The greatest evil is physical pain.
—St. Augustine
Pain is an unwanted and sometimes unavoidable consequence of intensive care procedures. Although some pain is mild to moderate, and hence psychologically manageable for the patient, the personal experience of pain is distinctly subjective. A procedure that is tolerable for one patient may be intolerable for another. Certain procedures, for instance, a lumbar puncture (1), are extremely painful for most patients. At a minimum, extreme pain is highly distressing and may lead to persistent feelings of anxiety and dread that at times warrant a diagnosis of post-traumatic stress disorder. Nearly 25% of patients undergoing surgical treatment of peritonitis developed some post-traumatic stress disorder symptoms (2), as did 33 of 45 patients who demonstrated delusional memories 2 weeks after intensive care unit (ICU) discharge (3). The importance of recognizing, avoiding, and managing procedural pain in the ICU is therefore ethically compelling for medical professionals and of paramount importance to patients and their families.
The report from Puntillo and colleagues (pp. 39–47) in this issue of the Journal brings new focus to the problem of procedural pain in the ICU (4). The Europain study was a massive effort that encompassed 4,812 medical procedures in 28 countries and 192 ICUs. In this thoughtfully planned study, the investigators administered patient questionnaires translated into 12 languages, established interrater reliability between procedure observers, gathered data before and after 12 commonly performed procedures, and conducted an audit of the entire database for accuracy.
Numerous results and observations confirm previous findings and common practice. The most painful procedures, as reported by patients, were chest tube removal, wound drain removal, and arterial line insertion, consistent with previous reports from this and other groups (5–7). Although an increase in pain occurred with all procedures, reports of severe pain were rare. Planned procedures allow more pain-prevention preparation than emergency procedures. The investigators discuss and suggest various mitigation efforts commonly used in ICUs, including the administration of opioids, use of preventive local lidocaine injections, and the use of patient education about planned procedures.
The authors found that patients reporting higher pain before a procedure often reported greater pain during the procedure. Emphasis is therefore placed on conducting a preprocedure pain assessment such as the 0–10 numeric rating scale used in the study to help prevent procedural pain. Where reported pain is increased, the most obvious intervention is preemptive use of opiates, typically used with fewer than 50% of ICU patients undergoing procedures (8). Paradoxically, however, preprocedure pain assessment followed by preemptive use of opiates in Puntillo and colleagues’ study was associated with greater procedural pain intensity. It remains unclear whether focusing on a preprocedure pain assessment actually results in lower procedural pain. The authors conclude correctly that further research is needed to validate that a preprocedural pain assessment decreases pain intensity or emotional distress. Suggested considerations for more effective preemptive pain mitigation included greater consideration of dose and timing of opiate administration. Further investigation can help determine whether more effective, tailored opiate use can be directed by the preprocedural pain assessment.
Another striking result was the finding that across all procedures, those conducted by a nurse were associated with less pain than those conducted by a physician, respiratory therapist, or physiotherapist. This finding, which presumably does not reflect variance in procedural skills, strongly suggests that patients may have felt more reassured and comfortable with a nurse and highlights the importance of psychological factors in the experience of pain. That heightened anxiety is associated with increased pain perception is well known (9). In turn, caregiver compassion is an antidote to both anxiety and pain (10). A large literature of psychological approaches to pain management is largely focused on children but nonetheless contains lessons for adult pain management. This literature includes emphasis on awareness of events before and during the procedure, with focus on verbal and nonverbal provider behavior (11). A systematic review of 28 trials involving 1,951 children undergoing needle-related procedures found strong evidence for cognitive-behavioral interventions, and more limited but positive evidence for the effectiveness of hypnosis, information/preparation, and distraction in reducing procedural pain (12). Another systematic review including 19 trials and 1,513 pediatric patients reported that listening to music reduced pain in children undergoing oral surgery, venipuncture, bone marrow transplant, colposcopy, and burn dressing change (13).
