Abstract
The purpose is to summarize the experience in full endoscopic transsphenoidal resection of pituitary adenoma in 28 patients by rhinologist, and introduce the surgical skill of otolaryngologist, especially skills and cautions when operating inside nose. We removed pituitary adenoma in 28 patients via entirely endoscopic transsphenoidal approach with the help of special-designed instruments; we performed the procedure bloodlessly within limited time. The skill emphasized bilateral nostrils and four hands technique which was as delicate as possible not to scratch nasal mucosa or injure nasal frame. The special instruments included curette with suction, monopolar electrotome and bipolar coagulation forceps with suction, powered surgical equipments (Diamond Bur, Irrigation Tubing for Blades and Burs for nasal endoscopic surgery). Among 28 patients, there were 16 total resections, 8 subtotal resections, 3 partial resections, and 1 only biopsy due to excessive bleeding and hard nature. Of 19 patients with preoperative visual impairment, 12 patients had postoperative improvement in visual acuity and visual field. All the procedures were finished within 60 to 90 min. Complications seldom occurred except transient diabetes insipidus, especially no nasal-related signs or complications but 1 had epistaxis. The full endoscopic transsphenoidal surgery is a promising approach for pituitary adenoma resection. Multidisciplinary collaboration will lead to optimal cure for the patients. New technique and special-designed instruments can facilitate greatly this procedure.
Keywords: Nasal endoscopy, Pituitary adenoma, Complication, Surgical skill
Introduction
The pituitary adenoma is one of the most common encephalomas in neurosurgery or skull base surgery. Surgical removal is the preferred treatment of this tumor. Transsphenoidal approach has been the standard access in pituitary surgery. The traditional transsphenoidal approaches include sublabial transseptal, nasal columella transseptal, and endonasal one-nostril approach via operating microscope [1]. Nasal endoscopy has been applied clinically for several decades in rhinology [2]. Through the patient’s natural nasal air passage and ostium, endoscope can be utilized to examine and manipulate sphenoid sinus conveniently. Thus the endoscope has become an essential tool for transsphenoidal pituitary surgeries because of the panoramic view and the ability to remove the sella lesion just behind the sphenoid sinus. Jankowski and his colleagues [3] first reported successful removal via endoscopy in 3 pituitary adenomas. From then on, more and more surgeons committed themselves to endoscopic transphenoidal pituitary surgery. Many successful cases were also reported in China [4, 5].
Many articles which compared the outcome of nasal endoscopy with traditional microscopy transsphenoidal surgery had been published [6–10]. Some of them [6–8] concluded that nasal endoscopic procedure overmatched microscopic surgery in terms of duration, remission rate, rate of total or subtotal excision, and the iatrogenic complications. Other articles [9, 10] however, indicated that endoscopic pituitary surgery had no difference in outcome compared with microscopic approach. Actually, the outcome of endoscopic pituitary surgery is closely associated with the skill of playing nasal endoscopy; and the initial operation that has been performed inside nose. For the sake of this reason, the experience and skill of rhinologist would be undoubtedly significant. The first author is engaged in nasal endoscopic surgery for 17 years and has performed endoscopic pituitary surgery for 5 years. Herein we present our experience in this field, especially the surgical skills of otolaryngologist.
Materials and Methods
Patients
28 cases were reviewed retrospectively from November 2005 to Match 2010. All had the endoscopic pituitary surgery. Most of them were referred from ophthalmology; the others were from endocrinology and neurology. Among these patients, male and female were 11 and 17, aged between 27 and 73 years (median 43). Based on endocrine testing and postoperative pathology reports, there were 17 nonfunctional adenoma (9 cases had hypopituitarism), 3 growth hormone adenoma, 5 prolactinoma, 2 ACTH (adrenocorticotropic hormone) adenoma and 1 mixed adenoma.
The clinical history revealed 19 cases had visual impairment; 16 had headache; 1 had pituitary apoplexy; 5 amenorrhea; 5 abnormal lactation; 1 infertility; 3 acromegaly.
