Abstract
The objective was to compare the immediate effects of local cryotherapy (LC) and passive cross-body stretch on the extensibility of the posterior shoulder muscle in individuals with posterior shoulder tightness. Eighty-seven healthy subjects with a between-shoulder difference in internal rotation (IR) range of motion (ROM) greater than 10° were randomly divided into three groups: LC group, stretching group, and control group (n = 29 in each group). Subjects in the LC group received LC on infraspinatus and posterior deltoid muscles and subjects in the stretching group performed passive cross-body stretch. Stretch sensation was measured at the end range of passive IR and horizontal adduction (HA) using numerical rating scale, and the pressure pain threshold (PPT) at the infraspinatus and posterior deltoid muscles was measured using pressure algometry. Passive and active ROM of IR and HA of the glenohumeral joint were measured using an inclinometer. All measurements were performed at pre-intervention, post- intervention, and 10-min follow-up. Stretch sensation was significantly decreased and PPT was significantly increased in the LC and stretching groups at post-intervention, and these effects were maintained at 10-min follow-up, compared to the control group. Both the LC group and stretching group had a significantly greater increase in passive and active ROM of IR and HA, compared to the control group at post-intervention and 10-min follow-up. However, there were no significant differences in stretch sensation, PPT, or ROM of IR and HA between the LC group and stretching group. LC can be used to decrease the stretch sensation and increase PPT and ROM of IR and HA as much as a stretching exercise. LC could be an alternative method for increasing the restricted ROM of glenohumeral IR and HA for individuals with posterior shoulder tightness, especially for patients and sports players who have severe stretching discomfort.
Key Points.
Local cryotherapy (LC) decreased the uncomfortable stretch sensation, and increased the pressure pain threshold (PPT) of infraspinatus and posterior deltoid muscles in subjects with posterior shoulder tightness.
Decreased stretch sensation by LC without passive stretching could improve the passive and active ROM of internal rotation and horizontal adduction in subjects with posterior shoulder tightness, similar to cross-body stretch.
LC can be an alternative method to increase extensibility when individuals with posterior shoulder tightness have high stretch sensitivity and low PPT in the infraspinatus and posterior deltoid muscles.
Key Words: Cryotherapy, muscle stretching exercise, shoulder
Introduction
Posterior shoulder tightness is a common cause of shoulder impingement syndrome, labral lesions, and rotator cuff tears in clinical rehabilitation and sport activities (Ludewig and Cook, 2002; Tyler et al., 2000; Wilk et al., 2002; 2005). Posterior shoulder tightness is often assessed by measuring the range of motion (ROM) of glenohumeral internal rotation (IR) and horizontal adduction (HA) (Bach and Goldberg, 2006; McClure et al., 2007). A restricted ROM of IR and HA is caused by tightness of posterior muscles (i.e., infraspinatus and posterior deltoid) and the posterior capsule (Borsa et al., 2005; Poser and Casonato, 2008; Yang et al., 2012). Passive cross-body stretch is an effective method for stretching these areas (McClure et al., 2007).
Short-term (3- to 8- week) stretching program increases ROM by changing mechanical properties, such as increasing the length of stretched muscle, inducing elongating connective tissue, and increasing the number of sarcomeres in series (McNair et al., 2001; Taylor et al., 1995; Reid and McNair, 2004). However, although ROM increases after single stretching session, increased muscle length is transient and some studies have demonstrated that muscle stiffness (passive torque/ angle curve) do not change significantly (Law et al., 2009; Ben and Harvey, 2010; BjÃrklund et al., 2001). Increased muscle extensibility after stretching is due to sensory modification, rather than increased muscle length, an idea referred to as sensory theory (Nelson and Bandy, 2004; Weppler and Magnusson, 2010). Namely, stretching can increase the stretch tolerance at the terminal position of the stretch, resulting in increased muscle extensibility and ROM (Folpp et al., 2006; de Weijer et al., 2003; Weppler and Magnusson, 2010).
A previous study speculated that local cryotherapy (LC) may help endure the uncomfortable stretch sensation, felt at the final position of the stretch (Brodowicz et al., 1996). Stretching the hamstring with ice on it more effectively improved supine hamstring flexibility than both stretching alone and stretching with heat (Brodowicz et al., 1996). In addition, whole body cryotherapy effectively increases the active ROM of glenohumeral flexion, abduction, external rotation, and IR in patients with adhesive shoulder capsulitis (Ma et al., 2013).