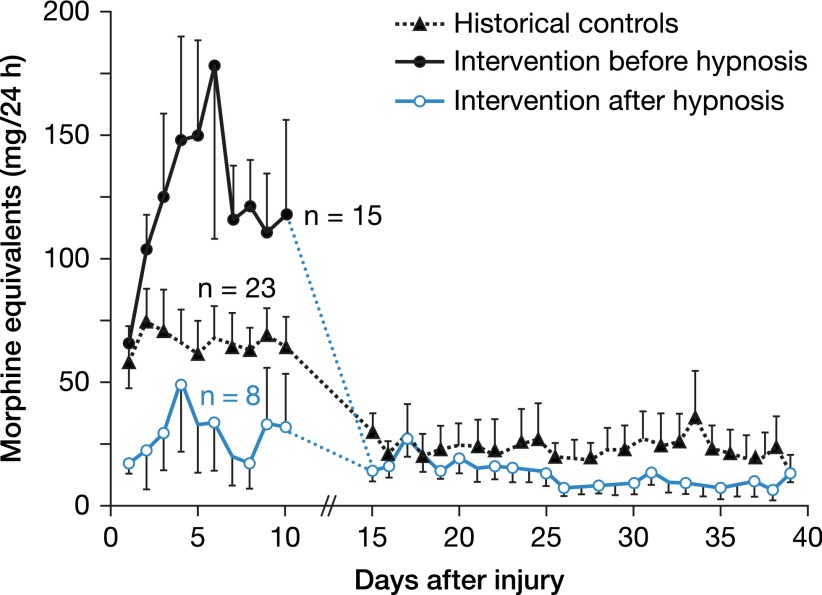
A far smaller literature has focused on complementary, nonpharmacologic procedures that may help reduce procedural pain in adults, including the use of noise-canceling headphones with music to reduce the perception of pain in men undergoing transrectal prostate biopsies (14), and the use of cognitive behavior therapy for chronic pain (15). A systematic review of 14 studies of pain interventions, 5 with ICU patients and most delivered by nurses, reported decreased pain and anxiety resulting from various relaxation strategies (16). Another investigation demonstrated opioid-sparing benefit when ICU burn patients received hypnosis. Twenty-three burn patients underwent hypnosis administered by trained ICU nurses, some immediately and others up to 2 weeks after admission. Compared with matched-control ICU burn patients, those who received hypnosis reported lower pain and anxiety scores, and had shorter hospital stays with reduced cost (Figure 1) (17). Although Puntillo and colleagues do not place primary emphasis on nonpharmacologic pain-reducing strategies, they do note the importance of using a soothing voice, preprocedural education, and inclusion of family members during procedures. The ICU—including its sounds, lights, equipment, multiple providers, and sense of urgency—can be frightening place, which in turn can fuel patient anxiety and pain apprehension. Further investigation of contextual changes, provider behaviors, and specific psychological and complementary interventions along with the use of opioids to reduce procedural pain is clearly needed.
Figure 1.
Opioid reduction in patients receiving hypnosis (17).
