Abstract
Rationale: Current guidelines limit latent tuberculosis infection (LTBI) evaluation to persons in the United States less than or equal to 5 years based on the assumption that high TB rates among recent entrants are attributable to high LTBI reactivation risk, which declines over time. We hypothesized that high postarrival TB rates may instead be caused by imported active TB.
Objectives: Estimate reactivation and imported TB in an immigrant cohort.
Methods: We linked preimmigration records from a cohort of California-bound Filipino immigrants during 2001–2010 with subsequent TB reports. TB was likely LTBI reactivation if the immigrant had no evidence of active TB at preimmigration examination, likely imported if preimmigration radiograph was abnormal and TB was reported less than or equal to 6 months after arrival, and likely reactivation of inactive TB if radiograph was abnormal but TB was reported more than 6 months after arrival.
Measurements and Main Results: Among 123,114 immigrants, 793 TB cases were reported. Within 1 year of preimmigration examination, 85% of TB was imported; 6 and 9% were reactivation of LTBI and inactive TB, respectively. Conversely, during Years 2–9 after U.S. entry, 76 and 24% were reactivation of LTBI and inactive TB, respectively. The rate of LTBI reactivation (32 per 100,000) did not decline during Years 1–9.
Conclusions: High postarrival TB rates were caused by detection of imported TB through active postarrival surveillance. Among immigrants without active TB at baseline, reported TB did not decline over 9 years, indicating sustained high risk of LTBI reactivation. Revised guidelines should support LTBI screening and treatment more than 5 years after U.S. arrival.
Keywords: United States, epidemiology, emigrants and immigrants, guideline, public health
At a Glance Commentary
Scientific Knowledge on the Subject
U.S. surveillance data have suggested that new entrant’s risk of progression from latent to active tuberculosis (TB) is highest during their immediate postarrival years and then wanes. Therefore, current guidelines for the foreign-born limit latent TB evaluation to persons within 5 years of U.S. arrival. However, previous analyses have been unable to evaluate whether excess early risk is caused by imported active TB rather than reactivation of latent TB infection (LTBI).
What This Study Adds to the Field
In the largest cohort study of immigrants arriving in the United States from a high TB incidence country yet reported, we found that excess TB risk in the immediate postarrival years resulted entirely from detection of imported active TB. Risk of LTBI reactivation among immigrants does not seem to decline during the first 9 years after U.S. arrival. These findings support extending the recommendation for LTBI screening and treatment beyond 5 years after U.S. arrival in revised guidelines.
Tuberculosis (TB) among foreign-born persons is a central challenge to TB elimination in the United States. The percentage of TB cases occurring among foreign-born persons has increased steadily for two decades to 63% of all new U.S. cases in 2012 (1). TB exposure is uncommon in the United States and most TB among foreign-born persons results from reactivation of latent TB infection (LTBI) acquired before arrival (2). U.S. policy therefore emphasizes targeted testing and treatment of LTBI after arrival (3, 4). National surveillance data in the 1990s showed TB rates greater than fivefold higher within 5 years of arrival compared with subsequent years (5–7). New arrivals from high-incidence countries were hypothesized to arrive with high-risk “early latency” because of ongoing exposure and reinfection with new TB strains until U.S. arrival (8, 9). Because TB risk is highest immediately after infection, high TB rates immediately after arrival were assumed to indicate that reactivation risk declines with time in the United States. U.S. guidelines therefore target LTBI testing and treatment toward foreign-born persons in the United States within 5 years of their arrival (3).
An alternative explanation for high postarrival TB rates is detection of imported TB disease that is already active when a person arrives in the United States (10). Recent surveillance data indicate that TB rates are four to six times higher during Year 1 than during Years 2–4 (8, 11, 12). Since 1991, TB screening for adults entering as legal permanent residents (immigrants) has included a preimmigration examination and chest radiograph at designated overseas Panel Physician Clinics. Immigrants whose radiograph is consistent with TB (henceforth referred to as abnormal radiograph) undergo postarrival follow-up evaluation by U.S. local health agencies (13). If immigrants with abnormal radiographs are diagnosed with TB within 6 months of arrival, it is assumed TB was already active before arrival and their case is classified as imported TB (14, 15). Conversely, TB reported among immigrants whose preimmigration examination was normal has been considered likely caused by LTBI reactivation (16). TB also occurs because of postarrival TB exposures, but the limited burden of ongoing TB transmission in the United States makes this less common. Distinguishing LTBI reactivation from imported TB has important implications for LTBI treatment guidelines. Analyses of surveillance data have not distinguished between LTBI reactivation and imported TB because surveillance data before 2011 do not distinguish among key categories of new arrivals (i.e., immigrant, refugee, student, business traveler), and consequently are unable to ascertain the role of preimmigration and postimmigration evaluation.
The Philippines has a high TB incidence (260 per 100,000 in 2011) and is the source of a large volume of immigrants to the United States (17, 18). More than 60% of Filipinos are estimated to have LTBI (19). Filipino immigrants have among the highest rates of TB diagnosis of any U.S. immigrant group (15). In 2007, preimmigration examination in the Philippines was enhanced to include sputum culture in addition to sputum microscopy to improve predeparture detection of prevalent TB among applicants with abnormal radiograph. To evaluate reactivation and imported TB among a cohort of Filipinos applying for U.S. legal permanent residency, we linked preimmigration examination records with subsequently occurring cases in the California TB Case Registry. Some of these results have been previously reported in the form of an abstract (20).
