Abstract
To evaluate the treatment of hypertrophy of inferior turbinates in patients diagnosed with allergic/non allergic rhinitis with the use of radiofrequency ablation technique. Ablation with radiofrequency was used in this study on the inferior turbinates of 200 patients diagnosed as allergic/non allergic rhinitis at our institution between January 2006 and December 2009. The results were evaluated subjectively by changes in pre and post operative symptoms, size of inferior turbinate, postoperative pain and assessment of ciliary function. Four patients (2%) at the end of 6 months and 4 patients (2%) at the end of 12 months reported persistent symptom of nasal obstruction. No patient reported nasal discharge, 28 patients (14%) at 6 months, 20 patients (10%) at 24 months reported persistence of sneezing. 8 patients (4%) at 6 months, 4 patients (2%) at 24 months reported persistence of snoring, no patient complained of persistence of hyposmia. 4 patients (2%) at 6 months, no patient at 24 months complained of crusting, no patient complained of bleeding at 6, 24 months. No alteration of ciliary function and anatomy of the inferior turbinate mucosa was noticed. These results suggests that ablation with radiofrequency is an easily applied, efficient and reliable technique in the treatment of hypertrophied inferior turbinate in allergic/non allergic rhinitis patients with no changes in the ciliary function and necrosis/atrophy of inferior turbinate.
Keywords: Radiofrequency, Radiofrequency ablation, Inferior turbinate
Introduction
Chronic nasal obstruction is one of the most common human problems and a very frequent symptom in the ear, nose, and throat field. Hypertrophy of the inferior turbinates is the most frequent cause and may be related to allergy, pseudoallergy, nonallergic rhinitis with eosinophilia syndrome, and iatrogenic rhinopathy [1, 2]. Even though medical treatments are frequently effective to restore comfortable nasal breathing, nasal obstruction is sometimes slightly improved, leading some patients to increase their consumption of local decongestants with a high risk of iatrogenic effects. In these cases, surgical reduction of inferior turbinates can be proposed. Various techniques are currently performed to reduce the volume of the mucosal (and sometimes bony) tissues of the inferior turbinates [3]. Although most of these techniques provide satisfactory results for a more or less long period, adverse events are frequently observed after such treatments: postoperative bleeding, crusting, foul odour, pain, hyposmia and synechiae [3, 4]. No technique is perfect, and each is associated with known short and long term complications. The variety of surgical techniques available indicates the lack of consensus on the optimal technique [5]. Recently, temperature-controlled radiofrequency tissue volume reduction (TCRFTVR) has been used for the treatment of the hypertrophied inferior turbinates. The use of radiofrequency energy for volumetric soft tissue reduction was first described by Powell et al. [10]. Therefore, radiofrequency could be useful for turbinate volume reduction because, theoretically, it should help to treat nasal obstruction without the disadvantages of the other techniques [11]. Recently, radiofrequency energy has been used for the treatment of the hypertrophied turbinate [12–14]. In studies on radiofrequency ablation of the turbinate, improvement of severity and frequency of nasal obstruction were reported in 81–100% of cases [9, 13]. The literature points to techniques such as visual along scale, rhinomanometry, and acoustic rhinometry, whereas no radiologic techniques are used [12, 15, 16]. It uses radiofrequency energy to create ionic agitation in the surrounding tissue, which induces submucosal necrosis. The circumscribed area of submucosal necrosis is replaced overtime by fibroblasts. Wound contraction by fibrosis results in submucosal tissue volume reduction and relief of nasal obstruction without causing damage to the overlying mucosa. Previous reports reflected that there is a recovery in patient-reported symptoms of obstruction with more than 90% improvement being achieved 8 weeks after treatment [6–8]. Mucociliary function is an important defense mechanism that protects the respiratory system against bacteria and other foreign particles. Nasal mucociliary function is impaired in the majority of surgical reductions of the inferior turbinate [5, 9].
Study Design
This is a prospective study on 200 patients diagnosed with allergic/non allergic rhinitis who underwent radiofrequency reduction of inferior turbinates between January 2006 and December 2009 at our hospital. The study was aimed at recording the effects of radiofrequency reduction of the inferior turbinate on the nasal symptomatology and physiological function of the nose. All patients provided written informed consent before being included in the study, which was approved by the ethics committee.
