Abstract
In disease-endemic areas, histoplasmosis is the main differential diagnosis for tuberculosis among human immunodeficiency virus (HIV)–infected patients. However, no study has compared the two diseases. Thus, the objective of this study was to compare tuberculosis and histoplasmosis in HIV-infected patients. A population of 205 HIV-infected patients (99 with tuberculosis and 106 with histoplasmosis) hospitalized in Cayenne, French Guiana during January 1, 1997–December 31, 2008 were selected retrospectively from the French Hospital Database on HIV. Multivariate analysis showed that tuberculosis was associated with cough (adjusted odds ratio [AOR] = 0.20, 95% confidence interval [CI] = 0.05–0.73) and a C-reactive protein level > 70 mg/L (AOR = 0.98, 95% CI = 0.97–0.99). Variables associated with disseminated histoplasmosis were a γ-glutamyl transferase level > 72 IU/L (AOR = 4.99, 95% CI = 1.31–18.99), origin from French Guiana (AOR = 5.20, 95% CI = 1.30–20.73), disseminated localization (AOR = 6.40, 95% CI = 1.44–28.45), a concomitant opportunistic infection (AOR = 6.71, 95% CI = 1.50–29.96), a neutrophil count < 2,750 cells/mm3 (AOR = 10.54, 95% CI = 2.83–39.24), a CD4 cell count < 60 cells/mm3 (AOR = 11.62, 95% CI = 2.30–58.63), and a platelet count < 150,000/mm3 (AOR = 19.20, 95% CI = 3.35–110.14). Tuberculosis and histoplasmosis have similarities, but some factors show a greater association with one of these diseases. Thus, adapted therapeutic choices can be made by using simple clinical and paraclinical criteria.
Introduction
With an acquired immunodeficiency syndrome (AIDS) incidence 10 times higher than the incidence in mainland France, and a prevalence > 1%, French Guiana is the French territory where the human immunodeficiency virus (HIV) epidemic is the most preoccupying.1 Histoplasmosis and tuberculosis are among the top four AIDS-defining illnesses. Disseminated histoplasmosis was the first AIDS-related cause of death in 2005.2,3
Histoplasmosis and tuberculosis during the HIV infection are often seen as disseminated infections. With the aggravation of immunodeficiency, dissemination of the pathogen causes a rapid and fatal evolution in the absence of treatment.4,5 At this stage, invasive diagnostic methods are necessary. Biological confirmation through pathogen identification by culture is long and sometimes difficult in cases of profound immunosuppression. Rapid and sensitive antigenic detection techniques are not available in most countries.6
The non-specific nature of the clinical, biologic, histologic, and radiologic findings for these two diseases makes differential diagnosis of histoplasmosis difficult in disease-endemic areas. Thus, numerous publications report cases of histoplasmosis mimicking tuberculosis, most often because of the absence of diagnostic facilities or because a diagnosis of histoplasmosis was not considered.7–11
Although studies before the HIV era reported a high prevalence of positive histoplasmin test results there have been few publications on this disease in the Caribbean and the Guianas.3,12,13 In low-resource countries, a number of AIDS cases may die of histoplasmosis mistaken for multidrug-resistant tuberculosis.10,14,15
In French Guiana, because of their high incidence, clinicians generally suspect histoplasmosis and tuberculosis in immunosuppressed patients at admission. Prolonged hospitalizations are often necessary for identification of infecting pathogens by invasive procedures. Mycologic and mycobacteriologic screening are systematically performed. Frequently, a presumptive treatment is initiated before culture results are obtained.16
In this context, a comparative study between tuberculosis and histoplasmosis seems straightforward and might be useful. A systematic review of the literature showed that since 1906, studies on the differential diagnosis of tuberculosis and histoplasmosis have not been conducted.17 Although it is assumed that these two diseases are similar, there is little basis for making this conclusion.
The objective of this study was to compare tuberculosis and histoplasmosis in HIV-infected patients to identify epidemiologic, clinical, biologic, and radiologic differences. A secondary objective was to help therapeutic decisions in life-threatening situations.
Materials and Methods
This retrospective study was conducted at Cayenne Hospital (Cayenne, French Guiana) during January 1997–December 2008. The study population consisted of HIV-infected patients from the French Hospital Database on HIV, a national cohort for which data have been routinely collected since 1992. This database was approved by the Commission Nationale Informatique et Libertés. The study database and protocol were approved by the Institut National de la Santé et de la Recherche Médicale (INSERM (IRB00000388, FWA00005831). Patients provided written informed consent.
Inclusion criteria for study participants were an age ≥ 18 years), admission to Cayenne Hospital or a visit to the outpatient department before admission (the inclusion date corresponding to the date of treatment initiation for tuberculosis or histoplasmosis), inclusion in the French Hospital Database, confirmed HIV infection (by Western blotting), confirmed tuberculosis (culture and identification of Mycobacterium tuberculosis) or histoplasmosis (direct examination and/or culture of Histoplasma capsulatum var. capsulatum), and pre-treatment biologic screening < 7 days before treatment initiation. Exclusion criteria were concomitant tuberculosis and histoplasmosis, a history of tuberculosis or histoplasmosis, immune reconstitution disease caused by tuberculosis or histoplasmosis, and a diagnosis of tuberculosis or histoplasmosis by polymerase chain reaction only, which is not a valid reference method for diagnosis.
Data were collected on a standardized form and included sociodemographic, clinical, biologic, radiologic, and therapeutic information. Clinical evaluation of the patients' general condition upon admission used the Eastern Cooperative Oncology Group score,18 also known as the World Health Organization performance status score. These data were then entered in an anonymized database.
Statistical analysis was performed by using Stata version 10.0 (StataCorp LP, College Station, TX).19 Descriptive and comparative analysis was performed by using Pearson's chi-square test or Fischer's exact test for categorical variables, Student's t test for normally distributed quantitative variables, or Mann-Whitney test for non-Gaussian distributions. Statistical significance was set at P < 0.05.
