Abstract
Background:
It is well accepted that persons with spinal cord injury (SCI) have impaired ability to regulate core temperature due to impaired vasomotor and sudomotor activity below their level of injury. Impaired heat dissipation puts SCI athletes at great risk of exercise-induced hyperthermia (EIH) (>37.8°C). There is minimal evidence for efficacy of any specific cooling method in SCI athletes in a thermoneutral sport-specific setting.
Objective:
To evaluate the extent of EIH in persons with and without SCI and subsequently examine the effect of a cooling vest to attenuate rise in core body temperature (Tc).
Methods:
SCI (n = 17) and able-bodied (AB; n = 19) athletes participated in a 60-minute intermittent sprinting exercise in a thermoneutral (21.1°C-23.9°C) environment. Participants were separated according to their level of injury: tetraplegia defined as above T1 (TP; n = 6), high paraplegia defined as T5 through T1 (HP; n = 5), low paraplegia defined as T6 and below (LP; n = 6), and AB (n = 19). Tc was recorded at 15-minute intervals using an ingestible thermometer pill. This protocol was completed with a cooling vest (V) and without a cooling vest (NV).
Results:
All SCI and most AB athletes experienced EIH. After 60 minutes, Tc of TP athletes was significantly increased compared to HP (P = .03) and AB athletes (P = .007). There was no significant effect of the vest on Tc over time for any group.
Conclusions:
TP athletes have the highest risk of exercise-induced hyperthermia. The cooling vest does not significantly attenuate rise in Tc in SCI or AB athletes.
Key words: body temperature, hyperthermia, spinal cord injury, thermoregulation
Injury to the spinal cord results in impairment of vasomotor and sudomotor function at and below the level of injury (LOI).1 In non–spinal-cord-injured individuals, internal heat gain from metabolically active muscles (eg, during exercise) and external heat gain from the ambient air is mitigated through processes regulated by the hypothalamus. The afferent input of heat gain results in neurological efferent signals that regulate vasomotor tone (convective cooling) and sudomotor activation (evaporative cooling). In persons with spinal cord injury (SCI), the output from the hypothalamus is blocked due to lesions within the spinal cord. Furthermore, the loss of skeletal muscle pump activity from the paralyzed limbs further impairs blood circulation and thus core temperature regulation. As a result, persons with SCI have difficulty dissipating heat during exercise compared to their able-bodied (AB) counterparts.1–3 The extent of such thermal impairment has been shown to be directly related to level and completeness of injury, with higher and complete lesions having more impairment than lower, incomplete lesions.4,5 Specifically, the vessels of the face and neck are sympathetically mediated from levels T1-4, upper extremity vessels mediated from T5-7, and vessels of the lower extremity from T10 to L3.6 Therefore, persons with complete tetraplegia have essentially no vasomotor control, whereas persons with high paraplegia have vasomotor control of face and neck and persons with low paraplegia have control of upper limbs and potentially some control of lower limb vessels depending on the LOI.
In the AB athlete, is it well accepted that elevated core temperature (Tc) due to internal and external heat gain during exercise can impair endurance and performance.7,8 Extreme elevations in Tc can result in exercise-induced hyperthermia (EIH) (>37.8°C-38.3°C) that that can lead to heat exhaustion (<40°C) or heat stroke (>40°C) as defined by American College of Sports Medicine (ACSM).9 For this reason, cooling methods such as whole body cooling, cooling vests, and hand/foot cooling are utilized before and during exercise in AB athletes.10–13 These devices have been shown to reduce thermal strain, increase endurance capacity, and improve performance.14–17
Due to the increased risk of EIH and heat-related illness from thermoregulatory dysfunction in persons with SCI, a number of commercially available cooling devices have been tested in a controlled laboratory setting in attempts to attenuate rise in Tc. Foot cooling garments, hand cooling garments, head and neck cooling garments, misting devices, and a cooling vest have been tested in SCI populations.18–22 This study sought to test the efficacy of the cooling device in a sport-specific environment. The cooling vest interferes minimally with wheelchair propulsion during sporting activities and was thus chosen for this study.
While the efficacy of the cooling vest in normalizing Tc in the AB population has been clearly documented, the efficacy of the vest in SCI populations has variable results from 3 small studies.14,23,24 Armstrong et al18 found that cooling (ice) vests worn during 30 minutes of wheelchair roller exercise in a hot-humid environment (~33°C and ~75% relative humidity) did not significantly decrease Tc in an SCI group (4 with paraplegia, 1 with tetraplegia). Webborn et al evaluated the effect of cooling vests in 2 studies of 8 persons with tetraplegia during an arm crank ergometry intermittent sprint protocol (defined as 14 two-minute exercise periods each consisting of 10 seconds passive rest, 5 seconds maximum sprint, and 105 seconds of active recovery). The first study reported a significant decrease in Tc and rate of perceived exertion when vests were used before (pre-cooling) or during 28 minutes of exercise in the heat.19 The second study also reported a significant decrease in Tc and time to exhaustion during 60 minutes in the heat when wearing the vest.25 Webborn recommended that tetraplegic athletes performing intermittent sprint exercise in hot conditions should wear a cooling vest before or during exercise to attenuate rise in Tc. This study tested Webborn’s recommendation to examine whether these findings translate to a nonlaboratory field-based environment of athletes engaging in intermittent sprint exercise during play of wheelchair basketball and rugby. This concept of testing has recently been recommended, as testing of athletes in their normal sports wheelchair and their natural environment may yield results that are more relevant than laboratory testing.26
The objectives of this study are 2-fold: (1) to evaluate the extent of EIH in persons with and without SCI, and (2) to examine the ability of a cooling vest to attenuate the rise in Tc of SCI and AB athletes during intermittent sprinting exercise.
