Abstract
Objective
To describe the results of different measures implemented to improve compliance with the healthcare worker (HCW) influenza immunization program at BJC HealthCare between 1997 and 2007.
Design
Descriptive retrospective study.
Setting
BJC HealthCare, a 13-hospital nonprofit healthcare organization in the Midwest.
Methods
Review and analysis of HCW influenza vaccination data from all BJC HealthCare Occupational Health Services and hospitals between 1997 and 2007. Occupational health staff, infection prevention personnel and key influenza vaccine campaign leaders were also interviewed regarding implementation measures during the study years.
Results
At the end of 2007, BJC HealthCare had approximately 26,000 employees. Using multiple progressive interventions, influenza vaccination rates among BJC employees increased from 45% in 1997 to 71.9% in 2007 (p<0.001). The influenza vaccination rate in 2007 was significantly higher than in 2006, 71.9% versus 54.2% (p<0.001). Five hospitals had influenza vaccination rates over the target goal of 80% in 2007. The most successful interventions were adding influenza vaccination rates to the incented quality scorecard and declination statements, both implemented in 2007. The most important barriers identified in the interviews related to HCWs’ misconceptions about influenza vaccination and a perceived lack of leadership support.
Conclusions
Influenza vaccination rates in HCWs significantly improved with multiple interventions over the years. However, the BJC HealthCare influenza vaccination target of 80% was not attained at all hospitals with these measures. More aggressive interventions such as implementing mandatory influenza vaccination policies are needed to achieve higher vaccination rates.
BACKGROUND
Influenza is a serious viral respiratory illness that causes annual epidemics worldwide, resulting in more than 200,000 hospitalizations and 36,000 deaths per year in the United States.1, 2 The economic impact of influenza has been estimated to range between three and $10.4 billion in annual direct costs.3, 4 Some populations, such as the elderly, inmunocompromised, critically ill patients and young children are at particular risk of influenza complications, especially in healthcare-settings. 2, 5, 6 Multiple studies have shown that infected healthcare workers, both symptomatic and asymptomatic, can transmit influenza to their vulnerable patients. Health care associated influenza outbreaks are well documented.5, 7–11
Influenza vaccination of healthcare workers (HCWs) has been shown to reduce transmission of influenza in health care settings, reduce employee illness and absenteeism, and decrease influenza-related morbidity and mortality among persons at increased risk for complications during influenza season.12–18 Although this evidence primarily comes from long-term care facilities, transmission of influenza from HCWs to patients can also occur in acute care facilities. Thus, influenza immunization of HCWs would be expected to significantly reduce the risk in acute care settings as well.
Current guidelines from the Healthcare Infection Control Practices Advisory Committee (HICPAC), the Advisory Committee on Immunization Practices (ACIP), the Society of Healthcare Epidemiology of America (SHEA) and other professional organizations strongly recommend annual influenza vaccination of HCWs.7, 19, 20 One of the U.S. National Health objectives for 2010 is to achieve HCW vaccination coverage levels of 60 %. Despite these recommendations, HCW influenza vaccination rates reported from different institutions remain low, with a national average of about 40%.7, 21, 22 Different measures to improve influenza vaccination rates in HCWs have been proposed and evaluated.7, 23 These measures include offering free influenza vaccination at convenient work sites, providing HCWs with education regarding the benefits and potential health consequences of influenza illness, providing modeling and support for influenza vaccination by institutional leaders and requiring signed declination statements from those refusing influenza vaccination. These initiatives have been demonstrated to moderately increase influenza vaccination acceptance.7, 24–30
Some influenza vaccine interventions in past studies have been bundled making it difficult to evaluate the impact of each aspect of the intervention. In one study 26 providing vaccine in locations and at times easily accessible by HCWs (mobile carts) significantly improved influenza vaccine acceptance from 44% to 66%. Providing education about influenza immunization substantially increased influenza vaccination coverage from 45% to 60% in one study.26 Modeling by leadership was reported to significantly increase influenza vaccination rates among employees.29 Polgreen et al recently reported a mean increase of 11.6% in influenza vaccination rates using declination statements.30
BJC HealthCare has had a comprehensive HCW influenza vaccination program since 1997 in order to increase annual vaccination rates. In 2007, a target goal of > 80% employee influenza vaccination coverage was set. This manuscript describes the results of different measures implemented by BJC HealthCare to improve compliance with their employee influenza immunization program between 1997 and 2007.
METHODS
Design
Aggregated data collected from the BJC Occupational Health Services database records between 1997 and 2007, and a structured interview of the key leaders and key participants of the annual employee influenza vaccination campaigns were used to evaluate the employee influenza vaccination program. The interview contained nine open-ended questions to assess each individual’s perspective regarding successful interventions and barriers to improving influenza vaccination rates. The data were reviewed for the baseline period from 1997 to 2000, and for two intervention periods: 2000–2004, and 2005–2007. During these two intervention periods additional influenza campaign initiatives were implemented to improve vaccination rates.
