Abstract
Tinnitus is a perception of sound in proximity to the head with the absence of an external source. It is estimated to occur in 15–20% of the world’s population, with 1–3% of cases severely affecting quality of life. Severe tinnitus is frequently associated with depression, anxiety and insomnia. Tinnitus has been associated with a variety of risk factors, including prolonged noise exposure, head and neck injury and infection. The most recent pathophysiologic theory of tinnitus suggests that the central nervous system is the source or “generator” of this condition. However, treatment modalities are still aimed at lessening the awareness of tinnitus and its impact on quality of life rather than attaining a definitive cure. Currently, no drug is available that has demonstrated replicable, long-term reduction of tinnitus impact in excess of placebo effects. However, the market value of such an agent is estimated to be $1.1 billion, with a potential for increase with an aging and longer-living population. This review assesses the current developments in the pathophysiology and treatment for tinnitus, which remains a chronic and debilitating condition.
Keywords: Tinnitus, Pathophysiology, Treatment
Introduction
Tinnitus, originating from the Latin word ‘tinnire’ (‘to ring’), is a perception of sound in proximity to the head with the absence of an external source [1]. It may be described as buzzing, ringing, roaring, whistling or hissing and can be variable and complex. Tinnitus may be intermittent, continuous or pulsatile, with the latter being at best annoying and often quite distressing. It is estimated that approximately 15–20% of the world population suffer from tinnitus [2, 3]. For about 25% of those affected, the condition interferes with daily activity, with 1–3% of cases severely affecting quality of life [3]. Severe tinnitus is frequently associated with depression, anxiety and insomnia [4, 5].
During the second half of the 20th century, several theories for the aetiology of tinnitus were proposed and treatment modalities in the form of medications and surgery were developed with varying degrees of success [6]. Even with these advances, tinnitus continues to be a debilitating condition with no definitive cure, sometimes driving the patient to suicide [7].
Classification
Tinnitus can be classified in two categories. Objective tinnitus is associated with generation of noise near the ear that, in some cases, can be heard by the examiner using a stethoscope [8]. Subjective tinnitus is the perception of sound in the absence of an acoustic stimulus and is heard only by the patient [8].
Objective tinnitus is an uncommon occurrence involving an audible, pulsatile hum and can be caused by turbulent flow through the carotid artery or jugular vein [9]. Highly vascular middle ear tumours (e.g. glomus jugulare tumours) and dural arteriovenous malformations may also cause objective tinnitus [10].
Subjective tinnitus is much more common and may occur with almost any ear disorder [9]. Common causes include sensorineural hearing loss (e.g. acoustic trauma), obstruction of the ear canal by cerumen, infections (e.g. otitis media), Eustachian tube obstruction and drugs such as salicylates [11]. The majority of patients have “sensorineural” tinnitus, which is associated with hearing loss at the cochlea or cochlear nerve level [12].
