving and Empowering Young Lives in Europe (SEYLE) project 33 was developed by a consortium of twelve European countries (Sweden, Austria, Estonia, France, Germany, Hungary, Ireland, Israel, Italy, Romania, Slovenia, Spain) and supported with funding by the European Commission (grant agreement HEALTH-F2-2009-22309). One of the aims of SEYLE was to gather information about European adolescents' health and well-being. Here we report the main epidemiological findings regarding alcohol and illegal drug use, smoking, sleep behavior, nutrition, physical activity, and sensation seeking, including their associations with self-destructive behaviors and psychiatric symptoms. The hypothesis being tested was that the prevalence of these behaviors varies by age and gender and that behaviors cluster in identifiable subgroups of adolescents suitable for targeted intervention.
METHODS
High school pupils (N=12,395; mean age 14.91±0.90, 83 missing; M/F: 5,529/6,799, 67 missing) were recruited in randomly selected schools (n=179) in eleven European countries. At each country study site, a list of all eligible schools was generated according to specific inclusion and exclusion criteria 33. Ethical approval was obtained from each local ethical committee. Data regarding the study sites, the representativeness of the sample and consent/participation rates of schools and pupils were previously analysed, showing that each study site is reasonably representative of the respective country and that the external validity of the sample is high 34.
A structured self-report questionnaire was administered to adolescents in the participating schools. It covered socio-demographic items, such as sex, age, country of birth of the adolescent and his/her parents, parental employment status, and belonging to a religious group. Risk behaviors were assessed through the Global School-based Student Health Survey (GSHS, 35), which is the international version of the Youth Risk Behavior Survey questionnaire 36. Psychiatric symptoms were assessed by the Beck Depression Inventory (BDI-II, 37), the Zung Self-Rating Anxiety Scale (Z-SAS, 38), the Strengths and Difficulties Questionnaire (SDQ, 39), the Paykel Suicide Scale (PSS, 40) and the Deliberate Self-Harm Inventory (DSHI, 41). The officially translated and validated versions of these instruments were used when available. If the instruments were not available in the required language, they were translated (and back-translated) and linguistically adapted. Internal reliability for all instruments was assessed through Cronbach's alpha, which was high or very high for all of them 34. All the assessment instruments were administered in a single classroom session.
The GSHS items were recoded to identify nine areas of risk behaviors: excessive alcohol use (drinks at least twice a week), illegal drug use (used illegal drugs at least three times during life), heavy smoking (smokes more than 5 cigarettes per day), reduced sleep (sleeps 6 hours per night or less), overweight (body mass index (BMI) above the 95th percentile for age 42), underweight (BMI below the 5th percentile for age 42), sedentary behavior (performs physical activity less than once a week), high media use (uses Internet, TV and videogames for reasons not related to school or work for 5 hours or more per day), truancy (skips school at least once a week without being ill or having another legitimate excuse). A dichotomous variable was generated for each risk behavior.
Psychopathological symptoms were recoded to stratify pupils into dichotomous categories: subthreshold depression (BDI-II score <20 and positive on items assessing core symptoms of depression, i.e., sadness and loss of pleasure 43); depression (BDI-II score ≥ 20); anxiety (Z-SAS score ≥ 60); subthreshold anxiety (Z-SAS score between 45 and 59 43); emotional symptoms (SDQ subscale ≥ 7); conduct problems (SDQ subscale ≥ 5); hyperactivity (SDQ subscale ≥ 7); peer problems (SDQ subscale ≥ 6), lack of prosocial behavior (SDQ subscale ≤ 4); non-suicidal self-injury (DSHI score ≥ 3); suicidal ideation (positive on at least one PSS item); and suicide attempter (lifetime history of suicide attempts). All psychopathological measures, with the exception of lifetime suicide attempt, referred to the past two weeks. All measures regarding risk behaviors and psychopathology were further stratified by gender and age. On the basis of the recruited sample, three age groups were identified: 14 years or less (n=4,007), 15 years (n=5,350), 16 years or more (n=2,955).
A chi-square test of independence was used to statistically define the differences between genders and age groups for socio-demographics, risk behaviors and psychopathology.
Latent class analysis (LCA) was applied without any a priori assumption about the nature of the latent categorization, thus identifying and characterizing clusters of pupils with similar risk behavior profiles. In order to account for the effect of age on different risk behaviors, a latent class logistic regression (LCLR) test was used with age as a covariate 44. The LCLR models were fitted starting with a two-class model, increasing the number of classes up to four. The Bayesian information criterion (BIC) was compared across models. The lowest BIC was used to identify the most parsimonious and best fitting model. LCLR was applied to the nine risk behaviors in a subsample of 9,035 pupils with no missing information for any risk behaviors. A chi-square test was used to identify significant differences in the socio-demographic and psychopathology variables between the different latent classes of risk identified by the LCA.
A multivariate multinomial logistic regression model adjusted for gender and age group was developed to describe the relationship between belonging to a latent class, selected as the dependent variable, and levels of psychopathology.
For all analyses, a critical value of p<0.05 was considered to be statistically significant. All statistical analyses were run in STATA IC 9.0 for Windows.
RESULTS
Risk behaviors
The prevalence of the nine identified areas of risk behaviors is reported in Table1.
Table 1.