Setting
BJC HealthCare is one of the largest nonprofit healthcare organizations in the Midwestern United States, delivering services to residents primarily in the greater St. Louis, southern Illinois and mid-Missouri regions. The organization includes 13 hospitals and more than 3200 staffed-beds. Two of the facilities are academic acute tertiary care hospitals affiliated with Washington University in St. Louis School of Medicine, one adult hospital with 1,252 staffed-beds, and one pediatric hospital with 250 staffed-beds. Four are large community hospitals and seven are small suburban or rural hospitals (each with fewer than 100 staffed-beds). Twelve of the current thirteen BJC HealthCare hospitals were included in the analysis. The thirteenth hospital is a small rural facility that is under a different management structure than all of the other facilities. This hospital did not participate fully in the influenza vaccination program and therefore was excluded. Data from BJC HealthCare associated extended care facilities and home health were also excluded. Extended care and home health were excluded from this analysis because their influenza vaccine record keeping was incomplete for all study years. All types of hospital employees defined as contracted personnel were included. The approximately 4,600 credentialed private physicians are offered free influenza vaccination but their vaccination rates were not tracked by BJC HealthCare because they are not hospital employees and so they were not included.
BJC HealthCare occupational health programs and procedures are standardized across the organization through the Council of Occupational Health Professionals. Each facility’s occupational health representative participates in bi-monthly meetings that include education and standardization of occupational health and safety surveillance and interventions. Each facility uses the BJC occupational health database computerized network to track employee vaccinations, injuries and exposures.
Statistical analysis
Influenza vaccination rates are expressed as the number of staff vaccinated per 100 employees. Vaccination rates were compared using the t Test for continuous variables. A p value <0.05 was considered statistically significant.
RESULTS
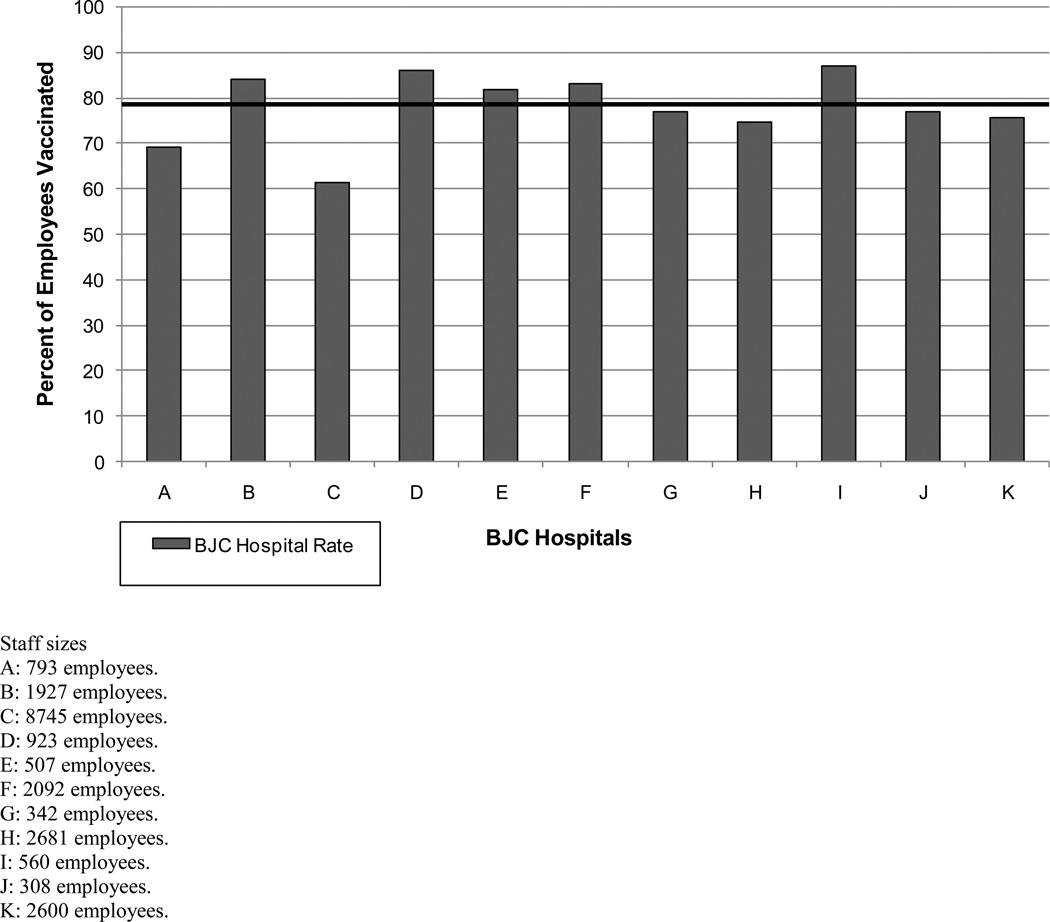
BJC HealthCare has historically provided influenza vaccine free to all BJC employees during annual campaigns as part of the occupational health and infection prevention policy. Influenza vaccination coverage data has been tracked since 1997. At the end of 2007, the organization had approximately 26,000 employees, including 900 physicians in training (fellows, residents and interns). The number of HCWs per hospital ranged between 308 and 8,745 employees (Figure 2).