To identify criteria independently associated with tuberculosis and histoplasmosis, stepwise unconditional logistic regression was used.20 Forward and backward models were used to verify convergence. The dependent variable was tuberculosis or histoplasmosis, coded 0 and 1 respectively. Odds ratios (ORs) and 95% confidence intervals were obtained. For an OR < 1, the variable was associated with tuberculosis, and for an OR > 1, the variable was associated with histoplasmosis.
To select variables for the multivariate model, bivariate logistic regression models used categorical independent variables. In the absence of similar studies in the literature, the cut-off value was the median or mean according to the distribution of continuous variables. For some variables, the reference laboratory threshold was used because it was clinically meaningful (i.e., for platelet counts, the median was 222,000/mm3, but categorization used a threshold < 150,000/mm3). For ferritinemia, some ferritin concentrations were > 1,000 μg/L. To avoid confusion, the variable was categorized as > or < 1,000 μg/L.
Age, sex, and variables that had a P < 0.2 were used in the multivariate model. Variables with a P < 0.2 (systolic and diastolic blood pressure, chest computed tomography scan, abdominal ultrasonography, albuminemia, serum iron level, ferritinemia, triglyceridemia, and fibrinogenemia) were not included in this model because of a large number of missing values and to avoid a large proportion of persons who were dropped from the final model. The saturated multivariate model included 156 patients.
Results
Results of univariate and bivariate analysis are shown in Table 1. The study population consisted of 205 HIV-positive persons. Two groups were defined: 99 persons with tuberculosis and 106 persons with histoplasmosis. There was a predominance of males in both groups. The mean ± SD age was similar in both groups (39.3 ± 11.6 for persons with tuberculosis and 41.6 ± 10.6 for persons with histoplasmosis) (P = 0.151).
Table 1.
Univariate and bivariate analyses of tuberculosis and histoplasmosis in 205 human immunodeficiency virus–infected patients, French Guiana*
| Variable | Tuberculosis, no. positive/no. tested (%) | Histoplasmosis, no. positive/no. tested (%) | Bivariate analysis | |
|---|---|---|---|---|
| OR (95% CI) | P | |||
| Sex† | ||||
| M | 70/99 (71) | 69/106 (65) | 1 | |
| F | 29/99 (29) | 37/106 (35) | 1.29 (0.72–2.33) | 0.391 |
| Age < 40 years† | 50/99 (50) | 51/106 (48) | 0.91 (0.52–1.57) | 0.732 |
| Geographic origin†‡ | ||||
| Haiti | 42/96 (44) | 33/105 (31) | 1 | |
| French Guiana | 12/96 (12) | 33/105 (31) | 3.50 (1.57–7.81) | 0.002 |
| Europe | 5/96 (5) | 2/105 (2) | 0.51 (0.09–2.79) | 0.437 |
| Guadeloupe | 3/96 (3) | 6/105 (6) | 2.54 (0.59–10.95) | 0.209 |
| Guyana | 19/96 (20) | 6/105 (6) | 0.40 (0.14–1.12) | 0.081 |
| Suriname | 1/96 (1) | 17/105 (16) | 21.64 (2.74–171.07) | 0.004 |
| Brazil | 12/96 (12) | 6/105 (6) | 0.64 (0.22–1.87) | 0.412 |
| Africa | 2/96 (2) | 1/105 (1) | 0.64 (0.05–7.33) | 0.717 |
| Time spent in French Guiana > 18 years†§ | 31/76 (41) | 60/99 (61) | 2.23 (1.21–4.11) | 0.010 |
| Residence location†‡ | ||||
| Cayenne urban community | 60/84 (72) | 64/101 (63) | 1 | |
| Homeless | 12/84 (14) | 8/101 (8) | 0.62 (0.24–1.63) | 0.338 |
| Outside Cayenne urban community | 12/84 (14) | 29/101 (29) | 2.27 (1.06–4.84) | 0.035 |
| AIDS-defining event | 77/92 (84) | 87/106 (82) | 0.89 (0.42–1.87) | 0.763 |
| Treatment on admission | ||||
| Antiretroviral drugs | 15/98 (15) | 16/105 (15) | 0.99 (0.46–2.14) | 0.989 |
| Primary prophylaxis | 20/98 (20) | 23/98 (23) | 2.00 (0.61–2.36) | 0.605 |
| Opportunistic infection | ||||
| History† | 15/98 (15) | 18/106 (17) | 1.13 (0.54–2.39) | 0.746 |
| Concomitant† | 17/98 (17) | 45/106 (42) | 3.51 (1.84–6.73) | < 0.001 |
| Drug addictions | ||||
| Tobacco† | 14/98 (14) | 1/104 (1) | 0.06 (0.01–0.46) | 0.007 |
| Alcohol | 11/98 (11) | 9/104 (9) | 0.76 (0.30–1.91) | 0.557 |
| Marijuana | 2/98 (2) | 1/104 (1) | 0.47 (0.04–5.27) | 0.541 |
| Crack cocaine† | 14/98 (14) | 7/104 (7) | 0.43 (0.17–1.12) | 0.085 |
| Multiple addictions (≥ 2) | 11/98 (11) | 2/103 (2) | 0.16 (0.03–0.73) | 0.18 |
| Isolate localization | ||||
| Pleuro-pulmonary | 91/99 (92) | 28/106 (26) | 0.03 (0.01–0.07) | < 0.001 |
| Lymph node | 18/99 (18) | 21/106 (20) | 1.11 (0.55–2.24) | 0.766 |
| Liver | 8/99 (8) | 28/106 (26) | 4.08 (1.76–9.48) | 0.001 |
| Peripheral blood | 6/99 (6) | 16/106 (15) | 2.76 (1.03–7.36) | 0.043 |
| Gastrointestinal | 4/99 (4) | 17/106 (16) | 4.54 (1.47–14.00) | 0.009 |
| Bone marrow | 1/99 (1) | 46/106 (43) | 75.13 (10.10–559.10) | < 0.001 |