Prevalence (%) of risk behaviors in the adolescent sample
| 14 years and below (n=4,007) |
15 years (n=5,350) |
16 years and above (n=2,955) |
All age groups (n=12,328) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n=1,833) | Female (n=2,167) | Both genders | Male (n=2,183) | Female (n=3,160) | Both genders | Male (n=1,490) | Female (n=1,456) | Both genders | Male (n=5,529) | Female (n=6,799) | Both genders | |
| Excessive alcohol use | 6.4* | 4.1 | 5.2** | 10.0* | 5.3 | 7.3 | 17.7* | 10.2 | 14.1 | 10.9* | 6.0 | 8.2 |
| Illegal drug use | 3.2* | 2.0 | 2.6** | 5.8* | 2.7 | 3.9 | 8.6 | 7.8 | 8.2 | 5.7* | 3.6 | 4.5 |
| Heavy smoking | 4.6 | 6.1 | 5.4** | 10.5* | 8.0 | 9.0 | 25.0* | 16.7 | 21.0 | 12.4* | 9.2 | 10.7 |
| Reduced sleep | 9.7* | 14.6 | 12.3** | 11.4* | 17.6 | 15.1 | 19.9 | 21.4 | 20.7 | 13.1* | 17.4 | 15.5 |
| Overweight | 4.8* | 2.5 | 3.5** | 5.4* | 1.6 | 3.1 | 6.1* | 2.3 | 4.2 | 5.4* | 2.0 | 3.5 |
| Underweight | 3.0 | 2.8 | 2.9 | 3.6 | 2.4 | 2.9 | 4.1 | 3.4 | 3.8 | 3.5 | 2.8 | 3.1 |
| Sedentary behavior | 9.4* | 16.8 | 13.5** | 14.2* | 23.4 | 19.6 | 17.7* | 29.3 | 23.5 | 13.6* | 22.6 | 18.5 |
| High media use | 10.8* | 7.2 | 8.8** | 10.6* | 8.8 | 9.6 | 14.1* | 11.3 | 12.7 | 11.7* | 8.8 | 10.1 |
| Truancy | 2.8* | 1.9 | 2.3** | 4.2* | 2.3 | 3.1 | 9.3* | 4.5 | 7.0 | 5.1* | 2.6 | 3.8 |
Significant difference between males and females of the same age (p<0.05),
significant difference across ages in both genders (p<0.05)
Less than ten percent (8.2%) of adolescents reported drinking alcohol at least twice a week. More than one-third (35.9%) of those who reported drinking had at least three drinks in one sitting; 14.2% reported having experienced being “really drunk”, and 7.7% reported having had a hangover. Alcohol use was higher among males and increased significantly with age.
Less than five percent (4.5%) of the total sample reported having used illegal drugs three times or more during their lifetime. Illegal drug use was higher among males and increased with age. More than ten percent (10.7%) of the sample reported smoking at least 5 cigarettes per day and more than forty-five percent (45.8%) reported smoking cigarettes at least once in their lifetime. Slightly more than ten percent (10.3%) of the sample reported having started smoking when they were eleven years old or younger.
More than fifteen percent (15.5%) of the adolescents reported sleeping 6 hours per day or less. Reduced sleep was more frequent among females and among older age pupils. More than forty percent (41.8%) reported sleeping less than 8 hours per day; slightly more than one-third (34.2%) reported waking up often or being always tired in the morning, a finding significantly more common among females (37.1% vs. 31.7%, p <0.05); approximately twenty-five percent (25.4%) of adolescents reported the habit of taking a nap in the afternoon, with a statistically significant higher prevalence among females than males (27.8% vs. 23.4%, p <0.05).
More than three percent (3.5%) of pupils had a BMI above the 95th percentile for age 42, with the prevalence of overweight being higher among males and increasing with age. Three percent (3.1%) of adolescents had a BMI below the 5th percentile for age 42, with no significant gender or age differences. More than one fourth (26.5%) of the sample did not regularly have breakfast, a behavior significantly more common in females than males (30.8% vs. 21.2%, p<0.05). Six percent (6.1%) reported never eating fruit or vegetables, while 62.5% reported eating them at least once every day. Less than twenty percent (18.5%) reported performing physical activity less than once a week. Sedentary behavior was more common among females and increased with age. More than two thirds (68.8%) of the adolescents reported performing sports on a regular basis, with a significant gender difference (77.3% males vs. 61.8% females, p<0.05).
Approximately ten percent (10.1%) of the adolescents reported spending at least 5 hours per day watching TV, playing videogames or surfing the Internet for reasons not related to school or work. This percentage was significantly higher in males and increased with age. Almost seventy-five percent (74.5%) of the adolescents reported using their own computer to surf the Internet, while 2.5% of the sample reported having never used the Internet.
Less than four percent (3.8%) of the adolescents reported often missing school without permission. This behavior was significantly more frequent among older pupils and among males. Ten percent (10.4%) reported having been in a physical fight in the past 12 months and almost half of them (45.2%) reported having started the fight. Approximately one-sixth (16.9%) of the pupils reported having been a passenger in a vehicle with a driver who had been drinking. Ten percent of the 14-year olds, 19% of the 15-year olds and 42.9% of the 16-year olds reported having had a sexual intercourse, with a significantly higher prevalence among males in each age group. Less than four percent (3.3%) of those engaging in sexual intercourse reported never or seldom having used a condom, with no significant age differences.