Pathophysiology
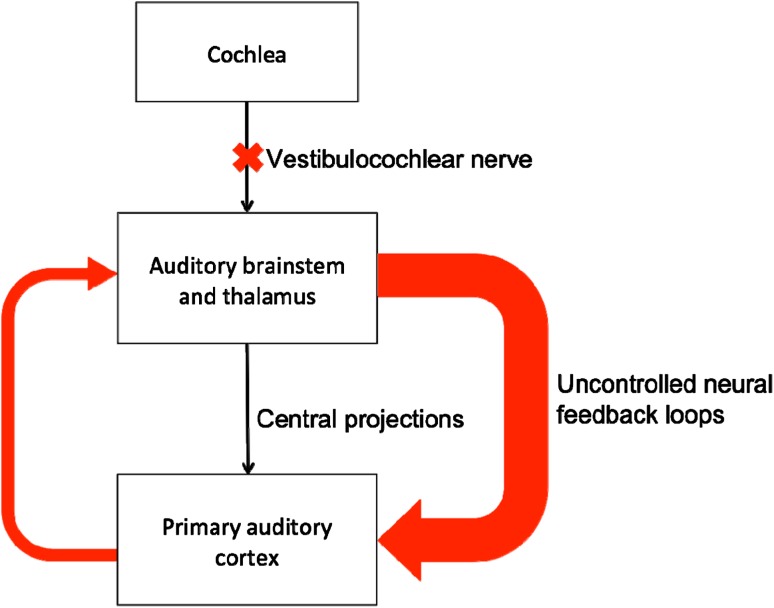
Tinnitus has been associated with a variety of risk factors, including prolonged noise exposure (22% of cases), head/neck injury (17% of cases) and infections (10% of cases) [13]. The most recent pathophysiologic theory suggests that the central nervous system is the source or “generator” of tinnitus [14]. Positron emission tomography (PET) scanning and functional magnetic resonance imaging (fMRI) studies indicate that a loss of cochlear input to neurons in the central auditory system (such as occurs in cochlear hair cell damage or a lesion of the vestibulocochlear nerve) can result in abnormal neural activity in the auditory cortex [15]. This activity is linked to the perception of tinnitus. In addition, there is also a loss of suppression of the neural feedback loops which help tune and reinforce auditory memory in the central auditory cortex [10]. Disruption of this feedback loop leads to the disinhibition of normal synapses and the creation of uncontrolled alternative neural synapses which lead to the abnormal auditory perception of tinnitus (Fig. 1) [16].
Fig. 1.
Pathophysiology of tinnitus
Recent improvements in neuro-otometry have confirmed the complex pathophysiologic mechanisms involved in tinnitus, elucidating sites in which these processes take place [17–19]. It is now known that approximately 24% of cases occur as a result of abnormalities within the otoacoustic periphery (i.e. inner ear and the vestibulocochlear nerve), 35% originate from the acoustic pathways and 41% have their cause within supratentorial structures [6]. A decrease in inhibition and/or increase in excitation may lead to an excitatory-inhibitory imbalance causing neuronal hyperexcitability in these regions and lead to the perception of tinnitus [20]. However, neuronal excitability can be modulated by different neurotransmitters and neuromodulators that act on voltage- or ligand-gated channels, thus providing potential pharmacologic targets [20].
Treatment
Since tinnitus is associated with marked irritability, agitation, stress, depression, insomnia and interference with daily life, even a drug that produces a small but significant effect would have a significant therapeutic impact. However, due to the myriad of aetiologies and complex pathogenic mechanisms proposed, definitive treatment for tinnitus is yet to be developed. There is currently no single Food and Drug Administration (FDA) or European Medicines Agency (EMEA) approved drug in the market. No studied drug in the literature provides replicable, long-term reduction of tinnitus impact in excess of placebo effects [21, 22]. Current treatment strategy is aimed at controlling underlying disorders and symptomatically suppressing the perception of tinnitus. The primary goal has thus been improvement in quality of life rather than absolute cure. This may be achieved through a variety of regimens, though none show complete efficacy.
Comprehensive management of tinnitus includes assessment of hypertension, blood lipids, thyroid function, allergies and informing patients of factors that aggravate tinnitus, such as stress, caffeine, nicotine, and aspirin [21]. Treatment of comorbidities may involve procedures such as embolization or ligation for vascular abnormalities such as arteriovenous malformations. Hearing aids for presbycusis, cochlear implants for sensorineural hearing loss and cessation of any offending medications are also important components of management [23].
Many patients with tinnitus exhibit signs of anxiety or depression, associated with elevated serum serotonin levels [24]. Serotonin and GABA receptors are found throughout the auditory system, and neurotransmitter abnormalities have been purported to play a role in some patients [25, 26]. Attempts at symptomatic relief have included antidepressants (e.g. amitriptyline) [27], anxiolytics (e.g. diazepam), anticonvulsants (e.g. clonazepam), diuretics, and antihistamines (e.g. dexchlorpheniramine maleate), all of which have yielded inconsistent and inconclusive results [28].