Inclusion Criteria
Patients aged between 10 and 60 years,
Patients with symptoms duration more than 6 months,
Patients with symptoms of rhinitis with h/o incomplete/failed treatment by medical methods (topical nasal steroids sprays, oral antihistamines) for 8 weeks.
Exclusion Criteria
Previous nasal surgery,
Recurrent epistaxis,
Olfactory abnormalities,
Anatomic abnormalities,
Nasal polyps,
Septal/bony deformity affecting nasal airway,
Active respiratory tract infection,
Patients with systemic diseases affecting nasal passage.
Genetic disorders accompanied by ciliary dysfunction, usage of topical or systemic medication with adverse effects on mucociliary functions, smoking, diabetes mellitus, oral steroid use, coagulation disorders, cardiac pacemaker, and uncontrolled hypertension were additional exclusion criteria Preoperative symptoms included nasal obstruction, nasal discharge, sneezing, snoring, hyposmia.
All subjects were subjected to Detailed history taking, General examination, Systemic examination, ENT examination, Diagnostic nasal endoscopic examination, Radiological investigations: CT Scan paranasal sinus—coronal/saggital section.
Inferior turbinate was graded into 1, 2, 3 on the basis of size of the inferior turbinates.
No odema: normal inferior turbinate.
Grade 1: Inferior turbinate is 25% of nasal cavity.
Grade 2: Inferior turbinate is 50% of nasal cavity
Grade 3: Inferior turbinate is 75% or more of nasal cavity.
Radiofrequency Equipment: Ellman Surgitron 4.0 DUAL RF/120 IEC-High Frequency/Low Temperature
The patented Ellman Surgitron dual frequency unit represents advanced radiowave technology that provides unparalleled surgical control, precision, versatility and safety. The high frequency of 4.0 MHz minimises heat dissipation and cellular alteration. Clinical benefits include minimal post operative discomfort, scar tissue formation, maximum readability of histological specimen, enhanced healing and excellent cosmetic results.
Cell Specific Radiowave Adsorption
High frequency radiowave energy has a strong affinity for water. Targeted tissue/cells readily adsorb energy due to high water content. Intracellular pressure increases as water molecule expands. Volatilization results in cell conversion to vapour. The process emits low temperature steam which results in coagulation. High frequency radiowaves are absorbed in cellular water resulting in shallow adsorption, reducing the risk of injury to surrounding structures and tissue.
Radiosurgery is an atraumatic method of cutting and coagulation of soft tissues without the post operative pain and tissue destruction of electrocautery. The cutting effect known as electrosection is performed without manual pressure or crushing tissue cells. It results from heat generated by the radiofrequency wave, which is applied by a fine wire called surgical electrode. The heat disintegrates and volatises the cells in the pathway of the waves. This causes the tissue to split apart as though it has been cut by a razor sharp knife. Electro coagulation is a non volatizing destruction of tissue cells by a radiofrequency wave.
Radiosurgery as a result accelerates, improves surgical procedures tremendously. It also helps to improve surgical procedures tremendously with minimal intra operative bleeding. It also helps to eliminate the unfavourable postoperative sequel such as swelling, infection, bleeding that is often experienced with traditional instrumentation.
