Abstract
Background
Cardiovascular diseases are the leading cause of death and disability in China. High blood pressure caused by excess intake of dietary sodium is widespread and an effective sodium reduction program has potential to improve cardiovascular health.
Design
This study is a large-scale, cluster-randomized, trial done in five Northern Chinese provinces. Two counties have been selected from each province and 12 townships in each county making a total of 120 clusters. Within each township one village has been selected for participation with 1:1 randomization stratified by county. The sodium reduction intervention comprises community health education and a food supply strategy based upon providing access to salt substitute. Subsidization of the price of salt substitute was done in 30 intervention villages selected at random. Control villages continued usual practices. The primary outcome for the study is dietary sodium intake level estimated from assays of 24 hour urine.
Trial status
The trial recruited and randomized 120 townships in April 2011. The sodium reduction program was commenced in the 60 intervention villages between May and June of that year with outcome surveys scheduled for October to December 2012. Baseline data collection shows that randomisation achieved good balance across groups.
Discussion
The establishment of the China Rural Health Initiative has enabled the launch of this large-scale trial designed to identify a novel, scalable strategy for reduction of dietary sodium and control of blood pressure. If proved effective, the intervention could plausibly be implemented at low cost in large parts of China and other countries worldwide.
BACKGROUND
Chronic diseases are a large and rapidly growing cause of premature death and disability in China1. Just as in urban regions, the chronic disease burden in rural China is substantially dependent upon adverse diets and behaviors2 that result in high levels of sodium consumption3,4 a chief cause of high blood pressure.1 The problem is particularly marked in rural and Northern China where sodium consumption, hypertension and the incidence of stroke are all very high.5 While there has been some ongoing debate about the effects of sodium on vascular disease, effects on blood pressure are well-established and several comprehensive reviews of the evidence have recommended population-wide sodium reduction strategies.6,7 Multi-faceted sodium reduction programs with strong government leadership, food industry engagement, clear targets, objective monitoring, and community education programs are believed to have the greatest likelihood of substantive impact.8
Salt substitution is a further novel option for communities in which most dietary sodium is from salt added during food preparation and its use has undergone extensive pilot testing in China. Salt substitutes have a high level of community acceptability, documented large beneficial effects on blood pressure9,10 and no identified safety issues11,12 with benefits accruing from both the reduction in dietary sodium and the increase in dietary potassium.3,4 The higher price of salt substitute (approximately double the price of regular salt) may present a barrier to widespread use although even in rural communities salt substitute is a low cost commodity. Accordingly, salt substitution in conjunction with health education and supportive policy measures should have significant potential in China, offering a plausible, low-cost, and low-tech approach to the huge blood pressure-related disease burden in the country.13
OBJECTIVES
The objective of this study is to identify a novel, low-cost, scalable and sustainable, community-based strategy for the prevention of blood pressure-related diseases in rural China. The primary aim is to define the effects of the sodium reduction strategy on average sodium intake level, as estimated from 24-hour urinary sodium excretion. The corresponding null hypothesis that will be tested is that the sodium reduction strategy will have no effect upon average 24-hour urinary sodium excretion.
METHODS
The “China Rural Health Initiative Sodium Reduction Study” is an open, large-scale, cluster-randomized, controlled trial conducted in rural China with the township as the unit of investigation. The trial was registered with clinicaltrial.gov in December 2010 and the registration number is NCT01259700. The study is supported by the US National Heart, Lung and Blood Institute (NIH), the National US Centers for Chronic Disease Prevention (Center for Global Health and National Center for Chronic Disease Prevention and Health Promotion, CDC) (Contract HHSN268200900027C), and the UnitedHealth Group Chronic Disease Initiative. Bruce Neal is supported by an Australian Research Council Future Fellowship and Nicole Li by an Australian National Health and Medical Research Council Overseas Fellowship. The authors were solely responsible for the design, all study analyses, and the drafting and editing of the paper. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention.