Figure 2. Influenza vaccination rates by hospital for 11 hospitals in the BJC HealthCare system, 2007.
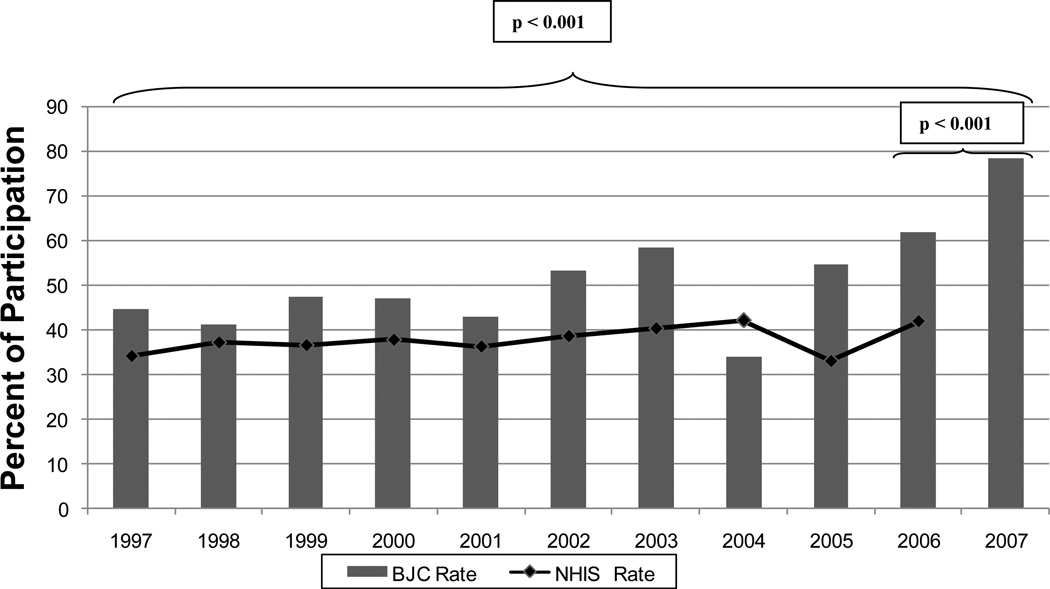
Figure 1 shows BJC HealthCare’s employee influenza vaccination rates between 1997 and 2007. In 1997, the rate was 45% compared with 71.9% in 2007 (p<0.001). The rate in 2007 was significantly higher than in 2006, 71.9% versus 54.2% (p<0.001). Each year, a target influenza vaccination rate was set by occupational health. The target goals of influenza vaccination coverage for all BJC HealthCare were incrementally increased each year ranging from 45% in 2002 to 80% in 2007. The target vaccination rate was only attained in 2002 with a mean influenza vaccination rate of 45.8%. However, the observed BJC employee vaccination rates were always above the National Health Interview Survey (NHIS) influenza vaccination rates31, except in 2004, which was the year of the influenza vaccine shortage. Five hospitals had influenza vaccination rates over 80% in 2007 (Figure 2). Three of the hospitals with > 80% employee influenza vaccination rates are small suburban or rural hospitals (each with fewer than 100 staffed-beds) and two are community hospitals (≤ 350 staffed-beds). The large, adult, teaching hospital influenza vaccination rate increased from 32% in 1997 to 61.5% in 2007 (p<0.001)
Figure 1. Employee influenza vaccination rates at BJC HealthCare, 1997 – 2007.
NHIS: National Health Interview Survey (Healthcare workers subgroup) 31 *Influenza vaccine shortage occurred in 2004.
