Abstract
Three of the most consistently reported and powerful predictors of depression are a recent major life event, a positive family history for depression, and a personal history of past depressive episodes. Little research, however, has evaluated the inter-relations among these predictors in depressed samples. Such information is descriptively valuable and potentially etiologically informative. In the present article we summarize the existing literature and test four predictions in a sample of 62 clinically depressed individuals: (1) participants who experienced a major life event prior to onset would be less likely than participants who did not experience a major life event to have a positive family history for depression; (2) participants with a recent major life event would have fewer lifetime episodes of depression than would participants without; (3) participants with a positive family history for depression would have more lifetime episodes of depression than would participants with a negative family history for depression; and (4) we would obtain a 3-way interaction in which participants with a positive family history and without a major life event would have the most lifetime episodes, whereas participants with a negative family history and a major life event would have the fewest lifetime episodes. The first three predictions were confirmed, and the fourth prediction partially confirmed. These novel findings begin to elucidate the complex relations among these three prominent risk factors for depression, and point to avenues of research that may help illuminate the origins of depressive episodes.
Keywords: Family History, Major Depressive Disorder, Stressful Life Events, Vulnerability, Recurrence, Major Depressive Disorder
Life Stress and Family History for Depression: The Moderating Role of Past Depressive Episodes
Three of the most consistent and powerful predictors of depression are a recent major life event, a positive family history for depression, and a personal history of depressive episodes. Specifically, people with a recent major life event are 2.5 – 12 times more likely to develop an episode of depression (Kendler, et al., 1995; Shrout et al, 1989). Similarly, people with a first-degree family member who has experienced depression are 2.8 – 10 times more likely to develop depression (Goodwin & Jamison, 2007; Wallace et al., 2002). Finally, approximately 40–60% of people suffering a first lifetime episode of depression will incur another, with risk rising further for those with more prior episodes (American Psychiatric Association, 1994; Monroe & Harkness, 2011).
Although these three risk indicators are widely recognized to be strongly associated with depression, little is known about how they are related to one another; indeed, no study has investigated all three factors in a well-characterized sample of depressed individuals. Following a brief review of prior work on this topic, we evaluate four predictions within a sample of depressed individuals regarding associations among pre-onset major life events, family history for depression, and personal history of depression.
Family History of Depression and Major Life Stress
Early work by Strecker (1922) suggested that manic-depressive patients with a history of recent life stress had fewer family members with a history of mental illness. The working premise for these observations was that “the more defective the family stock, the less likelihood there is of finding serious extraneous factors in the histories of mental patients” (p. 530). Other researchers added substance to these early observations by focusing specifically on major depression. For instance, Pollitt (1972) reported that, within a depressed sample, there was an inverse association between familial rates of depression and severe psychological stress.
Other research, however, has not uniformly confirmed these predictions. For example, Perris et al. (1982) hypothesized that patients without a family history of depression would be “less vulnerable from a genetic point of view” and, consequently, that such patients “would require more, or more severe, events to precipitate depression than the more vulnerable” patients with a family history of the disorder (p. 243). However, these investigators found no differences between patients who were positive and negative for family history with respect to life events three months prior to onset of the depression. Similarly, McGuffin et al. (1988) were unable to confirm the predicted “inverse association between the presence of familial loading and reactivity to stress” (p. 775; see also Behar et al., 1981; Thomson & Hendrie, 1972).
There are several explanations for these discrepancies, including differences in research designs, samples, and methods. Of particular concern is the adequacy of previous practices for assessing life stress (Monroe & Reid, 2008). Equally important and previously unrecognized, prior investigations have not taken into account the depressed person’s history of depressive episodes. Specifically, prior history of depression may be essential to consider for understanding of the associations between recent life events and family history for depression.