Methods
We identified a cohort of adult Filipino applicants for permanent legal residency intending to resettle in California and analyzed reported TB during the first 9 postimmigration years.
Human Subjects Approval
Institutional Review Boards at the CDC, California Department of Public Health, Denver Health, and the University of Texas Health Sciences Center, Houston approved this study.
Preimmigration Evaluation Records
We obtained records for visa applicants evaluated at the only preimmigration screening site in the Philippines, St. Luke’s Medical Center Extension Clinic (SLMCEC), from January 4, 2001 to December 29, 2009. Two different screening guidelines were in place during this period (see the online supplement) (13). Briefly, before October 2007, applicants greater than or equal to 15 years of age underwent a medical questionnaire, physical examination, and chest radiograph (1991 guidelines). Applicants with an abnormal radiograph provided three sputum samples for acid-fast bacilli (AFB) smears but mycobacterial culture was not performed. Applicants with positive smears were required to initiate TB therapy before clearance. Emigration was permitted after smears were negative. Beginning on October 1, 2007 (13), sputum specimens from applicants with abnormal radiographs undergo both AFB smear and mycobacterial culture (2007 guidelines). For applicants with positive cultures, emigration is not permitted until TB is treated to completion by directly observed therapy. Applicants with negative smears and cultures are permitted to emigrate within 3 months of negative cultures. After U.S. arrival, only those immigrants with abnormal radiographs are recommended to have a follow-up evaluation to detect and treat active TB or inactive TB (defined as LTBI with an abnormal radiograph).
California TB Case Registry
TB cases among Philippines-born persons reported from January 1, 2001 to December 31, 2010 were ascertained from the California Department of Public Health.
Linkage of Data Sources
Using established methods (21), we linked preimmigration records and California TB reports using Registry Plus LinkPlus 2.0, a probabilistic record linkage program (22). Records were matched on last name, first name, date of birth, year of examination, and sex. Two reviewers manually reviewed results, applying predetermined rules to classify comparison pairs as true or false matches including (1) exact match in all fields, (2) mismatch in a single field, (3) first and last name transposition, or (4) obvious typographic errors. In cases of disagreement, a third independent reviewer made the final classification. Improbable matches were those whose evaluation occurred after the date of TB diagnosis.
Definitions and Statistical Analysis
Immigrants were individuals who received a permanent residency visa after screening in the Philippines. Likely LTBI reactivation was TB in an immigrant with a normal preimmigration examination and radiograph. Likely imported TB was TB reported less than or equal to 6 months after arrival in an immigrant with an abnormal preimmigration radiograph. Likely reactivation of inactive TB was TB reported more than 6 months after arrival in an immigrant with an abnormal preimmigration radiograph.
Using lifetable methods (23), we estimated annual TB rates after preimmigration examination among immigrants with (1) normal radiograph, (2) abnormal preimmigration radiograph evaluated with only sputum AFB smears (1991 guidelines), and (3) abnormal preimmigration radiograph evaluated with both sputum AFB smears and cultures (2007 guidelines). The date of preimmigration examination was used for all rate calculations.
To test whether hazard for LTBI reactivation changed with time in the United States, we fit a Cox regression model with year-specific effects with linear and quadratic terms to records from immigrants with normal preimmigration radiographs. We compared the hazard for TB among immigrants with an abnormal radiograph evaluated according to 1991 and 2007 guidelines using the survival and KMsurv packages in the R statistical suite, version 2.15.2.
Results
Cohort Characteristics
During 2001–2009, of 333,768 adult immigrants screened at SLMCEC, 123,114 (37%) intended to settle in California. Of these, 17,160 (14%) had an abnormal preimmigration radiograph (Table 1). Immigrants with abnormal radiographs were significantly older, more frequently male, and more frequently had self-reported diabetes, history of tobacco use, and history of pulmonary TB than those with normal radiographs.
Table 1:
Baseline Characteristics of 123,114 California-bound Filipino Adults during 2001–2009 with Abnormal and Normal Preimmigration Radiographs
| Abnormal Preimmigration
Radiograph (n =
17,160) |
Normal Preimmigration
Radiograph (n =
105,954) |
P Value | |
|---|---|---|---|
| n (%)* | n (%)* | ||
| Male | 7,791 (45) | 41,765 (39) | <0.0001 |
| Age, yr, median (IQR) | 59 (47–67) | 35 (22–52) | <0.0001 |
| Medical risks at time of overseas evaluation | |||
| Diabetes mellitus† | 1,976 (12) | 4,247 (4) | <0.0001 |
| Current smoking† | 2,304 (13) | 14,154 (13) | NS |
| History of smoking† | 6,311 (37) | 25,025 (24) | <0.0001 |
| Renal insufficiency† | 89 (<1) | 168 (<1) | <0.0001 |
| Chronic hepatitis† | 28 (<1) | 171 (<1) | NS |
| Malignancy† | 302 (2) | 581 (<1) | <0.0001 |
| History of pulmonary tuberculosis† | 2,693 (16) | 655 (<1) | <0.0001 |
| Preimmigration evaluation regimen‡ | |||
| CDC 1991 guidelines | 11,625 (68) | 81,354 (77) | |
| CDC 2007 guidelines | 5,535 (32) | 24,600 (23) |
Definition of abbreviations: IQR = interquartile range; NS = not significant.