Methods
Setting
The data collection took place at a local indoor gym with an ambient temperature of 21.1°C-23.9°C measured by a sling psychrometer.
Participants
Study enrollment included 41 well-trained athletes: 22 men with chronic SCI (>1 year post injury) and 19 men without SCI (AB) (Table 1). Five SCI athletes did not complete the study due to their inability to attend all data collection times. All AB athletes completed the study. Seventeen SCI and 19 AB subjects completed the study. SCI athletes were separated into groups according to their level of injury as follows: tetraplegia defined as above T1 (TP; n = 6), high paraplegia defined as T5 through T1 (HP; n = 5), low paraplegia defined as T6 and below (LP; n = 6), and AB (n = 19). Lesion levels of SCI athletes in each group were as follows: TP group, C5-7; HP group, T3-5; and LP group, T7-12. American Spinal Injury Association Impairment Scale (AIS) ranged from A-C in the TP group, A (2 athletes with unknown AIS level) in the HP group, and A-D in the LP group (Table 1). No SCI athletes were community ambulators. SCI athletes’ ages ranged from 21 to 58 years old. AB athletes’ ages ranged from 24 to 61 years old. All SCI athletes (TP, HP, and LP groups) trained and competed regularly in a wheelchair basketball (n = 11) or wheelchair rugby (n = 6) team, whereas all AB athletes exercised at least 3 times a week for 30 minutes.
Table 1. Demographics of SCI and AB athletes.
| Demographics | SCI | TP | HP | LP | AB |
|---|---|---|---|---|---|
| No. | 17 | 6 | 5 | 6 | 19 |
| Mean age, years | 31.6 | 34.5 | 27.6 | 37.3 | 30.8 |
| Age range, years | 21-58 | 25-40 | 24-34 | 21-58 | 24-61 |
| Levels of injury | C5-C7 | T3-T5 | T7-T12 | ||
| AIS, n (%) | |||||
| A | 3 (50%) | 3 (60%) | 2 (33%) | ||
| B | 1 (17%) | 2 (33%) | |||
| C | 2 (33%) | 1 (17%) | |||
| D | 1 (17%) | ||||
| Unknown | 2 (40%) |
Note: AB = able-bodied; AIS = American Spinal Injury Association Impairment Scale; HP = high paraplegia; LP = low paraplegia; SCI = spinal cord injured; TP = tetraplegia.
This study was approved by the local institutional review board. All subjects provided informed consent to participate. The SCI group consisted of wheelchair basketball and rugby players from teams in San Antonio and Austin, Texas. All persons received compensation for participation.
Cooling vest
The cooling vest we selected for trial (Glacier Tek, Inc., West Melbourne, FL) contained renewable phase change material (RPCM) made from high-technology processed fats and oils that maintained temperatures of 15°C when cooled. The RPCM vest was reported not to cause cutaneous vasoconstriction and to be more comfortable on the skin when compared to the ice (0°C) vest (Arctic Heat; www.arcticheatusa.com). Furthermore, when compared head to head, RPCM vests have been shown to better attenuate rise in core temperature than ice vests.28
Each vest had 4 pockets to hold a cooling pack, 2 in front and 2 in back. Each pack measured 12 x 3 in. and was submerged in ice for 20 to 30 minutes until the pack converted to a solid form. Each pack was reported to maintain 15°C for 2 to 3 hours. Following pack placement, the vest weighed 5 lbs. The sleeveless vest covered the shoulders, back, anterior chest, and abdomen to the level of the umbilicus. Participants wore the vest directly over the skin to optimize the potential for conductive cooling. Despite the minimal risk of skin breakdown, participants’ skin was monitored periodically. All participants reported that the vest remained cold to the touch for the entire 60-minute exercise period.
Core temperature measurements
Subjects were asked to swallow a US Food and Drug Administration (FDA)–approved ingestible thermometer pill (HQ Inc., Palmetto, FL) at least 12 hours before each practice. Since gastrointestinal transit time is delayed in persons with SCI, we chose a longer time period than that recommended for AB athletes (8 ± 2.3 hours).29 The ingestible telemetry pill is a small electrical device that detects the surrounding temperature and then transmits it to a handheld external receiver via a radiofrequency interface. This device has been compared to rectal temperature and has been found to be a reliable, valid, and practical alternative to direct Tc measurement.30–32
Exercise protocol
During the no vest (NV) and vest (V) protocols, participants rested in the 21.1°C to 23.9°C gymnasium 20 minutes prior to the measurement of baseline Tc. Afterwards, Tc was measured at 15-minute intervals during 60 minutes of exercise without a cooling vest. The same procedure was followed in the V protocol, however a cooling vest was donned after baseline Tc measurement. The exercise pattern of a typical wheelchair basketball or rugby game consists of intermittent sprints of wheelchair propulsion up and down a standard basketball court.