Table 1 summarizes the interventions implemented to improve HCW’s influenza vaccination compliance through the years. Before 2000, influenza vaccination was given only at occupational health offices and leadership involvement only included the occupational health and infection prevention directors at each facility. Education consisted of lectures for house staff and posters in patient care areas. Email announcements were used as part of basic influenza vaccine marketing. No specific campaign themes were used. Between 2000 and 2004, BJC HealthCare increased its focus on making influenza vaccination more accessible to HCWs and on-site influenza vaccination was started. BJC HealthCare also began using standardized promotion materials for all hospitals, including more education and marketing activities, such as posters, communication forums, catchy slogans, emails and publishing employee influenza vaccination compliance results. Multiple incentives, including trinket incentives (pens, buttons and candy) and cash lotteries were also implemented during this timeframe by many of the individual hospitals.
Table 1.
Interventions Implemented to Improve Healthcare Worker Influenza Vaccination Rates at BJC Healthcare, 1997–2007
| Period | Policy | Access to vaccination | Education | Leadership involvement | Incentivesa | Marketing | Campaign Theme |
|---|---|---|---|---|---|---|---|
| Before 2000 baseline period | Free influenza vaccination for all BJC employees | OH office | Lectures for house staff, posters | IP director, OH director | Trinket incentives such as badge holders | E-mail announcements | None |
| 2000–2004 | Free influenza vaccination for all BJC employees, centralized promotion; 2003. Best Practiceb was developed 2004; influenza vaccine shortage, with vaccination based on priorities and LAIV availability | Focus on accessibility: onside vaccination | Posters and communication forums, announcements, BJC newspaper article | IP director, OH director, hospital epidemiologists | Pens, buttons, candy 2002 and 2003 cash incentives of up to $1,000 | Catchy slogans, posters, published results, e-mails | 2002–2003; “Flu Survivor” |
| 2005–2007 | Free influenza vaccination for all BJC employees; promotion at all organization levels; system comparative data to promote friendly competition; 2007: influenza vaccination rate included Best in Class scorecard; dedication statements LAIV offered | Vaccination given at multiple sites, at work site, cafeteria, halls; on multiple dates and times extra volunteer nurses giving shots, roving vaccination carts extended vaccination period to end of February | Additional influenza vaccine education: mailed and e-mailed letter, posters, lectures, BJC newspaper article | IP and OH directors, hospital epidemiologists, feed back to managers and senior hospital leadership | Pins, pens, magnets, key chains; raffle prizes; iPods, cash, gift baskets to shifts with best vaccination rates | Signs, posters; 2006: MBTV announcementsd 2007: photos of key leaders at each location receiving their vaccinations | 2005: “Flu Free at BJC” 2006: “Date to Care—Avoid the Flu” 2007: “Got My Shot” |
NOTE. OH, occupational health; IP, infection prevention; LAIV, live attenuated vaccine.
Incentives provided by BJC hospitals were different across the system during these 3 periods.
Best Practice is an OH policy outlining best practices for all BJC HealthCare facilities to maximize distribution of influenza vaccine.
“Best in Class” scorecard is a BJC HealthCare quality report that is used to provide leadership at each hospital with incentives based on reaching presstablished targets.
MBTV announcements are promotional messages displayed on television monitors in waiting rooms, hallways, and public areas.
In 2003, the BJC HealthCare influenza vaccination “Best Practice” policy was developed. The “Best Practice” influenza policy outlined the best practices for all BJC facilities to use in order to optimize the distribution of influenza vaccine. In 2004 there was an extreme influenza vaccine shortage, so that year influenza vaccination was focused only on high priority HCWs, i.e. those most likely to be exposed to influenza who were caring for the highest risk patients. The high priority group included physicians and nurses working in the emergency department, intensive care units, pediatric, obstetric, and medicine floors. Live attenuated intranasal vaccine was also made available to eligible HCWs.
Between 2005 and 2007, access to influenza vaccination was further enhanced by giving the vaccine at multiple worksites as well as in other high traffic locations, such as the cafeteria, hallways, at physician grand rounds and other clinical conferences. Influenza vaccine promotion was heightened at the organization and facility level using several new marketing strategies, including unique campaign themes and multiple incentives. Hospital vaccination rates were reported to all the BJC HealthCare hospitals to promote friendly competition between the facilities. Vaccine compliance data was provided to managers and administrators at each hospital. Senior leadership support for the influenza vaccination campaigns was also promoted.
In 2007, two additional important interventions were implemented. Declination statements were introduced for any employee refusing to be vaccinated and employee influenza vaccination rates were reported on the “Best in Class” (BIC) scorecard. Financial incentives for leadership at each hospital are based on metrics reported on the BJC HealthCare BIC scorecard. Leadership incentives are based on reaching pre-established scorecard targets. The influenza target was set at ≥ 80% vaccination rates for all facilities. In 2007, the overall influenza vaccination rate for BJC HealthCare was 71.9%, which was a 16.7% increase from 2006 (Figure 1). Implementing the declination and influenza vaccine reporting on the BIC scorecard required additional time and effort from occupational health, infection prevention and other nursing personnel working on the influenza campaigns. Those interviewed indicated that a significant amount of extra time and effort was spent on the influenza campaign in 2007 compared to earlier years, although there were no formal efforts to track the resources used for the influenza vaccination campaign over the study period. Collecting declination statements was noted to be particularly labor intensive.