Considering the size and extension of the tumor on neuroimaging, the patients were sorted into 3 groups: Microadenoma (≤1 cm) 5 cases; large adenoma (1 cm ≤ tumor ≤ 3 cm) 9 cases; macroadenoma (≥3 cm) 14 cases. Furthermore, 6 cases invaded cavernous sinus, and 12 cases expanded to suprasellar area.
Surgical Procedure
C-shaped incisions were done in the bilateral septal mucosa with a long monopolar electrotome (Fig. 1); the incisions were opposite to the free edge of bilateral middle turbinates and reached the septal bone. The bilateral mucoperiosteum flaps were elevated. The vomer behind the incision, sphenoidal rostrum and anterior wall of sphenoid sinus were gradually removed by the back-bite bone punch and microdrill (Diamond Bur for skull base surgery). Afterwards the back part of septum opposite to the middle turbinate became flexible; the sphenoethmoidal recesses were expanded; so the endoscope and instruments could be introduced into this narrow space and advanced in and out. After the ostiums of sphenoid sinuses were identified, the bilateral ostiums would be enlarged medially and meet each other. The anterior wall of the sphenoidal sinuses was removed and the sphenoidal sinuses were open at this moment. Attention was paid not to strip the sphenoidal sinus mucosa because inadvertent stripping caused unwanted oozing of blood from the bony sinus wall. Then the nose and sphenoid sinuses should be flushed with Iodophor. Once the sellar floor was identified, the sphenoidal sinus mucosa in this area was coagulated by bipolar coagulation forceps with suction. A bone window was opened with diamond bur; then the dura mater was exhibited and punctured with a long and fine syringe needle so as to obviate carotid artery and cavernous sinus. Coagulation was performed and a cruciate incision was made in the midline of the dura. The lesion could be removed using the curette and basket with suction. If the lesion invaded sellar diaphragm, Valsalva maneuver which was performed through anesthesia apparatus might make it sink from the suprasellar cistern into the sellar cavity. When the bleeding was controlled, an angled 30 or 45° endoscope was then advanced sequentially into the tumor resection cavity to insure no tumor remnants. Finally the sellar floor was reconstructed (Figs. 2, 3, 4).
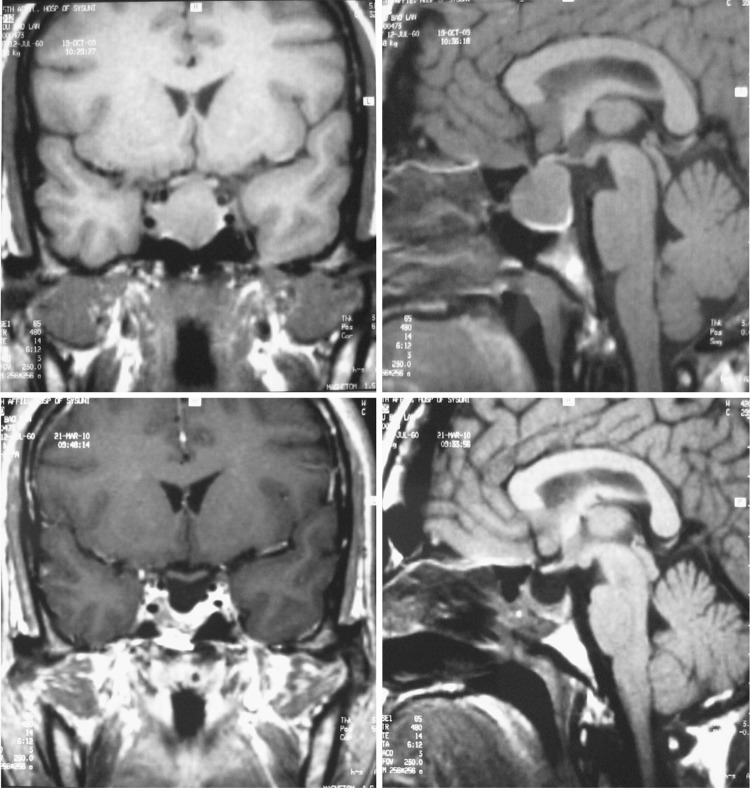
Fig. 1.