PROVINCES, TOWNSHIPS AND VILLAGES INCLUDED
The study is being done in five of China’s Northern Provinces utilizing collaborations established with local academic institutions and governments as part of the China Rural Health Initiative. The five Provinces included are Hebei, Liaoning, Ningxia, Shanxi and Shaanxi. These provinces are known to have high rates of vascular disease with a substantial burden caused by high blood pressure attributed to an average daily sodium intake of 260mmol/24hr (about 15g/24hr of salt).14
Two counties from each Province were selected to participate on the basis of their interest in and willingness to participate, their proximity to the local research team, and their being broadly representative of the socioeconomic development level of counties in the Province. In each of these 10 counties there are 12 townships engaged (for a total of 120 townships). Selection of townships was determined primarily through discussion with the leadership of the local county Bureau of Health to identify willing and accessible partners.
Each township comprises 10 to 20 villages, each with an average population of about 2,000 individuals. Within each township one village has been selected for the study, typically the village closest to the geographic center of the township. The goal of this strategy was to minimize the risk of contamination between adjacent intervention and control villages with most participating villages separated by 10 kilometers or more. In the event that the selected village declined to participate, or was the site of the township healthcare center, the next most geographically central village was asked to participate until a consenting village was found.
The township (rather than the village) has been selected as the unit of randomization for reasons of implementation. The delivery of the program requires the involvement of healthcare providers operating at the township level and it would be difficult to prevent contamination between intervention and control sites if villages within a given township were randomized to different conditions.
It is important to note that the non-random selection of the counties, townships and villages is not a significant issue for a study with this design. The key is that assignment of townships (and the selected village in each) to intervention or control is by chance alone and this is achieved by the randomization process. Furthermore, our efforts to include a broadly representative group of townships should ensure that trial results will be broadly generalizable throughout rural China.
Randomization
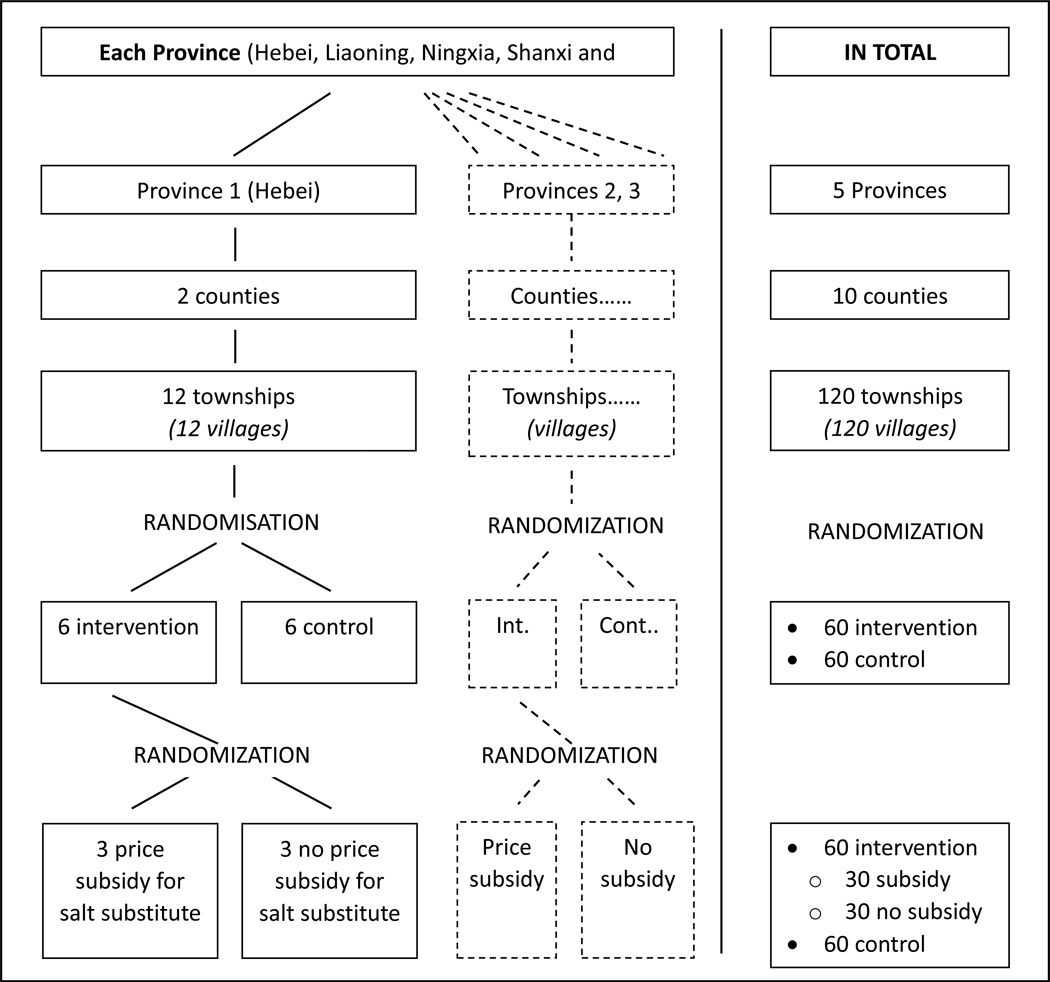
Randomization was done by computer, after consent was obtained from the village, through assignment of a random number with stratification by county and a 1:1 allocation of townships to the sodium reduction program or control (Figure 1). Intervention villages were then further assigned at random to receive subsidization of the price of salt substitute, or not, using the same approach to stratification.