Tinnitus-specific medications have also proven ineffective. Trials of the prostaglandin E1 analogue misoprostol [29], gabapentin [30], lidocaine [31] and dexamethasone [32] have only shown limited benefit. Complementary and alternative medicine (CAM) therapies are equally disappointing. Large trials of Ginkgo biloba, the most popular form of CAM therapy, have failed to yield definitive results [33].
In contrast, a number of non-medical treatments have been studied with some success. These include tinnitus retraining therapy (TRT), masking, biofeedback and cognitive behavioral therapy.
TRT is based on bypassing or overriding abnormal auditory cortex neural connections—the pathogenic mechanism postulated to drive tinnitus. It is based on the principle that all levels of the auditory pathways play essential roles in tinnitus, and induces habituation to the tinnitus signal [34]. The goal is to reach a stage in which patients are unaware of their condition unless they consciously focus on it. This habituation is achieved by directive counseling, combined with low-level noise generated by wearable generators and environmental sounds. Significant improvement has been reported in up to 80% of patients but well-controlled studies are not reported, the long-term impact is not known, and the therapy takes at least one to 2 years before effects are seen [35].
Masking devices are designed to produce low-level sounds that reduce the perception of tinnitus. It is not successful in all patients and some patients have even reported a worsening of their tinnitus [35].
Biofeedback is a relaxation technique teaching people to control certain autonomic body functions. The goal is to help people manage tinnitus-related distress by changing the patient’s reaction to it. Many people have noticed a reduction in tinnitus when they are able to modify their reaction to it [36], though well-controlled trials have not yet been completed.
Cognitive behavioral therapy aims to motivate patients to learn to alter their psychological response to tinnitus by identifying and reinforcing coping strategies, distraction skills and relaxation techniques. Several studies have shown benefit compared to control patients in reducing tinnitus-related distress, but no benefit on the loudness of the tinnitus [36].
It is now recognized that every patient with tinnitus has a unique medical, psychological and social experience. A number of recent studies recommend individualized management programs utilizing multimodal strategies designed to address the specific needs of each patient [11, 27, 35, 36]. These studies have suggested that a tinnitus management team, comprising of an otolaryngologist, audiologist, neurologist, psychologist and sleep or pain specialists, is essential for the successful treatment of tinnitus.
Future Therapy
Although there are no current FDA or EMEA approved drugs to treat tinnitus, a potential market appears to be emerging. The Royal National Institute of Deafness in the United Kingdom estimated the patient opportunity for a tinnitus drug would be 15 million by 2012. The market value of tinnitus retraining therapy and off-label pharmaceuticals was estimated in 2003 to be $127 million. The market value of the whole segment ‘symptomatic relief from tinnitus’ was estimated to be $1.1 billion, with a potential for increase if an effective drug is to become available. This is because there is a significant number of people with tinnitus who have stopped seeking medical treatment due to lack of efficacy, but who would probably be interested in treatment as soon as an effective compound is made available [37].
Currently, there are only a small number of drugs in development for the treatment of tinnitus. One of these is neramexane, a non-competitive, voltage-dependent NMDA antagonist which also blocks nicotinic cholinergic receptors expressed on hair cells in the inner ear [38–40]. After promising Phase 2 trial results, the drug is currently in Phase III multi-centre clinical trials to determine its efficacy, safety and tolerability.
LidoPAIN TV is a non-sterile patch delivering lidocaine, which is applied to the periauricular skin region. According to the company, it has demonstrated efficacy in a clinical proof-of-concept study and has been in Phase II trials for tinnitus.
Vesitipitant is a novel antagonist of the neurkinin-1 receptor which binds substance P. Neurokinin receptors are present in the inner ear, representing a potential therapeutic target for tinnitus [41]. Vestipitant and the combination of vestipitant and paroxetine are currently undergoing Phase 2 clinical trials for the treatment of tinnitus.
