Abstract
The objective of this paper was that fine-needle aspiration (FNA) has become a well-liked modality in the diagnosis, staging, and follow-up of head and neck masses. Limited studies exist regarding the value of FNA in the diagnosis of head and neck masses. We aimed to evaluate the diagnostic value of head and neck lymphomas. This cross-sectional study method was performed in Imam Hospital and Cancer Institute affiliated to Tehran University of Medical Sciences. In a 5 years period between January 2006 and June 2010, we enrolled all patients with cervical mass (es) who had undergone FNA as the primary diagnostic modality and then underwent biopsy (excisional or open). Results of FNA were compared with histopathological study as a gold standard method. Finally, 47 patients were recruited. It was found that FNA had a sensitivity of 88% (CI 95% = 79–97), a specificity of 81.2% (CI 95% = 70–92), a positive predictive value of 84.6% (CI 95% = 75–95), a negative predictive value of 85.7% (CI 95% = 77–95) and an accuracy of 85.1% (CI 95% = 75–95) in the diagnosis of head and neck lymphoma. We conclude that FNA has a considerable value in differentiation of head and neck lymphoma from non-lymphoma etiologies and is recommended as a screening test for the diagnosis of head and neck lymphoma.
Keywords: Fine aspiration, Lymphoma, Head and neck mass, Cervical mass
Introduction
In the recent decade, fine-needle aspiration (FNA) has become a well-liked modality in the diagnosis, staging and follow-up of head and neck masses [1, 2]. Lymphoma is one of the major causes of head and neck masses and has a high prevalence in Iran [3, 4]. Although, the gold standard method for the diagnosis of lymph node lesions is histopathology, it needs general or local anesthesia in order for the biopsy or surgery to be performed. Moreover, besides the need for the operation room setting, higher costs and being time consuming, several side effects of operation can occur.
A limited number of studies have been performed regarding the value of FNA in the diagnosis of head and neck lymphoma and the results are incompatible [5–9]. Since FNA has been described as safe and cost-effective for the diagnosis of head and neck masses, we aimed to evaluate its value in the diagnosis of head and neck lymphoma [2, 10].
Subjects and Methods
The present cross-sectional study was performed in Imam Hospital and Cancer Institute affiliated to the Tehran University of Medical Sciences. In a 5 years period between January 2006 and June 2010, all patients with cervical mass (es) who had undergone FNA, as the primary diagnostic modality, and then underwent biopsy (excisional or open) or surgery were recruited.
Exclusion criterion was incomplete medical recordings. Among 143 patients with cervical masses, only 58 patients had undergone both FNA and biopsy or surgery. Forty-seven patients were randomly recruited among those 58 patients. (Figs. 1, 2, and 3).
Fig. 1.
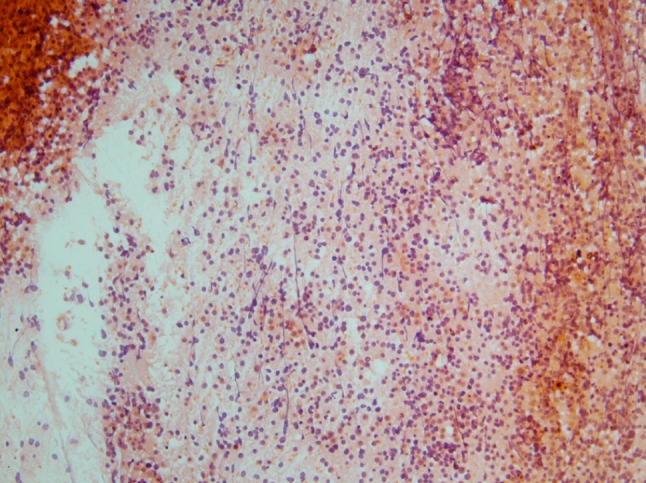
Histopathological examination of lymphoma (PAP stain with power 10 × 10)
Fig. 2.