| Disseminated† | 37/99 (37) | 98/106 (92) | 20.53 (8.97–46.97) | < 0.001 |
| Physical condition at admission | ||||
| WHO performance status score > 2† | 23/97 (24) | 42/52 (81) | 13.51 (5.87–31.10) | < 0.001 |
| Weight loss | 67/88 (76) | 35/43 (81) | 1.37 (0.55–3·41) | 0.497 |
| Physical examination | ||||
| Fever | 83/97 (86) | 93/106 (88) | 1.21 (0.54–2.71) | 0.650 |
| Systolic blood pressure < 90 mm Hg | 4/64 (6) | 10/29 (34) | 7.89 (2.22–28.09) | 0.001 |
| Diastolic blood pressure < 60 mm Hg | 7/64 (11) | 10/29 (34) | 4.29 (1.43–12.83) | 0.009 |
| Cough† | 70/98 (71) | 45/105 (43) | 0.30 (0.17–0.54) | < 0.001 |
| Dyspnea† | 13/98 (13) | 21/105 (20) | 1.63 (0.79–3.48) | 0.202 |
| Chest pain† | 20/98 (20) | 2/105 (2) | 0.08 (0.02–0.33) | 0.001 |
| Abdominal pain | 30/98 (31) | 34/105 (32) | 1.09 (0.60–1.96) | 0.786 |
| Diarrhea | 22/98 (22) | 29/105 (28) | 1.32 (0.70–2.50) | 0.397 |
| Ascitis | 1/98 (1) | 3/105 (3) | 2.85 (2.92–27.90) | 0.368 |
| Hepatomegaly† | 19/98 (19) | 41/105 (39) | 2.62 (1.39–4.95) | 0.003 |
| Splenomegaly† | 4/98 (4) | 21/105 (20) | 5.81 (1.92–17.59) | 0.002 |
| Lower digestive bleeding† | 1/98 (1) | 7/105 (7) | 6.93 (0.84–57.38) | 0.073 |
| Headache | 9/98 (9) | 10/105 (9) | 1.04 (0.40–2.68) | 0.934 |
| Confusion | 7/98 (7) | 5/105 (5) | 0.65 (0.20–2.12) | 0.475 |
| Cognitive and/or motor dysfunction | 5/98 (5) | 2/105 (2) | 0.36 (0.07–1.90) | 0.230 |
| Lymphadenopathy > 2 cm† | 15/97 (15) | 31/105 (29) | 2.29 (1.15–4.57) | 0.019 |
| Chest radiograph | ||||
| Interstitial syndrome | 35/92 (38) | 38/104 (36) | 0.94 (0.52–1.67) | 0.828 |
| Alveolar syndrome† | 30/92 (33) | 2/104 (2) | 0.04 (0.01–0.17) | < 0.001 |
| Pleural effusion† | 12/92 (13) | 1/104 (1) | 0.06 (0.01–0.51) | 0.009 |
| Pulmonary infiltrate† | 10/92 (11) | 1/104 (1) | 0.08 (0.01–0.63) | 0.017 |
| Chest CT scan | ||||
| Interstitial syndrome | 16/30 (53) | 2/11 (18) | 0.19 (0.04–1.06) | 0.058 |
| Alveolar syndrome | 11/30 (37) | 2/11 (18) | 0.38 (0.07–2.11) | 0.270 |
| Pleural effusion | 6/30 (20) | 1/11 (9) | 0.40 (0.04–3.76) | 0.423 |
| Mediastinal adenopathy | 16/30 (53) | 4/11 (36) | 0.50 (0.12–2.07) | 0.340 |
| Abdominal ultrasonography | ||||
| Hepatomegaly | 14/58 (24) | 20/34 (59) | 4.49 (1.81–11.15) | 0.001 |
| Splenomegaly | 4/58 (7) | 12/34 (35) | 7.36 (2.14–25.33) | 0.002 |
| Adenopathy | 19/58 (33) | 12/34 (35) | 1.12 (0.46–2.73) | 0.804 |
| Ascitis | 2/58 (3) | 1/34 (3) | 0.85 (0.07–9.72) | 0.895 |
| Abdominal CT scan | ||||
| Hepatomegaly | 3/15 (20) | 2/6 (33) | 2.00 (0.24–16.61) | 0.521 |
| Splenomegaly | 2/15 (13) | 1/6 (17) | 1.30 (0.09–17.73) | 0.844 |
| Adenopathy | 7/15 (47) | 3/6 (50) | 1.14 (0.17–7.60) | 0.890 |
| Standard biology | ||||
| CD4 cell count < 60 cells/mm3† | 30/95 (32) | 71/105 (68) | 4.52 (2.49–8.20) | < 0.001 |
| CD8 cell count < 650 cells/mm3† | 34/93 (37) | 58/98 (59) | 2.52 (1.40–4.51) | 0.002 |
| Hemoglobin level < 9 g/dL† | 41/97 (42) | 63/105 (60) | 2.05 (1.17–3.59) | 0.012 |
| Neutrophil count < 2,750 cells/mm3† | 22/92 (24) | 75/102 (74) | 8.84 (4.61–16.94) | < 0.001 |
| Platelet count < 150,000/mm3† | 9/96 (9) | 45/104 (43) | 7.37 (3.35–16.22) | < 0.001 |
| Creatinine level > 132.74 μmol/L† | 8/95 (8) | 15/101 (15) | 1.90 (0.76–4.70) | 0.167 |
| Protein level > 83 g/L | 33/91 (36) | 14/35 (40) | 1.17 (0.53–2.61) | 0.698 |
| Albumin level < 35 g/L | 4/6 (67) | 14/15 (93) | 7.00 (0.50–98.60) | 0.149 |
| AST level > 34 IU/L† | 43/96 (45) | 79/103 (77) | 4.06 (2.21–7.46) | < 0.001 |
| ALT level > 44 IU/L† | 15/96 (16) | 30/102 (29) | 2.25 (1.12–4.51) | 0.022 |
| γ-Glutamyl transferase level > 72 IU/L† | 37/94 (39) | 64/102 (63) | 2.59 (1.46–4.62) | 0.001 |
| Alkaline phosphatase level > 100 IU/L† | 39/95 (41) | 64/103 (62) | 2.36 (1.33–4.17) | 0.003 |
| Lactate dehydrogenase level > 385 IU/L† | 32/80 (40) | 55/96 (57) | 2.01 (1.10–3.68) | 0.023 |
| C-reactive protein level > 70 mg/L† | 52/90 (58) | 43/99 (43) | 0.56 (0.31–1.00) | 0.050 |
| Serum iron level < 9 μg/L | 27/33 (82) | 19/25 (76) | 0.70 (0.20–2.52) | 0.589 |
| Ferritin level > 1,000 μg/L | 11/39 (28) | 22/31 (71) | 6.22 (2.19–17.66) | 0.001 |
| Triglyceride level > 1.72 mmol/L | 7/37 (19) | 11/21 (52) | 4.71 (1.44–15.46) | 0.010 |
| Fibrinogen level > 4.2 g/L | 12/21 (57) | 4/20 (20) | 0.19 (0·05–0.76) | 0.019 |
| Prothrombin ratio < 70% | 20/55 (36) | 15/30 (50) | 1.75 (0.71–4.31) | 0.224 |
OR = odds ratio; CI = confidence interval; AIDS = acquired immunodeficiency syndrome; WHO = World Health Organization; CT = computed tomography; AST = aspartate aminotransferase; ALT = alanine aminotransferase. Bivariate analysis was conducted by using a logistic regression model.