Conclusion
Tinnitus may originate in any location along the auditory pathway from the cochlear nucleus to the auditory cortex. Some leading theories include injured cochlear hair cells which repetitively stimulate auditory nerve fibers, spontaneous activity in individual auditory nerve fibers, hyperactivity of auditory nuclei in the brain stem or a reduction in the usually suppressive activity of the central auditory cortex on peripheral auditory nerve activity.
Though there have been advances in the understanding of the pathophysiology of this condition, the treatment modalities are still aimed at lessening the awareness of tinnitus and its impact on quality of life rather than attaining a definitive cure. Currently, no drug is available that has demonstrated replicable, long-term reduction of tinnitus impact in excess of placebo effects. Medical therapy has been limited in efficacy and consistency and more research needs to be conducted into non-medical treatment modalities such as TRT, cognitive behavioral therapy and masking. As a result, tinnitus remains a chronic, often debilitating condition for a significant number of patients. However, the development of molecular, biochemical and imaging techniques are offering increasing insights into the underlying causes of tinnitus and for the development of new potential targets for treatment.
Acknowledgments
I accept to undertake all the responsibility for authorship during the submission and review stages of the manuscript. No financial support was received in the preparation of this article.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Crummer RW, Hassan GA. Diagnostic approach to tinnitus. Am Fam Physician. 2004;69(1):120–126. [PubMed] [Google Scholar]
- 2.Coles RR. Epidemiology of tinnitus: (1) prevalence. J Laryngol Otol Suppl. 1984;9:7–15. doi: 10.1017/S1755146300090041. [DOI] [PubMed] [Google Scholar]
- 3.Axelsson A, Ringdahl A. Tinnitus–a study of its prevalence and characteristics. Br J Audiol. 1989;23(1):53–62. doi: 10.3109/03005368909077819. [DOI] [PubMed] [Google Scholar]
- 4.Cronlein T, Langguth B, Geisler P, Hajak G. Tinnitus and insomnia. Prog Brain Res. 2007;166:227–233. doi: 10.1016/S0079-6123(07)66021-X. [DOI] [PubMed] [Google Scholar]
- 5.Langguth B, Kleinjung T, Fischer B, Hajak G, Eichhammer P, Sand PG. Tinnitus severity, depression, and the big five personality traits. Prog Brain Res. 2007;166:221–225. doi: 10.1016/S0079-6123(07)66020-8. [DOI] [PubMed] [Google Scholar]
- 6.Claussen CF. Rakel & Bope: Conn’s Current Therapy. 60. Philadelphia: Elsevier Inc.; 2008. [Google Scholar]
- 7.Jacobson GP, McCaslin DL. A search for evidence of a direct relationship between tinnitus and suicide. J Am Acad Audiol. 2001;12(10):493–496. [PubMed] [Google Scholar]
- 8.Lockwood AH. Tinnitus. Neurol Clin. 2005;23(3):893–900. doi: 10.1016/j.ncl.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad N, Seidman M. Tinnitus in the older adult: epidemiology, pathophysiology and treatment options. Drugs Aging. 2004;21(5):297–305. doi: 10.2165/00002512-200421050-00002. [DOI] [PubMed] [Google Scholar]
- 10.Lockwood AH, Salvi RJ, Burkard RF, Galantowicz PJ, Coad ML, Wack DS. Neuroanatomy of tinnitus. Scand Audiol Suppl. 1999;51:47–52. [PubMed] [Google Scholar]
- 11.Shulman A, Goldstein B. Medical Significance of Tinnitus. Int Tinnitus J. 1997;3(1):45–50. [PubMed] [Google Scholar]
