Abstract
Background
Cancer is the number one cause of death among men in China. Cigarette smoking is the most preventable cause of cancer. Data on the impact of continued smoking after cancer diagnosis on survival of cancer patients are sparse.
Methods
We studied the association between post-diagnosis smoking and risk of all-cause death among 1,632 incident cancer patients in the Shanghai Cohort Study, a population-based prospective cohort of 18,244 men in Shanghai. The change of smoking status after baseline interview was ascertained through annual in-person interviews. Cox proportional hazards regression models were used to estimate hazard ratio (HR) and 95% confidence interval (CI) for all-cause mortality associated with change in smoking status.
Results
Patients who continued smoking after cancer diagnosis experienced a statistically significant 59% (95% CI = 36–86%) increase in risk of death compared with cancer patients who did not smoke after cancer diagnosis. Among current smokers at cancer diagnosis, HRs (95% CIs) were 1.79 (1.49–2.16) in all cancer patients, 2.36 (1.63–3.42) in lung cancer patients, 1.63 (0.98–2.73) in stomach cancer patients, 2.31 (1.40–3.81) in colorectal cancer patients, and 2.95 (1.09–7.95) in bladder cancer patients who continued smoking compared with their counterparts who stopped smoking after cancer diagnosis.
Conclusion
Post-diagnosis cigarettes smoking significantly increased the risk of death for male cancer patients.
Impact
These data provide new information regarding smoking and cancer survival, which should inform future research into the contextual and individual-level barriers that may result in inadequate attention of smoking among cancer patients in the post-diagnosis setting.
Introduction
Cancer is the 1st and 2nd leading cause of death for men in China and the U.S., respectively (1, 2). Tobacco use is the most important recognized cause of cancer-related death (3). Among patients diagnosed with smoking-related cancers, smoking is attributable to 50% of the total mortality for men in China and 70% in the U.S. (4, 5). Strong evidence demonstrates the association between cigarette-smoking and increased cancer risk, as well as substantial health benefits as a result of smoking cessation (6–9). However, the impact of smoking after cancer diagnosed is not well studied. Existing evidence about impact of post-diagnosis smoking understandably focuses on treatment-related outcomes in lung or head and neck cancer patients, for whom smoking is an established strong cause. A few hospital-based studies found improved short-term survival in early staged lung cancer patients who quit smoking after diagnosis compared with persistent smokers (10, 11), while others did not detect such difference (12–19). The impact of post diagnosis smoking on long-term survival in cancer patients is even less clear.
The advancement of modern technology for early detection and the innovations of therapies for cancer patients resulted in increasing numbers of survivors and prolonged life expectancy after cancer occurrence. However, only a fraction of cancer patients received formal smoking cessation counseling (20). As a consequence, there is considerable room for improvement with regard to tobacco control in the post-diagnosis setting for the growing population of cancer survivors. In the present study, taking advantage of the population-based prospective cohort of Chinese men with 25 years of follow-up, we examined the association between post-cancer diagnosis smoking and overall survival in all cancer patients as well as patients with specific types of cancers including lung, stomach, colorectal, urinary bladder, and prostate. The aim of the study is to provide evidence for healthcare providers, patients and family, and policy makers of the impact of post-diagnosis smoking on survival after cancer, and to assist in addressing the critical issue of tobacco control in cancer survivorship.
Materials and Methods
The Shanghai Cohort Study
The Shanghai Cohort Study is a prospective cohort study investigating the association between lifestyle characteristics and risk of cancer development among middle-age or older men in Shanghai, China. The cohort has been followed for 25 years by the end of 2010. Detailed methods for subject recruitment and data collection have been previously published (21, 22). Briefly, all male residents between the ages of 45 and 64 years and resided in one of four geographically defined communities in Shanghai with no prior history of cancer were invited to participate in the study. Between January 1, 1986 and September 30, 1989, 18,244 men enrolled in the study. At enrollment, each participant completed an in-person interview using a structured questionnaire to obtain demographic information, history of tobacco and alcohol use, information of usual adult diet, and medical history.
