Abstract
Development of endoscopic endonasal surgery has made it possible to reach diseases located in difficult areas of nose, paranasal sinuses and skull base. Technical advancements such as development of electromagnetic navigation system have greatly revolutionized the field of endoscopic endonasal surgery. Electromagnetic navigation system has improved the precision and accuracy of performing surgery and complication rates. This paper will emphasize on the technical aspects, mechanism of working, advantages and disadvantages of using electromagnetic navigation system and compare it with optic tracking system. While navigation system has many benefits, it should be used as an adjunctive to the surgical skills of a surgeon but not as a substitute.
Keywords: Navigation system, Electromagnetic system, Endoscopic endonasal surgery, Skull base surgery, Pituitary tumor, Sinus surgery
Introduction
Advent of Endoscopic Sinus Surgery (ESS) has paved way to treating the diseases of skull base and orbit in addition to treating the diseases of sinuses. Several technical advancements in pre-operative procedures like the use of high-resolution computerized tomography and intra-operative techniques such as the use of better nasal endoscopes have enhanced the scope of performing difficult surgeries [1]. Despite the availability of these techniques, surgeons are sometimes challenged by intra-operative complications such as bleeding, trauma to the central nervous system, and even death due to the complex anatomy of this region [1]. Narrow spaces, anatomical variations in individual patients, and blood obscuring the visibility of surgical field are some of the factors that limit surgeon’s ability to locate the exact position of an instrument. Most intra-operative complications arise due to disruption of vessels and nerves while using surgical instruments, especially by the beginners [2].
Use of image guidance system and development of Computer Aided Sinus Surgery (CASS) has markedly improved the scope of ESS and the complication rate [1]. These procedures improve the precision with which a surgeon could use instruments and they offer accuracy up to 2 mm or better. Electromagnetic system is being widely used in recent times because it has better accuracy in performing surgeries. Navigation employs the use of electromagnetic system to locate anatomical landmarks while performing ESS and anterior skull base surgery. Use of electromagnetic navigation system has simplified the procedure of locating anatomical landmarks for the surgeon [1]. It has improved the ability to perform complex surgeries such as extended sinus diseases (extensive polyposis, fungal sinusitis, mucocele, distorted anatomy, and revision surgeries), skull base surgeries (pituitary tumor excision, removal of disease from pre-sellar and sellar regions, clival tumor removal), orbital surgeries (orbital decompression, optic nerve decompression), and odontoid process excision with ease and accuracy [1, 3, 4]. The use of electromagnetic navigation system has greatly reduced the occurrence of post-operative complications and the duration of hospital stay [3, 4].
CASS is a combination of the use of Computed Tomography (CT) and endoscopic images with a three-plainer navigation system. Use of endoscopy for performing pituitary tumor removal was initially proposed by Guiot in 1963 [5]. Through the work of other eminent surgeons and scientists, endoscopic endonasal transsphenoidal approach to reach sella is now the most preferred method to perform pituitary tumor excisions [6, 7]. Use of electromagnetic navigation system is the most significant recent advances for pituitary tumor excision and other skull base approaches [8–10].
We describe the technical aspects of electromagnetic navigation system, advantages of using the system in endonasal endoscopic skull base and sinus procedures and compare it with optic tracking navigation system. The electromagnetic navigation systems used in our Department of Otorhinolaryngology at University Klinikum, Graz are Instatrak-3500 plus from GE Health system USA, Fusion from Meditronics USA and Fiagon from Germany.
Technical Aspects and Working of Navigation System
Components of Navigation System
We are describing the components and working of Fiagon Electromagnetic Navigation system from Germany. This navigation system consists of navigation screen, navigation module, and tracking pointer. There are four windows in the 18″ navigation screen; three of which display raw CT and Magnetic Resonance Imaging (MRI) data of orthogonal cross-sectional images of the axial, coronal, and sagittal planes of the patient and the fourth windows displays the video image of the surgical field as visualized by the endoscope. The navigation module is equipped with a DVD or CD drive, USB port, plug points for navigation sensor, patient localizer, and pointer system. The pointer system is equipped with a connecting plug, sensor cable, and a pointer (Fig. 1).
Fig. 1.