Except as noted.
Self-reported at time of preimmigration examination.
After October 1, 2007, applicants with an abnormal radiograph underwent sputum culture in addition to sputum smear.
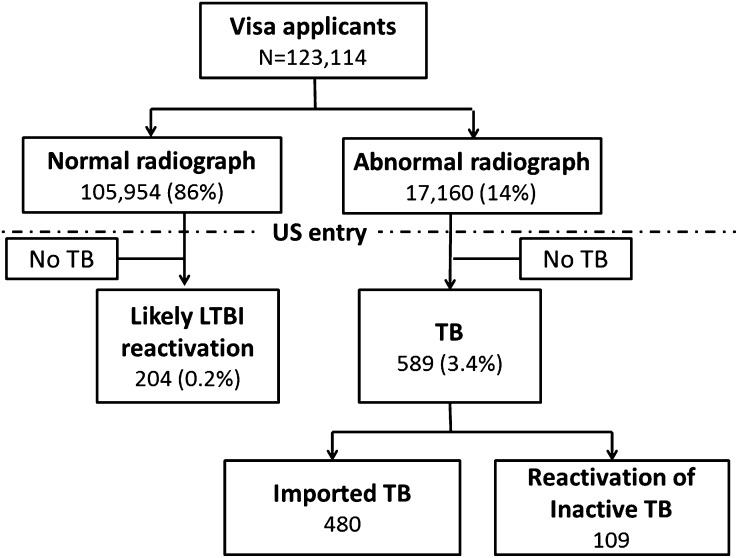
During 2001–2010, 4,324 Filipino adults were diagnosed with TB in California. For four individuals who had two episodes of TB, the second episode was excluded. Of the 3,900 (90%) with a recorded U.S. entry date, 1,316 (34%) reported entering during 2001–2009. Of these, 793 (60%) were linked to a preimmigration record at SLMCEC (Figure 1). Four additional records matched to California TB reports before the date of preimmigration evaluation and were excluded. Concordance between two independent reviewers during manual review was greater than 99%. During 2001–2010, postarrival evaluation was completed for 77% of California immigrants with abnormal preimmigration radiographs. Of these, 82% were completed within 6 months of arrival.
Figure 1.
Study flow. Overseas, preimmigration tuberculosis (TB) examination records for a cohort of 123,114 California-bound Filipino applicants for permanent U.S. residency were linked with the California TB case registry to ascertain which individuals developed TB. LTBI = latent tuberculosis infection.
TB Rate among Immigrants with Normal Preimmigration Radiographs (Likely LTBI Reactivation)
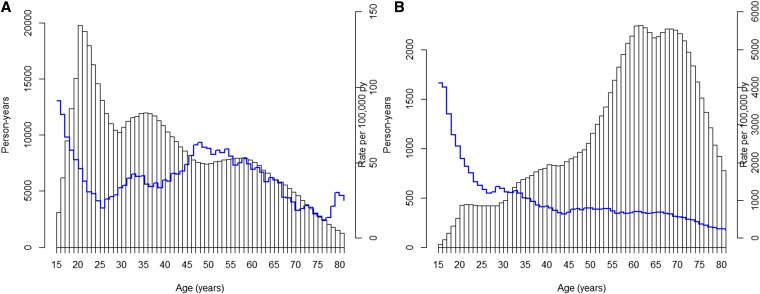
The rate of likely LTBI reactivation among immigrants with normal preimmigration examination and radiograph was 31.6 per 100,000 person-years (py) during the first 9 years in the United States. This rate did not change with increasing time in the United States (P value for trend in linear and quadratic models, 0.8 and 0.5, respectively) (Figure 2A). In the initial year after preimmigration examination, likely LTBI reactivation represented a small fraction of reported TB. During Year 1, 33 (5.8%) of 568 TB cases were likely LTBI reactivation with the remainder classified as imported or likely reactivation of inactive TB. Conversely, during subsequent years, 171 (76%) of 225 TB cases occurring in the entire cohort were likely LTBI reactivation.
Figure 2.
(A) Annual rates of likely latent tuberculosis (TB) infection reactivation among Filipino immigrants by year after overseas preimmigration TB examination. (B) Annual TB rates by year overseas preimmigration examination among three strata of immigrants: abnormal preimmigration radiograph evaluated according to 1991 guidelines with sputum smears only (red), abnormal preimmigration radiograph evaluated according to 2007 guidelines with both sputum smears and cultures (blue), and immigrants with normal preimmigration radiograph (likely latent TB infection reactivation, black). Inset table summarizes estimated annual rates during Year 1, Years 2–4, and Years 5–9. Immigrants evaluated under 1991 and 2007 guidelines had up to 9 years or 3 years of follow-up time, respectively. CI = confidence interval.
TB Rates among Immigrants with Abnormal Preimmigration Radiographs
TB rates among immigrants with abnormal radiographs differed depending on whether preimmigration examination included AFB smears alone (1991 guidelines) or smears and mycobacterial culture (2007 guidelines). During the initial year after preimmigration examination, TB rates among immigrants with abnormal radiographs evaluated according to 1991 and 2007 guidelines were more than 100 and more than 25 times higher than among immigrants with normal radiographs (4,172 and 903 per 100,000 vs. 31 per 100,000 py, respectively) (Figure 2B). Of 568 immigrants with TB in the year after preimmigration examination, 480 (84.5%) and 55 (9.7%) had imported TB and reactivation of inactive disease, respectively, because they had abnormal preimmigration radiographs and TB was reported within 6 months (imported) or after 6 months (reactivation of inactive disease) of arrival.