Procedure
Radiofrequency reduction of the inferior turbinate was done under local anaesthesia/general anaesthesia. Patient was placed in supine position with 15 degree head elevation. Patient nose was packed with 4% xylocaine and 1 in 1000 adrenaline 15 min before shifting into the theatre. Both the inferior turbinates were infiltrated with 2% xylocaine with 1 in 100000 adrenaline. In children and uncooperative patients we did the procedure under general anaesthesia. The radiofrequency bipolar probe is applied to the inferior turbinate by keeping in coagulation mode and setting the intensity at 5. Radiofrequency energy is applied submucosally along the length of the inferior turbinate for 3–4 s and the application is repeated. Heat is generated by the resistance of the tissues offered to the passage of the radiofrequency waves. Same procedure was repeated on the other side with the radiofrequency bipolar probe. The advantage of this method was that nasal packing was not required in any of the cases. All the cases were discharged on the same day of surgery. Post operatively patients were advised antibiotics, antihistamines, and liquid paraffin drops to softens the crusts over the inferior turbinate. Patients were asked to come for post operative follow up after 1 week, 2 weeks, and 1 month for the removal of crusts and nasal cleaning. Post operatively patient’s symptomatology (nasal obstruction, nasal discharge, headache, sneezing, hyposmia) were recorded and compared with preoperative symptoms. Post operatively patients complained of nasal block and discharge for 10 days due to radiofrequency application over the inferior turbinates. Post operatively size of the inferior turbinate was compared with the preoperative size of the inferior turbinate. All the symptoms and signs were recorded postoperatively at 1, 6 months, 1 and 2 years. Size of the inferior turbinate was graded into 1, 2, 3 postoperatively and the ciliary function was assessed by saccharin test and histopathological examination of the mucosa of the inferior turbinate.
Post Operative Asessment
State of nasal obstruction, nasal discharge, sneezing, snoring, hyposmia, crusting bleeding, turbinate necrosis/atrophy, size of the inferior turbinate, preservation of cilliary function—histopathological examination and saccharin test.
Results
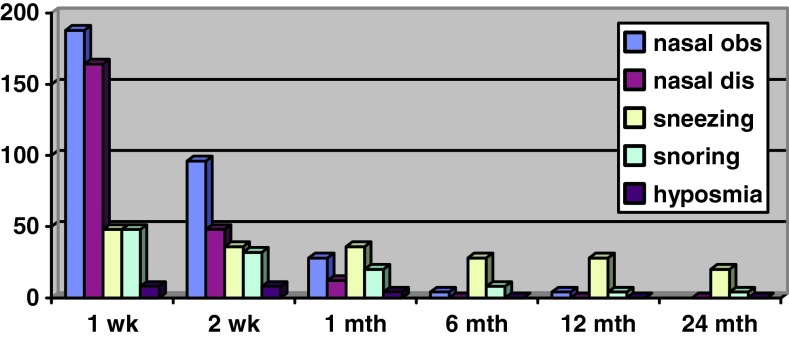
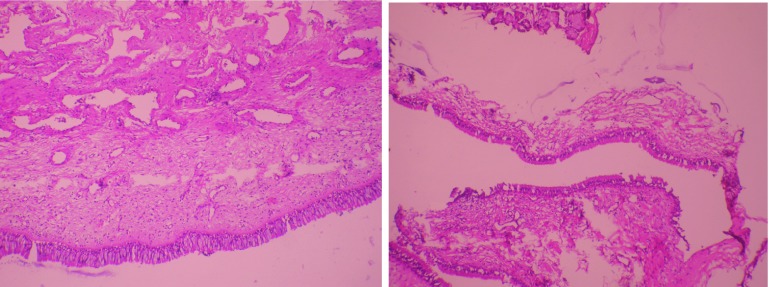
Of the 200 patients 112 were male and 88 were female and their ages ranged from 11 to 59 years. Pre operatively all 200 patients presented with nasal obstruction, associated symptoms of nasal discharge in 124 out of 200 patients (62%), sneezing in 92 patients (46%), snoring in 48 patients (24%) and hyposmia in 8 patients (4%) (Fig. 1).
Fig. 1.
Preoperative symptoms
Pre Operative Symptoms
See Fig. 1.
Post Operative Symptoms
See Table 1.
Table 1.
Post operative symptoms
| Post operative symptoms | 1 week | 2 week | 1 month | 6 month | 12 month | 24 month |
|---|---|---|---|---|---|---|
| Nasal obstruction | 188 | 96 | 28 | 4 | 4 | 4 |
| Nasal discharge | 164 | 48 | 12 | 0 | 0 | 0 |
| Sneezing | 48 | 36 | 36 | 28 | 28 | 20 |
| Snoring | 48 | 32 | 20 | 8 | 4 | 4 |
| Hyposmia | 8 | 8 | 4 | 0 | 0 | 0 |
Radiosurgery of the turbinates has shown to be well tolerated by patients. The postoperative course was satisfactory and comfortable in all the cases without complications. After an initial temporary improvement in the nasal obstruction, some patients reported worsening of the nasal patency for a few days because of crusting. Smith et al. [12], in their study in which they performed applications at only one point in the anterior regions of the turbinates, showed that even small scale changes in the turbinates provided improvement in the symptoms through increasing of airflow in the nasal valve.