Left 1: Sphenoethmoidal recess. Triangle indicates anterior wall of sphenoid sinus; square indicates superior concha; cycle indicates middle concha. The black line indicates the incision in septum. The ostium is lateralized and invisible owing to well pneumatized sphenoid sinus. Left 2: The ostium of sphenoid sinus. Left 3: Sellar floor is visible after sphenoidotomy. Right: Sellar floor 6 months after operation, the scar is visible. Notable: Both the noses in left 1 and left 2 are atrophic. In most of Chinese, the sphenoethmoidal recess is very narrow and invisible before widened
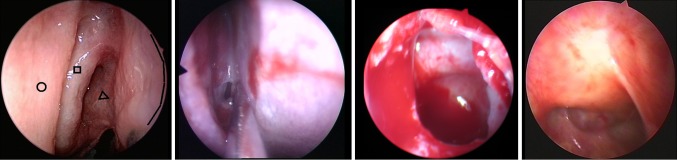
Fig. 2.
The MRI of the patient with nonfunctional pituitary adenoma. The above is preoperative; the under is postoperative 1 week
Fig. 3.
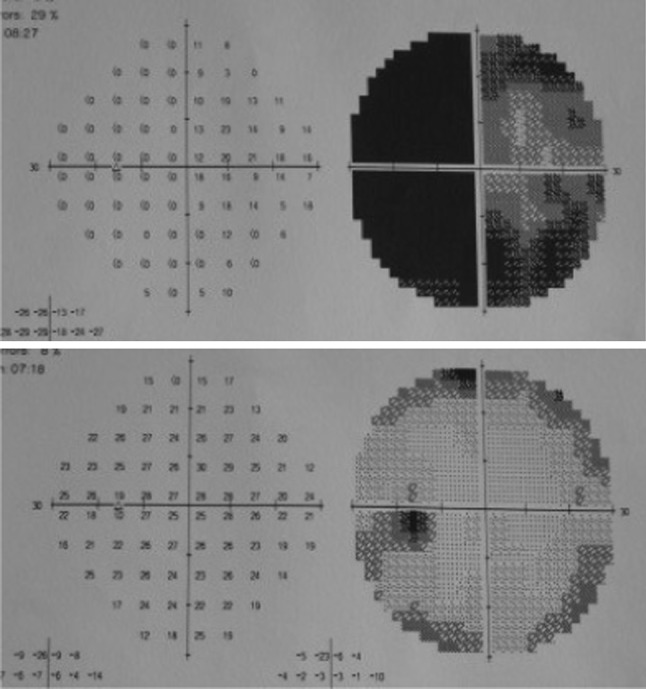
The visual field on left eye of above-mentioned patients. The above one is preoperative; the under one is postoperative
Fig. 4.
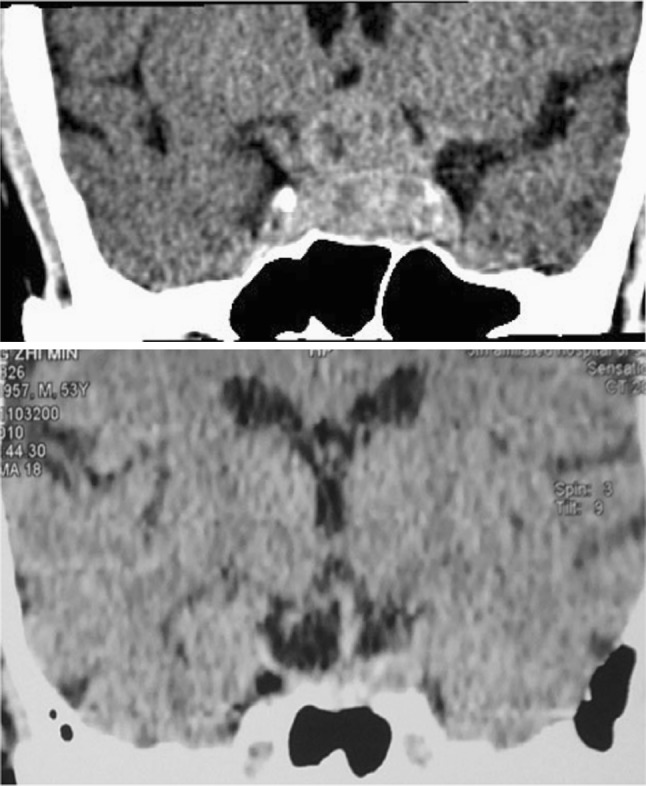
The CT of another patient with nonfunctional pituitary macroadenoma invading suprasellar and left cavernous sinus. The above one is preoperative CT image; the under is postoperative CT. Ramnant is visible in left side, and the regrowth was observed 1 year after operation; the patients was referred to radiotherapy. The left eye of this patient was only weak light perception in 4 days before surgery and gained remission in the next day after operation
In order to avoid the accidental encephalic complications, a neurosurgeon was invited to assist our performance and prepare for the emergency.