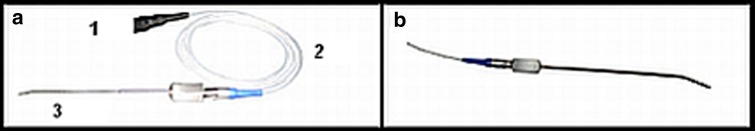
Picture showing various components of the pointer system. (a) Fine pointer-1.5 mm used for ear surgeries, in which 1 is connecting plug, 2 is sensor cable and 3 is fine point. (b) Flex pointer-malleable pointer that can reach any area of the brain with high precision and accuracy
The data obtained from pre-operative CT, MRI is stored in DICOM 3.0 format in a CD ROM. Image is loaded into the workstation through a CD, or DVD; USB stick, or network. Surface registration is used for image to patient registration in Fiagon system. Other navigation systems are equipped with automatic instrument recognition and dual instrument tracking features. The size of CT matrix is 512 × 512 pixels (pixel is the smallest element of a picture that can be represented).
The data obtained from CT and MRI scans is processed and radiological images of patient’s head are generated [11]. Images generated from CT data have a size of 512 × 512 × 170 voxels (voxel is a volumetric pixel), where each voxel is 0.44 × 0.44 × 1 mm, while the images generated from MRI data have a size of 512 × 512 × 100 voxels where each voxel is 0.4 × 0.4 × 1 mm [11].
Using Electromagnetic Navigation System
A detailed pre-operative clinical evaluation and imaging studies precede the use of navigation system in the operating room.
Pre-Operative Evaluation
Pre-operative evaluation of the patient first begins by assessing the general condition of the patient and evaluating cardio and respiratory parameters. These help in determining the patient’s fitness to be operated under general anesthesia. This is followed by a thorough examination of the neurological, endocrinological and ophthalmological systems. MRI is performed and cut sections of 2 mm are obtained that delineate the soft tissue anatomy of the skull base area especially the sellar and pre-sellar regions. CT is performed and it helps to define the bony anatomy of paranasal sinuses; pneumatization of sinuses; anatomical orientation of the sphenoid sinus to the surrounding structures with special reference to carotid artery, optic nerve, cavernous sinus, sellar, and pre-sellar areas. All this data from the imaging study is transferred to the workstation in the operating room and is used for the purpose of registration and navigation during the course of the surgery.
Anesthesia
Patient is operated under Total Intravenous Anesthesia.
Positioning the Patient
Patient is placed in supine position with the level of the head above the level of the heart. After induction of anesthesia a head set (caliper) is securely placed on the patient’s head. A reference pointer is fixed to the caliper that helps in registration and calibration. Patient’s head is freely positioned so that it could be easily moved during the course of the surgery to expose the anatomy of the lesion (Fig. 2).
Fig. 2.

Picture demonstrating patient set up on the surgical table with head set attached. (a) Demonstrates patient’s set up on the operating table. (b) Insert showing head module attached to the patient’s head
Registration of Apparatus
Registration is the process by which the position of an instrument in the surgical field is correlated with the CT images of the patient that were obtained pre-operatively. During this process, a tracking probe is registered to show its position with respect to the orthogonal CT images of the patient. A set of cross hairs or asterisk mark moves across the CT image in accordance with the movement of the tracking probe, but this varies from system to system. The head set is securely strapped to patient’s head and it moves along with the patient’s head in order to maintain registration throughout the surgical procedure.
Setting Registration Markers
Three anatomical markers are set by selecting bony prominences that are located directly beneath the skin. A triangular electromagnetic field is created by selecting three reference points. Two of these reference points are the lateral canthi of the right and left eyes and the third point is the base of the philtrum. In this triangular field using the tip of the reference pointer, the points that are selected have to be touched. Successfully touching an anatomic position generates a confirmation tone. Surface registration is used in Fiagon navigation system, automatic registration is used in Instatrak 3500 plus. Registration method varies from system to system (Fig. 3).
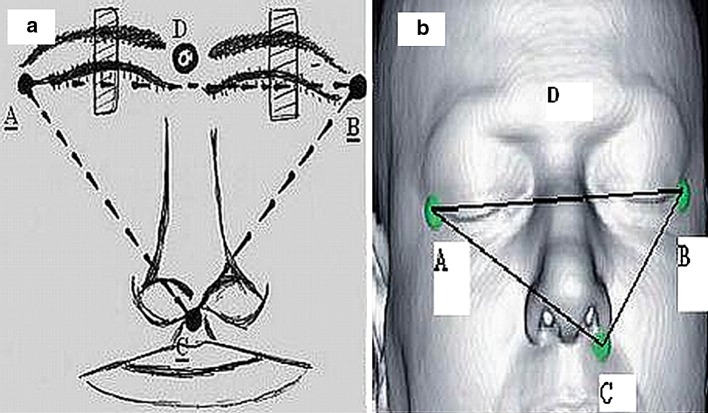
Fig. 3.