Footnotes
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Leffert LR, Schwamm LH. Neuraxial anesthesia in parturients with intracranial pathology: a comprehensive review and reassessment of risk. Anesthesiology. 2013;119:703–718. doi: 10.1097/ALN.0b013e31829374c2. [DOI] [PubMed] [Google Scholar]
- 2.Boer KR, Mahler CW, Unlu C, Lamme B, Vroom MB, Sprangers MA, Gouma DJ, Reitsma JB, De Borgie CA, Boermeester MA. Long-term prevalence of post-traumatic stress disorder symptoms in patients after secondary peritonitis. Crit Care. 2007;11:R30. doi: 10.1186/cc5710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones C, Griffiths RD, Humphris G, Skirrow PM. Memory, delusions, and the development of acute posttraumatic stress disorder-related symptoms after intensive care. Crit Care Med. 2001;29:573–580. doi: 10.1097/00003246-200103000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Puntillo KA, Max A, Timsit J-F, Vignoud L, Chanques G, Robleda G, Roche-Campo F, Mancebo J, Divatia JV, Soares M, et al. Determinants of procedural pain intensity in the intensive care unit: the Europain study. Am J Respir Crit Care Med. 2014;189:39–47. doi: 10.1164/rccm.201306-1174OC. [DOI] [PubMed] [Google Scholar]
- 5.Puntillo KA. Effects of interpleural bupivacaine on pleural chest tube removal pain: a randomized controlled trial. Am J Crit Care. 1996;5:102–108. [PubMed] [Google Scholar]
- 6.de Jong A, Molinari N, de Lattre S, Gniadek C, Carr J, Conseil M, Susbielles MP, Jung B, Jaber S, Chanques G. Decreasing severe pain and serious adverse events while moving intensive care unit patients: a prospective interventional study (the NURSE-DO project) Crit Care. 2013;17:R74. doi: 10.1186/cc12683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siffleet J, Young J, Nikoletti S, Shaw T. Patients’ self-report of procedural pain in the intensive care unit. J Clin Nurs. 2007;16:2142–2148. doi: 10.1111/j.1365-2702.2006.01840.x. [DOI] [PubMed] [Google Scholar]
- 8.Puntillo KA, Wild LR, Morris AB, Stanik-Hutt J, Thompson CL, White C. Practices and predictors of analgesic interventions for adults undergoing painful procedures. Am J Crit Care. 2002;11:415–429, quiz 430–431. [PubMed] [Google Scholar]
- 9.Pulvers K, Hood A. The role of positive traits and pain catastrophizing in pain perception. Curr Pain Headache Rep. 2013;17:330. doi: 10.1007/s11916-013-0330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duncan AD, Liechty JM, Miller C, Chinoy G, Ricciardi R. Employee use and perceived benefit of a complementary and alternative medicine wellness clinic at a major military hospital: evaluation of a pilot program. J Altern Complement Med. 2011;17:809–815. doi: 10.1089/acm.2010.0563. [DOI] [PubMed] [Google Scholar]
- 11.von Baeyer CL, Tupper SM. Procedural pain management for children receiving physiotherapy. Physiother Can. 2010;62:327–337. doi: 10.3138/physio.62.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uman LS, Chambers CT, McGrath PJ, Kisely S. Psychological interventions for needle-related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2006;(4):CD005179. doi: 10.1002/14651858.CD005179.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Klassen JA, Liang Y, Tjosvold L, Klassen TP, Hartling L. Music for pain and anxiety in children undergoing medical procedures: a systematic review of randomized controlled trials. Ambul Pediatr. 2008;8:117–128. doi: 10.1016/j.ambp.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Tsivian M, Qi P, Kimura M, Chen VH, Chen SH, Gan TJ, Polascik TJ. The effect of noise-cancelling headphones or music on pain perception and anxiety in men undergoing transrectal prostate biopsy. Urology. 2012;79:32–36. doi: 10.1016/j.urology.2011.09.037. [DOI] [PubMed] [Google Scholar]
- 15.Day MA, Thorn BE, Kapoor S. A qualitative analysis of a randomized controlled trial comparing a cognitive-behavioral treatment with education. J Pain. 2011;12:941–952. doi: 10.1016/j.jpain.2011.02.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Papathanassoglou ED. Psychological support and outcomes for ICU patients. Nurs Crit Care. 2010;15:118–128. doi: 10.1111/j.1478-5153.2009.00383.x. [DOI] [PubMed] [Google Scholar]
- 17.Berger MM, Davadant M, Marin C, Wasserfallen JB, Pinget C, Maravic P, Koch N, Raffoul W, Chiolero RL. Impact of a pain protocol including hypnosis in major burns. Burns. 2010;36:639–646. doi: 10.1016/j.burns.2009.08.009. [DOI] [PubMed] [Google Scholar]