- 12.Schleuning AJ., 2nd Management of the patient with tinnitus. Med Clin North Am. 1991;75(6):1225–1237. doi: 10.1016/s0025-7125(16)30383-2. [DOI] [PubMed] [Google Scholar]
- 13.Henry JA, Dennis KC, Schechter MA. General review of tinnitus: prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. 2005;48(5):1204–1235. doi: 10.1044/1092-4388(2005/084). [DOI] [PubMed] [Google Scholar]
- 14.Qiu C, Salvi R, Ding D, Burkard R. Inner hair cell loss leads to enhanced response amplitudes in auditory cortex of unanesthetized chinchillas: evidence for increased system gain. Hear Res. 2000;139(1–2):153–171. doi: 10.1016/S0378-5955(99)00171-9. [DOI] [PubMed] [Google Scholar]
- 15.Fortune DS, Haynes DS, Hall JW, 3rd, Tinnitus Current evaluation and management. Med Clin North Am. 1999;83(1):153–162. doi: 10.1016/S0025-7125(05)70094-8. [DOI] [PubMed] [Google Scholar]
- 16.Moller AR. Similarities between chronic pain and tinnitus. Am J Otol. 1997;18(5):577–585. [PubMed] [Google Scholar]
- 17.Konig O, Schaette R, Kempter R, Gross M. Course of hearing loss and occurrence of tinnitus. Hear Res. 2006;221(1–2):59–64. doi: 10.1016/j.heares.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Norena A, Micheyl C, Chery-Croze S, Collet L. Psychoacoustic characterization of the tinnitus spectrum: implications for the underlying mechanisms of tinnitus. Audiol Neurootol. 2002;7(6):358–369. doi: 10.1159/000066156. [DOI] [PubMed] [Google Scholar]
- 19.Roberts LE, Moffat G, Bosnyak DJ (2006) Residual inhibition functions in relation to tinnitus spectra and auditory threshold shift. Acta Otolaryngol Suppl 556:27–33 [DOI] [PubMed]
- 20.Langguth B, Salvi R, Elgoyhen AB. Emerging pharmacotherapy of tinnitus. Expert Opin Emerg Drugs. 2009;14(4):687–702. doi: 10.1517/14728210903206975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dobie RA. A review of randomized clinical trials in tinnitus. Laryngoscope. 1999;109(8):1202–1211. doi: 10.1097/00005537-199908000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Dobie R (2004) In: Snow J (ed) Tinnitus: theory and management. Decker, Hamilton
- 23.Jastreboff PJ, Gray WC, Gold SL. Neurophysiological approach to tinnitus patients. Am J Otol. 1996;17(2):236–240. [PubMed] [Google Scholar]
- 24.Simpson JJ, Davies WE. A review of evidence in support of a role for 5-HT in the perception of tinnitus. Hear Res. 2000;145(1–2):1–7. doi: 10.1016/S0378-5955(00)00093-9. [DOI] [PubMed] [Google Scholar]
- 25.Thompson GC, Thompson AM, Garrett KM, Britton BH. Serotonin and serotonin receptors in the central auditory system. Otolaryngol Head Neck Surg. 1994;110(1):93–102. doi: 10.1016/S0194-5998(94)70797-9. [DOI] [PubMed] [Google Scholar]
- 26.Woods CI, Azeredo WJ. Noradrenergic and serotonergic projections to the superior olive: potential for modulation of olivocochlear neurons. Brain Res. 1999;836(1–2):9–18. doi: 10.1016/S0006-8993(99)01541-3. [DOI] [PubMed] [Google Scholar]
- 27.Baldo P, Doree C, Lazzarini R, Molin P, McFerran DJ (2006) Antidepressants for patients with tinnitus. Cochrane Database Syst Rev (4):CD003853 [DOI] [PubMed]
- 28.Murai K, Tyler RS, Harker LA, Stouffer JL. Review of pharmacologic treatment of tinnitus. Am J Otol. 1992;13(5):454–464. [PubMed] [Google Scholar]
