Abstract
Overactive bladder (OAB) is a highly prevalent condition, affecting approximately 18% of adult Canadians. The impact of OAB is substantial, negatively affecting quality of life, sexuality and work productivity. Furthermore, patients with OAB are at increased risk of several other important comorbidities, including mood and anxiety disorders. Despite widespread availability of efficacious treatment, research has shown that OAB remains underdiagnosed and undertreated.
OAB: Prevalence
The current definition of overactive bladder (OAB) is “urgency, with or without urge incontinence, usually with frequency and nocturia.”1 Using this definition, the estimated prevalence of OAB in Canada is approximately 18%.2,3
Impact
The impact of OAB on a patient’s quality of life is substantial. Using the 36-Item Short-Form Health Survey (SF-36), research has demonstrated that the decrements in social and functional domains associated with OAB are more substantial than those of diabetes when compared to normal, healthy individuals (Fig. 1).4,5
Fig. 1.
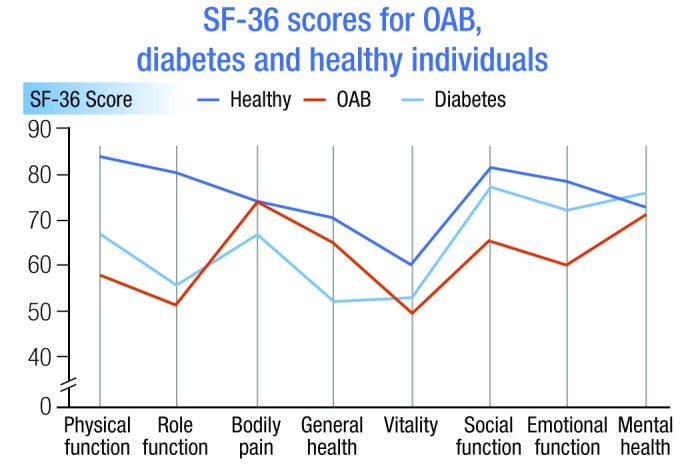
SF-36 scores for overactive bladder, diabetes and healthy individuals.
The Epidemiology of Lower Urinary Tract Symptoms (EpiLUTS) survey,6 which consisted of a battery of tests for OAB and lower urinary tract symptoms (LUTS), identified more than 7000 individuals with OAB in the United Kingdom, Sweden and the United States. Of the American respondents, 68% of women and 60% of men were bothered at least somewhat by their OAB, with the most bothersome symptoms reported to be urgency, urgency urinary incontinence and nocturia. These patients had low scores with respect to health-related quality of life, anxiety and depression.6
The burden of OAB also appears to extend beyond the bladder, as individuals with OAB are significantly more likely to have comorbid chronic conditions than individuals without OAB.7 The EPIC study, which was a cross-sectional, population-based survey of almost 20 000 adults in Canada, Germany, Italy, Sweden and the United Kingdom, showed that obesity, hypertension, depression, asthma, diabetes, chronic constipation and neurologic conditions (e.g., multiple sclerosis, stroke, Parkinsonism) were significantly more common among those with OAB than those without.7
Other researchers have shown that individuals with OAB, when compared to those without OAB or with minimal symptoms, have decreased sexual activity and sexual enjoyment,8,9 and that OAB is associated with a higher risk of work absenteeism, work disability and higher rates of unemployment.10,11 The impact of OAB on work parameters is similar to that of rheumatoid arthritis and asthma.11
In terms of financial impact, a 2010 American study estimated that the total annual cost of OAB in that country was over $65 billion in the year 2007, with costs projected to reach $82.6 billion in 2020.12 Importantly, the costs of pharmacologic therapy represent only a small fraction of total costs associated with OAB.12
Current shortcomings of OAB management
There appear to be substantial gaps in OAB knowledge among primary-care physicians and patients.13–15 For example, a survey of primary-care physicians showed that these healthcare professionals failed to identify 57.5% of patients with OAB.13 Among OAB patients, research has shown gaps in knowledge about physiology and understanding of diagnostic tests.15 Furthermore, patient expectations about treatment have been found to be unrealistic.15
OAB is also undertreated. An analysis of a large U.S. database (IMS Health) showed that only one-quarter of patients with a diagnosis of OAB are treated.16 Of these individuals, approximately three-quarters were women. A large part of the problem of under-treatment is related to very low rates of persistence with medication. An analysis of persistence rates with various antimuscarinic agents showed that the one-year persistence rates ranged from 14% to 35% (Fig. 2).17
Fig. 2.
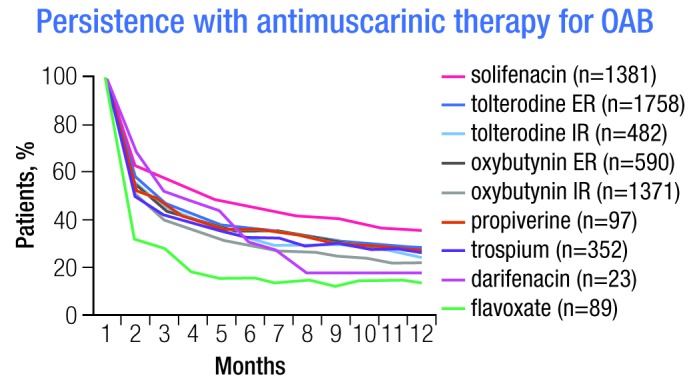
Persistence with antimuscarinic therapy for overactive bladder.