Identification of incident cancer cases and deaths among cohort participants has been accomplished via linkage analysis of the cohort database with the population-based Shanghai Cancer Registry and Shanghai Municipal Vital Statistics Office databases. Surviving cohort members have been contacted in-person annually. A study staff member visited the last known address of each surviving cohort member to administer the follow-up questionnaire. Medical histories including treatment received for cancer patients were also updated. As of July 2010, the cutoff date for case ascertainment for the present study, 550 (3.0%) original cohort participants were lost to annual follow-up interview. In addition, 492 (2.7%) subjects refused request for annual follow-up interviews. The cancer and vital status of these subjects were ascertained through record linkage analysis only.
Assessment of smoking status
At the baseline interview, nurse interviewers asked each participant about whether he had ever smoked one or more cigarettes per day for 6 months or longer. Among smokers, information of age at smoking initiation, current smoking status, number of cigarettes smoked per day, and number of years of smoking was obtained. For those who had quit smoking at the baseline, additional information on age at quitting was recorded. After the baseline interview, information of smoking status and number of cigarettes per day during the preceding years were collected in all surviving cohort members during annual follow-up interviews. Total number of pack-years of cigarettes smoked before cancer diagnosis was defined as the cumulative year of smoking until cancer diagnosis multiplied by the average number of packs (20 cigarettes per pack) smoked per day for a given smoker.
We define lifetime never smokers as patients who never smoked cigarettes over their lifetime from the baseline interview until the last annual follow-up interview immediately preceding cancer diagnosis, whereas current smokers were those who reported currently smoking cigarettes during the past 6 months at the last follow-up before diagnosis. The remaining patients, who ever smoked at or before enrollment but no longer smoked cigarettes at the last follow-up before cancer diagnosis, were defined as former smokers.
Recognizing that the change in smoking status for a given patient occurred frequently from cancer diagnosis to death or latest follow-up interview that were ascertained at multiple annual follow-up interviews, we calculated a ratio (r) of the number of years of smoking divided by the total number of years survived after cancer diagnosis to reflect the true smoking status for each patient over the years. This ratio had a value ranged from 0 to 1 whereby 0 meant a patient never smoked cigarettes after diagnosis and 1 meant a patient continued to smoke until death or the latest follow-up interview. A value of r between 0 and 1 indicated a patient stopped smoking for some years during follow-up period after cancer diagnosis.
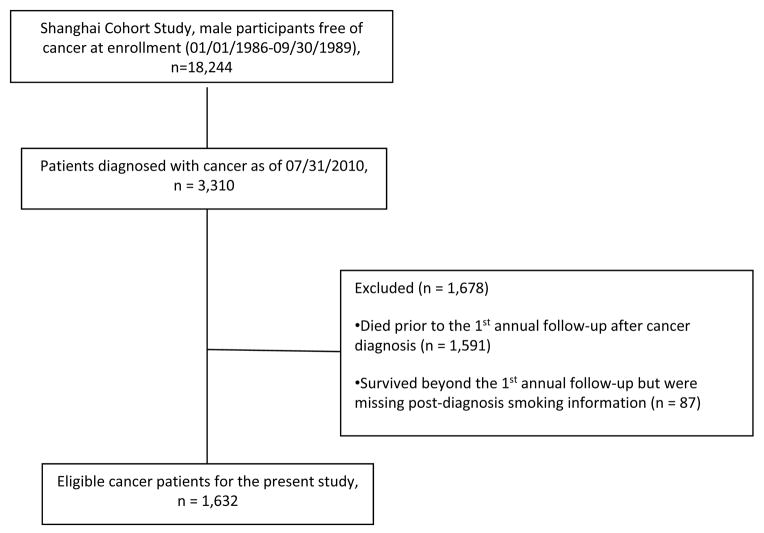
Statistical analysis
As of July 31, 2010, 3,310 participants of the Shanghai Cohort Study who were free of cancer at enrollment were diagnosed with cancer. Given our study’s primary interest of post-diagnosis smoking, patients who did not provide an updated smoking status after cancer diagnosis during annual follow-ups were ineligible. In addition, change on smoking status right after cancer diagnosis, especially during treatment course may have limited impact on the overall survival for patients who were dying within months. Therefore, 1,591 (48.1 %) patients died prior to their first annual follow-up interview after cancer diagnosis (on average 4.2 months of survival after cancer diagnosis), and an addition 87 (2.6%) patients who survived beyond the first follow-up but were not able to provide post-diagnosis smoking information were excluded from the study (Figure 1). The present study included 1,632 patients, 931 (57.1%) of whom died from any cause as of July 31, 2010. For each cancer patient, person-years at risk were calculated from the date of 1 year after cancer diagnosis to the date of death or the cut-off date (7/31/2010), whichever occurred first.