To date, no studies have investigated the effects of LC on posterior shoulder muscles for the improvement of ROM of IR and HA, through modification of the stretch sensation at the end range of passive IR and HA. Thus, in this study, we investigated the effects of LC on the stretch sensation and on the ROM of glenohumeral IR and HA, comparing it to passive cross-body stretch and no stretching. We also investigated the lasting effects of LC and stretching (separately) at a 10- min follow-up assessment. We hypothesized that LC would decrease the uncomfortable stretch sensation, resulting in an increased ROM of IR and HA and have a lasting effect, similar to stretching.
Methods
Subjects
We recruited 87 subjects with posterior shoulder tightness selected from students of Yonsei University, Korea (Table 1). Using previously published immediately changes in posterior shoulder tightness (Moore et al., 2011), a power of 80% and an α level of 0.05 were assumed and the difference of the glenohumeral IR ROM should be at least 4.2° between the three groups, which required at least 25 subjects were needed. The inclusion criteria for selection of healthy subjects with posterior shoulder tightness was a difference in the passive ROM of the glenohumeral IR of over 10° between the right and left side (between-side difference; mean ± standard deviation [SD], 16.93 ± 10.81) (McClure et al., 2007). We excluded subjects who had present or previous shoulder pain, history of shoulder surgery, reduced sensation, Raynaud’s disease, previous cold allergies or who were unable to perform glenohumeral active IR and HA. Random-number generator function in Microsoft Excel program automatically and randomly matched 87 subjects to each group: the LC group (29 subjects), the stretching group (29 subjects), and the control group (29 subjects). Then subjects were provided the allocation information. Before the study, the principal investigator explained all procedures to the subjects in detail and gave subjects one week to make a decision on participating this study. All subjects signed an informed consent form, and this study was approved by the Yonsei University Wonju Institutional Review Board.
Table 1.
Comparison of subject characteristics. Data are expressed as means (± SD).
| Characteristics | Local cryotherapy group (n = 29) |
Stretching group (n = 29) |
Control group (n = 29) |
|---|---|---|---|
| Gender (male/female) | 19/10 | 20/9 | 18/11 |
| Age (years) | 23.45 (1.90) | 23.35 (2.08) | 23.35 (2.08) |
| Body mass (kg) | |||
| male | 77.50 (3.35) | 76.20 (8.36) | 75.80 (6.36) |
| female | 56.00 (7.35) | 54.80 (8.15) | 55.10 (8.42) |
| Height (m) | |||
| male | 1.79 (.05) | 1.79 (.07) | 1.79 (.06) |
| female | 1.68 (.07) | 1.67 (.06) | 1.66 (.07) |
Measurements procedures
Glenohumeral active and passive ROM of IR and HA, stretch sensation, and pressure pain threshold (PPT) were measured at pre-intervention, post-intervention (immediately after intervention), and 10-min follow-up (10 min after the post-intervention period) by a single tester who was blinded to the random group allocation.
Measurement of posterior shoulder tightness
Measurement of posterior shoulder tightness included active and passive IR and HA using a gravity inclinometer (Acuangle, Isomed, USA). Prior to ROM measurements, subjects were asked to perform three bilateral shoulder flexion exercises with hands clasped, holding at the end of range for 10 s as a warm-up (McClure et al., 2007). Shoulder flexion exercise was used as warm-up to minimize the extensibility effect on posterior structures and IR and HA, and warm-up exercise was able to ensure subject’s safety and to facilitate the consistency of data being tested (Kolber and Hanney, 2010). The subjects were positioned in the resting supine position. To measure active ROM of IR, a subject’s arm was placed in glenohumeral abduction at 90° on a therapeutic table and elbow flexed at 90° without glenohumeral IR or ER. A tester’s hand was placed on the anterior region of the subject’s glenohumeral joint and the other hand was used to place an inclinometer on the distal, posterior part of the forearm. Subjects were asked to perform glenohumeral IR until the tester felt an upward movement of the anterior region of the glenohumeral joint. The tester recorded the value in degrees. ROM for passive IR was measured in the same position and a tester performed passive IR until the tester felt an upward movement of the anterior region of the glenohumeral joint (McClure et al., 2007). The tester recorded the value in degrees. Active and passive IR measurements were repeated three times with 30 s of rest between each trial and the mean value was used for data analysis.