Surgical Skill
Create Working Space
Expand the Space of Nasal Cavity
Cottonoids soaked with a mixture of 15 ml 1% Tetracaine and 2 ml 1/1,000 adrenaline; were inserted gently into each narrow space among sphenoethmoid recess, middle turbinate, middle meatus, and common meatus. This procedure was repeated (10 min/each time), and it could decongest the nasal mucosa so as to enlarge the space in the nasal cavity, what’s more, it supplied an adequate surgical pathway for the endoscope and instruments in and out. This procedure was time-consuming and boring but absolutely essential.
Widen the Sphenoethmoid Recess
Sphenoethmoid recess is such a narrow tunnel in most individuals which limits the straight endoscopic vision. We widened this space through two measures. (1) Coagulating posterior part of middle turbinate and removing it (the removal was immersed in antibiotics solution, available for sellar repair). We wouldn’t like to laterally fracture the middle turbinate, because the potential synechia might impede the mucociliary system in middle meatus; and even so, no adequate space would be gained; (2) removing the vomer, rostrum and anterior wall of sphenoid sinus under mucoperiosteum with a microdrill and bone punch. Thus the posterior part of septum was flexible and easy to be pushed contralaterally. This maneuver could refrain from a middle turbinate resection.
Control the Nasal Bleeding
Containing abundant blood vessel, the nasal mucosa is extremely prone to ooze especially in inferior turbinate. There were several details to prevent oozing of blood. (1) Cottonoids soaked with high concentration adrenaline could adequately decongest and contracted the mucosa. (2) Attention should be paid to less touching the mucosa to the greatest extent. All instruments such as suctions, forceps should be fine and delicate with smooth surface lest they scratch the tender mucosa. (3) A long monopolar electrotome was introduced to incise the mucoperiosteum of nasal septum, coagulate and cut at the same time. If the medial mucosa of middle turbinate oozed, coagulation should be performed point to point with bipolar forceps (no sweeping coagulation). (4) The mucosa around the ostium should be coagulated before sphenoidotomy. (5) The septal branch and the middle concha branch of sphenopalatine vessel had to be coagulated to prevent intraoperative and postoperative nasal bleeding. (6) The nasal cavity should be flushed with a great deal of warm saline, which cleaned out any nasal secretion and was favor of hemostasis.
Two-nostril and Four-hand Manipulation
If small nostril or excessive sellar hemorrhage presented, we would insert endoscope and instruments into one nostril (usually the right), meanwhile, the assistant inserted a suction tube into the other in order to clear the surgical vision. Recently an author [11] summarized and nominated it as “bilateral nostril technique”.