Figure 1.
Study flow chart – site selection and randomization
Intervention and control
The sodium reduction intervention is comprised of community-based health education and a food supply measure designed to promote the use of reduced sodium and added potassium salt substitute.
The community-based health education program has been designed on the basis of the health belief model15 and seeks to achieve population-level sodium reduction by increasing awareness of the health risks posed by excess sodium consumption, establishing community beliefs about the adverse effect of salt on personal wellbeing, and encouraging and facilitating improved healthy behaviors. Increasing awareness efforts will focus on the adverse effects of sodium on blood pressure and likely adverse effects on stroke. Changes in health beliefs will be achieved by repeated health education sessions, peer education, and child-to-parent education. Behavior will be influenced by teaching the community about the sources of sodium in their diet and how to reduce personal consumption by changing cooking and food pickling practices with specific advice about different food seasonings and a recommendation to use salt substitute (Table 1). Program delivery is by study staff working with the existing township health educators, the village council and village doctors who use public announcement systems, bulletin boards, and specially developed promotional materials. The community education program includes elements that target high risk individuals with severe hypertension or established vascular disease. Village doctors assist with identifying high risk individuals and coordinate face-to-face sessions between patients and township health educators.
The food supply measure makes salt substitute available for purchase in the village stores of all intervention villages and uses the township health educators, the village doctors and the village store keepers to promote the purchase and use of salt substitute instead of usual salt. The potential for salt substitute to reduce blood pressure to a similar extent as drug therapy, at the same or lower cost as drug treatment, is highlighted to villagers in an effort to have them consider adding salt substitute to other therapeutic strategies they might be using or considering using. Because salt substitute costs more than usual salt, this may create a barrier to its uptake. Thus, subsidization to make the price of the salt substitute comparable to that of usual salt, has been done for thirty of the intervention villages selected at random. The salt substitute contains, on average, 65% sodium chloride, 25% potassium chloride and 10% magnesium sulphate and is iodized and commercially available in China, but mostly not used in rural areas.
Table 1.
Main components of the health education program
| Phase one Increasing awareness (May to Jul 2011) | Program launch event in all villages Posters displayed sequentially in high traffic areas describing: Risks of excess sodium intake How to reduce sodium intake Benefit of using low sodium salt Stickers containing introduction of low sodium salt delivered and pasted on low sodium salt packages in village convenience stores Posters introducing the benefit of using low sodium salt displayed in village convenience stores Interactive sessions targeting high risk individuals addressing: Risks of excess sodium intake and the recommended daily salt intake level Methods to reduce sodium intake and benefits of use low sodium salt Distribution of materials to households including: Calendars Stickers for salt containers Invitation to attend community-wide health education sessions Community health education session introducing low sodium salt |
| Phase two Establishing Beliefs (Aug 2011 to Mar 2012) | First primary school students competition Community health education session recommending less high salt food and supporting the use of low sodium salt Posters providing key educational messages displayed in high traffic areas around villages Repeat distribution of educational materials to households. |
| Phase three Changing behavior (Apr 2012 to Sep 2012) | Community health education sessions Incorporating prior messages into local Chinese New Year celebrations Promoting low sodium salt Interactive sessions targeting high risk individuals: Teaching skills on how to successfully reduce sodium intake Experience sharing on how to use low sodium salt Posters repeating main educational messages displayed in high traffic areas around villages Second primary school students competition |
Control group villages continue their usual practices without the introduction of any of the sodium reduction initiatives described above. As such, control group villages are exposed to very little by way of efforts to achieve individual or population-wide salt reduction.