To measure the active glenohumeral HA ROM, subjects assumed a supine position with the glenohumeral joint at 90° of abduction and the elbow at 90° of flexion. A blinded tester grasped the scapular lateral border and applied force in the posterior direction to prevent scapular protraction and abduction movements. The other hand was used to place the inclinometer on the distal humerus, and 0° of HA ROM was obtained by placing the humerus perpendicularly to the examination table. Then subjects were asked to perform active glenohumeral HA as much as possible, until the tester felt scapular protraction; the tester recorded the active HA ROM value. ROM for passive HA was measured in the same position, and the tester performed passive HA until scapular protraction was felt (Laudner et al., 2006) and the value was recorded. The active and passive HA measurements were repeated three times with 30 s of rest between each trial and the mean value was used for data analysis. Intra-rater reliability was determined for a blinded tester on 29 shoulders with posterior shoulder tightness. The intraclass correlation coefficient (ICC, 3,1) was 0.98 with a 95% CI of 0.95-0.99 for IR and 0.97 with a 95% CI of 0.94-0.99 for HA.
Measurement of stretch sensation
Stretch sensation was measured to determine whether LC or stretching could modify stretch tolerance. An 11-point numerical rating scale was used to rate subjects’ perceptions of discomfort at the posterior aspect of the shoulder. All the subjects were asked to verbally report a number immediately on reaching at the terminal position of each passive IR and HA. “0” on the stretch sensation scale indicated “no discomfort” and “10” indicated “the worst possible discomfort and increased sensitivity”(Ben and Harvey, 2010). Subjects were given a pretest to familiarize 11-point stretch sensation scale. The pretest was performed with passive IR and HA to the opposite shoulder. For familiarization purposes, a tester would gradually increase the range of passive IR and HA to the end range and then the subjects verbally reported the level of discomfort at end range position of passive IR and HA. This procedure was more repeated twice. Stretch sensation measurements were repeated three times for passive IR and HA and the mean value was used for data analysis.
PPT Measurement
The PPT was measured to determine decreased sensitivity objectively (Castellote Caballero et al., 2013). To measure PPT, a pressure pain algometer (Wagner Instruments, Greenwich, USA) was used. A tester measured PPT by applying a calibrated mechanical algometer at a constant force rate of 1 kg·cm-2/s (Fuentes C et al., 2011). The PPT of the infraspinatus and posterior deltoid muscles were measured in the prone position. A folded towel and cushion were used to support the subject’s shoulder. A tester marked a landmark point of each muscle on the skin using a pen for a reliable PPT measurement at each time point. The landmarks represented the distal one-third of the infraspinatus and the midpoint of the deltoid (Jones et al., 2007). The tester applied perpendicular pressure to each muscle region using the algometer. The applied pressure was increased until the subject experienced a sensory conversion from pressure to pain. The pressure force recorded by the algometer was the minimal amount of pressure applied to evoke pain (Jones et al., 2007). The PPT measurement was repeated three times and the mean value was used for data analysis. Intra-rater reliability was determined for a blinded tester on 29 shoulders with posterior shoulder tightness. ICC (3,1) was 0.95 with a 95% CI of 0.93-0.97 for the infraspinatus and 0.97 with a 95% CI of 0.95-0.98 for the posterior deltoid.
Intervention (LC and Passive cross-body Stretch)
Interventions included LC on both the infraspinatus and posterior deltoid muscles for the LC group, and passive cross-body stretch for the stretching group. Subjects in the control group received neither treatment; they remained on the examination table for measurements at pre-, post-intervention, and 10-min follow-up.
Local cryotherapy
A cold flexible gel pack (28 × 11.5 cm; surface area, 322 cm2) was used as the LC in the present study. It was placed over the infraspinatus and posterior deltoid muscles. The middle of the ice bag was centered over the acromion region. Subjects removed their shirts to allow maximal contact with the ice pack. A shoulder strap was used to secure the pack. The subject was asked to lay on the treatment table in a resting supine position, and not stretch the infraspinatus or posterior deltoid muscles. When applying LC, subjects were asked to relax to prevent muscle activation and maintain the cold temperature. LC duration was 3 min, based on previous literature (Verducci, 2000).
Passive cross-body stretch
The stretching group performed a self cross-body stretch by passively pulling the humerus across the body into glenohumeral HA with the opposite arm (McClure et al., 2007). This stretch was performed six times, holding each stretch for 30 s in sitting position.