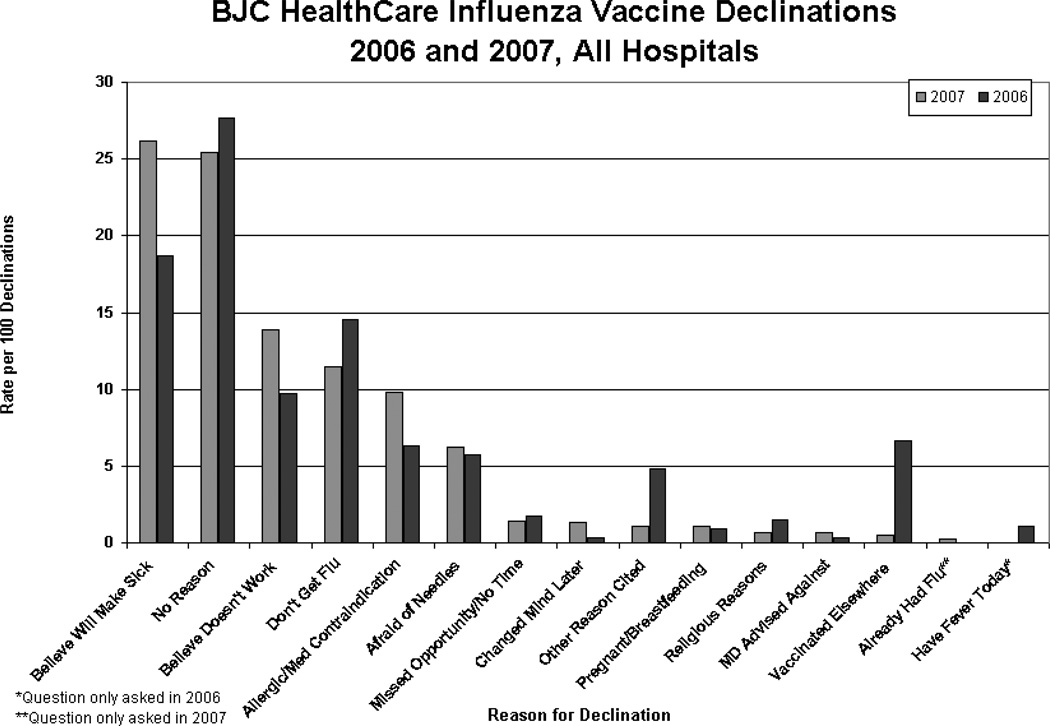
The reasons employees cited for declining influenza vaccination were tracked at all BJC HealthCare facilities in 2006 and 2007 (Figure 3). The most common reasons for declining vaccination were: “believe vaccine will make sick”, “no reason”, “believe vaccine does not work”, and “I do not get the flu”. “Religious reasons”, “medical doctor advised against”, and “already had flu” were occasionally given (<1%). Only 56% of unvaccinated HCWs actually signed a declination statement.
Figure 3. Reasons that employees declined influenza vaccination at BJC HealthCare facilities, 2006–2007.
Table 2 shows the results of the structured interviews about the successes and barriers of the influenza vaccination program. The most successful interventions identified were inclusion of the influenza vaccination rates on the BIC scorecard, acquiring leadership support, and use of declination statements. Barriers mentioned frequently in the interviews were HCWs’ misconceptions about influenza vaccine efficacy, benefits, and toxicity, and lack of leadership support.
Table 2.
Perceptions of interventions success and barriers to HCW influenza vaccination program identified from structured interviews.
| Successful interventions | Less successful interventions | Barriers |
|---|---|---|
| Free vaccine Professional marketing Roving vaccine carts Multiple dates and times for vaccination (vaccine readily available and easy to access at worksite) Including influenza vaccination in the Best in Class Scorecard* Competition between BJC facilities to achieve higher vaccination rates Any support by leadership Senior leadership support Declination statements |
Incentives, including prizes and cash Inconsistent follow up of non-compliant HCWs System level tokens and incentives Education |
HCW fears HCW misconceptions about influenza vaccine efficacy, benefits and toxicity Lack of knowledge regarding influenza consequences Variety of shifts, part- time personnel Tracking compliance data Time required Convenience of vaccine administration site Lack of leadership support |
Bold text shows perceptions mentioned by more than one interviewed participant.