OUTCOME EVALUATION
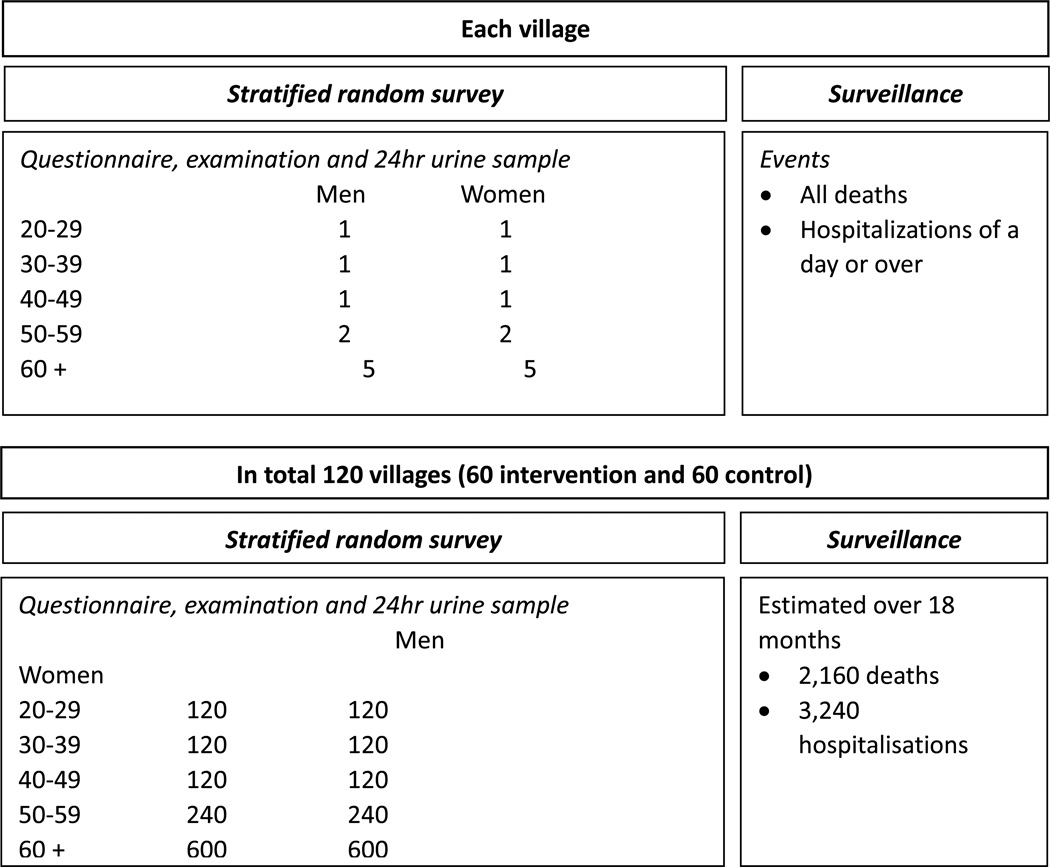
All outcome assessments will be done in exactly the same way in every village, regardless of its assignment to intervention or control (Figure 2). Since blinding of data collection staff to the randomized allocation of the villages may be difficult to maintain, there will be a strong focus on training staff to apply rigorously standardized evaluation techniques for every outcome assessed.
Figure 2.