Statistical analysis
The Kolmogorov-Smirnov test confirmed a normal distribution of data (p > 0.05). Baseline (pre-intervention period) measurements were compared between groups using analysis of variance (ANOVA). To test whether there was a difference in intervention efficacy between the three groups and adjust the baseline difference between groups, two-factor analyses of covariance (ANCOVA) mixed models with the pre-intervention data as a covariate, and the two factors of group (LC group, stretching group, control group) and time (data at post-intervention and 10-min follow-up) were performed on each outcome. Bonferroni correction was applied for comparison between groups at each time point. Analysis was performed using SPSS 17.0.1 software (SPSS Inc., Chicago, IL, USA). The effect size (Cohen d) was calculated to provide clinical meaningfulness of the changes in ROM, stretch sensation, and PPT using Microsoft Excel. Effect sizes were interpreted according to Cohen’s guidelines; small (d = 0.20), medium (d = 0.50), or large (d = 0.80) (Cohen, 1988).
Results
Baseline variables (passive and active ROMs of both IR and HA, stretch sensations at end range of passive IR and HA, and PPTs for both infraspinatus and posterior deltoid muscle) in each group were significantly different (p > 0.05) except for age, height, and weight (Table 1). The covariate-adjusted means of the pre-intervention measurement allowed for comparison of post-intervention and 10-min follow-up, as if all three groups had the same pre-intervention scores. For passive and active ROM of both IR and HA, a significant group × time interaction (p < 0.05) was found (Table 2). At post- intervention and 10-min follow-up, the passive and active ROM of both IR and HA were significantly improved in the LC and stretching groups compared to the control group (p < 0.05) (Figure 1). However, the means of these values were not significantly different between the treatment groups at post-intervention and 10-min follow-up (p > 0.05) (Figure 1). The calculated effect sizes of passive and active ROM of both IR and HA are shown in Table 2.
Table 2.
Between-group effect sizes and p values for covariate-adjusted results.
| Effect size | p value < | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Local cryotherapy versus Control group |
Stretching versus Control group |
Local cryotherapy versus Stretching group |
Time | Group | Time × Group |
||||
| Post- | Follow-up | Post- | Follow-up | Post- | Follow-up | ||||
| PROM for IR (°) | 1.06 | .69 | .86 | .68 | .08 | .02 | <.001* | <.001* | <.001# |
| AROM for IR (°) | .93 | .56 | .64 | .46 | .25 | .06 | <.001* | <.001* | <.001# |
| PROM for HA (°) | .81 | .57 | .54 | .64 | .09 | -.19 | <.001* | .002* | .031# |
| AROM for HA (°) | .51 | .49 | .50 | .44 | -.01 | -.10 | <.001* | .001* | .004# |
| SS for IR (cm) | -.73 | -.51 | -.47 | -.35 | -.16 | -.04 | <.001* | <.001* | .003# |
| SS for HA (cm) | -.50 | -.43 | -.32 | -.28 | -.09 | -.07 | <.001* | <.001* | <.001# |
| PPT for Infra (kg) | .67 | .60 | .32 | .53 | .30 | .15 | <.001* | <.001* | <.001# |
| PPT for Post.D (kg) | .50 | .46 | .44 | .35 | .19 | .25 | .001* | <.001* | .033# |
* Significant time and group main effect;
#Significant group by time for interaction.
PROM: passive range of motion, AROM: active range of motion, IR: internal rotation, HA: horizontal adduction, SS: stretch sensation, PPT: pressure pain threshold, Infra: infraspinatus muscle, Post. D: posterior deltoid muscle.
Figure 1.
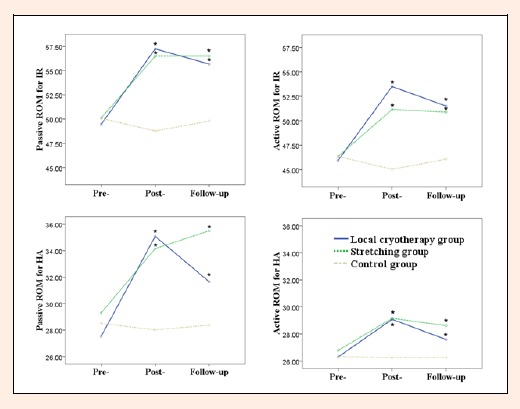
Covariate-adjusted value for ROM for passive and active glenohumeral IR and HA. * indicates significantly improved in intervention groups than those in the control group. ROM: range of motion, IR: internal rotation, HA: horizontal adduction.