SCI athletes (TP, HP, LP) played their respective sport (basketball or rugby) in wheelchairs for 60 minutes during 2 separate practice days that were at least 1 week apart. AB athletes played wheelchair basketball to keep the muscles used during exercise similar between both groups. For AB athletes, the same protocol was followed, except that the data were collected under NV and V conditions on the same day with a 2-hour interval between each condition. Downey and Darling reported that at least 1 hour is needed after exercise for Tc to return to baseline, so 2 hours was likely sufficient to minimize any carryover of elevated Tc.33 The AB group was counterbalanced where half of them (n = 10) exercised in the NV and half (n = 9) in the V condition in the morning then switched to the opposite condition in the afternoon.
All participants wore shorts and T-shirts during the NV practice and shorts without shirts during the V practice. Subjects were allowed to drink their choice of fluids without restriction.
Survey of vest on cooling and performance
Following completion of the NV and V practices, SCI participants were mailed an anonymous survey to evaluate their perception of the effect of the vest on their performance and subjective body temperature. Two questions were asked: “Did the cooling vest impact your performance?” and “Did you feel that the vest kept you cooler?”
Data analysis
A 2-factor analysis of variance (ANOVA) with one between-subject factor (group, with 4 levels) and one within-subject factor (vest, with 2 levels) was conducted on the initial baseline measures to determine whether there were any initial differences in core temperature among the groups or between the 2 vest conditions. Difference scores were then computed for each subject and treatment combination that measured the change in Tc from baseline to 30 minutes; a second set of difference scores measured the change from baseline to 60 minutes. For each set of difference scores, an ANOVA was conducted with one between-subject factor (group, with 4 levels) and one within-subject factor (vest, with 2 levels). Finally, an ANOVA was performed on each of the 3 measurement periods with one between-subject factor (group, with 4 levels) and one within-subject factor (vest, with 2 levels).
To further assess the effects of wearing the vest on Tc, a 2-way repeated-measures ANOVA with 2 levels of vest and 3 levels of time was conducted on Tc measures for each of the 4 groups separately.
In all ANOVAs conducted, any significant main between-subject (ie, group) effect was followed by Scheffe multiple comparisons to identify which groups differed. Any significant within-subject main effect or interaction effect (ie, involving vest or time) was followed (as appropriate) by within-subject nonparametric tests, such as the Wilcoxon test for 2 within-subject conditions and the Friedman test for more than 2 within-subject conditions, in order to determine which conditions differed.
Results
Demographic information and injury characteristics for all groups are presented in Table 1. Mean ages were similar between groups, with the average of 31.6 years in the SCI group and 30.8 years in the AB group.
Although Tc was supposed to be measured every 15 minutes, technical errors precluded several participants from adhering to that interval. However, all readings were obtained for all subjects and both conditions (NV, V) at 0 minutes (baseline), 30 minutes, and 60 minutes (end of exercise). The maximum core temperature (Tc max) for each subject from all 3 readings (baseline, 30 minutes, and 60 minutes) was determined, and those data are summarized in Table 2. For each group and condition combination, mean and standard deviation Tc max are presented as well as percent of participants in that condition who had a Tc max that exceeded 37.8°C, 38.3°C, and 38.9°C. Virtually all participants (all SCI and 16 of 19 AB) experienced EIH with Tc max >37.8°C, whereas 83% of all TPs reached Tc >38.9°C (in either NV or V condition) and thus approached the heat stroke criterion as defined for the AB population (>40°C). Despite this, no participant terminated participation early or demonstrated symptoms of heat exhaustion or heat stroke by ACSM criteria.9
Table 2. Means (SD) for Tc max over the entire 60-minute duration for all groups and conditions, and percent of subjects in each group/condition who had a Tc max greater than 37.8°C, 38.3°C, and 38.9°C.
|
%Tc
max |
||||
|---|---|---|---|---|
| Group /condition | Mean (SD) | >37.8°C | >38.3°C | >38.9°C |
| TP/NV | 38.9 (0.3) | 100% | 100% | 50.00% |
| TP/V | 39.0 (0.7) | 100% | 83.30% | 66.70% |
| HP/NV | 38.3 (0.2) | 100% | 40.00% | 0% |
| HP/V | 38.4 (0.5) | 100% | 20.00% | 20.00% |
| LP/NV | 38.4 (0.5) | 100% | 16.70% | 16.70% |
| LP/V | 38.4 (0.2) | 100% | 66.70% | 0% |
| AB/NV | 38.3 (0.4) | 84.20% | 36.80% | 5.30% |
| AB/V | 38.2 (0.4) | 78.90% | 36.80% | 0% |
Note: AB = able-bodied; HP = high paraglegia; LP = low paraplegia; NV = no vest; Tc = core body temperature; TP = tetraplegia; V = vest.
Descriptive statistics for all 4 groups, 2 vest conditions, and 3 measurement times are presented in Table 3. Analysis of the baseline measures indicated that, although there were no significant effects for vest or Group x Vest interaction, there was an initial difference among groups (P = .001), with the TP group (P = .004) and the LP group (P = .002) having a significantly higher baseline mean Tc than the AB group (see Figure 1). Analysis of Tc after 30 minutes of exercise revealed no significant effects due to group, vest, or Group x Vest interaction. Analysis of Tc after 60 minutes of exercise indicated no effect for vest or the Vest x Group interaction, but there was a significant main effect due to group (P = .004), with the TP group having significantly higher Tc than the AB group (P = .007) and the HP group (P = .03).