Evaluation plan – stratified random survey and surveillance
The population survey will be done at about 18 months after commencement of the intervention amongst an age- and sex-stratified random sample drawn from all 120 villages. In each village, the survey will collect data from at least 20 consenting adults (2,400 in total). Sampling will be done according to the following scheme: 1 man and 1 women aged 20–29, 1 man and 1 woman aged 30–39, 1 man and 1 woman aged 40–49 years, 2 men and 2 women aged 50–59 years and 5 men and 5 women aged 60 or over (Figure 2). This sampling scheme is designed to ensure that maximum sampling is done in the older age groups who are a particular target of the intervention while ensuring that reasonable numbers are also included from younger ages. Sampling will be done using village rosters with efforts made to sample only one individual from a household by having the village chief (or other informed alternate) review the list of selected individuals.
For every selected individual a brief interviewer-administered questionnaire will be completed. The questionnaire will collect data on demographics, disease history, medications used for blood pressure management, and knowledge and practices related to salt. Likewise, every individual sampled will have a physical examination comprising assessment of blood pressure, weight and height. Blood pressure measurements will be made in duplicate with the participant seated after 5 minutes rest. Measurements will be recorded at least two minutes apart using an automated electronic sphygmomanometer.
Materials and instructions for collecting a 24hr urine sample will be provided. On the day of collection, participants will be asked to urinate on waking, discard that sample and then collect all urine including that voided first thing after waking the next day. The samples will be collected and the volume will be recorded. An aliquot of the sample will be taken and shipped to a central lab for assay of sodium, potassium and creatinine with the remainder discarded. The likely completeness of collection will be assessed from the urine volume, from participants’ reports and from the 24-hour urinary creatinine excretion level.16
A process evaluation will be done to document the extent to which the intervention was implemented as planned and to help explain the observed outcomes.17,18 Surveys, interviews and other discussions with village doctors, convenience store owners and village chiefs will be done to gauge their understanding of the key issues related to the effects of salt and salt substitute on health, and their practices in regard to the promotion of sodium reduction efforts and the use of salt substitute. In addition, interviews and focus groups will be done at the end of the intervention amongst key stakeholders involved in the programs including county officials, township health care center leaders, village doctors, community health educators, and villagers.
Finally, we will seek to record deaths and non-fatal hospitalizations that occur in the villages during the study period. The diagnosis assigned in the existing administrative databases from which events are identified will be recorded with broad groupings made into major vascular and non-vascular causes.
OUTCOMES
The primary outcome will be the mean daily sodium consumption estimated from 24-hour urine collections. The secondary outcomes will be mean 24-hour urinary potassium excretion, mean urinary sodium:potassium ratio, mean systolic and diastolic blood pressure levels and the proportion with hypertension.
The key process outcomes recorded will be the self-reported presence of salt substitute in the house, consumption of salt substitute, purchases of salt substitute, efforts to reduce salt consumption, knowledge that excess salt consumption is harmful and knowledge that salt substitute represents a better alternate.
ECONOMIC EVALUATION
An economic evaluation will be conducted to provide an assessment of the cost-effectiveness of the intervention. The perspective to be adopted will be that of the health sector and will include costs to government in establishing and running the program including the costs associated with incentivizing providers but excluding protocol driven costs associated with conducting the research. The cost data will be extracted from financial statements from the project, from village stores and from healthcare providers. Data on use of health care services and medications will be drawn from patient records collected at the follow-up survey. These resource items will be costed at standard prevailing market rates while recognizing variation in unit costs across regions. Average costs per individual in each randomized group will be estimated over the period of follow-up. Cost effectiveness will be estimated initially in terms of cost per unit reduction in sodium but modeled to estimate cost per life year saved and cost per Disability Adjusted Life Year (DALY) averted. These estimates will utilize other evidence from the literature describing the quantitative associations of changes in salt consumption with disease. A series of sensitivity analyses will be done to estimate uncertainty about the primary findings associated with varying key parameters.