Variables selected for the multivariate analysis model.
Dummy variables were created for the geographic origin and the residence location with Haiti and the Cayenne urban community as the respective referent population coded as 1.
Threshold of 18 years corresponds to the median.
The proportion of patients from Guyana and Brazil was greater for those with tuberculosis than for those with histoplasmosis. The proportion of patients originating from French Guiana and Suriname was significantly greater for those with histoplasmosis than for those with tuberculosis. Similarly, the proportion of patients having spent > 18 years in French Guiana was greater for persons with histoplasmosis than for those with tuberculosis. The proportion of patients residing outside the Cayenne urban community (residing mostly in western French Guiana along the Maroni River) was significantly greater for person with histoplasmosis than for those with tuberculosis. More specifically, patients residing along the Maroni River represented 17% of persons with histoplasmosis and 7% of those with tuberculosis (P = 0.047).
Tuberculosis and histoplasmosis were AIDS-defining events for most persons. The proportion of persons receiving antiretroviral treatment and/or taking trimethoprim-sulfamethoxazole primary prophylaxis on admission was low in both groups. A history of opportunistic infections was in similar proportions in both groups. A major proportion of patients were febrile on admission in both groups. Dyspnea, abdominal pain, diarrhea, and neurologic signs were frequent in both groups, but there was no significant difference.
The presence of concomitant opportunistic infections was more frequent in persons with histoplasmosis than in those with tuberculosis. Tobacco addiction was more frequent in persons with tuberculosis than in those with histoplasmosis. Similarly, multiple addictions were significantly more frequent in persons with tuberculosis than in those with histoplasmosis.
The proportion of patients with a Eastern Cooperative Oncology Group/World Health Organization performance status score > 2 was significantly greater for persons with histoplasmosis than for those with tuberculosis. Although most patients were febrile at admission, the mean ± SD temperature was significantly higher for person with histoplasmosis (39.5 ± 0.9°C) than for persons with tuberculosis (39.0 ± 1.0°C) (P = 0.021). The median (interquartile range [IQR]) evolution duration of fever was 30 (8–60) days for persons with tuberculosis and 21 (10–30) days for persons with histoplasmosis (P = 0.390). The proportion of persons with a systolic blood pressure < 90 mm Hg and a diastolic blood pressure < 60 mm Hg was significantly higher in persons with histoplasmosis than in those with tuberculosis.
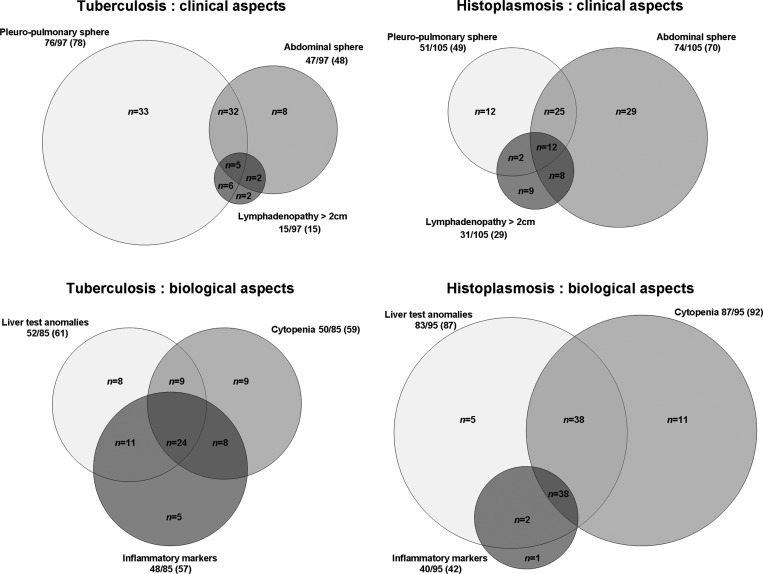
Initial physical examination showed that symptoms involving the pleuro-pulmonary sphere were more frequent in those with tuberculosis (78%) than in those with histoplasmosis (49%) (P < 0.001) (Figure 1). The proportion of patients with cough and/or chest pain was higher in persons with tuberculosis than in those with histoplasmosis. Symptoms involving the abdominal sphere were more frequent in persons with histoplasmosis (70%) than in those with tuberculosis (48%) (P = 0.001) (Figure 1). Hepatomegaly and/or splenomegaly was significantly more frequent in persons with histoplasmosis than in those with tuberculosis. Lymphadenopathy > 2 cm was greater in persons with histoplasmosis (29%) than in those with tuberculosis (15%) (Figure 1).
Figure 1.