Table 3. Means (SD) for Tc for all groups and conditions and changes in Tc over time.
| Group/condition | Baseline (0 min) | 30 min | 60 min | Delta (0→30 min) | Delta (0→60 min) |
|---|---|---|---|---|---|
| TP/NV TP/V |
37.9 (0.7) 38.0 (0.9) |
38.3 (0.7) 38.7 (0.9) |
38.9 (0.3) 39.0 (0.7) |
0.4 (1.2) 0.8 (0.6) |
1.0 (0.8) 1.1 (0.8) |
| HP/NV HP/V |
37.4 (0.7) 37.8 (0.5) |
38.2 (0.3) 38.1 (0.7) |
37.8 (0.4) 38.1 (0.3) |
0.8 (0.7) 0.3 (0.9) |
0.4 (1.1) 0.3 (0.7) |
| LP/NV LP/V |
37.9 (0.3) 38.1 (0.3) |
38.2 (0.7) 38.3 (0.3) |
38.3 (0.4) 38.4 (0.2) |
0.2 (0.7) 0.2 (0.4) |
0.4 (0.5) 0.3 (0.4) |
| AB/NV AB/V |
37.3 (0.5) 37.2 (0.7) |
38.2 (0.4) 38.1 (0.4) |
38.0 (0.8) 38.0 (0.5) |
0.9 (0.6) 0.9 (0.6) |
0.8 (1.0) 1.6 (1.2) |
Note: AB = able-bodied; HP = high paraglegia; LP = low paraplegia; NV = no vest; Tc = core body temperature; TP = tetraplegia; V = vest.
Figure 1. Mean core temperatures for all 4 groups at all intervals averaged across the 2 vest conditions. AB = able-bodied; HP = high paraglegia; LP = low paraplegia; TP = tetraplegia.
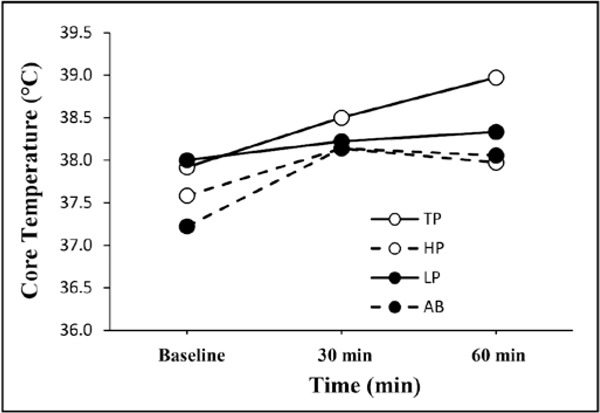
Analysis of difference scores in Tc from baseline to 30 minutes revealed no effect for vest or Group x Vest interaction, but there was a significant effect due to group (P = .041). The only pairwise comparison that approached significance was between the LP group and the AB group (P = .057), with a larger initial increase for the AB group than the LP group. Analysis of the changes in Tc from baseline to 60 minutes indicated no significant effects for group, vest, or Group x Vest interaction.
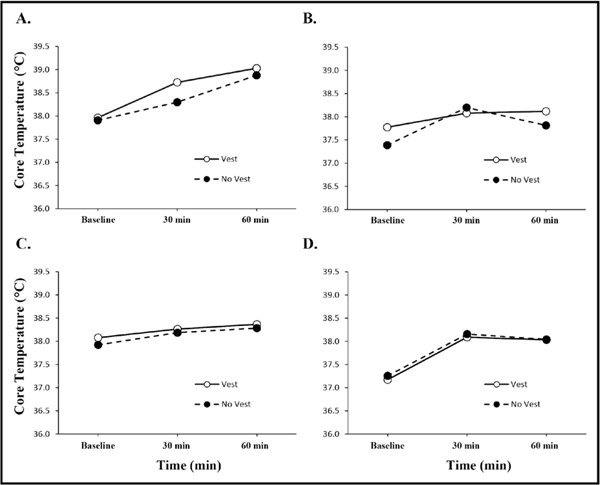
To further assess any possible effects due to wearing the vest, Tc for the V and NV conditions was assessed separately for each group across the 3 measurement times (any significant main or interaction effect for vest would be interpreted as an indication that wearing the vest affected core temperature). One analysis was conducted for each frame shown in Figure 2. For the TP group, there was a significant increase in Tc over time (P = .009), but no significant effect for vest or Vest x Time interaction. For the LP and HP groups, there were no effects for time, vest, or Time x Vest interaction. For the AB group, there was a significant effect due to time (P = .001), but no significant effects for vest or Vest x Time interaction.
Figure 2. Mean core temperatures for the vest and no vest conditions for all 4 groups at baseline, 30 minutes, and 60 minutes. A = tetraplegia group; B = high paraplegia group; C = low paraplegia group; D = able-bodied group.
Only 5 of the 17 athletes with SCI returned the surveys after the study. Although this was a low return rate (29%), there was consensus (4 of 5; P = .156) that the cooling vest was bulky and/or heavy and, therefore, it did impact their physical performance. Three of the 5 respondents (P = .313) reported feeling subjectively cooler with the vest.