STATISTICAL POWER AND ANALYSIS
The sample size has been selected to provide more than 90% statistical power (with a two-sided alpha=0.05) to detect a difference in mean 24-hour excretion of sodium of 11mmol/day (0.65g/day salt) or greater between intervention and control clusters. This estimate assumes a standard deviation of 24hr sodium excretion of 60mmol/day,19 an intra-cluster correlation coefficient of 0.05 and a sample of 2,400 individuals drawn from 120 clusters equally randomized between intervention and control. The primary analyses will compare the mean follow-up level of sodium amongst the individuals sampled from the 60 intervention villages with the mean levels of the individuals sampled from the 60 control townships. Analyses of these survey data will be by intention-to-treat and will include adjustment for the effects of clustering. Concurrently conducted with this trial in these villages is a separate cluster-randomized study of the effects of providing enhanced clinical care to individuals at high risk of cardiovascular disease. While conducted and analyzed separately, with different interventions and outcomes, evidence for interaction between the two randomized interventions will be explored.
ETHICS REVIEW AND HUMAN SUBJECT PROTECTION
The project has been reviewed and approved locally by the Ethics Committee of the Peking University Health Science Center in Beijing and in the United States by the Institutional Review Board of Duke University. All collaborating organizations and study personnel have received either on-line or in-person training on human subject protection. Consent for participation in the project has been sought at the cluster level and the individual level. Cluster level consent of the community was obtained through a consultation process involving the government (at a provincial, county and township level) and the village leaders. The project was explained, including the process of random assignment of communities to intervention and control conditions and the nature of the interventions, at a face-to-face meeting. Questions were answered and all relevant stakeholder groups were invited to consult with their members and reflect upon the project. Individual consent for participation in outcome surveys will be obtained from all persons selected in the usual way with provision of a participant information sheet, explanation and discussion as required, and the collection of written consent from those willing to take part. Participants identified during the survey that require medical attention will be referred to existing services in line with usual practice.
PROJECT STATUS
The trial has recruited and randomized 120 townships and the intervention program has commenced in all 60 villages selected for intervention. The sodium reduction intervention was initiated in the 60 intervention villages between May and June of 2011. Salt substitute has been made available to every intervention village with subsidization of the price of salt-substitute in 30 intervention villages as planned. Data collection for mortality and hospitalization outcomes is ongoing. Process measures tracking the delivery of the various components of the sodium reduction strategy are underway in all Provinces. The baseline questionnaire data demonstrate good balance of participant characteristics across intervention and control villages (Table 2).
Table 2.
Baseline characteristics of the study population 2010*
| Intervention |
Control |
||
|---|---|---|---|
| With price subsidy for salt substitute (n=1268) |
Without price subsidy for salt substitute (n=1253) |
(n=2529) | |
| Demographics | |||
| Female (%) | 50 | 50 | 50 |
| Age (years) ± standard deviation | 66±8.3 | 66±8.0 | 66±8.1 |
| Formal education (%) | |||
| 0 years | 32 | 33 | 31 |
| 1 to 6 years | 26 | 27 | 26 |
| 6 to 9 years | 27 | 24 | 25 |
| > 9 years | 15 | 15 | 18 |
| Behaviours (%) | |||
| Current smoker | 31 | 31 | 31 |
| Drink alcohol® | 21 | 22 | 20 |
| Disease history (%) | |||
| Coronary heart disease | 7.7 | 7.3 | 7.8 |
| Stroke | 6.6 | 7.9 | 6.4 |
| Diabetes | 2.9 | 2.9 | 3.3 |
| Hypertension | 50 | 50 | 52 |
| Physical Examination | |||
| SBP (mmHg) | 148±24 | 146±24 | 147±24 |
| DBP (mmHg) | 85±14 | 84±14 | 86±14 |
| Heart rate (beats per minute) | 76±12 | 76±12 | 76±12 |
| BMI (kg/m2) | 24.1±3.7 | 24.0±3.6 | 24.3±3.5 |
As reported by participant, unless directly measured
Drink alcohol is defined as having drunk any type of alcohol in the three months prior to baseline survey
DISCUSSION
In China, vascular diseases are a large and rapidly growing cause of disease burden. While some preventive care is available, much of the population has limited access to chronic disease services and little capacity to pay for them. This is particularly true for rural areas where half of the Chinese population currently lives. Low-cost strategies to improve health in rural areas are therefore urgently sought and extensive consultations with researchers, ministry officials and industry indicate that strengthening the evidence-base for sodium reduction would achieve significant support for policy change.