Protect the Nasal Mucosa and Frame
The details were as follows. (1) The cottonoids but not gauze should be used to decongest the nasal mucosa lest the scratch or damage were added to the delicate mucociliary system; (2) The lateralized middle turbinate (if so) should be replaced, and then a piece of Gelatin Sponge was inserted into middle meatus to prevent potential synechiae [3, 12]; (3) All prolapsed mucosa should be repositioned before ending the operation; (4) All synechiae were separated by nasal packing material; (5) If no CSF (cerebrospinal fluid) leak presented, there was no need in nasal packing which may hurt the mucosa and afflict the patients; (6) All free bone pieces should be cleaned out, and the nasal cavity was irrigated with saline solution to remove blood clot. This would promote the recovery of the nasal mucosa after operation; (7) Nasal steroids (Rhinocort, AstraZeneca) and secretolytic (Gelomyrtol Forte) drug would be administrated for 12 weeks, and the nose was douched until postoperative 4 weeks.
Reconstruct the Sellar Floor
The removed posterior portion of middle turbinate could be used to reconstruct sellar opening (7 patients). In cases without turbinectomy (21 patients), we used the septal mucosa to repair the opening (8 patients). Yano [11] detailed that flaps of nasal septum could be used to repair sellar floor. In the cases without evidence of CSF leak (13 patients), the incised dura was replaced and fixed with gelatin sponge (soaked with antibiotics), left without reconstruction.
Special Designed Instruments
Special designed instruments could greatly facilitate the endoscopic surgery for pituitary adenoma, and improved the efficacy and safety simultaneously. The main instruments included (1) the powered surgical equipments (Diamond Bur and Blades with irrigation and suction for endoscopic sinus surgery. Medtronic, Inc); (2) the curette and basket with suction, which could make the surgical vision clearer; (3) the electrotome and bipolar coagulation with suction, which control the bleeding exactly and non-foggedly; (4) the long and fine electrotome, which could incise the mucosa bloodlessly. The last three instruments were self-made by the first author, but the commercial production had been already available.
Results
Removal of the Tumor
According to the imaging of postoperative CT scan, total resection was demonstrated in 16 patients; subtotal resection (the extent of removal was greater than 90%) was in 8 patients; partial resection was in 3 patients. Only biopsy was done in one patient (GH secreting tumor) owing to unexpected excessive bleeding intra-operatively and hard quality of the tumor. Among 3 cases with partial resection, 2 had tumor growth seen on CT in the 6 months follow-up period; one resorted to radiotherapy, but the other refused and eventually lost to follow-up. All the procedures were completed within 90 min.
Visual Remission
Visual acuity improved evidently in 12 of the 19 patients with preoperative visual impairment; the rest 7 patients who referred to our hospital because one or two eyes were totally blind (no light perception) lasting for at least 6 months, had no improvement in their visual acuity.
The Remission in Endocrinology
The follow-up for endocrinology was carried out by endocrinologist from 3 days to 1 year after operation (2 patients lost to follow up after 3 months postoperatively). Among 17 patients with nonfunctional adenoma (9 had anterior pituitary insufficiency), 4 of them didn’t get any remission, and therefore the hormone replacement therapy was required. Two of 3 patients with GH-secreting tumor gained remission. Among the 5 prolactinomas, 2 gained remission; and 2 who finally missed follow-up had no remission according to the postoperative hormone test; the last one still had abnormal milk secretion and sterility. One of 2 ACTH tumors attained remission. The single patient with mixed adenoma was lost to follow up finally.
Complications
Eleven patients had transient diabetes insipidus, which persisted no longer than 7 days. No other complications were observed. The patients were monitored endoscopically when they visited periodically whereas some of them eventually were lost to follow up. None of the patients had any other nasal complaints such as obstruction, crust, dry, anosmia and hyposmia except one epistaxis (treated in outpatient and cured).
Discussion
A large proportion of our patients were referred by ophthalmologist; so most of them had non functional macroadenoma which only caused visual deterioration. Because some of them had been misdiagnosed and blind for a long time, thus visual improvement couldn’t be obtained even if the tumor had been total removed.
The comparison between microscopic approach and transnasal endoscopic approach had been discussed in a great number of literature [3–10]. We have no experiences in microscopic pituitary adenoma surgery; so we simply focus on the practical skill of transnasal endoscopic pituitary surgery. Because this kind of procedure is composed of three phases (nasal, sphenoidal, and sellar), the skill from the otolaryngologist is instructive for the physicians who may be concerned about it. Nasal cavity is very narrow space, moreover neighbors on vital structures such as orbit, optic nerve, and anterior skull base; the bones which separate the structures are very weak and prone to be damaged by accident. On the other hand, nasal mucosa is innervated and vascularized by a great deal of small vessels, so the slight damage can lead to blood oozing. Therefore expanding the pathway for endoscopy is a key to clear surgical vision.