Limitations
The main limitation of the study is that we did not document autonomic completeness of SCI for each subject. There is evidence that in AIS A persons, some autonomic function can remain intact, however we did not document this.34,35 Other limitations include uncontrolled exercise intensity, variable fluid intake, uncontrolled humidity of the environment, and variable body fat percentage of all participants. Medication lists were not gathered to determine any significant difference in Tc in persons taking anticholinergics, narcotics, or other prescription drugs. Finally, although AB athletes were counterbalanced, with half undergoing the NV protocol first and the other half undergoing the V protocol first, participants with SCI were not counterbalanced as there was little reason to expect any carryover of effect from the NV to V condition 1 week later.
Discussion
To our knowledge, this is the largest study examining the effect of a cooling intervention in a combined population of persons with tetraplegia and paraplegia (N = 17) in a field-based environment. This study supports prior investigations demonstrating that individuals with tetraplegia reach significantly higher Tc during exercise when compared to individuals with paraplegia.1–4,36 More than half of the TP group and 0% to 20% of the paraplegia group (HP, LP) reached a Tc max >38.2°C. Although ACSM and Sawka report considerable attrition from exercise in AB persons when Tc >40°C, Saboisky observed this at the lower temperature of 38.8°C. 9,37,38 Meanwhile in SCI athletes, Webborn noted volitional termination of exercise at T c >39°C.25 Although 83% of the TP group reached this Tc max >39°C in either condition (NV, V), none demonstrated symptoms consistent with heat-related illness and none terminated exercise prematurely. The critical Tc for heat stroke is 40°C for an individual without impairments to the autonomic nervous system, so future studies are necessary to establish a Tc for heat stroke in persons with impaired autonomic function as in SCI.7,9 It is unclear whether the critical Tc for heat stroke in persons with SCI is also 40°C, as there is a lack of data reporting incidence of heat-related illness in SCI. Many of the symptoms of heat stroke are due to dehydration. The TP groups have significantly impaired sudomotor activity that may be protective against dehydration, so this may explain why the TP group did not have any symptoms.9,39 The danger is that the lack of heat-related illness symptoms may not always result in cessation of exercise, and organ systems may be harmed as Tc rises.
The results also provide information to health care providers about the potential for EIH and heat-related illness in SCI athletes. It should be noted that the main source of heat gain during exercise was internal from metabolically active muscles rather than from the external ambient environment, as the gym was 21.1°C to 23.9°C. If this study were replicated under high ambient heat, Tc would likely be higher – with the largest effect likely seen in the TP group. Finally, the descriptive data emphasize the need to educate athletes with SCI about their increased risk of EIH and heat-related illness in neutral and heated environments.
Efficacy of the cooling vest
The vest was chosen for its ability contact a large skin surface area to maximize conductive cooling. In the SCI literature, vests composed of ice and gel have been tested. Ice vests (0°C) can cause local cutaneous vasoconstriction that may impair the ability of the body to dissipate heat through convective cooling and predispose insensate skin to breakdown. RPCM vests (a specific gel vest, as used in this study) have the ability to remain solid at higher temperatures (>10°C) than ice vests and thus are less likely to cause local vasoconstriction or skin breakdown.27
The cooling vest showed no significant effect on Tc in any group (TP, HP, LP, AB) or condition. There was a significant difference (P < .001) in mean baseline temperatures between persons with (namely the TP and LP groups) and without SCI. This reflects the impairment of heat dissipation from environmental heat gains in persons with SCI. We suspect this was due to the time of year the data were collected, which was mid Spring (April and May) to Summer (June, July, August). Average high temperatures in San Antonio in April and May are 27.2°C and 30.6°C, respectively, whereas high temperatures in June, July, and August are 33.3°C, 35°C, 35.6°C, respectively. Maximum daily temperatures often exceed 37.8°C in the summer months, with high relative humidity >50% in all months. The phenenomenon where the core temperature varies directly with ambient thermal conditions is known as partial poilikothermia and has been consistently observed in persons with SCI and documented extensively in the literature.39–43 It is possible that the athletes’ resting daytime Tc during these months could be hyperthermic due to partial poikilothermia. On the other hand, baseline Tc of the AB group was closer to physiologic resting Tc due to their improved physiologic ability to dissipate environmental heat gain.
Furthermore, as hypothesized, the mean change in temperature during exercise was higher in the TP group compared to the HP and LP groups. Even though change in temperature was greater in the TP group, it was not statistically significant. This is likely due to small sample size, and it may have been potentially skewed by the higher baseline temperatures from partial poikilothermia. This finding of greater change in Tc in the TP group during exercise has been documented as statistically significant in a more temperaturecontrolled lab setting.4
An unanticipated finding was that the mean change in Tc from 0 to 60 minutes was most similar between the TP and AB groups. However, in the AB group, the rate of change over time was greatest from 0 to 30 minutes and plateaued at 30 to 60 minutes, whereas the rate of change over time was consistent (almost linear) in the TP group from 0 to 60 minutes. Although their baseline Tc was on average 0.7°C different, the similar delta suggests a similar internal heat gain due to the exercise. Given that the AB group has a fully intact sympathetic nervous system, we would anticipate very little change in Tc with exercise (similar or less than the delta of the HP and LP groups). One study showed that athletes with paraplegia (HP, LP groups) retain enough ability to sweat and distribute heat to their lower extremities that their risk of complications associated with increased body temperature is no greater than the risk to AB athletes.36,44 The AB delta could be larger than the HP and LP groups in our study due to the lack of training with wheelchair propulsion causing decreased efficiency, increased energy expenditure, and impaired heat dissipation compared to the HP and LP athletes who are well conditioned to wheelchair propulsion.45 Whereas the AB delta may be higher than anticipated due to lack of training and lower efficiency with wheelchair propulsion, the TP delta more likely reflects true physiologic impaired heat dissipation given they were well trained in the sport.