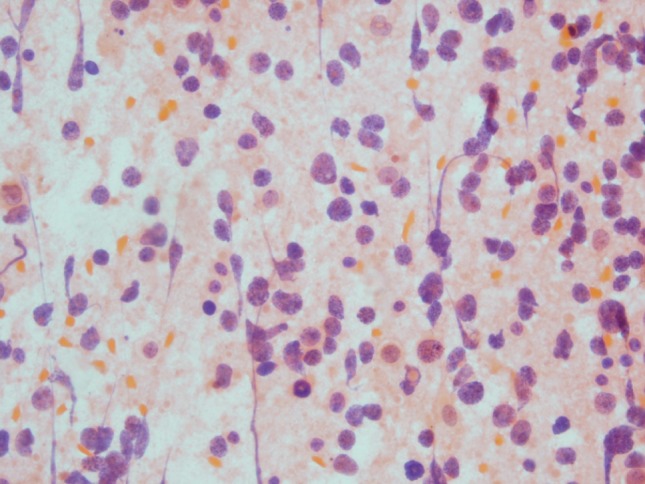
Histopathological examination of lymphoma (papanicolaou stain with power 40 × 10)
Fig. 3.
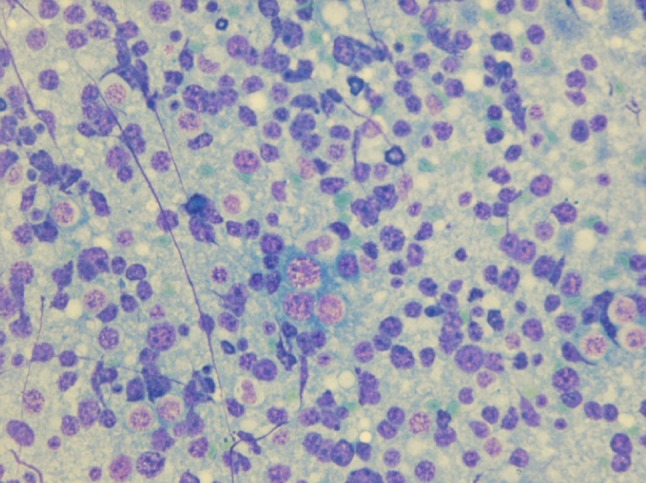
Histopathological examination of lymphoma (diff-quick stain with power 40 × 10)
The present study was reviewed and approved by the Ethics Committee of Tehran University of Medical Sciences to observe the Declaration of Helsinki. All data were evaluated with SPSS. Sensitivity, specificity, positive predictive value, negative predictive value and accuracy were calculated. The t-Student was used for descriptive purposes and Chi-square for determination of significant difference.
Results
The mean age of patients was 37.4 ± 19.2 years and 33 patients (70.2%) were female. Results from biopsies confirmed the diagnosis of lymphoma in 25 patients (53.2%) and non-lymphoma diseases in 22 patients (46.8%) while 26 patients (55.3%) were diagnosed with lymphoma and 21 patients (44.7%) were diagnosed with non-lymphoma diseases according to FNA results. However, 22 patients (46.8%) were diagnosed with lymphoma and 18 patients (38.4%) were diagnosed with non-lymphoma diseases according to results of both biopsy and FNA.
Fine aspiration reported lymphoma in four patients (8.4%) while biopsy reported these cases as non-lymphoma diseases (pseudo positive). Also, three patients (6.4%) were diagnosed with non-lymphoma diseases by FNA, whereas biopsy reported them as lymphoma (pseudo-negative). A statistically significant relationship was found between these two diagnostic methods (P = 0.001).
Fine-needle aspiration had a sensitivity of 88% (CI 95% = 79–97), a specificity of 81.2% (CI 95% = 70–92), a positive predictive value of 84.6% (CI 95% = 75–95), a negative predictive value of 85.7% (CI 95% = 77–95) and an accuracy of 85.1% (CI 95% = 75–95) in the diagnosis of head and neck lymphoma.