Picture or photograph demonstrating the three reference points of the triangular electromagnetic field. (a) A triangular electromagnetic field is created by selecting three reference points. Reference points A is located ≤2 mm medial to the right lateral canthus, point B is located ≤2 mm medial to the left lateral canthus, point C is located 2 mm from the base of the nasal philtrum, point D is a reference point where callipre is located. (b) Triangular mapping of the patient’s face
Testing of Accuracy
The accuracy with which the navigation system works is then verified by testing known landmarks on the patient’s face and correlating their position with the CT images. The data obtained from this process is saved and utilized to monitor the accuracy of the device during the surgery. The role of navigation system is vital in localizing a difficult frontal sinus, locating small sphenoid sinus, delineating skull base contour during a revision procedure, and distinguishing smooth-walled peripheral cells from surrounding landmarks [2] (Fig. 4).
Fig. 4.
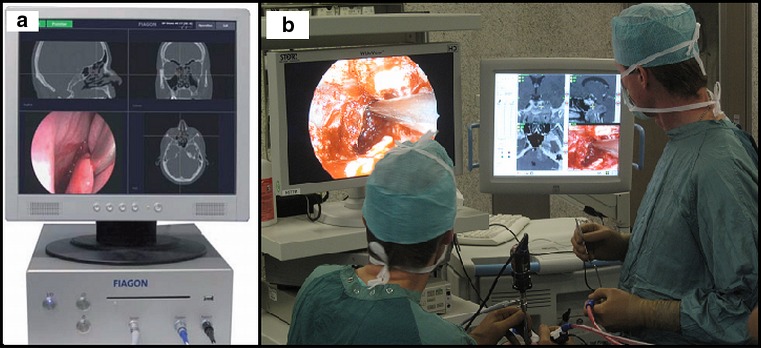
Picture of a surgical image on the navigation screen. (a) Picture demonstrating three orthogonal view—coronal, sagittal, and axial along with a 3D endoscopic image. (b) Picture demonstrating surgeon’s view of the endoscopic panoromic surgical field and the navigation screen
Discussion
The use of navigation technique was introduced into the field of Otorhinolaryngology in 1988 by Schlondorff [12]. Introducing navigation to ESS has contributed immensely to the development and progression of ESS. A combination of these two techniques has opened the opportunity to explore new surgical approaches and perform minimally invasive surgeries.
Indications
There are several indications to using navigation technique. Navigation technique plays a vital role in the resection of extensive diseases because anatomic landmarks are often destroyed in such cases [1]. Approaching sellar, parasellar and orbital areas has become much safer and easier ever since navigation system has been introduced. These areas are now being explored with greater accuracy and precision [3]. In cases of revision surgeries where there is extensive scarring and adhesions, navigation helps in identifying the distorted landmarks and distinguishing pathological lesions from normal areas [4, 6, 7]. Tumors residues that are not visible through endoscope can be revealed through navigation and complete resection of tumor can be performed in such cases [7].
Contraindications
Use of electromagnetic navigation system has to be avoided in patients that are installed with electronic devices to the brain or the nervous system, however optical tracking navigation system can be used in such patients. Use of navigation system was previously contraindicated in patients with cardiac pacemakers, but recent development in medical technology has enabled the use of navigation system in these patients.
Precautions
Use of electromagnetic devices like cell phones, pagers has to be avoided while using a navigator as they interfere with the working of the system. The electrical ratings prescribed by the system manufacturers should not be exceeded while performing the surgery.
Advantages
Navigation system offers the possibility to explore paranasal sinuses completely and helps in removing small cells that are lodged in narrow spaces [2]. Sphenoid sinus that has septations or altered anatomy can be approached with greater surgical precision [2]. Navigation technique makes it easier to approach ethmoid sinus and frontal sinus anatomy [2]. It helps in easy identification of anatomical landmarks that may have been distorted or made ambiguous by disease process [2]. Navigation technique provides the opportunity to reach difficult areas of the brain that could not have been accessed without retracting the cerebellum or causing neurovascular damage [6]. Navigation has improved the safety with which difficult procedures are performed because it provides accuracy up to 2 mm or better [3]. It has improved the precision with which a surgeon locates anatomical landmarks during the surgery [13]. Post-operative morbidity can be reduced by reducing the extent of neurovascular damage caused during the surgery by using a navigator [2].