Post Operative Symptoms
Fig. 2.
Postoperative symptoms
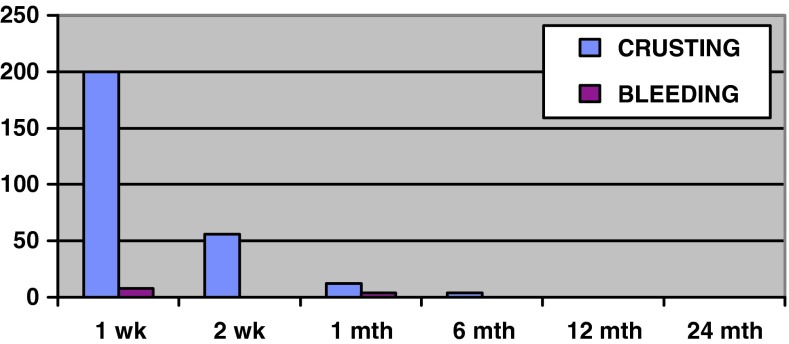
Fig. 3.
Postoperative complications
From the endoscopy performed in the days following the operation, we observed limited crusting on the surface of the turbinates where the needles were inserted and an edema with a more or less congested turbinate. All the patients complained of crusting in the first week post operative period which gradually reduced to 56 patients at 2 weeks, 12 patients at 1 month, 4 patients at 6 months and no patients at 1 and 2 years [Fig. 3]. The patient’s follow up enabled us to see that the mucosal surface normalized within 3–4 weeks. All the patients reported an improvement in their nasal obstruction in the checkups carried out after 2 weeks. 8 patients complained of bleeding in the first post operative period. No patient complained of bleeding at 6 months, 12 months, 24 months post op [Fig. 3]. There was no case of extended necrosis/atrophy of the inferior turbinate with the formation of persistent crusts and no sensation of nasal dryness and no post operative synechiae. Smith et al. [12]. showed that 90% of the reduction in the turbinate occurred in the first 21 days, that 100% of the reduction took place at the end of week 8, and that there was no statistically significant difference between the evaluation at the end of week 8 and at the end of 1 year. It is stated in the literature that reduction starts at postoperation week 3, that the change reaches maximum at the end of week 8, and that this rate is the same as the change at the end of 1 year [12, 13]. See Fig. 4.
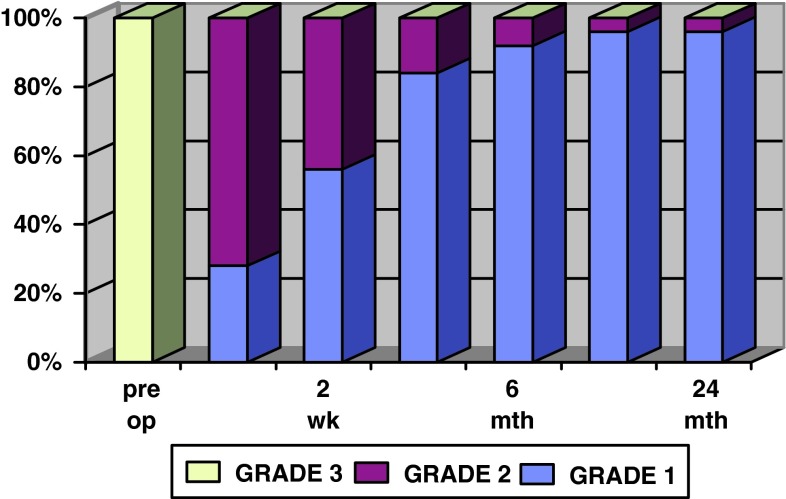
Fig. 4.