Among patients with lymphoma (25 cases), results of biopsy showed nine cases (36%) of Hodgkin’s lymphoma and 16 cases (64%) of non-Hodgkin’s lymphoma. Histopathological subtypes of the patients with Hodgkin’s lymphoma consisted of five cases (55.6%) of nodular sclerosis, three cases (33.3%) of mixed cellularity and one case (11.1%) of lymphocyte predominant. Regarding non-Hodgkin’s lymphoma, there were 14 cases of B cell lymphoma and two cases of peripheral T cell lymphoma. Among 26 cases of lymphoma according to the results of FNA, there were five cases (19.3%) of Hodgkin’s lymphoma and 21 cases (80.7%) of non-Hodgkin’s lymphoma. Table 1 compares the results of FNA and biopsy considering histopathological subtypes.
Table 1.
Frequency of accurate diagnosis of lymphoma subtypes by FNA in compare with biopsy
| Biopsy | FNA | ||
|---|---|---|---|
| Number (%) | True (%) | False (%) | |
| Non-Hodgkin lymphoma | 16 (64) | 4 (25) | 12 (75) |
| CLL | 7 (44) | 2 (29) | 5 (71) |
| Diffuse large B cell lymphoma | 3 (19) | 1 (33) | 2 (67) |
| Follicular lymphoma | 2 (13) | – | 2 (100) |
| Burkitt lymphoma | 1 (5.5) | – | 1 (100) |
| Mantle cell lymphoma | 1 (5.5) | – | 1 (100) |
| Peripheral T cell lymphoma | 2 (13) | 1 (50) | 1 (50) |
| Hodgkin lymphoma | 9 (36) | 4 (45) | 5 (56) |
| Total | 25 | 8 (32) | 5 (68) |
Results of 16 biopsies of non-Hodgkin’s lymphoma showed a high grade in nine cases (56.2%) and a low grade in seven cases (43.8%). Results of FNA in 21 patients with non-Hodgkin’s lymphoma showed a high grade in 16 cases (74.1%) and a low grade in five cases (25.9%). Both FNA and biopsy reported non-Hodgkin’s lymphoma in 15 patients. Table 2 compares the results of FNA and biopsy in these 15 patients.
Table 2.
Results of grading by FNA in non-Hodgkin lymphoma compare with biopsy
| Biopsy, N a (%) | ||||
|---|---|---|---|---|
| High grade | Low grade | Total | ||
| FNA | High grade | 8 (53) | 4 (27) | 12 (80) |
| Low grade | 1 (7) | 2 (14) | 3 (20) | |
| Total | 9 (60) | 6 (40) | 15 (100) | |
aNumber
Discussion
Considering the high prevalence of head and neck masses, utilization of non-invasive diagnostic methods seem necessary. On the other hand, the highly sensitive diagnostic methods are also needed to determine various and important causes of head and neck masses.
Gonzales et al. [11] described a sensitivity and a specificity of 95.08 and 98.11%, respectively, for FNA in diagnosis of head and neck masses. Also they found a PPV of 96.67% and a NPV of 97.20%. Carroll et al. [12] reported an accuracy of 87 and 95% for FNA in diagnosis of malignant and benign head and neck masses, respectively. el Hag et al. [13] reported that head and neck lymphomas could decrease the sensitivity and predictive value of FNA in diagnosis of head and neck masses. They found that if they eliminated head and neck lymphoma cases, the sensitivity (95%) and predictive value (96%) would be both 100%. These facts raise doubt regarding the value of FNA in the diagnosis of head and neck lymphoma.
After a study on 248 patients, Kuvezdic et al. [14] found a good value for FNA in the diagnosis of head and neck nodal lymphoma. A sensitivity of 90%, a specificity of 88%, a PPV of 97%, and a NPV of 61% was reported by Kuvezdic et al. [14]. A similar study reported a sensitivity of 97.7%, a specificity of 85.7%, and an accuracy of 96% [15]. Considering the sensitivity of these two studies and our results, it can be supposed that FNA has a good value. However, a pseudo positive value of 8.4% and a pseudo-negative value of 6.4% in our study further added to the clinical doubt on the value of FNA. This problem was also reported by Russell et al. [16]. They suggested FNA was only valuable in confirmation of suspected recurrence cases.