Best in Class Scorecard is a BJC Healthcare quality scorecard that includes incentives for facilities that reach pre-established targets.
DISCUSSION
The principal finding of this study was the significant improvement in HCW influenza vaccination compliance in BJC HealthCare over the years with progressive implementation of multiple interventions. Despite numerous interventions, the 2007 goal of 80% vaccination compliance for all BJC HealthCare facilities was only reached by a few hospitals in the organization. The facilities achieving more than 80% vaccination rates are small rural or community hospitals with a limited number of employees (ranging between 308 and 2,092 persons). The relatively small number of employees at these hospitals undoubtedly facilitated the vaccination process and required fewer resources to achieve better vaccination coverage. The lowest vaccination compliance rate through the years occurred at the largest academic tertiary care hospital in the organization, which has more than 8,700 employees and only three occupational health nurses. However, this hospital vaccinated more than 5,300 employees in 2007. The actual number of employees vaccinated at the largest hospital was greater the number of employees vaccinated at the five smaller hospitals combined. Vaccinating large numbers of employees requires greater resources and time than vaccinating small number of employees.
The largest increase in influenza vaccination compliance was observed between 2006 and 2007. This increase coincided with the implementation of declination statements and the inclusion of employee influenza vaccination rates on the BJC HealthCare BIC scorecard. Both of these interventions were implemented in the same year, so it is difficult to distinguish the impact of each intervention separately. HCWs had to either get the influenza vaccine or sign a declination statement, however, there were no penalties for employees that did not comply and not all unvaccinated HCWs filled out a declination form. The observed increase in vaccination rates was higher than the mean increase reported by other authors with the introduction of declination statements 30, which may reflect the contribution of additional leadership support obtained because of the financial incentives established by reporting vaccination rates on the BJC HealthCare BIC scorecard.
The most frequently cited reasons for declining influenza vaccination were related to HCWs’ misconceptions and fears regarding influenza vaccine efficacy, benefits and toxicity. This finding was also identified in the key participant interviews and has been consistently reported by other authors.27, 32, 33 Unfortunately, it was not possible to completely reverse HCWs’ misconceptions despite substantial educational efforts. Education was perceived as a less successful intervention in the structured interviews, probably because provision of education did not always translate into vaccine acceptance. Some authors have reported that participation in structured in-service education or conferences was associated with improvement in vaccination rates. 24, 26, 28, 34, 35 Developing leadership support was perceived as a successful intervention in the structured interviews, and has been also associated with higher vaccine acceptance rates among staff members under their leadership in the literature.36–38
There are some limitations to this study. First, we were unable to obtain complete data before 2000. Some data were obtained from the structured interviews, which may not be completely accurate due to the subjective nature of this data, reliance on participants’ memory, and the potential for recall bias. We were unable to obtain specifics about employee job titles in different facilities and influenza vaccination compliance among students was not tracked. Regarding physician influenza vaccination rates, this study only includes physicians who were employed by BJC HealthCare, primarily residents and fellows. Physicians in private practice or employed by Washington University in St. Louis were not officially tracked by BJC Occupational Health Services. The generalizability of these findings may be limited considering the complexity of this healthcare organization, the extent of leadership support and occupational health and infection prevention resources.
Despite significant improvement in influenza vaccination compliance among HCWs due to multiple interventions implemented over the years, the BJC HealthCare influenza vaccination target of 80% was not fully achieved. New interventions are needed to achieve higher vaccination rates. Mandatory influenza vaccination including penalties for non-compliance has been recommended by some experts as a logical step to ensure high HCW vaccination rates and protect patients from influenza. A recent survey of nurses from Mayo Clinic, reported that 56% of the responders stated that mandatory influenza vaccination was appropriate for HCWs.39 Virginia Mason Medical Center in Seattle, Washington reported a 98.5% overall influenza immunization rate among employees using mandatory influenza vaccination (P. Crome, personal communication, March 2007). Because BJC HealthCare vaccination compliance goals were not met in 2007 despite significant efforts, and because influenza vaccination of HCWs was viewed as an important patient safety issue, BJC HealthCare implemented mandatory influenza vaccination for employees in 2008. The initial results of the mandatory influenza vaccination program at BJC were encouraging as 98.4% of HCWs received influenza vaccination in the fall of 2008. 40 A more detailed description of the implementation and follow up of the mandatory influenza program is currently in progress.
ACKNOWLEDGMENTS
The authors gratefully acknowledge all the participants of the structured interviews for their generous contribution to this study as well as all BJC HealthCare occupational health nurses, infection prevention specialists and other nurses involved in the influenza vaccination campaigns through the years.
Financial support: no specific financial support was used for this article.