Grading of inferior turbinate, pre and postoperative comparision
Post Operative Size of Inferior Turbinate
Table 2.
Post operative size of inferior turbinate
| Grade | Grade 3 | Grade 2 | Grade 1 |
|---|---|---|---|
| Inf turbinate size pre op | 200 | – | – |
| IT 1 week post op | – | 144 | 56 |
| IT 2 week post op | – | 88 | 112 |
| IT 1 month post op | – | 32 | 168 |
| IT 6 month post op | – | 16 | 184 |
| IT 12 month post op | – | 8 | 192 |
| IT 24 month post op | – | 8 | 192 |
IT inferior turbinate
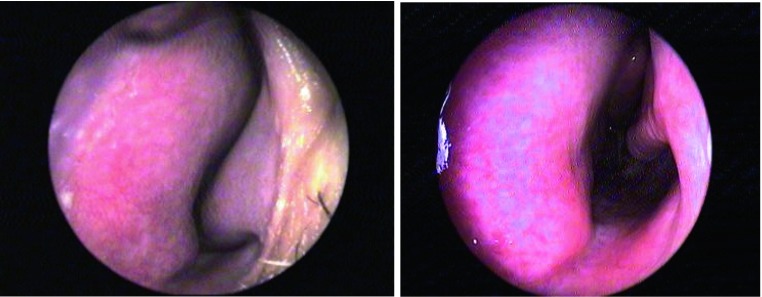
Fig. 5.
a Pre op left inferior turbinate b 6 months post op left inferior turbinate
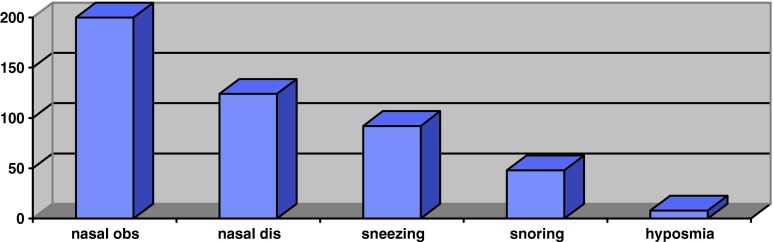
Asessment of Pain
See Fig. 6.
Fig. 6.
Visual analog scale for pain
Post operative pain was assessed using the visual analog scale for pain 1 week and 1 month post operatively. Patients were given questionnaires to scale the post operative pain on a scale of 0–10. Of the 200 patients only 12 patients (6%) complained of severe pain, 52 patients (26%) mild pain, 138 patients (69%) mentioned no pain post operatively 1 week following the procedure. No case of synechiae was observed in the follow up periods.
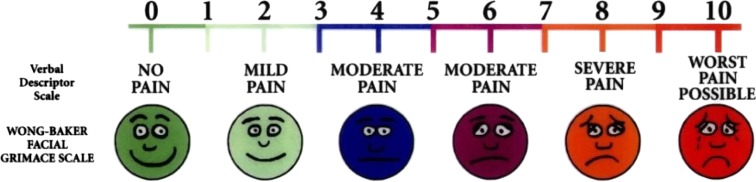
Assessment of Ciliary Function
Postoperative ciliary function was assessed by saccharin transit time and histopathological examination of the inferior turbinate mucosa.
Saccharin transit time in a normal subject is on an average 14–18 min. Patients included in this study with hypertrophied inferior turbinates had a mean saccharin transit test time of 14–16 min at the end of 6 months.
Histopathologically regeneration of the normal cilliary epithelium was seen by the end of 12 months with no sign of cilliary destruction and atrophy of the turbinates (Fig. 7).
Fig. 7.
a Pre operative- HPE: inferior turbinate mucosa. b Post operative- HPE: inferior turbinate mucosa.