Histopathological sub-classification is vital for the diagnosis and treatment approach of lymphoma. Because FNA provides a limited amount of cells, histopathological sub-classification based on biopsy specimens is not reliable and helpful. Similarly, Hehn et al. [17] found that FNA could provide true histopathological sub-classification in only 29% of lymphomas. We found 68% compatibility between the results of FNA and histopathology in sub-classification. Thus, FNA cannot be a reliable modality for planning a proper treatment approach.
In contrast, Landgren et al. [18] reported that results of FNA cytology and histopathology-based diagnoses were concordant in 74% of the patients. Despite limitations in diagnosis of some lymphoma entities (Hodgkin’s lymphoma and anaplastic large cell lymphoma), they suggested FNA as an accurate modality in diagnosis of lymphomas. However, Kolonic et al. [19] reported a good clinical value for FNA in differentiation between Hodgkin’s lymphoma and anaplastic large cell lymphoma. Our study showed a limited value for FNA in diagnosis of Hodgkin’s lymphoma. FNA could diagnose only five out of nine lymphoma cases. Since FNA could only diagnose two out of six cases with low grade malignant masses in our study, we concluded that FNA had a limited value in the diagnosis of such masses; this finding was also noted by Cohen et al. [20]. In contrast, considering high grade malignant masses, FNA could diagnose eight out of nine cases. This finding is not in agreement with the results of the study performed by Landgren et al. [18].
Regarding the differentiation of lymphoma from non-lymphoma diseases by FNA, an accuracy of 85% was found. Considering the sensitivity of 88%, utilization of FNA is recommended as a screening method for diagnosing head and neck lymphomas. However, we found a pseudo-negative rate of 6% for FNA but considering the clinical features and through using new methods, such as immunocytochemical analysis [7] and genotype analysis [8, 9, 21], this shortcoming could be somehow defeated. In conclusion, since we found a considerable value for FNA in differentiation of head and neck lymphoma from non-lymphoma etiologies, it is recommended as a screening test for the diagnosis of head and neck lymphoma.
Acknowledgments
Financial Support
This study was founded by a medical research grant received from the research Deputy of Tehran University of Medical Sciences, Tehran, Iran.
Conflict of interest
None declared.
References
- 1.Nicol T. The accuracy of combined cytopathologic and flow cytometric analysis of fine-needle aspirates of lymph nodes. Am J Clin Pathol. 2000;114:18–28. doi: 10.1309/MN6J-4NJY-C5CG-1PLH. [DOI] [PubMed] [Google Scholar]
- 2.Layfield LJ. Fine-needle aspiration of the head and neck. Pathology. 1996;4:409–438. [PubMed] [Google Scholar]
- 3.Naeimi M, Sharifi A, Erfanian Y, Velayati A, Izadian S, Golparvar S. Differential diagnosis of cervical malignant lymphadenopathy among Iranian patients. Saudi Med J. 2009;30:377–381. [PubMed] [Google Scholar]
- 4.Hashemi-Bahremani M, Parwaresch MR, Tabrizchi H, Gupta RK, Raffii MR. Lymphomas in Iran. Arch Iran Med. 2007;10:343–348. [PubMed] [Google Scholar]
- 5.Katz RL. Cytologic diagnosis of leukemia and lymphoma. Values and limitations. Clin Lab Med. 1991;11:469–499. [PubMed] [Google Scholar]
- 6.Katz RL, Caraway NP. FNA lymphoproliferative diseases: myths and legends. Diagn Cytopathol. 1995;12:99–100. doi: 10.1002/dc.2840120202. [DOI] [PubMed] [Google Scholar]