MCA received funding for her healthcare epidemiology research scholarship in the U.S. from the Pontificia Universidad Católica de Chile, the Chilean government (“Beca Internacional Presidente de la República, INTER 270, CONICYT. Resolución convenio becario 1232”) and the SHEA International Ambassador Program.
VJF receives funding from the CDC Epicenter grant 5U01CI000033302, NIH grant 5K24AI06779402, BJH Foundation grant 00808-1106-01, and NIH Clinical and Translational Science Award 1KL2 RR024994-01.
Footnotes
Potential conflicts of interest: MCA, KFW, HMB, NG and MJ report no potential conflicts of interest relevant to this article. VJF has been a speaker for Johnson & Johnson, and consultant for Hawaii Chitopure and Ancora, which are not related to this paper.
REFERENCES
- 1.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 3.Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25:5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 4.Doebbeling BN, Edmond MB, Davis CS, Woodin JR, Zeitler RR. Influenza vaccination of health care workers: evaluation of factors that are important in acceptance. Prev Med. 1997;26:68–77. doi: 10.1006/pmed.1996.9991. [DOI] [PubMed] [Google Scholar]
- 5.Salgado CD, Farr BM, Hall KK, Hayden FG. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 6.Rabagliati R, Benitez R, Fernandez A, et al. [Influenza-A as etiology of fever and respiratory insufficiency in adults hospitalized during an outbreak in Chile] Rev Med Chil. 2004;132:317–324. [PubMed] [Google Scholar]
- 7.Pearson ML, Bridges CB, Harper SA. Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006;55:1–16. [PubMed] [Google Scholar]
- 8.Maltezou HC, Drancourt M. Nosocomial influenza in children. J Hosp Infect. 2003;55:83–91. doi: 10.1016/s0195-6701(03)00262-7. [DOI] [PubMed] [Google Scholar]
- 9.Sartor C, Zandotti C, Romain F, et al. Disruption of services in an internal medicine unit due to a nosocomial influenza outbreak. Infect Control Hosp Epidemiol. 2002;23:615–619. doi: 10.1086/501981. [DOI] [PubMed] [Google Scholar]
- 10.Dash GP, Fauerbach L, Pfeiffer J, et al. APIC position paper: Improving health care worker influenza immunization rates. Am J Infect Control. 2004;32:123–125. doi: 10.1016/j.ajic.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Stott DJ, Kerr G, Carman WF. Nosocomial transmission of influenza. Occup Med (Lond) 2002;52:249–253. doi: 10.1093/occmed/52.5.249. [DOI] [PubMed] [Google Scholar]
- 12.Carman WF, Elder AG, Wallace LA, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000;355:93–97. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- 13.Potter J, Stott DJ, Roberts MA, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saxen H, Virtanen M. Randomized, placebo-controlled double blind study on the efficacy of influenza immunization on absenteeism of health care workers. Pediatr Infect Dis J. 1999;18:779–783. doi: 10.1097/00006454-199909000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Wilde JA, McMillan JA, Serwint J, Butta J, O'Riordan MA, Steinhoff MC. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA. 1999;281:908–913. doi: 10.1001/jama.281.10.908. [DOI] [PubMed] [Google Scholar]
- 16.Bridges CB, Thompson WW, Meltzer MI, et al. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: A randomized controlled trial. JAMA. 2000;284:1655–1663. doi: 10.1001/jama.284.13.1655. [DOI] [PubMed] [Google Scholar]
- 17.Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–928. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 18.Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333:1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fiore AE, Shay DK, Haber P, et al. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. MMWR Recomm Rep. 2007;56:1–54. [PubMed] [Google Scholar]
- 20.Talbot TR, Bradley SE, Cosgrove SE, Ruef C, Siegel JD, Weber DJ. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol. 2005;26:882–890. doi: 10.1086/502512. [DOI] [PubMed] [Google Scholar]
- 21.Harper SA, Fukuda K, Uyeki TM, Cox NJ, Bridges CB. Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2005;54:1–40. [PubMed] [Google Scholar]