Discussion
The gold standard for the treatment of the inferior turbinates hypertrophy is still missing. Several techniques have severe side effects in short and long term including bleeding, atrophic rhinitis, nasal dryness, crusting, pain and while others do not seem to be effective [17–20]. A wider nasal cavity does not necessarily mean that the nose function will be better [17, 21]. Thus, catastrophic techniques with no respect to nasal functionality, like total turbinectomy, are condemned by many authors [17, 22]. Many treatment methods have been reported with various results [17, 23–26]. Several studies report that treatment of inferior turbinate hypertrophy using bipolar RF offers an efficient alternative to other established methods [27]. By presenting our work we provide preliminary results of the treatment of turbinates hypertrophy with bipolar RF, under general/local anaesthesia. Advantages of this method comprise safety and convenience. It is an outpatient method with very few minor complications and with very minimal bleeding intraop needing no nasal packing. In addition its cost is rather reasonable in comparison with laser treatment, while its effectiveness regarding nasal obstruction, nasal discharge and improving the quality of life is very promising. Moreover with this technique, the mulberry type tails of the inferior turbinates are well amenable to treatment. Short term results were well comparable with other more sophisticated methods.
Conclusion
According to the results of our study, treatment of inferior turbinates hypertrophy in allergic/non allergic rhinitis patients using bipolar RF under local/general anaesthesia offers an efficient, cost effective, outpatient procedure with very rare minor complications.
References
- 1.Lippert BM, Werner JA. Nd: YAG laser light-induced reduction of nasal turbinates. Laryngorhinootologie. 1996;75:523–528. doi: 10.1055/s-2007-997626. [DOI] [PubMed] [Google Scholar]
- 2.Ottaviani F, Capaccio P, Cesana BM, et al. Argon plasma coagulation in the treatment of nonallergic hypertrophic inferior nasal turbinates. Am J Otolaryngol. 2003;24:306–310. doi: 10.1016/S0196-0709(03)00059-0. [DOI] [PubMed] [Google Scholar]
- 3.Coste A, Yona L, Blumen M, et al. Radiofrequency is a safe and effective treatment of turbinate hypertrophy. Laryngoscope. 2001;111:894–899. doi: 10.1097/00005537-200105000-00025. [DOI] [PubMed] [Google Scholar]
- 4.Passali D, Lauriello M, Anselmi M, et al. Treatment of hypertrophy of the inferior turbinate: long-term results in 382 patients randomly assigned to therapy. Ann Otol Rhinol Laryngol. 1999;108:569–575. doi: 10.1177/000348949910800608. [DOI] [PubMed] [Google Scholar]
- 5.Sapci T, Sahin B, Karavus A, et al. Comparison of the effects of radiofrequency tissue ablation, CO2 laser ablation, and partial turbinectomy applications on nasal mucociliary functions. Laryngoscope. 2003;103:514–519. doi: 10.1097/00005537-200303000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Elwany S, Gaimaee R, Fattah HA. Radiofrequency bipolar submucosal diathermy of the inferior turbinates. Am J Rhinol. 1999;13:145–149. doi: 10.2500/105065899782106715. [DOI] [PubMed] [Google Scholar]
- 7.Smith TL, Correa AJ, Kuo T, et al. Radiofrequency tissue ablation of the inferior turbinates using a thermocouple feedback electrode. Laryngoscope. 1999;109:1760–1775. doi: 10.1097/00005537-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Rhee CS, Kim DY, Won TB, et al. Changes of nasal function after temperature-controlled radiofrequency tissue volume reduction for the turbinate. Laryngoscope. 2001;111:153–158. doi: 10.1097/00005537-200101000-00026. [DOI] [PubMed] [Google Scholar]