Previous research has indicated that a cooling vest placed on AB individuals during exercise reduces thermal strain through decreasing skin temperature, Tc, and sweat loss.14,23,24,28,46–48 We could not reproduce this effect on Tc in our AB athletes. This could be a result of the vest precluding evaporative cooling (evaporation of sweat), lack of control for exercise intensity in all groups, peripheral vasoconstriction in the skin due to the cold vest temperature (though less likely), or lack of precooling with the vest as done in the studies by Hasegawa and Chou that reported positive results.23,28,49,50
Despite the lack of objective evidence for efficacy of the cooling vest on Tc, 3 of the 5 SCI athletes who responded to the mail survey reported feeling subjectively cooler with the vest. Although we do not have the information on the level of injury of each respondent (anonymous survey), one explanation is that persons with paraplegia have more intact chest skin sensation resulting in ascending afferent input of the conductive cooling. Because we did not monitor skin temperature, we cannot validate this hypothesis.
This effect of subjective cooling from external cooling devices without a change in Tc has previously been demonstrated. Goosey-Tolfrey et al51 reported that cooling garments had the counterproductive effect of decreasing thermal strain and causing inadequate fluid rehydration. Meanwhile, artificial sweat was found to be ineffective at reducing Tc in persons with paraplegia who subjectively “felt” cool from the intervention.22 Increase in Tc that is “masked” by subjective cooling (via vest, cooling garments, or artificial sweat) could prevent rehydration. This subjective cooling sensation could be dangerous, as it may result in athletes working harder or longer, creating a further rise in Tc and increasing the risk of EIH, heat-related illness, or even cardiac arrest. This possibility suggests that persons with SCI should use caution when wearing cooling devices that decrease subjective thermal strain but not Tc.
Conclusion
This study demonstrated that after 60 minutes of exercise, persons with tetraplegia have a significantly higher rise in Tc than HP or AB athletes and thus are at the highest risk of EIH and heat-related illness. Furthermore, the cooling vest was not effective at attenuating this rise in Tc in any group. Despite limitations of this investigation, the lack of significant findings brings into question the effectiveness of a cooling vest used in the field.
Improved understanding of the extent of thermo-dysregulation in persons with SCI will educate clinicians and athletes about the risk of EIH and heat-related illness and equip them to deal with the issue. Establishing the efficacy of specific cooling techniques in persons with SCI could improve safety and performance with exercise.
Acknowledgments
The authors declare no conflicts of interest. Financial support: Foundation for Physical Medicine and Rehabilitation, Paralyzed Veterans of America.
Additional contributions: The following persons contributed their professional support during this project: Nicholas Walsh, MD, PM&R Program Director, UTHSCSA, and Jenny Kiratli, PhD, Director Clinical Research, SCI Center, VA Palo Alto HCS. The following UTHSCAaffiliated students also provided technical support: UTHSCSA physical therapy students Vera Chavez, Kurt Dinkle, Randy Elizondo, and Ofelia Serrata and UTHSCSA medical students Delisa Guadarramma and Andrew Hsu.
References
- 1.Guttmann L, Silver J, Wyndham CH. Thermoregulation in spinal man. J Physiol. 1958;142(3):406–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price MJ. Thermoregulation during exercise in individuals with spinal cord injuries. Sports Med. 2006;36(10):863–879 [DOI] [PubMed] [Google Scholar]
- 3.Petrofsky JS. Thermoregulatory stress during rest and exercise in heat in patients with a spinal cord injury. Eur J Appl Physiol Occup Physiol. 1992;64(6):503–507 [DOI] [PubMed] [Google Scholar]
- 4.Price MJ, Campbell IG. Effects of spinal cord lesion level upon thermoregulation during exercise in the heat. Med Sci Sports Exerc. 2003;35(7):1100–1107 [DOI] [PubMed] [Google Scholar]
- 5.Price MJ, Campbell IG. Thermoregulatory responses of paraplegic and able-bodied athletes at rest and during prolonged upper body exercise and passive recovery. Eur J Appl Physiol Occup Physiol. 1997;76(6):552–560 [DOI] [PubMed] [Google Scholar]
- 6.Chila AG, American Osteopathic Association. Foundations of Osteopathic Medicine (3rd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011 [Google Scholar]