Psychiatric symptoms
The prevalence of psychiatric symptoms is reported in Table2.
Table 2.
Prevalence (%) of psychiatric symptoms in the adolescent sample
| 14 years and below (n=4.007) |
15 years (n=5.350) |
16 years and above (n=2.955) |
All age groups (n=12.328) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n=1,833) | Female (n=2,167) | Both genders | Male (n=2,183) | Female (n=3,160) | Both genders | Male (n=1,490) | Female (n=1,456) | Both genders | Male (n=5,529) | Female (n=6,799) | Both genders | |
| Subthreshold depression | 25.7* | 32.0 | 29.1** | 24.8* | 35.4 | 31.1 | 27.1* | 35.0 | 31.0 | 25.8 | 34.2 | 30.4 |
| Depression | 3.8* | 9.2 | 6.7** | 4.2* | 10.6 | 8.0 | 7.4* | 12.8 | 10.1 | 4.9 | 10.6 | 8.1 |
| Subthreshold anxiety | 14.0* | 26.6 | 20.8** | 14.7* | 30.8 | 24.2 | 19.7* | 31.1 | 25.3 | 15.8 | 29.5 | 23.3 |
| Anxiety | 1.6* | 4.6 | 3.2** | 2.4* | 6.9 | 5.1 | 3.2* | 8.8 | 6.0 | 2.3 | 6.6 | 4.7 |
| Emotional symptoms | 3.0* | 9.9 | 6.7** | 2.3* | 11.0 | 7.4 | 4.3* | 13.6 | 8.9 | 3.0 | 11.2 | 7.5 |
| Conduct problems | 10.7* | 7.5 | 9.0** | 11.4* | 8.6 | 9.8 | 16.1* | 9.3 | 12.7 | 12.5 | 8.4 | 10.3 |
| Hyperactivity | 10.9 | 9.1 | 9.9 | 8.6 | 9.0 | 8.8 | 9.6 | 9.8 | 9.6 | 9.6 | 9.2 | 9.4 |
| Peer problems | 3.1 | 2.7 | 2.9** | 3.7* | 2.7 | 3.1 | 7.0* | 3.3 | 5.1 | 4.4 | 2.9 | 3.6 |
| Lack of prosocial behavior | 9.5* | 3.1 | 6.0** | 9.9* | 4.0 | 6.5 | 12.7* | 4.7 | 8.7 | 10.6 | 3.9 | 6.9 |
| Non-suicidal self-injury | 6.8* | 10.7 | 8.9** | 7.6 | 8.8 | 8.3 | 9.7 | 12.2 | 11.0 | 7.9 | 10.2 | 9.1 |
| Suicidal ideation | 21.2* | 35.4 | 28.9** | 23.5* | 39.3 | 32.8 | 30.1* | 42.5 | 36.2 | 24.5 | 38.7 | 32.3 |
| Suicide attempts | 2.2* | 4.2 | 3.3** | 2.8* | 4.7 | 3.9 | 4.1* | 7.5 | 5.8 | 3.0 | 5.1 | 4.2 |
Significant difference between males and females of the same age (p<0.05),
significant difference across ages in both genders (p<0.05)
Approximately one third (30.4%) of pupils experienced subthreshold depression, with girls having a significantly higher prevalence than boys (34.2% vs. 25.8%, p<0.05). Approximately eight percent (8.1%) of the sample was categorized as depressed, with a significantly higher prevalence in females (10.6% vs. 4.9%, p<0.05). The prevalence of depressive symptoms increased with age.
More than twenty percent (23.3%) of pupils experienced subthreshold anxiety, with the prevalence increasing with age and being significantly higher among females (29.5% vs. 15.8%, p<0.05). Almost five percent (4.7%) of pupils reported severe to extreme anxiety, with the prevalence increasing with age and being significantly higher among girls (6.6% vs. 2.3%, p<0.05).
Emotional symptoms were reported by 7.5% of the sample. Their prevalence increased with age and was significantly higher among girls (11.2% vs. 3.0%, p<0.05).
Conduct problems occurred in 10.3% of the sample. Their prevalence increased with age and was significantly higher among boys (12.5% vs. 8.4%, p<0.05). Symptoms of hyperactivity were present in 9.4% of the pupils and did not differ significantly by gender.
More than three percent (3.6%) of the sample experienced peer problems; the prevalence increased with age and was significantly higher among boys (4.4% vs. 2.9%, p<0.05). Nearly seven percent (6.9%) of the sample reported lack of prosocial behavior; the prevalence increased with age and was significantly higher among boys (10.6% vs. 3.9%, p<0.05).
Suicidal ideation was present in approximately one third of the sample (32.3%), with a significantly higher prevalence in older pupils and among girls (38.7% vs. 24.5%, p<0.05). More than four percent (4.2%) of the sample reported attempting suicide during their lifetime, with a significantly higher prevalence among girls (5.1% vs. 3.0%, p<0.05). The frequency of suicide attempts for both genders increased with age.
Classes identified through LCA and their correlates
LCLR models were fitted to the nine risk behaviors reported above. A three-class model best fit the data. Figure 1 presents the patterns of response probability profiles for each of the three classes. The first class (“low-risk”), comprising 57.8% of the sample (M/F=2,557/3,497), included students with no or very low frequency of risk behaviors. The second class (“high-risk”), comprising 13.2% of the sample (M/F=622/562), included pupils who scored high on all risk behaviors. The third class, comprising 29% of the sample (M/F=687/1,109), included pupils who were positive for high media use, sedentary behavior and reduced sleep. This class was labelled “invisible risk”, as these behaviors are generally not obvious or recognized by observers, including parents and teachers, to be associated with mental health problems.