Comparison of clinical and biological aspects of tuberculosis and histoplasmosis, French Guiana. Circles indicate no. positive patients/no. tested (%). The scale used proportions to avoid distortion of data. Circles intersections indicate n, which corresponded to the number of patients concerned. Because of missing values, the total for each group is different from the 99 patients with tuberculosis and the 106 patients with histoplasmosis. Anomalous liver test results were defined by an aspartate aminotransferase level > 34 IU/L, an alanine aminotransferase level > 44 IU/L, a γ-glutamyl transferase level > 72 IU/L, or an alkaline phosphatase level > 100 IU/L. Cytopenia was defined by a hemoglobin level < 9 g/dL, a neutrophil count < 2,750 cells/mm3, or a platelet count < 150,000/mm3. Inflammatory markers were defined by a C-reactive protein level > 70 mg/L.
Chest radiographs showed an interstitial syndrome that was comparable in both groups. The proportion of patients with deep lymphadenopathy and/or ascitis was also similar in both groups. Chest radiographs also showed that an alveolar syndrome and/or pleural effusions and/or pulmonary infiltrates were greater in persons with tuberculosis than in those with histoplasmosis. Abdominal ultrasonography showed that hepatomegaly and/or splenomegaly were greater in persons with histoplasmosis than in those with tuberculosis.
Blood counts showed that the median CD4 cell count was low in both groups (111 cells/mm3, IQR = 48–259 for persons with tuberculosis and 37/mm3, IQR = 15–84 for persons with histoplasmosis). The average hemoglobin level was decreased in both groups. There was no significant difference in prothrombin rate for both groups.
Immunosuppression was more advanced for persons with histoplasmosis than for those with tuberculosis. Anemia (hemoglobin level < 9 g/dL) was significantly more pronounced for persons with histoplasmosis than for those with tuberculosis. Neutrophil count was significantly lower in persons with histoplasmosis than in those with tuberculosis. Thrombocytopenia (platelet count < 150,000/mm) was more frequent in persons with histoplasmosis than in those with tuberculosis (Figure 1). The proportion of patients with fibrinogenemia > 4.2 g/L (laboratory threshold) was significantly higher for persons with tuberculosis than for those with histoplasmosis.
Median levels of lactate dehydrogenase (LDH) were increased in both groups (328 IU/L, IQR = 231–491 for persons with tuberculosis and 446 IU/L, IQR = 316–1,216 for those with histoplasmosis). Renal failure or hypoalbuminemia was observed in both groups.
Abnormal liver test results were more frequent in persons with histoplasmosis than in those with tuberculosis (Figure 1). Hepatic cytolysis (aspartate aminotransferase levels > 34 IU/L and alanine aminotransferase levels > 44 IU/L) and cholestasis (γ-glutamyl transferase levels > 72 IU/L and alkaline phosphatase levels > 100 IU/L) were significantly more frequent in persons with histoplasmosis. Lactate dehydrogenase levels > 365 IU/L were more frequent in persons with histoplasmosis (57%) than in those with tuberculosis (40%). C-reactive protein levels > 70 mg/L were more frequent in persons with tuberculosis than in those with histoplasmosis (Figure 1). Ferritinemia > 1,000 μg/L and/or triglyceridemia >1.72 mmol/L (laboratory threshold) were significantly more frequent in persons with histoplasmosis than in those with tuberculosis.
Lymph node localizations of microorganisms were similar in both groups (18% for persons with tuberculosis and 20% for those with histoplasmosis). Isolates from pleural and pulmonary localizations were more frequent in persons with tuberculosis than in those with histoplasmosis. Isolates from localizations, such as bone marrow, liver, gastrointestinal tract and peripheric blood, were significantly more frequent in persons with histoplasmosis than in those with tuberculosis.
A subgroup of patients who did not have concomitant opportunistic infections was analyzed separately to verify that the results were not affected by concurrent opportunistic infections. There were 91 cases of tuberculosis and 80 cases of histoplasmosis. Replication of the above analyses in this subgroup showed identical differences, suggesting that concomitant infections did not confound the above results.
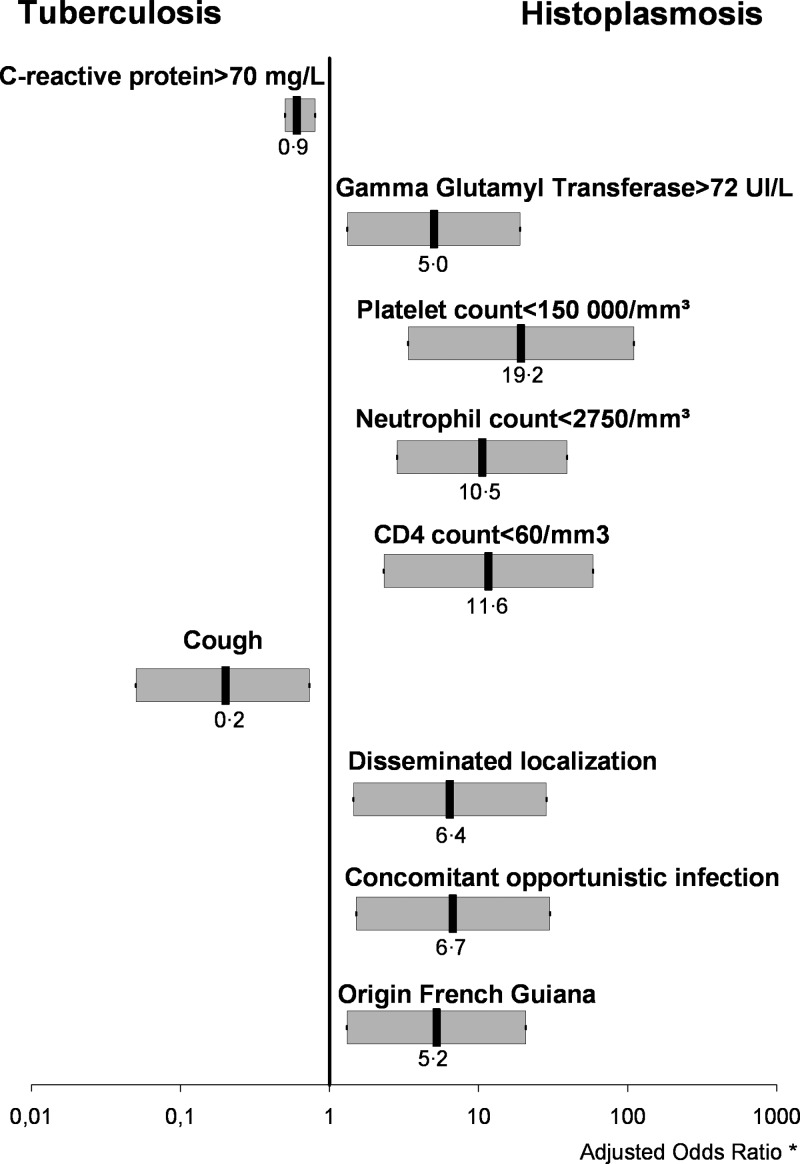
Multivariate analysis.