Personal History of Depression, Family History of Depression, and Major Life Stress
Personal history of past depressive episodes has consistently been associated with family history of depression (e.g., see Sullivan et al., 2000). For instance, Bland et al. (1986) examined first lifetime admissions of depression over a 12- to 18-year follow-up period and compared morbidity risk for depression in relatives for the depressed patients who subsequently did or did not have a recurrence. The morbidity risk for relatives of individuals who had a single lifetime episode of depression was significantly lower (5.4%) than it was for relatives of individuals who experienced recurrences (12.65%). Thus, a personal history of depression should be associated with a positive family history of depression.
In contrast, the presence of major stress prior to onset of depression has been found consistently to be associated with less personal history of depression (Post, 1992), likely because major life events precede onset of depressive episodes early in the life course, and are less common prior to recurrences later in the life course. Such findings are often ascribed to premise that depressed persons become increasingly sensitized (or ‘kindled’) to stress, so that progressively lower levels of stress become capable of triggering recurrences (Monroe & Harkness, 2005). Consequently, a greater personal history of depression should be associated with a lower likelihood of experiencing a major life event prior to onset. Indeed, a large body of research has provided evidence for this effect (e.g., Slavich et al., 2011; for a review, see Stroud et al., 2008).
What is unknown, and has not yet been evaluated, is how these three major risk factors operate collectively. As indicated, there is good evidence for bivariate associations among the three factors, yet we do not know how such associations are altered when all three are considered simultaneously. Such information could resolve inconsistencies in the literature. Finally, such information could advance theory and research on the causes and possible subtypes of major depression. Along these lines, we propose that the association between pre-onset major life stress and family history of depression is moderated by personal history of depression.
The Presen Study
In the present study we evaluated the relations between pre-onset major life events, family history for depression, and personal history of depression in a sample of 62 adults diagnosed with major depression. Based upon the literatures summarized above, we generated four predictions. First, participants who had a major life event prior to onset would be less likely to have a positive family history for depression. Second, participants with a pre-onset major life event would report fewer lifetime episodes of depression (as previously demonstrated for a subset of the present sample; Monroe et al., 2007). Third, participants with a positive family history for depression would report more lifetime episodes of depression.
Finally, given the lack of existing information, predictions for the key three-way interaction of all three risk factors are more difficult to generate with confidence. Nonetheless, based on stress sensitization theory and prior research, we predicted that the relation between a major life event and family history for depression would be moderated by personal history of depression. Specifically, we hypothesized that individuals with a positive family history for depression and without a recent major life event would have the greatest number of past depressive episodes, whereas individuals with a negative family history and a pre-onset major life event would have the fewest.
Method
Participants and Procedure
Participants were 62 adults (46 female) between the ages of 18 and 58 (M = 35.22, SD = 10.18). These individuals, all diagnosed with Major Depressive Disorder (MDD), were drawn from projects investigating the role of cognition in psychopathology (see Gotlib et al., 2004) and life stress in depression (see Monroe et al., 2007; Muscatell et al., 2009; Slavich et al., 2009). The present study included all participants with complete data on recent life stress, family history for depression, and personal history of depression. Individuals were recruited through community advertisements and flyers, and through referrals from two outpatient psychiatry clinics at Stanford University. The majority of participants were self-referred from the advertisements, and approximately half (53%) were receiving some form of treatment.
Participants initially were screened by telephone to recruit those with current depression, and a relatively recent onset (98% of participants in the original sample had an onset within 2½ years); if the participant had experienced prior depression, a minimum interval of six months without MDD was required prior to the index episode. Individuals potentially eligible for the study were invited to complete a diagnostic interview and a battery of self-report questionnaires in the Department of Psychology at Stanford University. Participants who met full criteria for study inclusion were requested to return approximately one week later to complete additional measures. Following these two initial sessions, participants were invited for a third session to complete the life stress interview. After the protocol was fully explained, participants provided written informed consent and were paid $25 per hour. The research was approved by the University of Oregon and Stanford University Institutional Review Boards.