Figure 1.
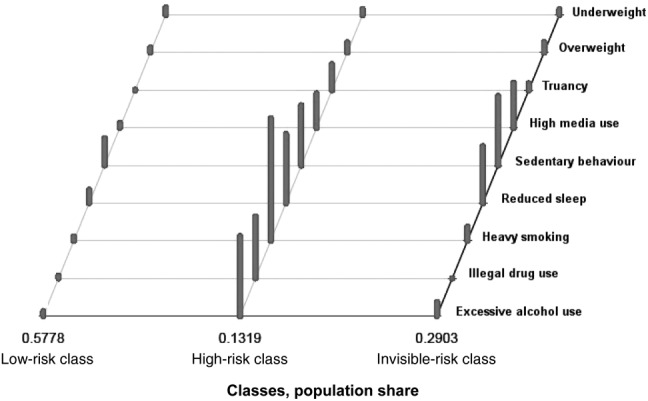
Results of the latent class analysis
Table3 describes the relationship between the classes identified through LCA and socio-demographic variables. The percentage of pupils not born in the study site country was significantly higher in the high-risk compared to both the invisible- and the low-risk groups (10.0% vs. 6.9% and 4.8%, p<0.05). A similar pattern was observed for pupils with parents not born in the study site country. Having someone in the family who had lost his/her job during the previous year was significantly more frequent in the high- and invisible-risk groups than in the low-risk one (11.6% and 12.1% vs. 8.3%, p<0.05). Living with a single parent was significantly more frequent in the high-risk than in the invisible-risk group (31.1% vs. 23.6%, p<0.05).
Table 3.
Socio-demographic features (%) by latent class risk groups
| Socio-demographic features | Low-risk class n=6,054 (M/F=2,557/3,497) | High-risk class n=1,184 (M/F=622/562) | Invisible-risk class, n=1,796 (M/F=687/1,109) |
|---|---|---|---|
| Females* | 57.8 | 47.5 | 61.8 |
| Not born in the country* | 4.8 | 10.0 | 6.9 |
| Parents not born in the country* | 15.1 | 27.0 | 20.6 |
| Doesn't belong to a religious denomination | 31.2 | 34.0 | 31.3 |
| Someone in your family lost job last year** | 8.3 | 11.6 | 12.1 |
| Single parent household* | 17.5 | 31.1 | 23.6 |
The three groups differ significantly from each other (p<0.05),
the high-risk and the invisible-risk groups differ significantly from the low-risk group (p< 0.05)
As shown in Table4, the prevalence of depressive and anxiety symptoms (both severe and subthreshold) and of suicidal ideation was very similar in the invisible- and the high-risk groups, and significantly higher in each of these groups compared with the low-risk one (p<0.05). Emotional symptoms and peer problems were significantly more prevalent in the invisible-risk than in the high-risk group, and more frequent in both these groups than in the low-risk one (p<0.05). Conduct problems, hyperactivity, non-suicidal self-injury and lifetime suicide attempts were significantly more prevalent in the high-risk group compared with both the invisible- and the low-risk ones (p<0.05).
Table 4.
Psychiatric symptoms (%) by latent class risk groups
| Psychiatric symptoms | Low-risk class, n=6,054 (M/F=2,557/3,497) | High-risk class, n=1,184 (M/F=622/562) | Invisible-risk class, n=1,796 (M/F=687/1,109) |
|---|---|---|---|
| Subthreshold depression** | 29.4 | 34.0 | 33.2 |
| Depression** | 4.2 | 14.7 | 13.4 |
| Subthreshold anxiety** | 19.0 | 31.3 | 31.0 |
| Anxiety** | 2.5 | 9.2 | 8.0 |
| Emotional symptoms* | 5.8 | 9.0 | 11.6 |
| Conduct problems* | 6.4 | 23.2 | 11.5 |
| Hyperactivity* | 6.1 | 18.6 | 11.8 |
| Peer problems*** | 2.3 | 3.0 | 5.0 |
| Lack of prosocial behavior** | 4.5 | 9.9 | 8.1 |
| Non-suicidal self-injury* | 5.5 | 22.3 | 12.4 |
| Suicidal ideation** | 27.1 | 44.0 | 42.2 |
| Suicide attempter* | 1.7 | 10.1 | 5.9 |
The three groups differ significantly from each other (p<0.05),
the high-risk and the invisible-risk groups differ significantly from the low-risk group (p< 0.05),
the low-risk and the invisible-risk groups differ significantly from the high-risk group (p<0.05)
Multivariate multinomial logistic regression
Results from the multivariate multinomial logistic regression model of psychiatric symptoms and latent classes, adjusted for gender and age, are presented in Table5. Symptoms of depression, anxiety, lack of prosocial behavior and suicidal ideation were associated with significant and similarly increased relative risk ratios of being in both the invisible- and the high-risk groups. Having symptoms of hyperactivity, non-suicidal self-injury or having attempted suicide were associated with significantly increased relative risk ratios of being in the high-risk group and, even if at a lower level, of being in the invisible-risk group.
Table 5.