Forward and backward stepwise logistic regression converged on identical models. Results from multivariate analysis are shown in Table 2 and significant results according to the forward model are shown in Figure 2.
Table 2.
Multivariate analysis of tuberculosis and histoplasmosis in 205 human immunodeficiency virus–infected patients, French Guiana*
| Variable | AOR (95% CI) | P |
|---|---|---|
| Geographic origin† | ||
| French Guiana | 5.20 (1.30–20.73) | 0.020 |
| Opportunistic infection | ||
| Concomitant | 6.71 (1.50–29.96) | 0.013 |
| Isolate localization | ||
| Disseminated | 6.40 (1.44–28.45) | 0.015 |
| Physical condition on admission | ||
| WHO performance status score > 2 | 0.29 (0.07–1.24) | 0.095 |
| Physical examination | ||
| Cough | 0.20 (0.05–0.73) | 0.015 |
| Lymphadenopathy > 2 cm | 2.89 (0.64–12.95) | 0.166 |
| Standard biology | ||
| CD4 cell count < 60 cells/mm3 | 11.62 (2.30–58.63) | 0.003 |
| CD8 cell count < 650 cells/mm3 | 0.31 (0.08–1.29) | 0.107 |
| Neutrophil count < 2,750 cells/mm3 | 10.54 (2.83–39.24) | < 0.001 |
| Platelet count < 150,000/mm3 | 19.20 (3.35–110.14) | 0.001 |
| γ-glutamyl transferase level > 72 IU/L | 4.99 (1.31–18.99) | 0.018 |
| C-reactive protein level > 70 mg/L | 0.98 (0.97–0.99) | 0.008 |
AOR = adjusted odds ratio; CI = confidence interval; WHO = World Health Organization. Multivariate analysis was conducted by using a forward stepwise unconditional logistic regression model.
A dummy variable was created for the geographic origin with Haiti as the respective referent population coded as 1.
Figure 2.
Comparison of significant results (P < 0.05) in multivariate analysis for tuberculosis and histoplasmosis, French Guiana. Adjusted odds ratios and 95% confidence intervals (horizontal gray bars) are indicated on a logarithmic scale.
Variables significantly associated with tuberculosis were cough and a C-reactive protein level > 70 mg/L. Variables significantly associated with histoplasmosis were γ-glutamyl transferase level > 72 IU/L, origin from French Guiana, disseminated localizations, concomitant opportunistic infections, neutrophil count < 2,750 cells/mm3, CD4 cell count <60 cells/mm3, and platelet count < 150,000/mm3.
Discussion
Tuberculosis and histoplasmosis have similar symptoms.8,21,22 This study tested whether histoplasmosis and tuberculosis are indiscernible in HIV-infected patients. Although these pathologies share certain similarities, there are clinical and laboratory differences. Tuberculosis was more frequent among patients from Guyana and Brazil, and histoplasmosis was more frequent among patients from French Guiana and Suriname. Residence duration in French Guiana and residence location outside urban was more frequent in persons with histoplasmosis. Thus, tuberculosis seemed to be an urban pathology and histoplasmosis seemed more to be a rural pathology, notably near the Maroni River.
Most patients did not take any treatment (antiretroviral or primary prophylaxis) at the time of diagnosis. It was therefore not surprising to observe concurrent opportunistic infections, notably in patients with histoplasmosis.
The initial clinical presentation in both groups was dominated by prolonged fever in a context of poor general condition, notably weight loss. However, this condition was more pronounced in persons with histoplasmosis.
Symptoms involving the pleuro-pulmonary sphere were more frequent in persons with tuberculosis, and M. tuberculosis was more frequently identified at the pleuro-pulmonary level (Figure 1). Similarly, cough or chest pain associated with abnormal chest radiograph results were more frequent in persons with tuberculosis. Although an interstitial syndrome was observed in both groups, alveolar syndrome and pulmonary infiltrate were more evocative of tuberculosis.
Conversely, symptoms or abnormal medical imagery results involving the abdominal sphere were more frequent in persons with histoplasmosis. Histoplasma capsulatum was identified more frequently at the abdominal level (liver and gastrointestinal tract). Hepatomegaly, splenomegaly, and lower digestive bleeding associated with abnormal abdominal ultrasonographic results were more frequent in persons with histoplasmosis. Although the presence of deep lymphadenopathy was similar in both groups, hepatomegaly or splenomegaly were more frequent in persons with histoplasmosis. Lymph node localizations were frequently observed in both groups, but lymphadenopathy > 2 cm seemed more evocative of histoplasmosis. Most cases of histoplasmosis were disseminated forms, presumably because of greater immunodepression than in tuberculosis cases, facilitating dissemination of the pathogen.
Results of standard biologic tests showed numerous differences. Although anemia was common in both groups, it was more frequent in persons with histoplasmosis. It was generally part of pancytopenia, which was also significantly more frequent in persons with histoplasmosis. Moreover, abnormal liver test results (hepatic cytolysis and cholestasis), increased LDH levels, and hypertriglyceridemia were more frequent in persons with histoplasmosis than in those with tuberculosis. Conversely and independent of CD4 cell counts, inflammatory markers were more frequent in persons with tuberculosis than in those with histoplasmosis (increased levels of C-reactive protein and fibrinogen), but ferritinemia (ferritin concentration > 1,000 μg/L) was more frequent in persons with histoplasmosis.