Disadvantages
Navigation system requires training and experience on the part of the surgeon and cannot be used by beginners. Registering the tracking probe and important landmarks before beginning the surgery could be time consuming. Setting up imaging system is time-consuming (takes about 10–15 min) and costly [14]. Any crash in the computer system could cause failure of the navigation system. Overenthusiastic dissection by the surgeon could cause damage to vascular structures and complicate the surgery. Wide resection of the nasal turbinates or ethmoid cells can damage lamina cribrosa and cause CSF leakage [6]. Wide resection of medial pterygoid could cause injury to vidian nerve and anterior genu of carotid artery [6]. Despite the availability of navigation system the surgeon needs to have good surgical skills and knowledge about anatomy of the surgical field. Navigation system is an asset but not a substitute to the skills of the surgeon [7].
Comparison Between Optical Tracking Navigation Systems
Optic tracking navigation system is another type of navigation system in which an overhead digitizer or camera array is placed in line of sight with the surgical instruments and reference frame [15, 16]. If the line of sight is disturbed at any point during the surgery, the orthogonal images on the navigation screen are disturbed. The differences between optical and electromagnetic tracking systems are described in Table 1 [16, 17].
Table 1.
Comparison between optical and electromagnetic tracking systems
| Electromagnetic tracking system | Optical tracking system | |
|---|---|---|
| Registering probe | A registration probe is used which is an electro-magnetic sensor and it is completely integrated with the headset | Four Infra-red light-emitting diodes are used and the positions of these diodes are measured through an infra-red 3-D based localizer |
| Headset | A headset which has a navigation sensor is placed on the patient’s head | A headset permitting attachment of reference frame with light-emitting diodes for optical tracking is placed on the patient’s head |
| Registration | Surface registration protocol in which several anatomically distinct positions on the patient’s face are touched is used in Fiagon system, automatic registration is performed in Instatrak 3500 plus and Fusion systems | Point merge protocol in which anatomical fiducial points are used for marking or surface merge protocol where contour mapping is used for marking are the registration protocols commonly used |
| Anatomical contours | Lateral canthi of both the eyes, base of the nasal philtrum are the typically used contours | Medial brows, nasal dorsum, tragi are the typically used contours |
| Registration verification | Registration is verified by localizing known bony landmarks on the face where the skin is tightly adherent to the bone | Registration is verified by localizing known bony landmarks on the skull and in the nasal cavity |
| Instrument localization | Instrument can be localized within the triangular electromagnetic field at any point during the surgery and exact anatomical location can be verified | Interruption in the line of sight between the overhead digitizer, surgical instrument or the surgeon’s operating hand could lead to disturbance in the anatomical location |
Future Directions
CT images that delineate bony structures benefit otolaryngologists better and MRI guidance helps neurosurgeons better by providing in enhanced visualization of intracranial soft tissues. Integrating CT and MRI as one image guidance system could benefit both otolaryngologists and neurosurgeons to integrate their work [2]. Further development in the field of bioengineering could make the process of registration and usage of navigator less time consuming and more user friendly to beginners. Techniques that use fluorescent dyes to differentiate tumor cells from normal areas can be used along with intra-operative navigation system to make tumor identification and removal more effective. The navigation screen size can be reduced and made more compact.
Robotic surgery can be integrated with navigation system to develop an advanced surgical technique. Robot assisted surgery uses a surgical robot that has four articulated arm ports [18]. One arm port carries a dual-channel endoscope coupled with a camera for 3-D visualization of the surgical field, the other two arm ports carry right and left surgical arms that permit surgical manipulations, the fourth arm port is used as a spare arm that could be used for retraction or for inserting another instrument. Robotic surgery provides the opportunity to perform a two-handed tremor free procedure and eliminates the need for manual stabilization [18–20]. Combining robotic surgery with navigation technique could help in further progression of endoscopic approach to skull base and offer the scope to perform surgeries with greater accuracy and precision (Fig. 5).