Results of multivariate multinomial logistic regression of latent class variables by gender, age group and psychopathological scores (n=8,579)
| Invisible-risk vs. low-risk class | High-risk vs. low-risk class | |
|---|---|---|
| RRR (95% CI) | RRR (95% CI) | |
| Gender (male/female) | 0.95 (0.84, 1.08) | 0.51* (0.44, 0.60) |
| Age group 15 years/14 years or younger | 2.41* (2.08, 2.79) | 4.50* (3.55, 5.69) |
| Age group 16 years or older/14 years or younger | 7.88* (6.67, 9.30) | 27.62* (21.66, 35.23) |
| Subthreshold depression | 1.10 (0.96, 1.27) | 1.21* (1.02, 1.43) |
| Depression | 1.97* (1.50, 2.58) | 1.82* (1.30, 2.53) |
| Subthreshold anxiety | 1.62* (1.40, 1.88) | 1.58* (1.32, 1.90) |
| Anxiety | 1.81* (1.31, 2.52) | 1.93* (1.31, 2.86) |
| Emotional symptoms | 0.80 (0.63, 1.02) | 0.47* (0.34, 0.65) |
| Conduct problems | 1.24 (1.00, 1.52) | 2.74* (2.21, 3.40) |
| Hyperactivity | 1.59* (1.29, 1.95) | 2.49* (1.99, 3.13) |
| Peer problems | 1.23 (0.89, 1.70) | 0.47* (0.29, 0.74) |
| Lack of prosocial behavior | 1.60* (1.26, 1.74) | 1.54* (1.17, 2.03) |
| Non-suicidal self-injury | 1.40* (1.13, 1.74) | 2.99* (2.37, 3.79) |
| Suicidal ideation | 1.29* (1.12, 1.48) | 1.30* (1.09, 1.55) |
| Suicide attempter | 1.69* (1.22, 2.35) | 2.62* (1.83, 3.74) |
RRR – relative risk ratio,
p=0.05 (two-tailed tests)
DISCUSSION
The results of this study indicate that the prevalence of risk behaviors and psychopathology among European adolescents is relatively high. Almost all studied risk behaviors show an increase with age and most of them are significantly more frequent among boys. The only exceptions are sedentary behavior and reduced sleep, which are more frequent among girls, who also have more internalizing (emotional) psychiatric symptoms, such as depression, anxiety and suicidal ideation.
In this large sample, LCA identified three groups of adolescents. The first group, representing 13.2% of the adolescents, scored high on all examined risk behaviors and can be called “high-risk group”. Most interventions today target this population 45,46. The largest group, comprising almost two thirds (57.8%) of the adolescents, scored low on most risk behaviors and has accordingly been called “low-risk group”. Even pupils in this low-risk group, however, reported suicide attempts (1.7%), suicidal ideation (27%), subthreshold depression (29%) and subthreshold anxiety (19%). These findings highlight the need for large-scale preventive interventions and outreach in schools, as reported in previous studies 43,47.
Most importantly, this study also identified, for the first time, a third group labelled the “invisible-risk” group, which includes 29% of the adolescents. These pupils clustered on three specific risk behaviors (reduced sleep, low physical activity and high media use), while simultaneously having significantly increased prevalence of psychiatric symptoms. The level of psychiatric symptoms found in this “invisible” group is, in many cases, very similar to the high-risk group. The group includes adolescents who spend an excessive amount of time watching TV, being on the Internet or playing videogames, including going to sleep late in order to prolong the use of these media activities and who, perhaps as a direct consequence, neglect other healthy activities such as sports. Adult observers (e.g., parents, teachers and mental health professionals) do not generally perceive these behaviors as particularly harmful or reasons for concern. Nevertheless, the high- and the invisible-risk groups have a very similar prevalence of depressive symptoms, anxiety symptoms and suicidal thoughts. In comparison with pupils in the high-risk group, those in the invisible-risk group have a higher prevalence of emotional symptoms and peer problems but a lower prevalence of conduct problems and hyperactivity. The differences between the high- and invisible-risk groups do not depend on gender representation in these groups, as multivariate analyses indicated that these associations remained significant when adjusting for age and gender.
Adolescents in the invisible- and high-risk groups have different patterns compared with the low-risk group concerning country of origin (adolescent or one of his/her parents born outside study site country), belonging to a single parent household, or a family where a parent lost his/her job in the previous year. Interestingly, belonging to a religious denomination (as perceived by adolescents), which is generally considered protective 48, did not confer any difference in risk group membership. These findings suggest that adolescents in the invisible group may more likely have a lower socioeconomic status and thus, perhaps, be even more invisible to existing interventions and outreach activities.
A major strength of this study is the large sample of adolescents (n=12,395), recruited from randomly selected schools across study sites in eleven European countries, which are reasonably representative of the respective European country 34. The students were recruited and evaluated with homogeneous procedures across countries in terms of inclusion and exclusion criteria and outcome measures. Furthermore, the study comprised a very large geographic area. One potential limitation of this study is that all data were collected through self-report. Although it has been shown that data acquired through self-report are reasonably reliable 36,49,50, the prevalence of risk behaviors and psychopathology may have been underestimated. Another limitation is that only one site per country was chosen for study participation. Even though study sites were shown to be reasonably representative of the respective country, inclusion of more than one site per country might have improved representation of the urban and rural areas and possibly allowed stratification of risk groups by population density.