Increased LDH levels have been reported as an indicator for diagnosis of tuberculosis and histoplasmosis16,23,24 and as a prognostic factor in severe disseminated forms of histoplasmosis.6 In the present study, after adjusting for CD4 cell counts, we found no significant difference in LDH levels between persons with tuberculosis and those with histoplasmosis. Thus, increased LDH levels could not discriminate tuberculosis from histoplasmosis.
Ferritin concentration has also been described as an indicator for the diagnosis of severe disseminated histoplasmosis.25 However, because of a large number of missing values, this variable was not selected for multivariate analysis.
This study had limitations. Data were collected retrospectively, which might have led to selection biases. Missing values for certain variables that were not included in the regression model may not have been missing randomly and were most likely influenced by clinical experience of the physicians. Histoplasmosis and tuberculosis represent only 50% of AIDS-defining illnesses in French Guiana, a finding that does not enable definition of decisional algorithms adapted to clinical situations.
Despite its limitations, this study is the first to compare tuberculosis and histoplasmosis among HIV-positive patients. A study reported excessive mortality in patients receiving antituberculosis treatment because of lack of knowledge about histoplasmosis or diagnostic difficulties.10 Thus, not knowing the differences between tuberculosis and histoplasmosis is a serious concern because it should strongly encourage clinicians in disease-endemic areas to conduct invasive diagnostic procedures or initiate presumptive treatment, notably in the presence of severity criteria.16,26
Nevertheless, in addition to a high clinical suspicion index, there is a need for an affordable, specific, sensitive, user friendly, robust, rapid, equipment free, and deliverable diagnostic tool to help clinicians in low-resource countries diagnose histoplasmosis.
The question initiating this study was whether tuberculosis and histoplasmosis in HIV-infected patients are clinically similar. The answer to this question is no. Although tuberculosis and histoplasmosis have similarities, a certain number of particularities described in this report can aid therapeutic decisions by clinicians, notably when a short-term prognosis is at risk.
Footnotes
Financial support: This study was supported by the grant Investissement d'Avenir from the Agence Nationale de la Recherche (CEBA reference no. ANR-10-LABX-0025).
Authors' addresses: Antoine Adenis, Mathieu Nacher, Matthieu Hanf, and Célia Basurko, Centre d'Investigation Clinique Epidémiologie Clinique Antilles-Guyane, INSERM CIE 802, Centre Hospitalier de Cayenne, Cayenne, French Guiana, and Equipe EA3593, Epidémiologie des Parasitoses et des Mycoses Tropicales, Université des Antilles et de la Guyane, Cayenne, French Guiana, E-mails: antoine.adenis@gmail.com, mathieu.nacher@ch-cayenne.fr, matthieu.hanf@ch-cayenne.fr, and c.basurko@free.fr. Julie Dufour and Florence Huber, Equipe EA3593, Epidémiologie des Parasitoses et des Mycoses Tropicales, Université des Antilles et de la Guyane, Cayenne, French Guiana, and Service de Dermatologie Vénérologie, Centre Hospitalier de Cayenne, Cayenne, French Guiana, E-mails: dufour-julie@orange.fr and flottehuber@yahoo.fr. Christine Aznar, Equipe EA3593, Epidémiologie des Parasitoses et des Mycoses Tropicales, Université des Antilles et de la Guyane, Cayenne, French Guiana, and Laboratoire Hospitalo-Universitaire de Parasitologie-Mycologie, Centre Hospitalier de Cayenne, Cayenne, French Guiana, E-mail: christine.aznar1@wanadoo.fr. Bernard Carme, Centre d'Investigation Clinique Epidémiologie Clinique Antilles-Guyane, INSERM CIE 802, et Laboratoire Hospitalo-Universitaire de Parasitologie-Mycologie, Centre Hospitalier de Cayenne, Cayenne, French Guiana, and et Equipe EA3593, Epidémiologie des Parasitoses et des Mycoses Tropicales, Université des Antilles et de la Guyane, Cayenne, French Guiana, E-mail: bernard.carme@ch-cayenne.fr. Pierre Couppie, Equipe EA3593, Epidémiologie des Parasitoses et des Mycoses Tropicales, Université des Antilles et de la Guyane, Cayenne, French Guiana, and et Service de Dermatologie Vénérologie, Centre Hospitalier de Cayenne, Cayenne, French Guiana, E-mail: couppie.pierre@voila.fr.