- 22.Lugo NR. Will carrots or sticks raise influenza immunization rates of health care personnel? Am J Infect Control. 2007;35:1–6. doi: 10.1016/j.ajic.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Poland GA, Tosh P, Jacobson RM. Requiring influenza vaccination for health care workers: seven truths we must accept. Vaccine. 2005;23:2251–2255. doi: 10.1016/j.vaccine.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 24.McArthur MA, Simor AE, Campbell B, McGeer A. Influenza vaccination in long-termcare facilities: structuring programs for success. Infect Control Hosp Epidemiol. 1999;20:499–503. doi: 10.1086/501659. [DOI] [PubMed] [Google Scholar]
- 25.Saito R, Suzuki H, Oshitani H, Sakai T, Seki N, Tanabe N. The effectiveness of influenza vaccine against influenza a (H3N2) virus infections in nursing homes in Niigata, Japan, during the 1998–1999 and 1999–2000 seasons. Infect Control Hosp Epidemiol. 2002;23:82–86. doi: 10.1086/502011. [DOI] [PubMed] [Google Scholar]
- 26.Bryant KA, Stover B, Cain L, Levine GL, Siegel J, Jarvis WR. Improving influenza immunization rates among healthcare workers caring for high-risk pediatric patients. Infect Control Hosp Epidemiol. 2004;25:912–917. doi: 10.1086/502319. [DOI] [PubMed] [Google Scholar]
- 27.Lester RT, McGeer A, Tomlinson G, Detsky AS. Use of effectiveness of attitudes regarding influenza vaccine among house staff. Infect Control Hosp Epidemiol. 2003;24:839–844. doi: 10.1086/502146. [DOI] [PubMed] [Google Scholar]
- 28.Harbarth S, Siegrist CA, Schira JC, Wunderli W, Pittet D. Influenza immunization: improving compliance of healthcare workers. Infect Control Hosp Epidemiol. 1998;19:337–342. doi: 10.1086/647825. [DOI] [PubMed] [Google Scholar]
- 29.Sartor C, Tissot-Dupont H, Zandotti C, et al. Use of mobile cart influenza program for vaccination of hospital employees. Infect Control Hosp Epidemiol. 2004;25:918–922. doi: 10.1086/502320. [DOI] [PubMed] [Google Scholar]
- 30.Polgreen PM, Septimus EJ, Parry MF, et al. Relationship of influenza vaccination declination statements and influenza vaccination rates for healthcare workers in 22 US hospitals. Infect Control Hosp Epidemiol. 2008;29:675–677. doi: 10.1086/588590. [DOI] [PubMed] [Google Scholar]
- 31. [Accessed May 14, 2009];Self-reported influenza vaccination coverage trends 1989–2006 among adults by age group, risk group, race/ethnicity, health-care worker status, and pregnancy status, United States, National Health Interview Survey (NHIS) at http://www.cdc.gov/flu/professionals/vaccination/pdf/NHIS89_07fluvaxtrendtab.pdf.
- 32.Van den Dool C, Van Strien AM, den Akker IL, Bonten MJ, Sanders EA, Hak E. Attitude of Dutch hospital personnel towards influenza vaccination. Vaccine. 2008;26:1297–1302. doi: 10.1016/j.vaccine.2007.12.045. [DOI] [PubMed] [Google Scholar]
- 33.Shah SI, Caprio M. Availability of trivalent inactivated influenza vaccine to parents of neonatal intensive care unit patients and its effect on the healthcare worker vaccination rate. Infect Control Hosp Epidemiol. 2008;29:309–313. doi: 10.1086/527515. [DOI] [PubMed] [Google Scholar]
- 34.Watanakunakorn C, Ellis G, Gemmel D. Attitude of healthcare personnel regarding influenza immunization. Infect Control Hosp Epidemiol. 1993;14:17–20. [PubMed] [Google Scholar]
- 35.Talbot TR. Improving rates of influenza vaccination among healthcare workers: educate; motivate; mandate? Infect Control Hosp Epidemiol. 2008;29:107–110. doi: 10.1086/527573. [DOI] [PubMed] [Google Scholar]
- 36.Sartor C, Tissot-Dupont H, Zandotti C, Martin F, Roques P, Drancourt M. Use of a mobile cart influenza program for vaccination of hospital employees. Infect Control Hosp Epidemiol. 2004;25:918–922. doi: 10.1086/502320. [DOI] [PubMed] [Google Scholar]
- 37.Nafziger DA, Herwaldt LA. Attitudes of internal medicine residents regarding influenza vaccination. Infect Control Hosp Epidemiol. 1994;15:32–35. doi: 10.1086/646815. [DOI] [PubMed] [Google Scholar]
- 38.Ohrt CK, McKinney WP. Achieving compliance with influenza immunization of medical house staff and students. A randomized controlled trial. JAMA. 1992;267:1377–1380. [PubMed] [Google Scholar]
- 39.Poland GA, Ofstead CL, Tucker SJ, Beebe TJ. Receptivity to mandatory influenza vaccination policies for healthcare workers among registered nurses working on inpatient units. Infect Control Hosp Epidemiol. 2008;29:170–173. doi: 10.1086/526432. [DOI] [PubMed] [Google Scholar]
- 40.Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination: Translating Policy to Practice. 19th SHEA Annual Scientific Meeting, abstract # 517; San Diego, California. 2009. [Google Scholar]