The results of this study are in agreement with the classical distinction between internalizing and externalizing disorders 51, with the former (emotional) being more common among girls and the latter (behavioral) among boys. Similar patterns of age- and gender- related differences have been previously reported in American studies, such as the Study of Disruptive Behavior Disorders in Puerto Rican Youth 5, the NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study 13 and the YRBSS 15. Until now, investigations conducted in Europe, such as the ESPAD study 26, focused exclusively on substance abuse and did not include a wider range of risk behaviors as in the SEYLE study. Regarding substance abuse, however, SEYLE results are in line with previous findings, confirming the high burden of substance abuse among European adolescents and its relationship with various types of psychopathology 52. In general, SEYLE results indicate that it would be a great advantage to establish within Europe a system to routinely collect data regarding adolescents' mental health and lifestyles, as regularly done in the United States with the YRBSS.
Because specific age- and gender-related differences change over time, monitoring them may have important implications for the prevention of risk behaviors. The increase in risk behaviors and psychopathology by age, as observed in this study, is very steep but in agreement with other investigations 53,54. Importantly, in the SEYLE data, a simultaneous increase in the prevalence of each assessed risk behavior was observed for each single increase in years of age. However, data about the longitudinal life-time trajectory of these risk behaviors and their predictive value and potential consequences for subsequent psychopathological and psychosocial outcomes are not yet available. Nonetheless, the cross-sectional correlations between the high- and invisible-risk groups and psychopathological variables, as presented here, warrant the development of systematic psychosocial support and intervention for these pupils.
In summary, the results of this study confirm the need for early prevention and intervention in the mental health field 55,56. The most common risk behaviors among girls are a reduced number of hours of sleep and a sedentary lifestyle, while drug and alcohol use are more common among boys. Thus, preventive interventions should be tailored specifically for boys and girls. The most important findings of this study arise from the LCA. In addition to the classical low- and high- risk groups, we identified a third group, accounting for almost one third of the adolescents, who engage in behaviors that are easily overlooked as they are generally not perceived by adults, including mental health professionals, as troublesome. Pupils in this invisible-risk group show high rates of depression, anxiety and suicidal ideation, which are at the same level as among pupils belonging to the high-risk group. While most parents, teachers and clinicians would react to an adolescent using drugs or getting drunk, they may easily overlook adolescents engaging in unobtrusive behaviors such as watching too much TV, not playing sports, or sleeping too little. The causality of the relationships between these risk behaviors and psychopathology remains unclear. However, common psychiatric disorders, such as depression, are already known to often show bidirectional relationships with reduced sleep 57, low levels of activity 58 and high media consumption 59. Thus, our findings have implications for gatekeepers delivering information and education about adolescent health and lifestyle to pupils and parents, as well as for policy makers and clinicians. While discussions with adolescents often focus on substance abuse and delinquency, the risk behaviors identified here need to be considered, and special attention given to encouraging sufficient sleep, participation in sports and using new media moderately.
These data afforded a unique opportunity to profile typical schools throughout Europe serving regular pupils. However, a number of unanswered questions remain. For example, not having more specific individual socio-economic data on the participating adolescents precluded better identification of the relationship of these factors with risk behaviors and psychiatric symptoms. An epidemiologic household study should be conducted, including detailed socio-economic data collection, to help explore the correlations between psychopathology, risk behaviors and the general socio-economic status. Moreover, this study evaluated psychiatric symptoms cross-sectionally in the general population through psychometric self-report instruments. Diagnostic interviews would allow a better understanding of the relationship between psychiatric disorders and risk behaviors.
Regardless of these limitations, the SEYLE study established an important multi-national cohort of European adolescents that ideally will be studied longitudinally, in order to identify the trajectories from risk behaviors to psychopathology and thus help to elucidate causality. Such a study would also allow for the assessment of the course and prognostic trajectories of various adolescent risk behaviors.
Acknowledgments
The SEYLE project is supported through Coordination Theme 1 (Health) of the European Union Seventh Framework Program (FP7), grant agreement HEALTH-F2-2009-223091.