Among immigrants with abnormal preimmigration radiographs, TB declined markedly after the first year. Rates among those evaluated according to the smear-based 1991 guidelines declined 40- to 50-fold compared with the next 2–4 and 5–9 years (4,172 per 100,000 py vs. 95 per 100,000 py and 82 per 100,000 py, respectively). Rates among those evaluated with both sputum smears and culture according to 2007 guidelines declined from 903 per 100,000 py in the first year after preimmigration examination to 82 per 100,000 in Years 2–4. Despite the decline during Years 2–9, the TB rate among immigrants with abnormal radiographs was more than three times higher than among immigrants with normal radiographs (hazard ratio [HR], 3.8; 95% confidence interval [CI], 2.6–4.8).
Comparison with National Surveillance Data
The TB rate in the entire California-bound cohort (normal and abnormal radiographs combined for comparison with existing surveillance data) was more than 10 times higher during Year 1 than during Years 2–4 and 5–9 (463, 44, and 42 per 100,000 py, respectively). This is similar to recent U.S. surveillance data that estimate TB rates among new entrants from the Philippines to be 500 per 100,000 during Year 1 and 30–40 per 100,000 thereafter (8, 11).
Impact of Adding Sputum Culture to Preimmigration Examination (2007 Guidelines)
After mycobacterial culture was added to the preimmigration examination in October 2007, 7.0% of applicants with abnormal radiographs had Mycobacterium tuberculosis–positive sputum cultures and were therefore provided directly observed TB treatment before emigration. Of these, 74.8% were AFB smear-negative and would not have been detected under previous screening guidelines. After October 2007, hazard for TB diagnosis in California within the first year decreased by 79% compared with persons evaluated according to the 1991 guidelines (HR, 0.21; 95% CI, 0.16–0.28). After implementation, an average of 43 fewer imported TB cases were diagnosed each year compared with the preimplementation period (average 61 per year preimplementation vs. 18 per year postimplementation). In Years 2–9, TB risk among immigrants with abnormal radiographs did not differ based on whether or not they underwent sputum culture at preimmigration examination (HR, 0.63; 95% CI, 0.24–1.67).
Age and TB Rates
Age-specific differences in TB rates between immigrants with normal and abnormal radiographs are illustrated in Figure 3. The age distribution of immigrants with abnormal radiographs is shifted “rightward” relative to those with normal radiographs reflecting substantially older age at entry. Among immigrants with normal radiographs, the TB rate was high in late adolescence, declined in the twenties, then gradually increased to peak around age 50 (Figure 3A). By contrast, among immigrants with abnormal radiographs, rates were more than 4,000 per 100,000 py in late adolescence and declined fourfold by 35 years of age with a slow decline with increasing age thereafter (Figure 3B).
Figure 3.
Cumulative person-years (py) of observation (gray bars) and age-specific rate of tuberculosis (TB) diagnosis per 100,000 py (blue lines). (A) Among 105,987 Filipino immigrants with a normal preimmigration radiograph, young adults contributed most py of observation. The TB rate was high in late adolescence, dipped in the twenties, and rose to peak around age 50. (B) Among 17,127 Filipino immigrants with abnormal preimmigration radiograph, elderly persons contributed the most py of observation. The TB was highest in the youngest age and declined consistently over time. Age-specific rates are smoothed with a centered weighted 10-year moving average.
Clinical Characteristics of Likely LTBI Reactivation and Imported TB
Likely LTBI reactivation and imported TB differed in ways likely to influence transmission risk (Table 2). Immigrants with imported TB were significantly more frequently diagnosed with pulmonary TB than immigrants with likely LTBI reactivation (chi-square P < 0.0001). Of immigrants with pulmonary TB, those with imported TB were significantly less frequently sputum smear-positive (13%) than either immigrants with likely reactivation of inactive TB (23% smear-positive, P = 0.007) or likely LTBI reactivation (44% smear-positive, P < 0.0001).
Table 2:
Clinical Characteristics of 793 Adult Filipino Immigrants Evaluated at SLMCEC during 2001–2010 Who Were Subsequently Reported with TB in California
| Abnormal Preimmigration Radiograph |
Normal Preimmigration Radiograph | ||
|---|---|---|---|
| Imported TB* (n = 480) | Reactivation of Inactive TB† (n = 109) | Likely Latent TB Infection Reactivation‡ (n = 204) | |
| n (%) | n (%) | n (%) | |
| Primary site of disease | |||
| Pulmonary | 474 (99)§ | 99 (91)§ | 136 (67) |
| Pleural | 1 (<1) | 3 (3) | 6 (3) |
| Lymphatic | 1 (<1) | 3 (3) | 29 (14) |
| Other | 1 (<1) | 3 (3) | 31 (15) |
| Missing | 3 (1) | 1 (1) | 2 (1) |
| Sputum smear-positive|| | 60 (13)§ | 23 (23)|| | 60 (44) |
| Culture positive (any site) | 343 (71)§ | 65 (60) | 103 (50) |
| Clinical case¶ | 136 (28) | 39 (36) | 39 (19) |
Definition of abbreviations: SLMCEC = St. Luke’s Medical Center Extension Clinic; TB = tuberculosis.