Blood pressure, as the single most important determinant of vascular disease in China20 is a clear target for which improvement of diet, through sodium reduction, appears to offer enormous and largely untapped potential.21,22 A series of systematic reviews that have assessed the totality of the evidence-base provide a strong scientific rationale for population-wide sodium reduction with recent targets set by the World Health Organisation. While there has been some debate about the merits of sodium reduction in the scientific and general media, there is a broad consensus that the key scientific questions for sodium reduction efforts in China now relate to how to achieve a population-wide lowering of average intake levels. Discussions with senior Chinese government representatives indicate that clear evidence in this regard would provide a compelling case to support up-scaling of national sodium reduction efforts within the National Chronic Disease Control and Prevention Strategy.
It is widely believed that a multifaceted approach is required to achieve population sodium reduction. The intervention tested here is based upon the health beliefs model/5 implemented through a community education program and supported by a food supply measure. Clear evidence about the separate effects of the various components of the intervention is absent but it was elected to include all elements that might contribute to the sodium reduction goal. In this way the potential for a positive outcome was maximized and a process evaluation was included to allow a post hoc analysis of the relative impact of each component.
The large size and randomized design of the trial are significant methodological strengths. Likewise, the real world setting in which the study is being done and the efforts made to incorporate the intervention within existing structures will provide for ready translation of positive findings into policy and practice. The open design is non-optimal but the use of standardized and objective methods for the collection of the primary and secondary efficacy data should ensure that biases are minimized. While there will nonetheless be imprecise and incomplete collection of data this should be non-differential between groups and the randomised design should therefore provide for substantively unbiased estimates of the effects of the intervention. Cluster-randomization has been used to suit the nature of the intervention under investigation and the reduction in study power that ensued has been addressed by enrolling a large number of clusters and individuals. This has provided excellent power for assessing the key primary and secondary outcomes although there will be less power to explore other questions such as the importance of price subsidization, or the effects of the intervention in population subgroups. Care has been taken to ensure that the clusters are geographically and organizationally separated although there is still some risk that elements of the intervention will be partially implemented in the control group clusters. To mitigate this risk, we have power to detect quite small effects on the primary and secondary outcomes.
In conclusion, centrally implemented, population-based approaches to salt reduction have been identified by the World Health Organization and other national and international entities as amongst the most cost-effective possible strategies for vascular disease prevention in both developed and developing countries alike.23 The evidence provided by this study about the effectiveness of this implementation strategy, while directly applicable to rural China, will have broader generalizability to other settings around the world in which salt added during food preparation in the home constitutes a significant proportion of daily sodium intake.
ACKNOWLEDGEMENTS
The Steering Committee for the China Rural Health Initiative is comprised of: Qide Han (Honorary Chair), Yang Ke (Chair), Yangfeng Wu (Vice Chair and Secretary General), Michael Merson (vice chair), Bruce Neal (vice chair), Paul Elliott, Xiangxian Feng, Stephen Leeder, Lingzhi Kong, Alan Lopez, Qun’an Mao, Jingpu Shi, Jianxin Zhang, Ruijuan Zhang and Yuhong Zhang. The Scientific Committee for the Sodium Reduction Study is comprised of Bruce Neal (Chair), Lijing L. Yan (Vice Chair), Elizabeth DeLong, Michael Dibley, Jixiang Ma, Wenyi Niu, Yangfeng Wu. Ad hoc members of the Scientific Committee are Darwin Labarthe and Paul Elliott. We acknowledge the assistance and support provided by Jing Zhang, Li Yan, and Tao Wu during the design stage of the study.