- 7.Sneige N. Diagnosis of lymphoma and reactive lymphoid hyperplasia by immunocytochemical analysis of fine-needle aspiration biopsy. Diagn Cytopathol. 1990;6:39–43. doi: 10.1002/dc.2840060109. [DOI] [PubMed] [Google Scholar]
- 8.Jeffers MD, McCorriston J, Farquharson MA, Stewart CJ, Mutch AF. Analysis of clonality in cytologic material using the polymerase chain reaction (PCR) Cytopathology. 1997;8:114–121. doi: 10.1111/j.1365-2303.1997.tb00593.x. [DOI] [PubMed] [Google Scholar]
- 9.Stewart CJ, Farquharson MA, Kerr T, McCorriston J. Immunoglobulin light chain mRNA detected by in situ hybridization in diagnostic fine-needle aspiration cytology specimens. J Clin Pathol. 1996;49:749–754. doi: 10.1136/jcp.49.9.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tatomirovic Z, Skuletic V, Bokun R, et al. Fine-needle aspiration cytology in the diagnosis of head and neck masses: accuracy and diagnostic problems. J BUON. 2009;14:653–659. [PubMed] [Google Scholar]
- 11.Gonzalez M, Blanc JM, Pardo J, Bosch R, Vinuela JA. Head and neck fine-needle aspiration: cytohistological correlation. Acta Otorrinolaringol Esp. 2008;59:205–211. doi: 10.1016/S0001-6519(08)73296-5. [DOI] [PubMed] [Google Scholar]
- 12.Carroll CM, Nazeer U, Timon CI. The accuracy of fine-needle aspiration biopsy in the diagnosis of head and neck masses. Ir J Med Sci. 1998;167:149–151. doi: 10.1007/BF02937926. [DOI] [PubMed] [Google Scholar]
- 13.el Hag IA, Chiedozi LC, al Reyees FA, Kollur SM. Fine-needle aspiration cytology of head and neck masses. Seven years’ experience in a secondary care hospital. Acta Cytol. 2003;47:387–392. doi: 10.1159/000326538. [DOI] [PubMed] [Google Scholar]
- 14.Kuvezdic KG, Aurer I, Ries S, et al. FNA based diagnosis of head and neck nodal lymphoma. Coll Antropol. 2010;34:7–12. [PubMed] [Google Scholar]
- 15.Senjug P, Ostovic KT, Miletic Z, et al. The accuracy of fine-needle aspiration cytology and flow cytometry in evaluation of nodal and extranodal sites in patients with suspicion of lymphoma. Coll Antropol. 2010;34:131–137. [PubMed] [Google Scholar]
- 16.Russell J, Orell S, Skinner J, Seshadri R. Fine-needle aspiration cytology in the management of lymphoma. Aust N Z J Med. 1983;13:365–368. doi: 10.1111/j.1445-5994.1983.tb04482.x. [DOI] [PubMed] [Google Scholar]
- 17.Hehn ST, Grogan TM, Miller TP. Utility of fine-needle aspiration as a diagnostic technique in lymphoma. J Clin Oncol. 2004;22:3046–3052. doi: 10.1200/JCO.2004.02.104. [DOI] [PubMed] [Google Scholar]
- 18.Landgren O, MacDonald AP, Tani E, et al. A prospective comparison of fine-needle aspiration cytology and histopathology in the diagnosis and classification of lymphomas. Hematol J. 2004;5:69–76. doi: 10.1038/sj.thj.6200316. [DOI] [PubMed] [Google Scholar]
- 19.Kolonic SO, Prasek-Kudrna K, Roso V, et al. Value of fine-needle aspiration cytology in diagnosis of Hodgkin’s lymphoma and anaplastic large cell lymphoma: one center experience. Coll Antropol. 2010;34:75–79. [PubMed] [Google Scholar]
- 20.Cohen EG, Patel SG, Lin O, et al. Fine-needle aspiration biopsy of salivary gland lesions in a selected patient population. Arch Otolaryngol Head Neck Surg. 2004;130:773–778. doi: 10.1001/archotol.130.6.773. [DOI] [PubMed] [Google Scholar]
- 21.Wan JH, Sykes PJ, Orell SR, Morley AA. Rapid method for detecting monoclonality in B cell lymphoma in lymph node aspirates using the polymerase chain reaction. J Clin Pathol. 1992;45:420–423. doi: 10.1136/jcp.45.5.420. [DOI] [PMC free article] [PubMed] [Google Scholar]