TB diagnosed within 6 months of U.S. arrival in an immigrant with an abnormal preimmigration radiograph.
TB diagnosis after 6 months of U.S. arrival in an immigrant with an abnormal preimmigration radiograph.
TB diagnosed in an immigrant with a normal preimmigration radiograph.
Significantly different from imported TB group (chi-square P value < 0.001)
Significantly different from imported TB group (chi-square P value < 0.01)
No molecular or culture confirmation.
Discussion
Among Filipino immigrants whose preimmigration examination showed no evidence of active or inactive TB, the TB rate once in the United States did not decline over a 9-year period, remaining approximately 25-times higher than the 2012 TB rate among U.S.-born persons (1). Our findings are consistent with stable and persistent risk of LTBI reactivation. The perception that reactivation risk decreases over time has been based primarily on the observation that TB rates are highest immediately after arrival. In this cohort, high postarrival TB rates were entirely caused by imported TB, likely detected through active postarrival surveillance. Our observation of a sustained high risk of LTBI reactivation adds to mounting evidence that LTBI treatment should not be limited to the first 5 years after U.S. arrival (15, 24).
By distinguishing imported TB from likely reactivation TB, this cohort study provides critical insight into TB risk among immigrants and has important implications for clinicians and guidelines. The cause of the high TB rates consistently observed during initial postarrival years in U.S. national surveillance data (5, 6, 8, 11, 15) has been debated (10) but has generally been attributed to transiently increased risk of LTBI reactivation. Importantly, previous studies lacked preimmigration examination data and were unable to estimate the contribution of imported TB detected through active postarrival surveillance. The TB rate in our entire cohort (normal and abnormal radiographs combined) is consistent with previous surveillance estimates (8, 11) but stratification according to preimmigration radiographic status demonstrates that excess early TB risk is entirely caused by imported TB in the subgroup of immigrants with abnormal radiographs. Immigrants with normal preimmigration radiographs (86% of immigrants in this cohort) had no excess TB risk in the immediate postarrival years.
Our observation that TB risk among immigrants with normal preimmigration radiographs does not decline over time is consistent with cohorts of refugees and asylum seekers to low-incidence settings including Denmark (25, 26), Norway (27), Canada (28), Australia, and the United States (29). These studies consistently report a high burden of prevalent imported TB detected through active postarrival evaluation followed by persistently elevated TB incidence in ensuing years. Our estimates are consistent with studies from decades ago that observed TB rates of approximately 40–80 per 100,000 among immigrants with a normal preimmigration radiograph during the first 4–5 years after their immigration to the United States (16, 28, 29). A more recent U.S. case control study did not identify evidence of decreasing reactivation risk with time (10).
Preimmigration evaluation is designed to detect and prevent importation of active TB among applicants with abnormal radiographs. Routine LTBI testing is conducted only for immigrants with abnormal radiographs who complete postarrival follow-up. Our findings highlight that substantial further reduction in TB among immigrants requires expanding LTBI treatment among those with normal radiographs either overseas or after arrival (4, 15, 24, 30). In this study, 86% of adult immigrants had a normal preimmigration radiograph and this group accounted for 76% of TB diagnosed during Years 2–9 (after the initial period of active detection of imported TB), likely caused by progression of LTBI to active TB disease (2). Adding LTBI testing and treatment to the preimmigration evaluation of adults was encouraged by a 2000 Institute of Medicine report (4) but change has been hampered by concerns about feasibility, cost effectiveness, and legal authority to delay immigration for persons who do not pose an immediate public health risk (31–34). The development of IFN-γ release assays and shorter-course weekly LTBI therapy (35) could potentially make overseas LTBI evaluation and treatment feasible.
Expanding LTBI testing and treatment for foreign-born persons already in the United States could also reduce the occurrence of domestic TB. Key challenges are that current guidelines do not recommend LTBI evaluation for foreign-born persons in the United States more than 5 years who do not have a coexisting medical or additional epidemiologic risk, and that existing LTBI recommendations are not effectively implemented (36, 37). Several lines of evidence suggest that restricting LTBI evaluation to the first 5 years leaves foreign-born persons at substantial TB risk. In 2011, 65% of TB cases among foreign-born persons were diagnosed more than 5 years after arrival (38). A recent cost-effectiveness study identified the foreign-born in the United States more than 5 years as the largest potential opportunity for domestic TB prevention. Screening foreign-born persons who have lived in the United States more than 5 years prevented more cases at a lower cost per quality-adjusted life-year gained than screening other groups currently recommended for LTBI evaluation, such as U.S.-born persons who are incarcerated or have medical conditions (24). Finally, we note that the most desirable (and likely most cost-effective [33, 34]) means of preventing TB among the foreign-born in the United States is reducing TB incidence in the countries of origin.
By comparing two periods with distinct preimmigration guidelines, our results support an earlier report (14) that enhanced screening has substantially reduced imported active TB. Before October 2007, applicants with abnormal radiographs received only AFB smears without mycobacterial culture. Because of the limited sensitivity of AFB smears, rates of TB diagnosis at postarrival follow-up evaluation in the United States were extremely high. Implementation of mycobacterial culture dramatically reduced (but did not entirely eliminate) imported active disease. Postarrival follow-up evaluation therefore remains an important additional opportunity for case detection (13). Predeparture treatment of applicants with evidence of culture-negative active TB or inactive pulmonary TB is a potential strategy to further reduce imported TB among screened immigrants.