Conclusions
OAB is highly prevalent and has a substantial impact on both patients and society. While there are many therapies available to help patients with this chronic condition, including several novel agents, clear barriers to effective management remain. Many patients are not being diagnosed, those who are diagnosed may not receive treatment, and those who do receive treatment may not continue with therapy over the long term. Given these dynamics, strategies to improve access and treatment rates may be just as important as finding even more novel therapies.
Footnotes
Competing interests: This article is part of a CUAJ supplement sponsored by Astellas Pharma Canada, Inc. Dr. Herschorn is an ongoing paid consultant for, or has received speaker fees, educational grants, and/or travel assistance from Allergan, American Medical Systems, Astellas, Merus Labs, Pfizer, and Promedon.
References
- 1.Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–78. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 2.Herschorn S, Gajewski J, Schulz J, et al. A population-based study of urinary symptoms and incontinence: the Canadian Urinary Bladder Survey. BJU Int. 2008;101:52–8. doi: 10.1111/j.1464-410X.2007.07198.x. [DOI] [PubMed] [Google Scholar]
- 3.Corcos J, Schick E. Prevalence of overactive bladder and incontinence in Canada. Can J Urol. 2004;11:2278–84. [PubMed] [Google Scholar]
- 4.Abrams P, Kelleher CJ, Kerr LA, et al. Overactive bladder significantly affects quality of life. Am J Manag Care. 2000;6:S580–90. [PubMed] [Google Scholar]
- 5.Komaroff AL, Fagioli LR, Doolittle TH, et al. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Am J Med. 1996;101:281–90. doi: 10.1016/S0002-9343(96)00174-X. [DOI] [PubMed] [Google Scholar]
- 6.Milsom I, Kaplan SA, Coyne KS, et al. Effect of bothersome overactive bladder symptoms on health-related quality of life, anxiety, depression, and treatment seeking in the United States: results from EpiLUTS. Urology. 2012;80:90–6. doi: 10.1016/j.urology.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Irwin DE, Milsom I, Kopp Z, et al. Comorbidities associated with overactive bladder: results from the EPIC study. Neurourol Urodyn 2007. Poster 141. Presented at the 37th Annual Meeting of the International Continence Society; August 20–24, 2007; Rotterdam, Netherlands. [Google Scholar]
- 8.Irwin DE, Milsom I, Kopp Z. Impact of overactive bladder and stress urinary incontinence on sexual quality of life in women. Presented at: International Society for the Study of Women’s Sexual Health 2007 Annual Meeting; February 22–25, 2007; Lake Buena Vista, Florida. [Google Scholar]
- 9.Coyne KS, Sexton CC, Thompson C, et al. The impact of OAB on sexual health in men and women: results from EpiLUTS. J Sex Med. 2011;8:1603–15. doi: 10.1111/j.1743-6109.2011.02250.x. [DOI] [PubMed] [Google Scholar]
- 10.Wu EQ, Birnbaum H, Marynchenko M, et al. Employees with overactive bladder: work loss burden. J Occup Environ Med. 2005;47:439–46. doi: 10.1097/01.jom.0000161744.21780.c1. [DOI] [PubMed] [Google Scholar]
- 11.Coyne KS, Sexton CC, Thompson CL, et al. Impact of overactive bladder on work productivity. Urology. 2012;80:97–103. doi: 10.1016/j.urology.2012.03.039. [DOI] [PubMed] [Google Scholar]
- 12.Ganz ML, Smalarz AM, Krupski TL, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75:526–32. doi: 10.1016/j.urology.2009.06.096. [DOI] [PubMed] [Google Scholar]
- 13.Goepel M, Hoffmann JA, Piro M, et al. Prevalence and physician awareness of symptoms of urinary bladder dysfunction. Eur Urol. 2002;41(3):234–9. doi: 10.1016/S0302-2838(02)00014-3. [DOI] [PubMed] [Google Scholar]
- 14.Shaw C, Tansey R, Jackson C, et al. Barriers to help seeking in people with urinary symptoms. Fam Pract. 2001;18:48–52. doi: 10.1093/fampra/18.1.48. [DOI] [PubMed] [Google Scholar]
- 15.Smith AL, Nissim HA, Le TX, et al. Misconceptions and miscommunication among aging women with overactive bladder symptoms. Urology. 2011;77:55–9. doi: 10.1016/j.urology.2010.07.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Helfand BT, Evans RM, McVary KT. A comparison of the frequencies of medical therapies for overactive bladder in men and women: analysis of more than 7.2 million aging patients. Eur Urol. 2010;57:586–91. doi: 10.1016/j.eururo.2009.12.025. [DOI] [PubMed] [Google Scholar]
- 17.Wagg A, Compion G, Fahey A, et al. Persistence with prescribed antimuscarinic therapy for overactive bladder: a UK experience. BJU Int. 2012;110:1767–74. doi: 10.1111/j.1464-410X.2012.11023.x. [DOI] [PubMed] [Google Scholar]