For stretch sensation and PPT, there was significant group × time interaction (p < 0.01) (Table 2). At post-intervention and 10-min follow-up, stretch sensations were significantly decreased and PPTs were both significantly increased in both groups compared to the control (p < 0.01) but not compared to each other (p > 0.05) (Figure 2). The calculated effect sizes of stretch sensation and PPT are shown in Table 2.
Figure 2.
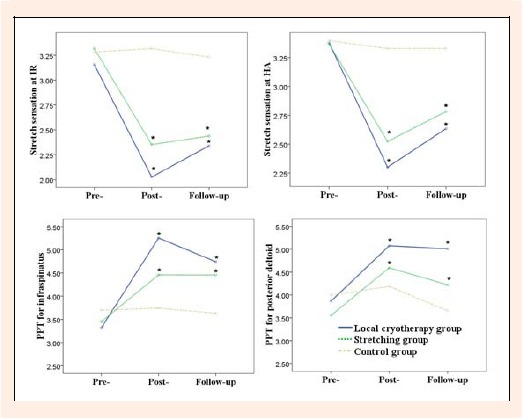
Covariate-adjusted value for stretch sensation when performing passive IR and HA, and PPT for infraspinatus and posterior deltoid muscles. * indicates significantly improved in intervention groups than those in the control group. IR: internal rotation, HA: horizontal adduction, PPT: pressure pain threshold.
Discussion
LC decreased the uncomfortable stretch sensation, increased the PPT, and improved passive and active ROM of IR and HA at post-intervention as well as at 10-min follow-up, similar to passive stretching. To the best of our knowledge, this is the first study to demonstrate that LC without passive stretching can decrease the uncomfortable stretch sensation, resulting in the improvement of passive and active ROM of IR and HA in individuals with posterior shoulder tightness. This finding may help clinicians improve posterior shoulder extensibility for patients or sports players with posterior shoulder tightness, who have high stretch sensitivity and low PPT in the infraspinatus and posterior deltoid muscles.
Our results are in agreement with a previous study that demonstrated that stretching with ice application provided better immediate improvement in hamstring flexibility than stretching with heat or stretching alone (Brodowicz et al., 1996). There are several explanations for ROM improvement after ice application. Based on sensory theory, modified stretch sensations and PPTs can improve a restricted ROM (Weppler and Magnusson, 2010). Brodowicz et al., 1996 speculated that ice application helped with the mild discomfort commonly felt at the end range of the stretch. In addition, the hypoalgesic effect of ice, known to increase PPT, reduce stretch sensitivity (Anaya Terroba et al., 2010). In the present study, after LC, PPT significantly increased and stretch sensation significantly decreased at the end range of passive glenohumeral IR and HA, resulting in increased ROM. A second plausible explanation for ROM gains is physiological reactions caused by LC. Surface application of LC decreases nerve conduction velocity and muscle spasm, and increases vascular response (Burke et al., 2001; Weston et al., 1994). However, LC in present study was performed for 3 minutes, while duration of several cryotherapy modalities in previous studies (varied from ice pack application to water immersion) was from 5 to 30 minutes (Burke et al., 2001; Costello and Donnelly, 2010; Dover and Powers, 2004). In present study, it is not clear whether 3 minutes of LC enough to change the vascular response and nerve conduction velocity. Hence, decreased stretch sensation via LC may be more influence on IR and HA ROM gains than vascular response and nerve conduction in present study.
Previous studies have demonstrated that passive cross-body stretch increases the ROM of passive IR in individuals with posterior shoulder tightness, however, these studies did not investigate the stretch sensation or muscle stiffness after exercise (McClure et al., 2007; Manske et al., 2010). In the present study, passive cross-body stretch decreased the uncomfortable stretch sensation, increased PPT, and improved ROM of IR and HA. The exact mechanism by which cross-body stretch improved ROM is unknown (Nichols et al., 2012). It might inhibit the activation of posterior deltoid and infraspinatus muscles, and release the posterior capsule (Nichols et al. 2012). Indeed, a previous study found that contract-relax stretching to release the glenohumeral horizontal abductor also immediately improved the ROM of passive IR (4.2° improvement) and HA (6.7° improvement) in individuals with posterior shoulder tightness; the authors speculated that the technique decreased stretch sensitivity which in turn improved the ROM (Moore et al., 2011). In our study, subjects showed an improved ROM of passive IR (6.4° improvement) and HA (6.2° improvement) and decreased stretch sensitivity at the end range of passive IR (27% reduction) and HA (27% reduction) after passive cross-body stretch. The LC group showed similar improvements in ROM of passive IR (7.8° improvement) and HA (8.9° improvement), and decreased stretch sensitivity at the end range of passive IR (42% reduction) and HA (32% reduction).