References
- 1.Nacher M, El Guedj M, Vaz T, Nasser V, Randrianjohany A, Alvarez F, Sobesky M, Magnien C, Couppié P. Risk factors for late HIV diagnosis in French Guiana. AIDS. 2005;19:727–729. doi: 10.1097/01.aids.0000166096.69811.b7. [DOI] [PubMed] [Google Scholar]
- 2.Lewden C, Sobesky M, Cabié A, Couppié P, Boulard F, Bissuel F, May T, Morlat P, Chêne G, Lamaury I, Salmon D. Group d'Étude Mortalité 2000 Causes of death among HIV infected adults in French Guyana and the French West Indies in the era of highly active antiretroviral therapy (HAART [in French] Med Mal Infect. 2004;34:286–292. [PubMed] [Google Scholar]
- 3.Nacher M, Aznar C, Blanchet D, Demar M, El Guedy M, Vaz T, Clyti E, Carme B, Couppié P. AIDS-related disseminated histoplasmosis in the greater Caribbean: how frequent is it? AIDS. 2006;20:951–952. doi: 10.1097/01.aids.0000218568.43391.78. [DOI] [PubMed] [Google Scholar]
- 4.Wheat LJ, Connolly-Stringfield PA, Baker RL, Curfman MF, Eads ME, Israel KS, Norris SA, Webb DH, Zeckel ML. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore) 1990;69:361–374. doi: 10.1097/00005792-199011000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Jones BE, Young SM, Antoniskis D, Davidson PT, Kramer F, Barnes PF. Relationship of the manifestations of tuberculosis to CD4 cell counts in patients with human immunodeficiency virus infection. Am Rev Respir Dis. 1993;148:1292–1297. doi: 10.1164/ajrccm/148.5.1292. [DOI] [PubMed] [Google Scholar]
- 6.Couppié P, Aznar C, Carme B, Nacher M. American histoplasmosis in developing countries with a special focus on patients with HIV: diagnosis, treatment, and prognosis. Curr Opin Infect Dis. 2006;19:443–449. doi: 10.1097/01.qco.0000244049.15888.b9. [DOI] [PubMed] [Google Scholar]
- 7.Chan KS, Looi LM, Chan SP. Disseminated histoplasmosis mimicking miliary tuberculosis: a case report. Malays J Pathol. 1993;15:155–158. [PubMed] [Google Scholar]
- 8.Tong P, Tan WC, Pang M. Sporadic disseminated histoplasmosis simulating miliary tuberculosis. Br Med J (Clin Res Ed) 1983;287:822–823. doi: 10.1136/bmj.287.6395.822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greene L, Peters B, Lucas SB, Pozniak AL. Extrapulmonary tuberculosis masking disseminated histoplasmosis in AIDS. Sex Transm Infect. 2000;76:54–56. doi: 10.1136/sti.76.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bulmer AC, Bulmer GS. Incidence of histoplasmin hypersensitivity in the Philippines. Mycopathologia. 2001;149:69–71. doi: 10.1023/a:1007277602576. [DOI] [PubMed] [Google Scholar]
- 11.Rezende RE, Brunaldi MO, Girão MS, Zucoloto S, Garcia SB, Machado AA, Módena JL. Case report: esophageal histoplasmosis associated with disseminated tuberculosis in acquired immunodeficiency syndrome. Am J Trop Med Hyg. 2009;80:347–350. [PubMed] [Google Scholar]
- 12.Hay RJ, White HS, Fields PE, Quamina DB, Dan M, Jones TR. Histoplasmosis in the eastern Caribbean: a preliminary survey of the incidence of the infection. J Trop Med Hyg. 1981;84:9–12. [PubMed] [Google Scholar]
- 13.Floch H. Histoplasmosis in French Guiana [in French] Ann Parasitol Hum Comp. 1953;28:108–125. [PubMed] [Google Scholar]
- 14.Eza D, Cerrillo G, Moore DA, Castro C, Ticona E, Morales D, Cabanillas J, Barrantes F, Alfaro A, Benavides A, Rafael A, Valladares G, Arevalo F, Evans CA, Gilman RH. Postmortem findings and opportunistic infections in HIV-positive patients from a public hospital in Peru. Pathol Res Pract. 2006;202:767–775. doi: 10.1016/j.prp.2006.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Souza SL, Feitoza PV, Araújo JR, Andrade RV, Ferreira LC. Causes of death among patients with acquired immunodeficiency syndrome autopsied at the Tropical Medicine Foundation of Amazonas [in Portuguese] Rev Soc Bras Med Trop. 2008;41:247–251. doi: 10.1590/s0037-86822008000300005. [DOI] [PubMed] [Google Scholar]
- 16.Huber F, Nacher M, Aznar C, Pierre-Damar M, El Guedj M, Vaz T, Vantilcke V, Mahamat A, Magnien C, Chauvet C, Carme A, Couppié P. AIDS-related Histoplasma capsulatum var. capsulatum infection: 25 years experience of French Guiana. AIDS. 2008;22:1047–1053. doi: 10.1097/QAD.0b013e3282ffde67. [DOI] [PubMed] [Google Scholar]
- 17.Darling ST. A protozoon general infection producing pseudotubercles in the lungs and focal necrosis in the liver, spleen and lymph nodes. JAMA. 1906;46:1283–1285. [Google Scholar]
- 18.Oken MM, Creech RH, Tormey DC, Horton J, Davies TE, McFAdden ET, Carbone RP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–655. [PubMed] [Google Scholar]
- 19.StataCorp . Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- 20.Hosmer DW, Jr, Wang CY, Lin IC, Lemeshow S. A computer program for stepwise logistic regression using maximum likelihood estimation. Comput Programs Biomed. 1978;8:121–134. doi: 10.1016/0010-468x(78)90047-8. [DOI] [PubMed] [Google Scholar]
- 21.Walls K, Furcolow ML, Lehan PH. Histoplasmosis as a problem in tuberculosis sanatoriums throughout the United States. J Lab Clin Med. 1958;51:266–270. [PubMed] [Google Scholar]
- 22.Furcolow ML, Brasher CA. Chronic progressive (cavitary) histoplasmosis as a problem in tuberculosis sanatoriums. Am Rev Tuberc. 1956;73:609–619. doi: 10.1164/artpd.1956.73.5.609. [DOI] [PubMed] [Google Scholar]
- 23.Corcoran GR, Al-Abdely H, Flanders CD, Geimer J, Patterson TF. Markedly elevated serum lactate dehydrogenase levels are a clue to the diagnosis of disseminated histoplasmosis in patients with AIDS. Clin Infect Dis. 1997;24:942–944. doi: 10.1093/clinids/24.5.942. [DOI] [PubMed] [Google Scholar]
- 24.Dos Santos RP, Scheid KL, Goldani LZ. Laboratory features for presumptive diagnosis of disseminated tuberculosis in HIV-infected patients. Int J Tuberc Lung Dis. 2008;12:1340–1343. [PubMed] [Google Scholar]
- 25.Guturu P, Sarria JC. Extreme hyperferritenemia in an AIDS patient with disseminated histoplasmosis. J Infect. 2008;57:356–357. doi: 10.1016/j.jinf.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Couppié P, Sobesky M, Aznar C, Bichat S, Clyti E, Bissuel F, El Guedj M, Alvarez F, Demar M, Louvel D, Pradinaud R, Carme B. Histoplasmosis and acquired immunodeficiency syndrome: a study of prognostic factors. Clin Infect Dis. 2004;38:134–138. doi: 10.1086/379770. [DOI] [PubMed] [Google Scholar]