All participants were interviewed with the Structured Clinical Interview for DSM-IV (SCID; First et al., 1996) and met criteria for current MDD according to the Diagnostic and Statistical Manual of Mental Disorders (4th edition; DSM-IV; APA, 1994). These individuals were screened to exclude current comorbid panic disorder and social phobia, as well lifetime history of mania, hypomania, or psychotic symptoms. Participants were also excluded if they had a recent history (past 6 months) of alcohol or psychoactive substance abuse or dependence, or a history of brain injury or mental retardation. Interviewers were advanced psychology graduate students and post-baccalaureate research assistants. To assess diagnostic inter-rater reliability for the overall project, an independent trained rater who was unaware of group membership evaluated 15 randomly selected audiotapes of SCID interviews. These interviews were drawn from individuals who did and did not meet study criteria, and they included people who met criteria for depression, social phobia, panic disorder, and those who did not meet diagnostic criteria. In all 15 cases, diagnostic decisions made by the independent rater matched those made by the original interviewer, κ = 1.00.
Measures
Lifetime History of Depression
Lifetime history of MDD for each participant was assessed routinely as part of the SCID. Interviewers carefully probed each prior depressive experience to determine if it met criteria for MDD. The frequency of lifetime depressive episodes (including the index episode) ranged from 1 to “too many to count.” The majority of participants had five or fewer lifetime episodes (n = 36; 58.1%), and there were sufficient frequencies of participants within each of these five categories for more detailed analysis. Beyond five lifetime episodes, however, the frequency of participants per specific number of past depressive episodes decreased. Consequently, to provide a more uniform index of depression history and approximately equal numbers of participants per grouping, individuals reporting more than five lifetime episodes were collapsed into three lifetime history categories (6–10 episodes, 11–36 episodes, > 36 episodes/“too many to count;” see Monroe et al., 2007).
Family History for Depression
Detailed information regarding participants’ family history of depression was collected as part of a comprehensive medical history questionnaire that participants completed following the SCID. Participants were first asked if any immediate family members had experienced major depression. If they answered “yes,” they identified who (mother, father, sibling, child), and then reported whether the individual was formally diagnosed (yes, no), hospitalized, and treated with medication. Participants were judged to be positive for a family history of depression if they reported that a family member had suffered from depression.
Life Stress Assessment
The Life Events and Difficulties Schedule (LEDS; Brown & Harris, 1978) was used to assess and operationalize life stress. The LEDS system employs a semi-structured interview that systematically probes for stressors across ten domains of functioning (e.g., health, work, education, relationships, etc.). Interviewers use numerous follow-up questions to stimulate recall of past experiences. After completing the LEDS interview at Stanford University with the participant, the interviewer presented detailed life stress information via teleconferencing to raters at the University of Oregon. The Oregon team performed all ratings after discussion and consensus agreement, and was blind to relevant dependent measures (e.g., timing of depression onset, emotional responses to the event, personal and family history of depression). For all of these operations, the LEDS manuals provided anchoring examples and assisted with standardization (e.g., the 520-page manual contains thousands of case vignettes to assist in defining events and assigning threat ratings). On average, the interviews and rating sessions each required approximately two hours to complete.
Previous research with the LEDS has established severe acute life events as especially strong predictors of depression onset (Brown & Harris, 1989; Hammen, 2005; Harkness et al., 2010; Mazure, 1998; Monroe et al., 2009). These events are characterized by a high degree of contextual threat and unpleasantness, a high likelihood of prolonged consequences, and include events such as the termination of a core relationship, a broken engagement, and a very serious fight with a spouse. Non-severe events are characterized by lower threat, fewer prolonged consequences, and may be events that primarily impact family or close friends; they include events such as an argument with a family member, non-serious illnesses, undesirable (but not drastic) changes at work. Within the LEDS system, all events are rated based on extensive information about the circumstances surrounding the event and on the particular individual’s biographic details (i.e., “contextual” ratings; see Brown & Harris, 1978, 1989). Presence or absence of a severe event occurring within 12 weeks prior to onset of MDD represents a standard procedure for operationalizing life stress within the LEDS system (Brown & Harris, 1978, 1989).