- 7.Binkley HM, Beckett J, Casa DJ, Kleiner DM, Plummer PE. National Athletic Trainers’ Association Position Statement: Exertional heat illnesses. J Athl Train. 2002;37(3):329–343 [PMC free article] [PubMed] [Google Scholar]
- 8.Gonzalez-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol. 1999;86(3):1032–1039 [DOI] [PubMed] [Google Scholar]
- 9.Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand. Exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572 [DOI] [PubMed] [Google Scholar]
- 10.Armstrong LE, Crago AE, Adams R, Roberts WO, Maresh CM. Whole-body cooling of hyperthermic runners: Comparison of two field therapies. Am J Emerg Med. 1996;14(4):355–358 [DOI] [PubMed] [Google Scholar]
- 11.Clements JM, Casa DJ, Knight J, et al. Ice-water immersion and cold-water immersion provide similar cooling rates in runners with exercise-induced hyperthermia. J Athl Train. 2002;37(2):146–150 [PMC free article] [PubMed] [Google Scholar]
- 12.Smith JE. Cooling methods used in the treatment of exertional heat illness. Br J Sports Med. 2005;39(8):503-507; discussion 507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giesbrecht GG, Jamieson C, Cahill F. Cooling hyperthermic firefighters by immersing forearms and hands in 10°C and 20°C water. Aviat Space Environ Med. 2007;78(6):561–567 [PubMed] [Google Scholar]
- 14.Duffield R, Dawson B, Bishop D, Fitzsimons M, Lawrence S. Effect of wearing an ice cooling jacket on repeat sprint performance in warm/humid conditions. Br J Sports Med. 2003;37(2):164–169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khomenok GA, Hadid A, Preiss-Bloom O, et al. Hand immersion in cold water alleviating physiological strain and increasing tolerance to uncompensable heat stress. Eur J Appl Physiol. 2008;104(2):303–309 [DOI] [PubMed] [Google Scholar]
- 16.Bennett BL, Hagan RD, Huey KA, Minson C, Cain D. Comparison of two cool vests on heat-strain reduction while wearing a firefighting ensemble. Eur J Appl Physiol Occup Physiol. 1995;70(4):322–328 [DOI] [PubMed] [Google Scholar]
- 17.Castle PC, Macdonald AL, Philp A, Webborn A, Watt PW, Maxwell NS. Precooling leg muscle improves intermittent sprint exercise performance in hot, humid conditions. J Appl Physiol. 2006;100(4):1377–1384 [DOI] [PubMed] [Google Scholar]
- 18.Armstrong LE, Maresh CM, Riebe D, et al. Local cooling in wheelchair athletes during exercise-heat stress. Med Sci Sports Exerc. 1995;27(2):211–216 [PubMed] [Google Scholar]
- 19.Webborn N, Price MJ, Castle PC, Goosey-Tolfrey VL. Effects of two cooling strategies on thermoregulatory responses of tetraplegic athletes during repeated intermittent exercise in the heat. J Appl Physiol. 2005;98(6):2101–2107 [DOI] [PubMed] [Google Scholar]
- 20.Hagobian TA, Jacobs KA, Kiratli BJ, Friedlander AL. Foot cooling reduces exercise-induced hyperthermia in men with spinal cord injury. Med Sci Sports Exerc. 2004;36(3):411–417 [DOI] [PubMed] [Google Scholar]
- 21.Goosey-Tolfrey V, Swainson M, Boyd C, Atkinson G, Tolfrey K. The effectiveness of hand cooling at reducing exercise-induced hyperthermia and improving distance-race performance in wheelchair and able-bodied athletes. J Appl Physiol. 2008;105(1):37–43 [DOI] [PubMed] [Google Scholar]
- 22.Pritchett RC, Bishop PA, Yang Z, et al. Evaluation of artificial sweat in athletes with spinal cord injuries. Eur J Appl Physiol. 2010;109(1):125–131 [DOI] [PubMed] [Google Scholar]
- 23.Hasegawa H, Takatori T, Komura T, Yamasaki M. Wearing a cooling jacket during exercise reduces thermal strain and improves endurance exercise performance in a warm environment. J Strength Cond Res. 2005;19(1):122–128 [DOI] [PubMed] [Google Scholar]
- 24.Doerr DF. Divers unlimited suit heat stress assessment and a countermeasure [abstract]. Kennedy Space Center, FL: Biomedical Laboratory; November1997 [Google Scholar]
- 25.Webborn N, Price MJ, Castle P, Goosey-Tolfrey VL. Cooling strategies improve intermittent sprint performance in the heat of athletes with tetraplegia. Br J Sports Med. 2010;44(6):455–460 [DOI] [PubMed] [Google Scholar]
- 26.Goosey-Tolfrey VL, Leicht CA. Field-based physiological testing of wheelchair athletes. Sports Med. 2013;43(2):77–91 [DOI] [PubMed] [Google Scholar]
- 27.House JR, Lunt HC, Taylor R, Milligan G, Lyons JA, House CM. The impact of a phase-change cooling vest on heat strain and the effect of different cooling pack melting temperatures [published online ahead of print November 15, 2012]. Eur J Appl Physiol. [DOI] [PubMed] [Google Scholar]
- 28.Chou C, Tochihara Y, Kim T. Physiological and subjective responses to cooling devices on firefighting protective clothing. Eur J Appl Physiol. 2008;104(2):369–374 [DOI] [PubMed] [Google Scholar]