The first draft of the paper was prepared by Nicole Li, Lijing L. Yan and Bruce Neal. All authors reviewed the paper and their comments were incorporated.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 2.Chen J, Campbell T, Li J, Peto R. Diet, lifestyle and mortality in China. Oxford: Oxford University Press; 1990. [Google Scholar]
- 3.China Ministry of Health, China Ministry of Science and Technology, Statisitics. aCSBo. The Nutrition and Health Status of the Chinese People. Beijing, China: Press Conference of the State Council Information Office; 2004. [Google Scholar]
- 4.Zhao L, Stamler J, Yan L, Zhou B, Wu Y, Liu K, et al. Blood pressure differences between northern and southern Chinese: role of dietary factors: the International Study on Macronutrients and Blood Pressure. Hypertension. 2004;43:1332–1337. doi: 10.1161/01.HYP.0000128243.06502.bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian H-G, Guo Z-Y, Hu G, Yu S-J, Sun W, Pietinen P, et al. Changes in sodium intake and blood pressure in a community-based intervention project in China. J Hum Hypertens. 1995;9:959–968. [PubMed] [Google Scholar]
- 6.Cook N, Cutler J, Obarzanek E, Buring J, Rexrode K, Kumanyika S, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334(7599):885. doi: 10.1136/bmj.39147.604896.55. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang H-Y, Hu Y-W, Yue C-SJ, Wen Y-W, Yeh W-T, Hsu L-S, et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. American Journal of Clinical Nutrition. 2006;83:1289–1296. doi: 10.1093/ajcn/83.6.1289. [DOI] [PubMed] [Google Scholar]
- 8.Kirsten Bibbins-Domingo K, Chertow G, Coxson P, Moran A, Lightwood J, Pletcher M, et al. Projected effect of dietary salt reductions on future cardiovascular disease. New Eng J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The China Salt Substitute Study Collaborative Group. Salt substitution - a low cost strategy for blood pressure control among rural Chinese: a randomized controlled trial. J Hypertens. 2007;25:2011–2018. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 10.Taylor R, Ashton K, Moxham T, Hooper L, Ebrahim S. Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database of Systematic Reviews. 2011;(7):CD009217. doi: 10.1002/14651858.CD009217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karppanen H, Tanskanen A, Tuomilehto J, Puska P, Vuori J, Jantti V, et al. Safety and effects of potassium- and magnesium-containing low sodium salt mixtures. J Cardiovasc Pharmacol. 1984;6(Suppl 1):S236–S243. doi: 10.1097/00005344-198400061-00037. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health (UK) Scientific Advisory Committee on Nutrition: Salt and Health. 2003
- 13.Yang Q, Liu T, Kuklina E, Flanders D, Hong Y, Gillespie C, et al. Sodium and Potassium Intake and Mortality Among US Adults. Prospective Data From the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2011;171:1183–1191. doi: 10.1001/archinternmed.2011.257. [DOI] [PubMed] [Google Scholar]
- 14.Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118(25):2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 15.Rosenstock I, Strecher V, Becker M. Social learning theory and the health belief model. Health Education Quarterly. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 16.Cutler J, Follmann D, Allender P. Randomized trials of sodium reduction: an overview. Am J Clin Nutr. 1997;65(2):643S–651S. doi: 10.1093/ajcn/65.2.643S. [DOI] [PubMed] [Google Scholar]
- 17.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oakley A, Strange V, Bonell C, Allen E, Stephenson J. Process evaluation in randomised controlled trials of complex interventions. BMJ. 2006;332(7538):413–416. doi: 10.1136/bmj.332.7538.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood pressure lowering regimens on major cardiovascular events: Second cycle of prospectively designed overviews. Lancet. 2003;362:1527–1535. doi: 10.1016/s0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 20.Rodgers A, Ezzati M, Vander Hoorn S, Lopez A, Lin R, et al. Distribution of Major Health Risks: Findings from the Global Burden of Disease Study. PLoS Med. 2004:e27. doi: 10.1371/journal.pmed.0010027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Assembly FSWH, editor. World Health Organization. Global strategy on diet, physical activity and health. 2004. Available from: http://www.who.int/dietphysicalactivity/goals/en/index.html. [Google Scholar]
- 22.World Health Organization. Preventing Chronic Diseases: A Vital Investment. Geneva: 2005. [Google Scholar]
- 23.Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, et al. Priority actions for the non-communicable disease crisis. Lancet. 2011;377(9775):1438–1447. doi: 10.1016/S0140-6736(11)60393-0. [DOI] [PubMed] [Google Scholar]