The LEDS has established psychometric validity and is widely regarded as a state-of-the-art instrument for assessing life stress (Brown, 1989; Hammen, 2005). Reliability for the present project for pair-wise comparisons ranged from .72 to .79 (M = .76; Cohen’s kappa, corrected for differences in the number of raters per event; Uebersax, 1982). Previous research indicates high reliability for assessing severe events for up to ten years retrospectively (Brown, 1989; Neilson et al.,1989).
Data Analyses
Chi-square analyses were conducted for the cross-tabulation of pre-onset severe events with family history of depression. Hierarchical regression analyses were performed to predict lifetime depression history, with the presence or absence of a severe life event entered first and the presence or absence of a family history for depression entered second. Finally, to test the interaction of recent major events with family history of depression, the cross-product interaction term was entered into the equation last (Cohen & Cohen, 1983). All tests were two-tailed except as noted.
Results
The first prediction was that participants who with a major life event prior to onset would be less likely to report a positive family history for depression. It was strongly supported. Whereas only 10.5% (4 of 38) of the positive family history group had a pre-onset major life event, 41.7% (10 of 24) of the negative family history group had such an event, χ2(1, N = 62) = 8.16, p ≤ .004. The presence of a pre-onset major life event was approximately four-fold greater in the absence of a family history for depression.
The second and third predictions evaluated pre-onset major life events and family history for depression as main effects for lifetime history of depression. Consistent with our prediction and previous report employing a different subset of the present sample (Monroe et al., 2007), pre-onset major life events were associated with fewer lifetime depressive episodes, F(1, 60) = 6.12, p < .02. Separate t-test comparisons substantiated that participants with a pre-onset major event had significantly fewer lifetime episodes of depression (M = 2.93, SD = 2.46) than participants without (M = 4.83, SD = 2.55), t(60) = 2.47, p < .02. Moreover, adding family history in the second step of the regression analysis yielded a significant increment in prediction, Fchange (1,59) = 7.78, p < .01. As hypothesized, family history for depression predicted a greater history of depression. Separate t-test comparisons substantiated that positive family history participants had more lifetime episodes of depression (M = 5.26, SD = 2.41) than their negative family history counterparts (M = 3.04, SD = 2.44), t(60) = 3.52, p ≤ .001.
Finally, we tested the moderating role of personal history of depression with regard family history for depression and pre-onset life stress. As predicted, family history and pre-onset major life stress interacted significantly to predict lifetime episodes, , Fchange (1,58) = 2.98, p < .05 (one-tailed based upon the a priori directional prediction). Based on a priori contrast predictions, follow-up t-tests were conducted to more precisely specify the effects. As predicted for the positive family history group, participants without a pre-onset major life event had significantly more lifetime depressive episodes compared to participants with such an event (M = 5.56, SD = 2.29 vs. M = 2.75, SD = 2.22, respectively), t(36) = 2.33, p < .03. In contrast and contrary to predictions, the negative family history participants with and without pre-onset major life stress did not differ with respect to lifetime MDD (M = 3.00, SD = 2.67 vs. M = 3.07, SD = 2.37), t(22) = 0.07, p > .90. Overall as illustrated in Figure 1, depressed persons with a positive family history for depression and without a pre-onset major life event evidenced the greatest history of MDD compared to all three other groups.
Figure 1.