Some reports [13] from neurosurgeon often emphasized on “single nostril” approach. According to the experience of rhinologist, “two nostrils” approach is more convenient than “single nostril”. It is true especially in the scene of macroadenoma, bleeding adenoma, hard tumor, and small nostril. The surgeon have to hold the endoscope with one hand while working with the other one; so developing another route for assistant to insert a suction tube will be certainly helpful for the main surgeon. Yano [11] had detailed it as “bilateral nostrils technique”.
Some clinical investigations [14, 15] suggested that the learning curve to grasp the endoscopic pituitary surgery required 40 to 80 operations. We consider this number never enough for a surgeon to be proficient in the practice of nasal endoscope. In fact, neurosurgeons have little opportunity to practise the manipulation of endoscope except in operation. Rhinologists undertake pituitary surgery infrequently, but they perform a large number of operations in treating chronic sinusitis, and often practise examining the nose with endoscope. It usually requires 500 cases of practice for fresh otolaryngologists to be familiar with both endoscopy and endoscopic anatomy. So the authors propose that the neurosurgeons who pursue endoscopic pituitary surgery should often attend the routine nasal endoscopic examination in ENT clinics, in order to become proficient rapidly in endoscopy.
Nose isn’t a life-threatening organ, but it interacts with environment constantly. The function of nose can influence the life quality profoundly, especially when the patients live in an air-polluted environment. Excessive damage to the nose will lead to refractory nasal trouble [16]. Inappropriate endonasal performance is prone to give rise to nasal morbidity [8]. We hope our skill presented above is helpful to reduce the nose related complications during the pituitary surgery.
There have been three decades since the introduction of nasal endoscopy; a lot of special designed equipments and instruments have been developed and modified to accommodate the nature of endoscopic procedure. These instruments ensure the efficacy and safety of endoscopic procedure. Some innovations such as ultrasonic curette [17], suction basket/curette and suction coagulator can facilitate this procedure greatly.
Neurosurgery plays the leading role within endoscopic pituitary surgery; but one discipline alone will never be able to cure the patients perfectly. So, rhinologist, ophthalmologist, endocrinologist and gynecologist also matter. The author suggested that a pituitary center in which multidiscipline collaborated should be founded in large medical center. This could be a best choice to treat pituitary.
In the pituitary surgery, the procedure by nasal endoscope has a lot of advantages that microscope can’t afford [3–15, 17], though it also has several disadvantages, however which will be overcomed along with the continuously developing of new instruments and new techniques.
Acknowledgments
Conflict of Interest
All authors have no competing interest to declare.
Contributor Information
Yun-ping Fan, Phone: +86-13005763411, FAX: +86-756-2261253, Email: fanyunping@sohu.com.
Wei-ping Wen, Email: wwp1901@yahoo.com.cn.
Hua-bin Li, Phone: +86-13802966937, Email: Noseli@163.com.