Our findings reinforce existing evidence that postarrival follow-up prevents the spread of TB in the United States (14, 39, 40). Among immigrants with abnormal preimmigration radiographs, those diagnosed within 6 months of entry likely as a result of follow-up evaluation (imported TB) were less frequently smear-positive than those who were diagnosed after 6 months (reactivation of inactive TB). This suggests that active follow-up of immigrants with abnormal radiographs detects TB at an earlier, less infectious stage of disease. Evaluating and treating inactive TB is an important secondary priority of postarrival evaluation. Effective LTBI evaluation and treatment or previous TB treatment may explain why the TB rate during Years 2–9 among persons with an abnormal preimmigration radiograph was lower than in historical cohorts of patients with untreated inactive TB (41, 42).
This study has several limitations. Our analysis is based on the conservative assumption that all applicants arrived and remained in California for capture of TB occurrence. Applicants who did not arrive would cause underestimation of the true rate in Year 1. Persons who died or migrated out of California would cause underestimation during subsequent years. Second, our analysis considered only legal permanent residents from the Philippines but we believe results are likely to be similar for screened immigrants entering from other countries with high rates of TB. Immigrants account for only about 500,000 of over 30 million foreign-born U.S. entrants each year. The remainder includes students, business travelers, tourists, and unauthorized visitors (12) who do not benefit from prearrival evaluation or active postarrival follow-up and are therefore less likely to have early detection of imported TB. Third, we do not know whether immigrants with normal radiographs were evaluated and treated for LTBI after U.S. arrival as guidelines recommend (3). We suspect most were not because a recent national survey indicated only 11.6% of foreign-born persons in the United States with a positive tuberculin skin test reported prior treatment for TB or LTBI (43). LTBI treatment would contribute to a lower rate. Finally, we have assumed that most TB among adult immigrants with normal preimmigration radiographs resulted from TB exposures in the Philippines for two reasons. The likelihood of acquiring LTBI over a lifetime in the Philippines (TB incidence > 60 times higher than in the United States) is substantially higher than acquiring LTBI in the United States during a shorter period. Second, more than 96% of TB among Asians in California occurs among foreign-born persons, suggesting domestic transmission within Asian communities is relatively uncommon. It is conceivable that some primary TB occurs because of new exposures occurring during return visits to the Philippines but 80% of Filipinos with reported TB in California had not returned to the Philippines in the 2 years before diagnosis (unpublished data). Disease occurring because of TB exposures in the United States or on return visits to the Philippines would cause overestimation of the LTBI reactivation rate but would not change our primary conclusions about the lack of decline in LTBI risk over time and the need to extend LTBI evaluation in this population.
Conclusions
In a large cohort of Filipino immigrants, the rate of likely LTBI reactivation among immigrants with a baseline normal preimmigration screening examination did not decline over 9 years. The very high early rate of TB frequently observed among immigrants is caused by imported active TB, likely detected as a result of active follow-up evaluation. Our findings suggest that current U.S. guidelines should be revised to support LTBI screening and treatment among immigrants from high TB-burden countries beyond the current first 5 years.
Footnotes
Supported by TB Epidemiologic Studies Consortium, U.S. Centers for Disease Control and Prevention (M.P., Y.F., and R.R.), and National Institutes of Health grant K-12 5K12HL090147-04 (N.D.W.).
Author Contributions: Conception and design, N.D.W., J.P., P.L., J.F., Y.F., and R.R. Data acquisition, N.D.W., J.P., P.L., Y.F., R.A., and R.R. Analysis and interpretation, N.D.W., J.P., M.P., P.L., J.F., Y.F., R.A., and R.R. Drafting the manuscript for important intellectual content, N.D.W., J.P., J.F., and R.R. Critical revision and final approval of manuscript, all authors.
Originally Published in Press as DOI: 10.1164/rccm.201308-1480OC on December 5, 2013
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Centers for Disease Control and Prevention (CDC) Trends in tuberculosis—United States, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:201–205. [PMC free article] [PubMed] [Google Scholar]
- 2.Ricks PM, Cain KP, Oeltmann JE, Kammerer JS, Moonan PK. Estimating the burden of tuberculosis among foreign-born persons acquired prior to entering the U.S., 2005-2009. PLoS ONE. 2011;6:e27405. doi: 10.1371/journal.pone.0027405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Thoracic Society. Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep. 2000;49:1–51. [PubMed] [Google Scholar]