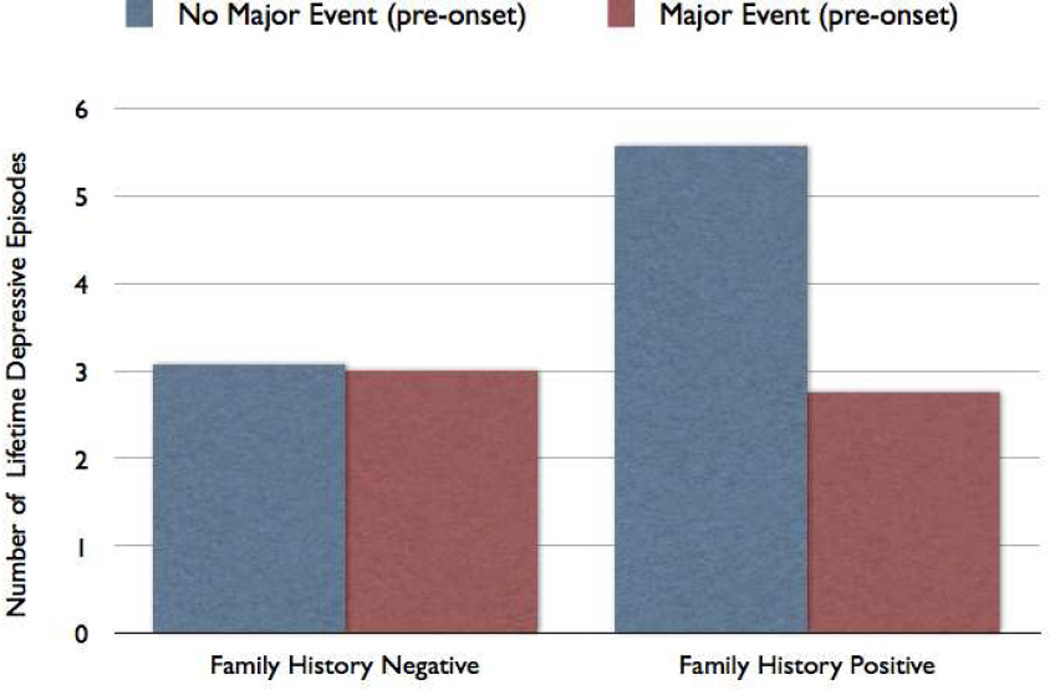
Interaction between the presence vs. absence of a major life event in the 12 weeks prior to onset of depression by family history for depression in relation to personal lifetime history of depressive episodes
Discussion
We found clear and strong evidence for a reciprocal relation between the presence of a pre-onset major life event and a positive family history for depression. Participants with a major life event prior to onset had an almost four-fold greater likelihood of not having a family history for depression. This suggests that major life stress plays a different role with regard to depression onset for the two family history groupings. Indeed, the relatively low rate of pre-onset major life events for the positive family history group approximates population base rates, suggesting that major events are not a critical trigger of depression for family history positive individuals. In contrast, the comparatively high rate of pre-onset major life stress for participants without a family history clearly exceeds population base rates (Mazure, 1998; Monroe & Simons, 1991), and is consistent with the formulation that these major events play an important causal role in the development of depression for individuals without a family history for depression.
As proposed, however, the patterning of family history of depression with respect to pre-onset major life events alone does not provide a complete picture of the role that life stress plays in depression for individuals with and without a family history of the disorder. This is because participants differ with respect to lifetime history of depression and its recurrences, which also is robustly associated with risk for new episodes. To gain a clearer understanding of this multifaceted issue, data are required for all three risk factors. We addressed this issue by first evaluating the bivariate associations individually. These analyses revealed that both family history for depression and pre-onset major life events were related to lifetime history of depression, yet each in an opposite manner.
Most important and novel, however, are the findings regarding how life stress plays a more nuanced role in relation to family history for depression as a function of the lifetime history of depression. Along these lines, we found that the association between pre-onset major life events and family history for depression was moderated by personal history of the disorder. Particularly noteworthy is that depressed persons with a positive family history, yet without major stress pre-onset, exhibited the greatest lifetime history of MDD (see Figure 1). Being especially vulnerable to depression, these individuals may require little provocation to initiate another episode. Viewed in this way, major events may be unrelated to recurrence of depression for this family history positive group. A key question concerns whether this group has become sensitized or kindled with respect to the effects of stress over repeated episodes, or whether this group represents a distinct recurrent subtype for which stress is not an important causal ingredient (Monroe & Harkness, 2005; Post, 1992). Future work focusing on non-severe life events and chronic life stress may be of value for determining whether this family history positive group without a pre-onset severe life event is sensitized to other forms of stress, or, alternatively, whether stress is not causally relevant for onset with these types of people.