References
- 1.Senior BA, Ebert CS, Bednarski KK, Bassim MK, Younes M, Sigounas D, et al. Minimally invasive pituitary surgery. Laryngoscope. 2008;118:1842–1855. doi: 10.1097/MLG.0b013e31817e2c43. [DOI] [PubMed] [Google Scholar]
- 2.Kennedy DW. Functional endoscopic sinus surgery. Tech Arch Otolaryngol. 1985;111:643–649. doi: 10.1001/archotol.1985.00800120037003. [DOI] [PubMed] [Google Scholar]
- 3.Jankowski R, Auque J, Simon C, Marchal JC, Hepner H, Wayoff M. Endoscopic pituitary tumor surgery. Laryngoscope. 1992;102:198–202. doi: 10.1288/00005537-199202000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Xu YG. Evolutions of transsphenoidal pituitary surgery: personal experience in 15 years. Chin J Neurooncol (Chin) 2009;7:17–21. [Google Scholar]
- 5.Zhang QH, Ni ZL. Endoscopic transsphenoidal approach in surgical treatment of pituitary adenomas. Chin Minim Invasive Neurosurg (Chin) 2001;6:76–78. [Google Scholar]
- 6.Charalampaki P, Ayyad A, Kockro RA, Perneczky A. Surgical complications after endoscopic transsphenoidal pituitary surgery. J Clin Neurosci. 2009;16:786–789. doi: 10.1016/j.jocn.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 7.D’Haens J, Rompaey K, Stadnik T, Haentjens P, Poppe K, Velkeniers B. Fully endoscopic transsphenoidal surgery for functioning pituitary adenomas-A retrospective comparison with traditional transsphenoidal microsurgery in the same institution. Surg Neurol. 2009;72:336–340. doi: 10.1016/j.surneu.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 8.Petry C, Soares LC, Pereira-Lima J, Gerbardt K, Sant GD, Oliveira MC. Oronasal complications in patients after transsphenoidal hypophyseal surgery. Braz J Otorhinolaryngol. 2009;75:345–349. doi: 10.1590/S1808-86942009000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins TS, Courtemanche C, Karakla D, Strasnick B, Singh RV, Koen JL, et al. Analysis of transnasal endoscopic versus transseptal microscopic approach for excision of pituitary tumors. Am J Rhinol. 2008;22:649–652. doi: 10.2500/ajr.2008.22.3246. [DOI] [PubMed] [Google Scholar]
- 10.O’Malley BW, Jr, Grady MS, Gabel BC, Cohen MA, Heuer GG, Pisapia J, et al. Comparison of endoscopic and microscopic removal of pituitary adenomas: single-surgeon experience and the learning curve. Neurosurg Focus. 2008;25:E10. doi: 10.3171/FOC.2008.25.12.E10. [DOI] [PubMed] [Google Scholar]
- 11.Yano S, Kawano T, Kudo M, Makino K, Nakamura H, Kai Y, et al. Endoscopic endonasal transsphenoidal approach through the bilateral nostrils for pituitary adenoma. Neurol Med Chir (Tokyo) 2009;49:1–7. doi: 10.2176/nmc.49.1. [DOI] [PubMed] [Google Scholar]
- 12.Fan YP, Shi JP, Xu G. Iatrogenic rhinosinusitis. Chin Med Abstr Otolaryngol (chin) 2005;20:153–154. [Google Scholar]
- 13.Qin J, Lei T, Shu K, Chen JC, Li L. Removal of pituitary adenomas by surgery through endoscope-assisted endosnasal transsphenoidal approach and study of microanatomy related to this approach to sellar region Chin. J Clin Neurosurg. 2007;12:202–204. [Google Scholar]
- 14.Kena K, Ihsan A, Dileck O, Burak C, Gurkan K, Savas C. The learning curve in endoscopic pituitary surgery and our experience. Neurosurg Rev. 2006;29:298–305. doi: 10.1007/s10143-006-0033-9. [DOI] [PubMed] [Google Scholar]
- 15.Cappabianca P, Cavallo LM, Colao A, de Divitiis E. Surgical complications associated with the endoscopic endonasal transsphenoidal approach for pituitary adenomas. J Neurosurg. 2002;97:293–298. doi: 10.3171/jns.2002.97.2.0293. [DOI] [PubMed] [Google Scholar]
- 16.Sethi DS, Leong JL. Endoscopic pituitary surgery. Otolaryngol Clin N Am. 2006;39:563–583. doi: 10.1016/j.otc.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Cappabianca P, Cavallo LM, Esposito I, Barakat M, Esposito F. Bone removal with a new ultrasonic bone curette during endoscopic endonasal approach to the sellar-suprasellar area: technical note. Neurosurgery. 2010;66:E118. doi: 10.1227/01.NEU.0000365929.26699.02. [DOI] [PubMed] [Google Scholar]