The effects of improved ROM, decreased stretch sensation, and increased PPT were significantly maintained in the LC group at the 10-min follow-up, similar to the stretching group. A previous study showed that increased extensibility by muscle stretching greatly declined within 15 min (de Weijer et al., 2003). In the present study, no significant changes were observed at 10-min after stretching. However, how long the decreased stretch sensation resulting from LC lasts is unknown.
This study has several limitations. First, our findings cannot be generalized to other populations because all subjects in our study were young. Second, we investigated the immediate effects of LC and stretching on joint ROM, and further long-term investigations are needed. Third, LC was applied for 3 min, which is a short duration, but sufficient to change the stretch sensation and PPT in a pilot test. Further study is necessary to investigate how long the effects of LC last.
Conclusion
LC immediately decreases stretch sensitivity and increases PPT, resulting in the improvements of the ROM of IR and HA of the glenohumeral joint, similar to stretching in subjects with posterior shoulder tightness. LC can be an alternative method when individuals with posterior shoulder tightness have high stretch sensitivity and low PPT in the infraspinatus and posterior deltoid muscles.
Biographies

Kyue-nam PARK
Employment
Department of Physical Therapy, Kinetic Ergocise Based on Movement Analysis Laboratory, Yonsei University, Wonju, South Korea
Degree
PhD
Research interests
Motion analysis of movement dysfunction in musculoskeletal disorders and Management of sports and playing-related musculoskeletal disorders.
E-mail: kema00@yonsei.ac.kr

Oh-yun KWON
Employment
Department of Physical Therapy, Kinetic Ergocise Based on Movement Analysis Laboratory, Yonsei University, Wonju, South Korea
Degree
PhD
Research interests
Mechanisms of movement impairment, movement analysis, and prevention and management of the work and sports related musculoskeletal pain syndrome
E-mail: kwonoy@yonsei.ac.kr

Jong-hyuck WEON
Employment
Department of Physical Therapy, Joongbu University, Wonju, Repulic of Korea
Degree
PhD
Research interests
Evaluation and management of movement impairments and Rehabilitaion in sport.
E-mail: jhweon@joongbu.ac.kr

Sung-dae CHOUNG
Employment
Department of Physical Therapy, Graduate School, Yonsei Univ., Wonju, South Korea
Degree
BSc
Research interests
Altered movement pattern and muscles activity in musculoskeletal disorders and Motion analysis in upper extremity
E-mail: dae282282@hanmail.net

Si-hyun KIM
Employment
Department of Physical Therapy, Graduate School, Yonsei Univ., Wonju, South Korea
Degree
MS
Research interests
Movement analysis and EMG study in musculoskeletal pain, including shoulder and lumbopelvic region / Rehabilitation of the movement impairment or sports injuries
E-mail: sihyun0411@naver.com
References
- Anaya Terroba L., Arroyo Morales M., Fernández-de-Las-Peñas C., Díaz-Rodríguez L., Cleland J.A. (2010) Effects of ice massage on pressure pain thresholds and electromyography activity postexercise: a randomized controlled crossover study. Journal of Manipulative and Physiological Therapeutics 33(3), 212-219 [DOI] [PubMed] [Google Scholar]
- Bach H.G., Goldberg B.A. (2006) Posterior capsular contracture of the shoulder. Journal of the American Academy of Orthopaedic Surgeons 14(5), 265-277 [DOI] [PubMed] [Google Scholar]
- Ben M., Harvey L.A. (2010) Regular stretch does not increase muscle extensibility: a randomized controlled trial. Scandinavian Journal of Medicine & Science in Sports 20(1), 136-144 [DOI] [PubMed] [Google Scholar]
- BjÃrklund M., Hamberg J., Crenshaw A. G. (2001) Sensory adaptation after a 2-week stretching regimen of the rectus femoris muscle. Archives of Physical Medicine and Rehabilitation 82(9), 1245-1250 [DOI] [PubMed] [Google Scholar]