Individuals with both a positive family history and a pre-onset major life event had comparatively fewer lifetime episodes of depression than did those with a positive family history and no pre-onset major life event. This suggests two interesting possibilities. First, in keeping with the ‘kindling’ hypothesis and stress sensitization, there may be a progression of increasing susceptibility to stress with successive episodes (Post, 1992). However, these positive family history participants with recent major life stress may not as yet be sufficiently sensitized to become depressed with the relative absence of major stress (i.e., they still require major stress to trigger an episode; Monroe & Harkness, 2005). With more recurrences, though, they may transition to be more like their no major stress family history counterparts. Second, it is rarely recognized that not all individuals who have a positive family history for depression necessarily acquire the familial or genetic diathesis for the disorder. Family history is a useful but inexact indicator of susceptibility; some individuals with a family history for depression will be vulnerable, but some inevitably will not. (One need only contemplate recent molecular genetic studies to recognize that, for instance, having a positive family history may or may not confer the underlying risk allele.) Viewed in this light, and recognizing that lifetime history of MDD for this group is quite close to the lifetime history of depressive episode for the two negative family history groups, an intriguing explanation emerges. Perhaps these family history positive individuals are more akin genetically and psychobiologically to the negative family history group, and require major acute stress to precipitate recurrences.
In contrast and counter to our second a priori prediction for the three-way interaction, the negative family history group with pre-onset major life stress did not evidence the fewest number of lifetime episodes of depression. In fact, these individuals were essentially indistinguishable with respect to the past depressive episodes from their negative family history counterparts who had not experienced a major life event (and, as just noted, from the positive family history group with pre-onset major life stress; see Figure 1). Based on these findings, major stressors often are required to initiate recurrences for people without a family history of the disorder, irrespective of personal history of depression. Put differently, the vulnerability to depression that negative family history individuals possess may remain relatively constant over repeated episodes of depression, with major life stress often required to trigger each new recurrence. Overall, this interpretation suggests that kindling processes are more pertinent for individuals with a positive family history of depression (cf. Kendler et al., 2001).
These findings help explain inconsistencies in prior research on the relation between major life stress and family history of depression. As noted, although several previous studies report an inverse association between major stress and family history for depression, other studies have not replicated the association. It is likely that studies have varied in terms of the prevalence of past depressive episodes in their samples. Our results suggest that research including participants with a wide range of lifetime episodes is necessary to detect the inverse association between life stress and family history for depression.
Strengths of the present study include a clinically depressed sample informative for a wide range of depression histories, use of the interview-based LEDS system to assess life stress, and most importantly, the inclusion of measures for all three risk factors within the same sample. Although our family history measure was similar to many used in other studies, it likely provides an underestimate compared to state-of-the-art approaches (e.g., Klein et al., 2005). Yet the relative insensitivity of our measure was sufficient to establish a strong effect, and was unlikely to be biased in ways that could produce spurious results. Because family history is not synonymous with genetic liability, future research could also provide additional insights by using genetically informed research designs or by taking advantage of advances in molecular genetic techniques (e.g., Caspi et al., 2003; Kendler et al., 2001).
In summary, the present report is the first to find that the association between major life stress and family history for depression is moderated by prior history of depressive episodes. These results underscore the importance of taking into account all three factors in the context of research on depression. They also point to future research agendas that may shed additional light on how these risk indicators, individually and collectively, can be informative for understanding the nature of depression and its recurrences.
Table 1.