- 29.Sparling PB, Snow TK, Millard-Stafford ML. Monitoring core temperature during exercise: Ingestible sensor vs. rectal thermistor. Aviat Space Environ Med. 1993;64(8):760–763 [PubMed] [Google Scholar]
- 30.O’Brien C, Hoyt RW, Buller MJ, Castellani JW, Young AJ. Telemetry pill measurement of core temperature in humans during active heating and cooling. Med Sci Sports Exerc. 1998;30(3):468–472 [DOI] [PubMed] [Google Scholar]
- 31.Mittal BB, Sathiaseelan V, Rademaker AW, Pierce MC, Johnson PM, Brand WN. Evaluation of an ingestible telemetric temperature sensor for deep hyperthermia applications. Int J Radiat Oncol Biol Phys. 1991;21(5):1353–1361 [DOI] [PubMed] [Google Scholar]
- 32.Byrne C, Lim CL. The ingestible telemetric body core temperature sensor: A review of validity and exercise applications. Br J Sports Med. 2007;41(3):126–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gonzalez EG, Myers SJ, Edelstein JE, Lieberman JS, Downey JA. Downey and Darling’s Physiological Basis of Rehabilitation Medicine (3rd ed.). Waltham, MA: Butterworth Heinemann; 2001 [Google Scholar]
- 34.Mills PB, Krassioukov A. Autonomic function as a missing piece of the classification of paralympic athletes with spinal cord injury. Spinal Cord. 2011;49(7):768–776 [DOI] [PubMed] [Google Scholar]
- 35.Curt A, Weinhardt C, Dietz V. Significance of sympathetic skin response in the assessment of autonomic failure in patients with spinal cord injury. J Auton Nerv Syst. 1996;61(2):175–180 [DOI] [PubMed] [Google Scholar]
- 36.Olive JL, McCully KK, Dudley GA. Blood flow response in individuals with incomplete spinal cord injuries. Spinal Cord. 2002;40(12):639–645 [DOI] [PubMed] [Google Scholar]
- 37.Saboisky J, Marino FE, Kay D, Cannon J. Exercise heat stress does not reduce central activation to non-exercised human skeletal muscle. Exp Physiol. 2003;88(6):783–790 [DOI] [PubMed] [Google Scholar]
- 38.Sawka MN, Young AJ, Latzka WA, Neufer PD, Quigley MD, Pandolf KB. Human tolerance to heat strain during exercise: Influence of hydration. J Appl Physiol. 1992;73(1):368–375 [DOI] [PubMed] [Google Scholar]
- 39.Downey JA, Huckaba CE, Kelley PS, Tam HS, Darling RC, Cheh HY. Sweating responses to central and peripheral heating in spinal man. J Appl Physiol. 1976;40(5):701–706 [DOI] [PubMed] [Google Scholar]
- 40.Guttmann L. Reflection on the 1976 Toronto Olympiad for the physically disabled. Paraplegia. 1976;14(3):225–240 [DOI] [PubMed] [Google Scholar]
- 41.Downey JA, Darling RC, Chiodi HP. The response of tetraplegia patients to cold. Arch Phys Med Rehabil. 1967;48(12):645–649 [PubMed] [Google Scholar]
- 42.Downey JA, Chiodi HP, Darling RC. Central temperature regulation in the spinal man. J Appl Physiol. 1967;22(1):91–94 [DOI] [PubMed] [Google Scholar]
- 43.Downey JA, Huckaba CE, Myers SJ, Darling RC. Thermoregulation in the spinal man. J Appl Physiol. 1973;34(6):790–794 [DOI] [PubMed] [Google Scholar]
- 44.Price M, Goosey-Tolfrey V. Heat flow of the paraplegic and able-bodied lower limb during resting heat exposure. J Therm Biol. 2008;33(4):255–260 [Google Scholar]
- 45.Havenith G, van Middendorp H. The relative influence of physical fitness, acclimatization state, anthropometric measures and gender on individual reactions to heat stress. Eur J Appl Physiol Occup Physiol. 1990;61(5-6):419–427 [DOI] [PubMed] [Google Scholar]
- 46.Kenny GP, Schissler AR, Stapleton J, et al. Ice cooling vest on tolerance for exercise under uncompensable heat stress. J Occup Environ Hyg. 2011;8(8):484–491 [DOI] [PubMed] [Google Scholar]
- 47.Gao C, Kuklane K, Holmer I. Cooling vests with phase change materials: The effects of melting temperature on heat strain alleviation in an extremely hot environment. Eur J Appl Physiol. 2011;111(6):1207–1216 [DOI] [PubMed] [Google Scholar]
- 48.Muir IH, Bishop PA, Ray P. Effects of a novel icecooling technique on work in protective clothing at 28°C, 23°C, and 18°C WBGTs. Am Ind Hyg Assoc J. 1999;60(1):96–104 [DOI] [PubMed] [Google Scholar]
- 49.Lopez RM, Cleary MA, Jones LC, Zuri RE. Thermoregulatory influence of a cooling vest on hyperthermic athletes. J Athl Train. 2008;43(1):5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barwood MJ, Newton PS, Tipton MJ. Ventilated vest and tolerance for intermittent exercise in hot, dry conditions with military clothing. Aviat Space Environ Med. 2009;80(4):353–359 [DOI] [PubMed] [Google Scholar]
- 51.Goosey-Tolfrey VL, Diaper NJ, Crosland J, Tolfrey K. Fluid intake during wheelchair exercise in the heat: Effects of localized cooling garments. Int J Sports Physiol Perform. 2008;3(2):145–156 [DOI] [PubMed] [Google Scholar]