Fig. 5.
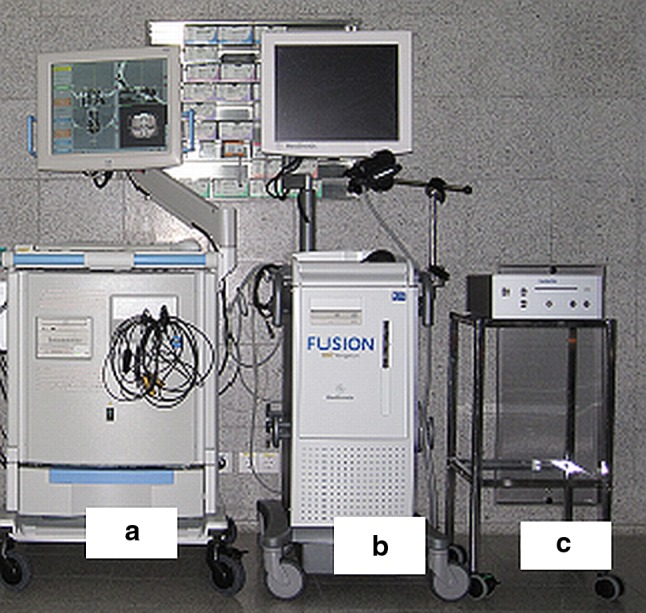
Picture shows three navigation systems from Instatrak 3500 plus, Fusion and Fiagon. It shows a comparison in size between the three systems. Comparison between three electromagnetic navigation systems is seen above-huge body (a, b) as opposed to lighter and compact system (c). System a is Instatrak 3500 plus from GE (USA), system (b) is Fusion from Meditronics (Germany), and system (c) is Fiagon (Germany)
Conclusion
Introducing electromagnetic navigation system to anterior skull base surgeries and ESS, particularly to endoscopic endonasal surgeries has revolutionized and moved the field forward. It provides an opportunity to localize the surgical trajectory and monitor it on a continuous basis. Navigation system has enhanced the precision by which a surgeon can operate as it provides accuracy up to 2 mm or better. Approaching difficult and non-accessible regions of the skull base have been made safer and easier through the use of navigation system as it provides better delineation of anatomical landmarks. Using navigation system requires good amount of training and expertise on the part of the surgeon. Navigation system is an adjunctive to the surgical skills of a surgeon while performing surgery but not a substitute. The surgeon still needs to have good knowledge about the anatomy of the surgical field. There is scope for further development of the field of Otorhinolaryngology and head and neck surgery by integrating newer techniques like robotic assisted sinus and skull base surgery with navigation system.
Acknowledgments
The authors would like to thank Dr. Andrea Rose from Fiagon, Germany, Dr. Köle W (Associate Professor, Department of Otorhinolaryngology and Head and Neck Surgery), Mr. Gerstenberger Claus (biomedical engineer) and Mr. Michael Amschl (operating theatre in charge) from University Klinikum, Graz for their help and support in writing this paper.
Conflicts of interest
The authors declare that they have no conflict of interest.