References
- 1.Blum RW, Bastos FI, Kabiru CW, et al. Adolescent health in the 21st century. Lancet. 2012;379:1567–8. doi: 10.1016/S0140-6736(12)60407-3. [DOI] [PubMed] [Google Scholar]
- 2.Patton GC, Coffey C, Cappa C, et al. Health of the world's adolescents: a synthesis of internationally comparable data. Lancet. 2012;379:1665–75. doi: 10.1016/S0140-6736(12)60203-7. [DOI] [PubMed] [Google Scholar]
- 3.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication – Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaffer D, Fisher P, Dulcan MK, et al. The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study. Methods for the Epidemiology of Child and Adolescent Mental Disorders Study. J Am Acad Child Adolesc Psychiatry. 1996;35:865–77. doi: 10.1097/00004583-199607000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Bird HR, Davies M, Duarte CS, et al. A study of disruptive behavior disorders in Puerto Rican youth: II. Baseline prevalence, comorbidity, and correlates in two sites. J Am Acad Child Adolesc Psychiatry. 2006;45:1042–53. doi: 10.1097/01.chi.0000227879.65651.cf. [DOI] [PubMed] [Google Scholar]
- 6.Costello EJ, Angold A, Burns BJ, et al. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53:1129–36. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 7.Jiang N, Kolbe LJ, Seo DC, et al. Health of adolescents and young adults: trends in achieving the 21 Critical National Health Objectives by 2010. J Adolesc Health. 2011;49:124–32. doi: 10.1016/j.jadohealth.2011.04.026. [DOI] [PubMed] [Google Scholar]
- 8.Park MJ, Brindis CD, Chang F, et al. A midcourse review of the healthy people 2010: 21 critical health objectives for adolescents and young adults. J Adolesc Health. 2008;42:329–34. doi: 10.1016/j.jadohealth.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197:378–85. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merikangas KR, Zhang H, Avenevoli S, et al. Longitudinal trajectories of depression and anxiety in a prospective community study: the Zurich Cohort Study. Arch Gen Psychiatry. 2003;60:993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- 11.Bird HR, Canino GJ, Davies M, et al. A study of disruptive behavior disorders in Puerto Rican youth: I. Background, design, and survey methods. J Am Acad Child Adolesc Psychiatry. 2006;45:1032–41. doi: 10.1097/01.chi.0000227878.58027.3d. [DOI] [PubMed] [Google Scholar]
- 12.Johnson JG, Cohen P, Gould MS, et al. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Arch Gen Psychiatry. 2002;59:741–9. doi: 10.1001/archpsyc.59.8.741. [DOI] [PubMed] [Google Scholar]
- 13.Lahey BB, Flagg EW, Bird HR, et al. The NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study: background and methodology. J Am Acad Child Adolesc Psychiatry. 1996;35:855–64. doi: 10.1097/00004583-199607000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Merikangas K, Avenevoli S, Costello J, et al. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48:367–9. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brener ND, Kann L, Shanklin S, et al. Methodology of the Youth Risk Behavior Surveillance System – 2013. MMWR Recomm Rep. 2013;62:1–23. [PubMed] [Google Scholar]
- 16.Eaton DK, Kann L, Kinchen S, et al. Youth Risk Behavior Surveillance – United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 17.Hu MC, Griesler P, Schaffran C, et al. Risk and protective factors for nicotine dependence in adolescence. J Child Psychol Psychiatry. 2011;52:1063–72. doi: 10.1111/j.1469-7610.2010.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu P, Bird HR, Liu X, et al. Childhood depressive symptoms and early onset of alcohol use. Pediatrics. 2006;118:1907–15. doi: 10.1542/peds.2006-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kandel DB, Johnson JG, Bird HR, et al. Psychiatric comorbidity among adolescents with substance use disorders: findings from the MECA Study. J Am Acad Child Adolesc Psychiatry. 1999;38:693–99. doi: 10.1097/00004583-199906000-00016. [DOI] [PubMed] [Google Scholar]
- 20.McCrea RL, Berger YG, King MB. Body mass index and common mental disorders: exploring the shape of the association and its moderation by age, gender and education. Int J Obes. 2012;36:414–21. doi: 10.1038/ijo.2011.65. [DOI] [PubMed] [Google Scholar]
- 21.Anderson SE, Cohen P, Naumova EN, et al. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. 2007;69:740–7. doi: 10.1097/PSY.0b013e31815580b4. [DOI] [PubMed] [Google Scholar]
- 22.Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. 2011;45:886–95. doi: 10.1136/bjsports-2011-090185. [DOI] [PubMed] [Google Scholar]
- 23.Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug Alcohol Depend. 2001;64:1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 24.Berg I. Absence from school and mental health. Br J Psychiatry. 1992;161:154–66. doi: 10.1192/bjp.161.2.154. [DOI] [PubMed] [Google Scholar]
- 25.Hale DR, Viner RM. Policy responses to multiple risk behaviours in adolescents. J Public Health. 2012;34(Suppl. 1):i11–9. doi: 10.1093/pubmed/fdr112. [DOI] [PubMed] [Google Scholar]
- 26.Hibell B, Ahlstrom S, Balakireva O, et al. The 2007 ESPAD report: substance use among students in 35 European countries. Stockholm: Swedish Council for Information on Alcohol and Other Drugs; 2009. [Google Scholar]
- 27. European Monitoring Centre for Drugs and Drug Addiction. Annual report 2008: the state of the drugs problem in Europe. http://www.emcdda.europa.eu.
- 28.Flisher AJ, Kramer RA, Hoven CW, et al. Risk behavior in a community sample of children and adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39:881–7. doi: 10.1097/00004583-200007000-00017. [DOI] [PubMed] [Google Scholar]
- 29.Harakeh Z, Looze de ME, Schrijvers CT, et al. Individual and environmental predictors of health risk behaviours among Dutch adolescents: the HBSC study. Public Health. 2012;126:566–73. doi: 10.1016/j.puhe.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 30.Johnson KE, Taliaferro LA. Health behaviors and mental health of students attending alternative high schools: a review of the research literature. J Spec Pediatr Nurs. 2012;17:79–97. doi: 10.1111/j.1744-6155.2011.00311.x. [DOI] [PubMed] [Google Scholar]
- 31.Kim Y. Adolescents' health behaviours and its associations with psychological variables. Cent Eur J Public Health. 2011;19:205–9. doi: 10.21101/cejph.a3694. [DOI] [PubMed] [Google Scholar]
- 32.Zhou Z, Xiong H, Jia R, et al. The risk behaviors and mental health of detained adolescents: a controlled, prospective longitudinal study. PLoS One. 2012;7:e37199. doi: 10.1371/journal.pone.0037199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wasserman D, Carli V, Wasserman C, et al. Saving and empowering young lives in Europe (SEYLE): a randomized controlled trial. BMC Public Health. 2010;10:192. doi: 10.1186/1471-2458-10-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carli V, Wasserman C, Wasserman D, et al. The Saving and Empowering Young Lives in Europe (SEYLE) Randomized Controlled Trial (RCT): methodological issues and participant characteristics. BMC Public Health. 2013;13:479. doi: 10.1186/1471-2458-13-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. World Health Organization. Global School-Based Student Health Survey. http://www.who.int.