- 29.Yilmaz I, Akkuzu B, Cakmak O, Ozluoglu LN. Misoprostol in the treatment of tinnitus: a double-blind study. Otolaryngol Head Neck Surg. 2004;130(5):604–610. doi: 10.1016/j.otohns.2003.08.027. [DOI] [PubMed] [Google Scholar]
- 30.Bauer CA, Brozoski TJ. Effect of gabapentin on the sensation and impact of tinnitus. Laryngoscope. 2006;116(5):675–681. doi: 10.1097/01.MLG.0000216812.65206.CD. [DOI] [PubMed] [Google Scholar]
- 31.Sanchez TG, Balbani AP, Bittar RS, Bento RF, Camara J. Lidocaine test in patients with tinnitus: rationale of accomplishment and relation to the treatment with carbamazepine. Auris Nasus Larynx. 1999;26(4):411–417. doi: 10.1016/S0385-8146(99)00020-6. [DOI] [PubMed] [Google Scholar]
- 32.Garduno-Anaya MA, Couthino De Toledo H, Hinojosa-Gonzalez R, Pane-Pianese C, Rios-Castaneda LC. Dexamethasone inner ear perfusion by intratympanic injection in unilateral Meniere’s disease: a two-year prospective, placebo-controlled, double-blind, randomized trial. Otolaryngol Head Neck Surg. 2005;133(2):285–294. doi: 10.1016/j.otohns.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 33.Rejali D, Sivakumar A, Balaji N. Ginkgo biloba does not benefit patients with tinnitus: a randomized placebo-controlled double-blind trial and meta-analysis of randomized trials. Clin Otolaryngol Allied Sci. 2004;29(3):226–231. doi: 10.1111/j.1365-2273.2004.00814.x. [DOI] [PubMed] [Google Scholar]
- 34.Berry JA, Gold SL, Frederick EA, Gray WC, Staecker H. Patient-based outcomes in patients with primary tinnitus undergoing tinnitus retraining therapy. Arch Otolaryngol Head Neck Surg. 2002;128(10):1153–1157. doi: 10.1001/archotol.128.10.1153. [DOI] [PubMed] [Google Scholar]
- 35.Andersson G, Lyttkens L. A meta-analytic review of psychological treatments for tinnitus. Br J Audiol. 1999;33(4):201–210. doi: 10.3109/03005369909090101. [DOI] [PubMed] [Google Scholar]
- 36.Zachriat C, Kroner-Herwig B. Treating chronic tinnitus: comparison of cognitive-behavioural and habituation-based treatments. Cogn Behav Ther. 2004;33(4):187–198. doi: 10.1080/16506070410029568. [DOI] [PubMed] [Google Scholar]
- 37.Vio M (2003) Tinnitus market situation analysis. Royal National Institute of Deafness, London
- 38.Elgoyhen AB, Vetter DE, Katz E, Rothlin CV, Heinemann SF, Boulter J. alpha10: a determinant of nicotinic cholinergic receptor function in mammalian vestibular and cochlear mechanosensory hair cells. Proc Natl Acad Sci USA. 2001;98(6):3501–3506. doi: 10.1073/pnas.051622798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elgoyhen AB, Johnson DS, Boulter J, Vetter DE, Heinemann S. Alpha 9: an acetylcholine receptor with novel pharmacological properties expressed in rat cochlear hair cells. Cell. 1994;79(4):705–715. doi: 10.1016/0092-8674(94)90555-X. [DOI] [PubMed] [Google Scholar]
- 40.Plazas PV, Savino J, Kracun S, Gomez-Casati ME, Katz E, Parsons CG, et al. Inhibition of the alpha9alpha10 nicotinic cholinergic receptor by neramexane, an open channel blocker of N-methyl-D-aspartate receptors. Eur J Pharmacol. 2007;566(1–3):11–19. doi: 10.1016/j.ejphar.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 41.Sun W, Ding DL, Wang P, Sun J, Jin X, Salvi RJ. Substance P inhibits potassium and calcium currents in inner ear spiral ganglion neurons. Brain Res. 2004;1012(1–2):82–92. doi: 10.1016/j.brainres.2004.03.051. [DOI] [PubMed] [Google Scholar]