- Borsa P. A., Wilk K. E., Jacobson J. A., Scibek J. S., Dover G. C., Reinold M., Andrews J. R. (2005) Correlation of range of motion and glenohumeral translation in professional baseball pitchers. American Journal of Sports Medicine 33(9), 1392-1399 [DOI] [PubMed] [Google Scholar]
- Brodowicz G.R., Welsh R., Wallis J. (1996) Comparison of stretching with ice, stretching with heat, or stretching alone on hamstring flexibility. Journal of Athletic Training 31(4), 324-327 [PMC free article] [PubMed] [Google Scholar]
- Burke D.G., Holt L.E., Rasmussen R., MacKinnon N.C., Vossen J.F., Pelham T.W. (2001) Effects of hot or cold water immersion and modified proprioceptive neuromuscular facilitation flexibility exercise on hamstring length. Journal of Athletic Training 36(1), 16-19 [PMC free article] [PubMed] [Google Scholar]
- Castellote-Caballero Y., Valenza M.C., Martín-Martín L., Cabrera-Martos I., Puentedura E.J., Fernández-de-Las-Peñas C. (2013) Effects of a neurodynamic sliding technique on hamstring flexibility in healthy male soccer players. A pilot study. Physical Therapy in Sport 14(3), 156-162 [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical power analysis for the behavioural sciences. 2nd edition Erlbaum, Hillsdale [Google Scholar]
- Costello J.T., Donnelly A.E. (2010) Cryotherapy and joint position sense in healthy participants: a systematic review. Journal of Athletic Training 45(3), 306-316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Weijer V.C., Gorniak G.C., Shamus E. (2003) The effect of static stretch and warm-up exercise on hamstring length over the course of 24 hours. The Journal of Orthopaedic and Sports Physical Therapy 33(12), 727-733 [DOI] [PubMed] [Google Scholar]
- Dover G., Powers M.E. (2004) Cryotherapy does not impair shoulder joint position sense. Archives of Physical Medicine and Rehabilitation 85(8), 1241-1246 [DOI] [PubMed] [Google Scholar]
- Folpp H., Deall S., Harvey L.A., Gwinn T. (2006) Can apparent increases in muscle extensibility with regular stretch be explained by changes in tolerance to stretch? Australian Journal of Physiotherapy 52(1), 45-50 [DOI] [PubMed] [Google Scholar]
- Fuentes C J., Armijo Olivo S., Magee D.J., Gross D.P. (2011) A preliminary investigation into the effects of active interferential current therapy and placebo on pressure pain sensitivity: a random crossover placebo controlled study. Physiotherapy 97(4), 291-301 [DOI] [PubMed] [Google Scholar]
- Jones D.H., Kilgour R.D., Comtois A.S. (2007) Test-retest reliability of pressure pain threshold measurements of the upper limb and torso in young healthy women. The Journal of Pain 8(8), 650-656 [DOI] [PubMed] [Google Scholar]
- Kolber M.J., Hanney W.J. (2010) The reliability, minimal detectable change and construct validity of a clinical measurement for identifying posterior shoulder tightness. North American Journal of Sports Physical Therapy 5(4), 208-219 [PMC free article] [PubMed] [Google Scholar]
- Laudner K.G., Stanek J.M., Meister K. (2006) Assessing posterior shoulder contracture: the reliability and validity of measuring glenohumeral joint horizontal adduction. Journal of Athletic Training 41(4), 375-380 [PMC free article] [PubMed] [Google Scholar]
- Law R.Y., Harvey L.A., Nicholas M.K., Tonkin L., De Sousa M., Finniss D.G. (2009. Stretch exercises increase tolerance to stretch in patients with chronic musculoskeletal pain: a randomized controlled trial. Physical Therapy 89(10), 1016-1026 [DOI] [PubMed] [Google Scholar]
- Ludewig P.M., Cook T.M. (2002) Translations of the humerus in persons with shoulder impingement symptoms. The Journal of Orthopaedic and Sports Physical Therapy 32(6), 248-259 [DOI] [PubMed] [Google Scholar]