Demographic and Clinical Variables for the Family History Positive versus Family History Negative Groups, and for Severe versus No Severe Pre-Onset Life Event Groups1
| Positive Family History of Depression |
Negative Family History of Depression |
Pre-Onset Severe Life Event |
No Pre-Onset Severe Life Event |
|
|---|---|---|---|---|
| Age (yrs)2 | 37.51 | 31.00 | 35.62 | 35.10 |
| Gender (% Female) | 68.4 | 83.3 | 78.6 | 72.9 |
| Marital Status (% Married or cohabitating) | 35.1 | 37.5 | 50.0 | 31.9 |
| Lifetime MDD Episodes3 | 5.26 | 3.04 | 2.93 | 4.83 |
| Age of first MDD | 18.65 | 19.63 | 20.82 | 18.43 |
| Current MDD Severity4 | 6.58 | 6.26 | 6.71 | 6.38 |
| Current MDD Length (mos) | 8.88 | 9.53 | 7.89 | 9.49 |
| N | 38 | 24 | 14 | 48 |
Numbers may vary across analyses due to missing values.
Positive Family History versus Negative Family History, t (52)=2.54, p < .03.
See text for statistical comparisons between groups.
Number of codable SCID symptoms.
Acknowledgements
We thank Lauren Anas, Erica Aronson, Kathryn Dingman, and Danielle Keenan-Miller for conducting life stress interviews, and Faith Brozovich for assisting with data management. For participating in stress ratings, we thank Keely Muscatell, Leandro Torres, Julien Guillaumot, Corrie Doyle, and Tiffany Thornton. This work was supported in part by National Institute of Mental Health Research Grants MH60802 (Scott M. Monroe) and MH59259 (Ian H. Gotlib), and by a Society in Science: Branco Weiss Fellowship (George M. Slavich).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
In consultation with Ian Gotlib and George Slavich, Scott Monroe designed the study, performed the literature review, conducted the statistical analyses, and wrote the initial draft of the article. Ian Gotlib and George Slavich oversaw data acquisition and management, and provided extensive editorial feedback on manuscript drafts. All authors contributed to and have approved the final manuscript.
Contributor Information
Scott M. Monroe, Department of Psychology, University of Notre Dame
George M. Slavich, Cousins Center for Psychoneuroimmunology and Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles
Ian H. Gotlib, Department of Psychology, Stanford University
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, D.C.: American Psychiatric Association; 1994. [Google Scholar]
- Behar D, Winokur G, Van Valkenburg C, Lowry M, Lachenbruch PA. Clinical overlap among familial subtypes of unipolar depression. Neuropsychobiology. 1981;7:179–184. doi: 10.1159/000117848. [DOI] [PubMed] [Google Scholar]
- Brown GW. Life events and measurement. In: Brown GW, Harris TO, editors. Life events and illness. London: The Guilford Press; 1989. pp. 3–45. [Google Scholar]
- Brown GW, Harris TO. Social origins of depression: A study of psychiatric disorder in women. New York: The Free Press; 1978. [Google Scholar]
- Brown GW, Harris TO. Depression. In: Brown GW, Harris TO, editors. Life events and illness. London: The Guilford Press; 1989. pp. 49–93. [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multivariate regression/correlation analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RI, Gibbon M, Williams JB. User’s Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version. New York State Psychiatric Institute. New York, NY: Biometrics Research Department; 1996. [Google Scholar]
- Gotlib IH, Kasch KL, Traill S, Joormann J, Arnow BA, Johnson SL. Coherence and specificity of information-processing biases in depression and social phobia. Journal of Abnormal Psychology. 2004;113:386–398. doi: 10.1037/0021-843X.113.3.386. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Harkness KL, Tabari N, Monroe SM, Slavich GM, Gotlib IH, Bagby RM. Sex differences in life events prior to onset of major depressive disorder: The moderating effect of age. Journal of Abnormal Psychology. 2010;119:791–803. doi: 10.1037/a0020629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Kessler RC, Walters EE, MacLean CJ, Sham PC, Neale MC, et al. Stressful life events, genetic liability and onset of an episode of major depression in women. American Journal of Psychiatry. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Genetic risk, number of previous depressive episodes, and stressful life events in predicting onset of major depression. American Journal of Psychiatry. 2001;158:582–586. doi: 10.1176/appi.ajp.158.4.582. [DOI] [PubMed] [Google Scholar]