- 4.Geiter L, editor. Washington, DC: National Academy Press; 2000. Ending neglect: the elimination of tuberculosis in the United States. [PubMed] [Google Scholar]
- 5.Zuber PLF, McKenna MT, Binkin NJ, Onorato IM, Castro KG. Long-term risk of tuberculosis among foreign-born persons in the United States. JAMA. 1997;278:304–307. [PubMed] [Google Scholar]
- 6.McKenna MT, McCray E, Onorato I. The epidemiology of tuberculosis among foreign-born persons in the United States, 1986 to 1993. N Engl J Med. 1995;332:1071–1076. doi: 10.1056/NEJM199504203321606. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Recommendations for prevention and control of tuberculosis among foreign-born persons. Report of the Working Group on Tuberculosis among Foreign-Born Persons. MMWR Recomm Rep. 1998;47:1–29. [PubMed] [Google Scholar]
- 8.Cohen T, Murray M. Incident tuberculosis among recent US immigrants and exogenous reinfection. Emerg Infect Dis. 2005;11:725–728. doi: 10.3201/eid1105.041107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guo H, Wu J. Persistent high incidence of tuberculosis among immigrants in a low-incidence country: impact of immigrants with early or late latency. Math Biosci Eng. 2011;8:695–709. doi: 10.3934/mbe.2011.8.695. [DOI] [PubMed] [Google Scholar]
- 10.Patel S, Parsyan AE, Gunn J, Barry MA, Reed C, Sharnprapai S, Horsburgh CR., Jr Risk of progression to active tuberculosis among foreign-born persons with latent tuberculosis. Chest. 2007;131:1811–1816. doi: 10.1378/chest.06-2601. [DOI] [PubMed] [Google Scholar]
- 11.Cain KP, Haley CA, Armstrong LR, Garman KN, Wells CD, Iademarco MF, Castro KG, Laserson KF. Tuberculosis among foreign-born persons in the United States: achieving tuberculosis elimination. Am J Respir Crit Care Med. 2007;175:75–79. doi: 10.1164/rccm.200608-1178OC. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Weinberg MS, Ortega LS, Painter JA, Maloney SA. Overseas screening for tuberculosis in U.S.-bound immigrants and refugees. N Engl J Med. 2009;360:2406–2415. doi: 10.1056/NEJMoa0809497. [DOI] [PubMed] [Google Scholar]
- 13.CDC. Atlanta: Centers for Disease Control and Prevention; 2009. CDC immigration requirements: technical instructions for tuberculosis screening and treatment using cultures and directly observed therapy. [Google Scholar]
- 14.Lowenthal P, Westenhouse J, Moore M, Posey DL, Watt JP, Flood J. Reduced importation of tuberculosis after the implementation of an enhanced pre-immigration screening protocol. Int J Tuberc Lung Dis. 2011;15:761–766. doi: 10.5588/ijtld.10.0370. [DOI] [PubMed] [Google Scholar]
- 15.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the United States. JAMA. 2008;300:405–412. doi: 10.1001/jama.300.4.405. [DOI] [PubMed] [Google Scholar]
- 16.Marks GB, Bai J, Simpson SE, Sullivan EA, Stewart GJ. Incidence of tuberculosis among a cohort of tuberculin-positive refugees in Australia: reappraising the estimates of risk. Am J Respir Crit Care Med. 2000;162:1851–1854. doi: 10.1164/ajrccm.162.5.2004154. [DOI] [PubMed] [Google Scholar]
- 17.United States. Department of Homeland Security. Yearbook of immigration statistics: 2010. Washington, DC: U.S. Department of Homeland Security, Office of Immigration Statistics; 2011 [Google Scholar]
- 18.World Health Organization. Geneva: World Health Organization; 2011. Global tuberculosis control: WHO report 2011. [Google Scholar]
- 19.Tupasi TE, Radhakrishna S, Pascual ML, Quelapio MID, Villa ML, Co VM, Sarol J, Mangubat N, Reyes AC, Sarmiento A, et al. BCG coverage and the annual risk of tuberculosis infection over a 14-year period in the Philippines assessed from the Nationwide Prevalence Surveys. Int J Tuberc Lung Dis. 2000;4:216–222. [PubMed] [Google Scholar]
- 20.Walter ND, John P, Jennifer F, Yunxin F, Kirsten W, Matthew P, Philip L, Redentor A, Randall R. Impact of enhanced pre-immigration evaluation on diagnosis of tuberculosis in California: a retrospective cohort study of Filipino immigrants based on electronic linkage [abstract] Am J Respir Crit Care Med. 2012;185:A2330. [Google Scholar]
- 21.Xia Q, Westenhouse JL, Schultz AF, Nonoyama A, Elms W, Wu N, Tabshouri L, Ruiz JD, Flood JM. Matching AIDS and tuberculosis registry data to identify AIDS/tuberculosis comorbidity cases in California. Health Informatics J. 2011;17:41–50. doi: 10.1177/1460458210380524. [DOI] [PubMed] [Google Scholar]
- 22.CDC. Atlanta: National Program of Cancer Registries; 2007. Registry plus link plus 2.0. [Google Scholar]
- 23.Rosner B. Boston: Brooks/Cole; 2011. Fundamentals of biostatistics. [Google Scholar]
- 24.Linas BP, Wong AY, Freedberg KA, Horsburgh CR., Jr Priorities for screening and treatment of latent tuberculosis infection in the United States. Am J Respir Crit Care Med. 2011;184:590–601. doi: 10.1164/rccm.201101-0181OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilcke JT, Poulsen S, Askgaard DS, Enevoldsen HK, Rønne T, Kok-Jensen A. Tuberculosis in a cohort of Vietnamese refugees after arrival in Denmark 1979-1982. Int J Tuberc Lung Dis. 1998;2:219–224. [PubMed] [Google Scholar]