- Ma S., Je H.D., Jeong J.H., Kim H. (2013) Effects of whole-body cryotherapy in the management of adhesive capsulitis of the shoulder. Archives of Physical Medicine and Rehabilitation 94(1), 9-16 [DOI] [PubMed] [Google Scholar]
- Manske R.C., Meschke M., Porter A., Smith B., Reiman M. (2010) A randomized controlled single-blinded comparison of stretching versus stretching and joint mobilization for posterior shoulder tightness measured by internal rotation motion loss. Sports Health 2(2), 94-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure P., Balaicuis J., Heiland D., Broersma M. E., Thorndike C. K., Wood A. (2007) A randomized controlled comparison of stretching procedures for posterior shoulder tightness. The Journal of Orthopaedic and Sports Physical Therapy 37(3), 108-114 [DOI] [PubMed] [Google Scholar]
- McNair P.J., Dombroski E.W., Hewson D.J., Stanley S.N. (2001) Stretching at the ankle joint: viscoelastic responses to holds and continuous passive motion. Medicine and Science in Sports and Exercise 33(3), 354-358 [DOI] [PubMed] [Google Scholar]
- Moore S.D., Laudner K.G., McLoda T.A., Shaffer M.A. (2011) The immediate effects of muscle energy technique on posterior shoulder tightness: a randomized controlled trial. The Journal of Orthopaedic and Sports Physical Therapy 41(6), 400-407 [DOI] [PubMed] [Google Scholar]
- Nelson R.T., Bandy W.D. (2004) Eccentric Training and static stretching improve hamstring flexibility of high school males. Journal of Athletic Training 39(3), 254-258 [PMC free article] [PubMed] [Google Scholar]
- Nichols J., Calver S., Chester R. (2012) Are stretches effective in the prevention and treatment of glenohumeral internal rotation deficit? Physical Therapy Reviews, 17(5), 261-270 [Google Scholar]
- Poser A., Casonato O. (2008) Posterior glenohumeral stiffness: capsular or muscular problem? A case report. Manual Therapy, 13(2), 165-170 [DOI] [PubMed] [Google Scholar]
- Reid D.A., McNair P.J. (2004) Passive force, angle, and stiffness changes after stretching of hamstring muscles. Medicine and Science in Sports and Exercise 36(11), 1944-1948 [DOI] [PubMed] [Google Scholar]
- Taylor B.F., Waring C.A., Brashear T.A. (1995) The effects of therapeutic application of heat or cold followed by static stretch on hamstring muscle length. The Journal of Orthopaedic and Sports Physical Therapy 21(5), 283-286 [DOI] [PubMed] [Google Scholar]
- Tyler T.F., Nicholas S.J., Roy T., Gleim G.W. (2000) Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. American Journal of Sports Medicine 28(5), 668-673 [DOI] [PubMed] [Google Scholar]
- Verducci F.M. (2000) Interval cryotherapy decreases fatigue during repeated weight lifting. Journal of Athletic Training 35(4), 422-426 [PMC free article] [PubMed] [Google Scholar]
- Weppler C.H., Magnusson S.P. (2010) Increasing muscle extensibility: a matter of increasing length or modifying sensation? Physical Therapy 90(3), 438-449 [DOI] [PubMed] [Google Scholar]
- Weston M., Taber C., Casagranda L., Cornwall M. (1994) Changes in local blood volume during cold gel pack application to traumatized ankles. The Journal of Orthopaedic and Sports Physical Therapy 19(4), 197-199 [DOI] [PubMed] [Google Scholar]
- Wilk K.E., Meister K., Andrews J.R. (2002) Current concepts in the rehabilitation of the overhead throwing athlete. American journal of Sports Medicine 30(1), 136-151 [DOI] [PubMed] [Google Scholar]
- Wilk K.E., Reinold M., Dugas J.R., Arrigo C.A., Moser M.W., Andrews J.R. (2005) Current concepts in the recognition and treatment of superior labral (SLAP) lesions. The Journal of Orthopaedic and Sports Physical Therapy 35(5), 273-291 [DOI] [PubMed] [Google Scholar]
- Yang J., Jan M., Chang C., Lin J. (2012) Effectiveness of the end-range mobilization and scapular mobilization approach in a subgroup of subjects with frozen shoulder syndrome: a randomized control trial. Manual Therapy 17(1), 47-52 [DOI] [PubMed] [Google Scholar]