References
- 1.Al-Swiahb JN, Al Dousary SH. Computer-aided endoscopic sinus surgery: a retrospective comparative study. Ann Saudi Med. 2010;30(2):149–152. doi: 10.4103/0256-4947.60522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sadoughi B, Brown SM, Nachlas NE, Fried MP (2010) Image-guided surgery. http://emedicine.medscape.com/article/875524. Accessed 20 Mar 2011
- 3.Tabaee A, Hsu AK, Shrime MG, Rickert S, Close LG. Quality of life and complications following image-guided endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2006;135(1):76–80. doi: 10.1016/j.otohns.2006.02.038. [DOI] [PubMed] [Google Scholar]
- 4.Javer AR, Genoway KA. Patient quality of life improvements with and without computer assistance in sinus surgery: outcomes study. J Otolaryngol. 2006;35(6):373–379. doi: 10.2310/7070.2006.0083. [DOI] [PubMed] [Google Scholar]
- 5.Guiot G, Bouche J, Hertzog E, Vourc’h G, Hardy J. Hypophysectomy by trans-sphenoidal route. Ann Radiol (Paris) 1963;6:187–192. [PubMed] [Google Scholar]
- 6.Ceylan S, Koc K, Anik I. Extended endoscopic approaches for midline skull-base lesions. Neurosurg Rev. 2009;32(3):309–319. doi: 10.1007/s10143-009-0201-9. [DOI] [PubMed] [Google Scholar]
- 7.Ahn JY, Jung JY, Kim J, Lee KS, Kim SH. How to overcome the limitations to determine the resection margin of pituitary tumours with low-field intra-operative MRI during trans-sphenoidal surgery: usefulness of Gadolinium-soaked cotton Pledgets. Acta Neurochir (Wien) 2008;150:763–771. doi: 10.1007/s00701-008-1505-1. [DOI] [PubMed] [Google Scholar]
- 8.Al-Mefty O, Pravdenkova S, Gragnaniello C. A technical note on endonasal combined microscopic endoscopic with free head navigation technique of removal of pituitary adenomas. Neurosurg Rev. 2010;33(2):243–249. doi: 10.1007/s10143-010-0241-1. [DOI] [PubMed] [Google Scholar]
- 9.Tabaee A, Anand VK, Fraser JF, Brown SM, Singh A, Schwartz TH. Three-dimensional endoscopic pituitary surgery. Neurosurgery. 2009;64(5):288–295. doi: 10.1227/01.NEU.0000338069.51023.3C. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz TH, Stieg PE, Anand VK. Endoscopic transsphenoidal pituitary surgery with intraoperative magnetic resonance imaging. Neurosurgery. 2006;58(1 Suppl):44–51. doi: 10.1227/01.neu.0000193927.49862.b6. [DOI] [PubMed] [Google Scholar]
- 11.Neubauer A, Wolfsberger S, Forster M, Mroz L, Wegenkittl R, Bühler K. Advanced virtual endoscopic pituitary surgery. IEEE Trans Vis Comput Graph. 2005;11(5):497–507. doi: 10.1109/TVCG.2005.70. [DOI] [PubMed] [Google Scholar]
- 12.Mosges R, Schlondorff G. A new imaging method for intraoperative therapy control in skull-base surgery. Neurosurg Rev. 1988;11(3–4):245–247. doi: 10.1007/BF01741417. [DOI] [PubMed] [Google Scholar]
- 13.Tabaee A, Kacker A, Kassenoff TL, Anand V. Outcome of computer-assisted sinus surgery: a 5-year study. Am J Rhinol. 2003;17(5):291–297. [PubMed] [Google Scholar]
- 14.Strauss G, Koulechov K, Röttger S, Bahner J, Trantakis C, Hofer M, Korb W, Burgert O, Meixensberger J, Manzey D, Dietz A, Lüth T. Evaluation of a navigation system for ENT with surgical efficiency criteria. Laryngoscope. 2006;116(4):564–572. doi: 10.1097/01.MLG.0000202091.34295.05. [DOI] [PubMed] [Google Scholar]
- 15.Lasio G, Ferroli P, Felisati G, Broggi G. Image-guided endoscopic transnasal removal of recurrent pituitary adenomas. Neurosurgery. 2002;51(1):132–137. doi: 10.1097/00006123-200207000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Olson G, Citardi MJ. Image-guided functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2000;123(3):188–194. doi: 10.1067/mhn.2000.107453. [DOI] [PubMed] [Google Scholar]
- 17.Hanna EY, Holsinger C, DeMonte F, Kupferman M. Robotic endoscopic surgery of the skull base. Arch Otolaryngol Head Neck Surg. 2007;133(12):1209–1214. doi: 10.1001/archotol.133.12.1209. [DOI] [PubMed] [Google Scholar]
- 18.O’Malley BW, Jr, Weinstein GS. Robotic skull base surgery. Arch Otolaryngol Head Neck Surg. 2007;133(12):1215–1219. doi: 10.1001/archotol.133.12.1215. [DOI] [PubMed] [Google Scholar]
- 19.Nathan CO, Chakradeo V, Malhotra K, D’Agostino H, Patwardha R. The voice-controlled robotic assist scope holder AESOP for the endoscopic approach to the Sella. Skull Base. 2006;16(3):123–131. doi: 10.1055/s-2006-939679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caversaccio M, Langlotz F, Nolte L, Hausler R. Impact of a self-developed planning and self constructed navigation system on skull base surgery: 10 years experience. Acta Otolaryngol. 2007;127:403–407. doi: 10.1080/00016480601002104. [DOI] [PubMed] [Google Scholar]