- 36.Brener ND, Kann L, McManus T, et al. Reliability of the 1999 Youth Risk Behavior Survey questionnaire. J Adolesc Health. 2002;31:336–42. doi: 10.1016/s1054-139x(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 37.Beck AT, Steer RA, Ball R, et al. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588–97. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 38.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–9. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 39.Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7:125–30. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- 40.Paykel ES, Myers JK, Lindenthal JJ, et al. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–9. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 41.Gratz K. Measurement of deliberate self-harm: preliminary data on the Deliberate Self-Harm Inventory. J Psychopathol Behav Assess. 2001;23:253–63. [Google Scholar]
- 42.WHO Multicentre Growth Reference Study Group. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. Geneva: World Health Organization; 2006. [Google Scholar]
- 43.Balazs J, Miklosi M, Kereszteny A, et al. Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. J Child Psychol Psychiatry. 2013;54:670–7. doi: 10.1111/jcpp.12016. [DOI] [PubMed] [Google Scholar]
- 44.Linzer DA, Lewis JB. poLCA: An R package for polytomous variable latent class analysis. J Stat Softw. 2011;42:1–29. [Google Scholar]
- 45.Jackson CA, Henderson M, Frank JW, et al. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. J Public Health. 2012;34(Suppl. 1):i31–40. doi: 10.1093/pubmed/fdr113. [DOI] [PubMed] [Google Scholar]
- 46.Yuma-Guerrero PJ, Lawson KA, Velasquez MM, et al. Screening, brief intervention, and referral for alcohol use in adolescents: a systematic review. Pediatrics. 2012;130:115–22. doi: 10.1542/peds.2011-1589. [DOI] [PubMed] [Google Scholar]
- 47.Olsson GI, Knorring von AL. Adolescent depression: prevalence in Swedish high-school students. Acta Psychiatr Scand. 1999;99:324–31. doi: 10.1111/j.1600-0447.1999.tb07237.x. [DOI] [PubMed] [Google Scholar]
- 48.Mouttapa M, Huang TT, Shakib S, et al. Authority-related conformity as a protective factor against adolescent health risk behaviors. J Adolesc Health. 2003;33:320–1. doi: 10.1016/s1054-139x(03)00252-0. [DOI] [PubMed] [Google Scholar]
- 49.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003;33:436–57. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 50.Brener ND, Grunbaum JA, Kann L, et al. Assessing health risk behaviors among adolescents: the effect of question wording and appeals for honesty. J Adolesc Health. 2004;35:91–100. doi: 10.1016/j.jadohealth.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 51.Achenbach TM. The Child Behavior Profile: I. Boys aged 6-11. J Consult Clin Psychol. 1978;46:478–88. doi: 10.1037//0022-006x.46.3.478. [DOI] [PubMed] [Google Scholar]
- 52.Kokkevi A, Richardson C, Florescu S, et al. Psychosocial correlates of substance use in adolescence: a cross-national study in six European countries. Drug Alcohol Depend. 2007;86:67–74. doi: 10.1016/j.drugalcdep.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 53.Barone C, Weissberg RP, Kasprow WJ, et al. Involvement in multiple problem behaviors of young urban adolescents. J Prim Prev. 1995;15:261–83. doi: 10.1007/BF02197475. [DOI] [PubMed] [Google Scholar]
- 54.Brodbeck J, Bachmann MS, Croudace TJ, et al. Comparing growth trajectories of risk behaviors from late adolescence through young adulthood: an accelerated design. Dev Psychol. 2013;49:1732–8. doi: 10.1037/a0030873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stenbacka M, Stenbacka M, Stattin H, et al. Adolescent use of illicit drugs and adult offending: a Swedish longitudinal study. Drug and Alcohol Review. 2007;26:397–403. doi: 10.1080/09595230701373875. [DOI] [PubMed] [Google Scholar]
- 56.Lier van PAC, Huizink A, Crijnen A. Impact of a preventive intervention targeting childhood disruptive behavior problems on tobacco and alcohol initiation from age 10 to 13 years. Drug and Alcohol Dependence. 2009;100:228–33. doi: 10.1016/j.drugalcdep.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 57.Clarke G, Harvey AG. The complex role of sleep in adolescent depression. Child Adolesc Psychiatr Clin N Am. 2012;21:385–400. doi: 10.1016/j.chc.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Biddle SJ, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. 2011;45:886–95. doi: 10.1136/bjsports-2011-090185. [DOI] [PubMed] [Google Scholar]
- 59.Carli V, Durkee T, Wasserman D, et al. The association between pathological internet use and comorbid psychopathology: a systematic review. Psychopathology. 2013;46:1–13. doi: 10.1159/000337971. [DOI] [PubMed] [Google Scholar]