- Klein D, Dougherty L, Olino T. Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:412–432. doi: 10.1207/s15374424jccp3403_3. [DOI] [PubMed] [Google Scholar]
- McGuffin P, Katz R, Bebbington P. The Camberwell Collaborative Depression Study III. Depression and adversity in the relatives of depressed probands. British Journal of Psychiatry. 1988;153:775–782. doi: 10.1192/bjp.152.6.775. [DOI] [PubMed] [Google Scholar]
- Mazure CM. Life stressors as risk factors in depression. Clinical Psychology: Science and Practice. 1998;5:291–313. [Google Scholar]
- Monroe SM, Harkness KL. Life stress, the ‘Kindling’ Hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological Review. 2005;112:417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Recurrence in major depression: A conceptual analysis. Psychological Review. 2011;118:655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Reid MW. Gene-environment interactions in depression research: Genetic polymorphisms and life-stress polyprocedures. Psychological Science. 2008;19:947–956. doi: 10.1111/j.1467-9280.2008.02181.x. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Slavich GM, Georgiades K. The social environment and life stress in depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. Second Edition. New York: The Guilford Press; 2009. pp. 340–360. [Google Scholar]
- Monroe SM, Slavich GM, Torres L, Gotlib IH. Major life events and major chronic difficulties are differentially associated with history of major depressive episodes. Journal of Abnormal Psychology. 2007;116:116–124. doi: 10.1037/0021-843X.116.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Muscatell KA, Slavich GM, Monroe SM, Gotlib IH. Stressful life events, chronic difficulties, and the symptoms of clinical depression. Journal of Nervous and Mental Disease. 2009;197:154–160. doi: 10.1097/NMD.0b013e318199f77b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neilson E, Brown GW, Marmot M. Myocardial infarction. In: Brown GW, Harris TO, editors. Life events and illness. London: The Guilford Press; 1989. pp. 313–342. [Google Scholar]
- Pollitt J. Relationship between genetic and precipitating factors in depressive illness. British Journal of Psychiatry. 1972;121:67–70. doi: 10.1192/bjp.121.1.67. [DOI] [PubMed] [Google Scholar]
- Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. American Journal of Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Link BG, Dohrenwend BP, Skodol AE, Stueve A, Mirotznik J. Characterizing life events as risk factors for depression: The role of fateful loss events. Journal of Abnormal Psychology. 1989;98:460–467. doi: 10.1037//0021-843x.98.4.460. [DOI] [PubMed] [Google Scholar]
- Slavich GM, Monroe SM, Gotlib IH. Early parental loss and depression history: Associations with recent life stress in major depressive disorder. Journal of Psychiatric Research. 2011;45:1146–1152. doi: 10.1016/j.jpsychires.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Thornton T, Torres LD, Monroe SM, Gotlib IH. Targeted rejection predicts hastened onset of major depression. Journal of Social and Clinical Psychology. 2009;28:223–243. doi: 10.1521/jscp.2009.28.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud CB, Davila J, Moyer A. The relationship between stress and depression in first onsets versus recurrences: A meta-analytic review. Journal of Abnormal Psychology. 2008;117:206–213. doi: 10.1037/0021-843X.117.1.206. [DOI] [PubMed] [Google Scholar]
- Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry. 2000;157:1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- Thomson KC, Hendrie HC. Environmental stress in primary depressive illness. Archives of General Psychiatry. 1972;26:130–132. doi: 10.1001/archpsyc.1972.01750200034007. [DOI] [PubMed] [Google Scholar]
- Uebersax JS. A generalized kappa coefficient. Educational and Psychological Measurement. 1982;42:181–183. [Google Scholar]
- Wallace J, Schneider T, McGuffin P. Genetics of depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. New York: The Guilford Press; 2002. pp. 169–191. [Google Scholar]