- 26.Lillebaek T, Andersen AB, Dirksen A, Smith E, Skovgaard LT, Kok-Jensen A. Persistent high incidence of tuberculosis in immigrants in a low-incidence country. Emerg Infect Dis. 2002;8:679–684. doi: 10.3201/eid0807.010482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnsen NL, Steen TW, Meyer H, Heldal E, Skarpaas IJK, June GB. Cohort analysis of asylum seekers in Oslo, Norway, 1987-1995: effectiveness of screening at entry and TB incidence in subsequent years. Int J Tuberc Lung Dis. 2005;9:37–42. [PubMed] [Google Scholar]
- 28.Wang JS, Allen EA, Enarson DA, Grzybowski S. Tuberculosis in recent Asian immigrants to British Columbia, Canada: 1982-1985. Tubercle. 1991;72:277–283. doi: 10.1016/0041-3879(91)90054-v. [DOI] [PubMed] [Google Scholar]
- 29.Nolan CM, Elarth AM. Tuberculosis in a cohort of Southeast Asian Refugees: a five-year surveillance study. Am Rev Respir Dis. 1988;137:805–809. doi: 10.1164/ajrccm/137.4.805. [DOI] [PubMed] [Google Scholar]
- 30.Cain KP, Mac Kenzie WR. Editorial commentary: Overcoming the limits of tuberculosis prevention among foreign-born individuals: next steps toward eliminating tuberculosis. Clin Infect Dis. 2008;46:107–109. doi: 10.1086/523732. [DOI] [PubMed] [Google Scholar]
- 31.Mandalakas AM, Menzies D. Is screening immigrants for latent tuberculosis cost-effective? Lancet Infect Dis. 2011;11:418–419. doi: 10.1016/S1473-3099(11)70102-5. [DOI] [PubMed] [Google Scholar]
- 32.Schwartzman K, Menzies D. Tuberculosis screening of immigrants to low-prevalence countries. A cost-effectiveness analysis. Am J Respir Crit Care Med. 2000;161:780–789. doi: 10.1164/ajrccm.161.3.9902005. [DOI] [PubMed] [Google Scholar]
- 33.Schwartzman K, Oxlade O, Barr RG, Grimard F, Acosta I, Baez J, Ferreira E, Melgen RE, Morose W, Salgado AC, et al. Domestic returns from investment in the control of tuberculosis in other countries. N Engl J Med. 2005;353:1008–1020. doi: 10.1056/NEJMsa043194. [DOI] [PubMed] [Google Scholar]
- 34.Dasgupta K, Menzies D. Cost-effectiveness of tuberculosis control strategies among immigrants and refugees. Eur Respir J. 2005;25:1107–1116. doi: 10.1183/09031936.05.00074004. [DOI] [PubMed] [Google Scholar]
- 35.Sterling TR, Villarino ME, Borisov AS, Shang N, Gordin F, Bliven-Sizemore E, Hackman J, Hamilton CD, Menzies D, Kerrigan A, et al. TB Trials Consortium PREVENT TB Study Team. Three months of rifapentine and isoniazid for latent tuberculosis infection. N Engl J Med. 2011;365:2155–2166. doi: 10.1056/NEJMoa1104875. [DOI] [PubMed] [Google Scholar]
- 36.Horsburgh CR, Jr, Goldberg S, Bethel J, Chen S, Colson PW, Hirsch-Moverman Y, Hughes S, Shrestha-Kuwahara R, Sterling TR, Wall K, et al. Tuberculosis Epidemiologic Studies Consortium. Latent TB infection treatment acceptance and completion in the United States and Canada. Chest. 2010;137:401–409. doi: 10.1378/chest.09-0394. [DOI] [PubMed] [Google Scholar]
- 37.Sterling TR, Bethel J, Goldberg S, Weinfurter P, Yun L, Horsburgh CR Tuberculosis Epidemiologic Studies Cosortium. The scope and impact of treatment of latent tuberculosis infection in the United States and Canada. Am J Respir Crit Care Med. 2006;173:927–931. doi: 10.1164/rccm.200510-1563OC. [DOI] [PubMed] [Google Scholar]
- 38.CDC. Atlanta: U.S. Department of Health and Human Services, CDC; 2012. Reported tuberculosis in the United States, 2011. [Google Scholar]
- 39.Liu Y, Painter JA, Posey DL, Cain KP, Weinberg MS, Maloney SA, Ortega LS, Cetron MS. Estimating the impact of newly arrived foreign-born persons on tuberculosis in the United States. PLoS ONE. 2012;7:e32158. doi: 10.1371/journal.pone.0032158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maloney SA, Fielding KL, Laserson KF, Jones W, Nguyen TN, Dang QA, Nguyen HP, Nguyen AT, Duong TC, Vo TC, et al. Assessing the performance of overseas tuberculosis screening programs: a study among US-bound immigrants in Vietnam. Arch Intern Med. 2006;166:234–240. doi: 10.1001/archinte.166.2.234. [DOI] [PubMed] [Google Scholar]
- 41.International Union Against Tuberculosis Committee on Prophylaxis. Efficacy of various durations of isoniazid preventive therapy for tuberculosis: five years of follow-up in the IUAT trial. Bull World Health Organ. 1982;60:555–564. [PMC free article] [PubMed] [Google Scholar]
- 42.Ferebee SH. Controlled chemoprophylaxis trials in tuberculosis. A general review. Bibl Tuberc. 1970;26:28–106. [PubMed] [Google Scholar]
- 43.Bennett DE, Courval JM, Onorato I, Agerton T, Gibson JD, Lambert L, McQuillan GM, Lewis B, Navin TR, Castro KG. Prevalence of tuberculosis infection in the United States population: the National Health and Nutrition Examination Survey, 1999-2000. Am J Respir Crit Care Med. 2008;177:348–355. doi: 10.1164/rccm.200701-057OC. [DOI] [PubMed] [Google Scholar]