- 9.Nuutinen J. Asymmetry in the nasal mucociliary transport rate. Laryngoscope. 1996;106:1424–1428. doi: 10.1097/00005537-199611000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Powell NB, Riley RW, Troell RJ, et al. Radiofrequency volumetric tissue reduction of the palate in subjects with sleepdisordered breathing. Chest. 1998;113:1163–1174. doi: 10.1378/chest.113.5.1163. [DOI] [PubMed] [Google Scholar]
- 11.Nq BA, Ramsey RG, Corey JP. The distribution of nasal erectile mucosa as visualized by magnetic resonance imaging. Ear Nose Throat J. 1999;78(159):163–166. [PubMed] [Google Scholar]
- 12.Smith TL, Correa AJ, Kuo T, Reinisch L. Radiofrequency tissue ablation of the inferior turbinates using a thermocouple feedback electrode. Laryngoscope. 1999;109:1760–1765. doi: 10.1097/00005537-199911000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Utley DS, Goode RL, Hakim I. Radiofrequency energy tissue ablation for the treatment of nasal obstruction secondary to turbinate hypertrophy. Laryngoscope. 1999;109:683–686. doi: 10.1097/00005537-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Elwany S, Gaimaee R, Fattah HA. Radiofrequency bipolar submucosal diathermy of the inferior turbinates. Am J Rhinol. 1999;13:145–149. doi: 10.2500/105065899782106715. [DOI] [PubMed] [Google Scholar]
- 15.Sapci T, Sahin B, Karavus A, Akbulut UG. Comparison of the effects of radiofrequency tissue ablation, CO2 laser ablation, and partial turbinectomy applications on nasal mucociliary functions. Laryngoscope. 2003;113:514–519. doi: 10.1097/00005537-200303000-00022. [DOI] [PubMed] [Google Scholar]
- 16.Bozkurt Z, Sapcı T, Sahin B, Akbulut UG. Results of radiofrequency tissue ablation. Kulak Burun Bogaz Ihtis Derg. 2002;9:30–36. [PubMed] [Google Scholar]
- 17.Hol Mk, Huizing EH. Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniques. Rhinology. 2000;38:157–166. [PubMed] [Google Scholar]
- 18.Berenholz L, Kessler A, Sarfati S, et al. Chronic sinusitis: a sequela of inferior turbinectomy. Am J Rhinol. 1998;12:257–261. doi: 10.2500/105065898781390046. [DOI] [PubMed] [Google Scholar]
- 19.Garth RJN, Cox HJ, Thomas MR. Hemorrhage as a complication of inferior turbinectomy: a comparison of anterior and radical trimming. Clin Otolaryngol. 1995;20:236–238. doi: 10.1111/j.1365-2273.1995.tb01856.x. [DOI] [PubMed] [Google Scholar]
- 20.Rettinger G, Christ P. Visual loss following intranasal injection. Rhinol Suppl. 1989;9:66–72. [PubMed] [Google Scholar]
- 21.Huizing EH. Functional surgery of the nasal turbinates. In: Bunnach H, Muntarbhorn K, editors. Asian rhinological practice. Siriyod: Bangkok; 1998. pp. 300–308. [Google Scholar]
- 22.Passali D, Lauriello M, Anselmi M, et al. Treatment of hypertrophy of the inferior turbinate: Long-term results in 382 patients randomly assigned to therapy. Ann Otol Rhinol Laryngol. 1999;108:569–575. doi: 10.1177/000348949910800608. [DOI] [PubMed] [Google Scholar]
- 23.Lippert BM, Werner JA. Long-term results after laser turbinectomy. Lasers Surg Med. 1998;22:126–134. doi: 10.1002/(SICI)1096-9101(1998)22:2<126::AID-LSM9>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 24.Seeger J, Zenev E, Gundlach P, et al. Bipolar radiofrequency-induced thermotherapy of turbinate hypertrophy. Pilot study and 20 month’s follow up. Laryngoscope. 2003;113:130–135. doi: 10.1097/00005537-200301000-00024. [DOI] [PubMed] [Google Scholar]
- 25.Moore JRM, Bicknell PG. A comparison of cryosurgery and submucous diathermy in vasomotor rhinitis. J Laryngol Otol. 1980;94:1411–1413. doi: 10.1017/S0022215100090253. [DOI] [PubMed] [Google Scholar]
- 26.Papadakis CE, Skoulakis CE, Nikolidakis AA, et al. Swiftlase inferior turbinoplasty. Am J Rhinol. 1999;13:479–482. doi: 10.2500/105065899781329638. [DOI] [PubMed] [Google Scholar]
- 27.Zenev E. Die bipolare Thermpotherapie der Nasenmuschelhyperplasie-Applikatorerprobung an Invivo-Gewebe. Berlin: Institut fur Med/technisce Physik und Lasemedezin, Universitätklinikum Benzamin Franklin Freie Universitat Berlin; 1999. [Google Scholar]