Figure 1.
Consort diagram for eligible cancer patients of the present study
To evaluate the impact of post-diagnosis smoking on mortality, we used Cox proportional hazards regression to estimate hazard ratios (HR) and associated 95% confidence intervals (CI). In addition, we developed a time-dependent variable which measured the current smoking status (yes or no) on a yearly basis after cancer diagnosis. Similar to the ratio (r), the time-dependent variable integrated the dynamic changes in smoking status over all annual follow-up interviews for a given patient after diagnosis (23). All Cox models included the following covariates: age at cancer diagnosis (continuous), level of education (less than primary school, middle school, and college or above), cumulative pack-years prior to cancer diagnosis (continuous), and the type of therapies (surgery, radiation and chemotherapy) that a patient received for cancer (yes or no for each therapy). The association between smoking status after diagnosis and risk of all-cause mortality was examined in all patients as well as patients with specific types of cancers including lung, stomach, colorectal, urinary bladder, and prostate. The Kaplan-Meier method and log-rank test were used to compare overall survival in smokers by smoking status after cancer diagnosis.
All statistical analyses were carried out using SAS software version 9.3 (SAS Institute, Cary, North Carolina). All P values reported are two-sided, and those that were <0.05 were considered to be statistically significant.
Results
With a mean follow-up of 5.3 (± 4.8) years after cancer diagnosis and a median survival time of 5.4 years, the mean age at diagnosis (± standard deviation) for all 1,632 eligible cancer patients in this cohort of Chinese men was 68.8 (±7.2) years. Table 1 shows that after adjustment for potential prognostic factors, the 545 patients who quit smoking before diagnosis (i.e., former smokers) and the 747 patients who were smoking at diagnosis (current smokers) had a comparable hazard ratio of death relative to the 340 lifelong nonsmokers. Among the total of 747 current smokers at diagnosis, 214 (28.6%) patients completely quitted smoking after diagnosis (r = 0) whereas 197 (26.4%) patients continued smoking persistently (r = 1). The remaining 336 (45.0%) patients smoked intermittently (0 < r < 1 or the median value of r = 0.47). The Spearman correlation coefficient between r and number of years of survival after cancer diagnosis was 0.09 (P = 0.17).
Table 1.
Selected characteristics and risk of death for cancer patients who had eligible post-diagnosis information on smoking status, by smoking status before and after cancer diagnosis, The Shanghai Cohort Study 1986–2010
| No. of Cases | No. of Deaths (%) | Person-years at risk* | Average Person-years* | Median Survival (year) | Average Age at Diagnosis | Received Surgery (%) | Received Chemotherapy (%) | Received Radiation Therapy (%) | HR† (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|
| All cancer patients | 1632 | 931(57.0%) | 6971 | 4.3 | 5.4 | 68.8 | 73.9 | 45.7 | 18.0 | |
| Lifetime never nonsmokers | 340 | 170(50.0%) | 1696 | 5.0 | 7.5 | 68.6 | 76.5 | 43.2 | 17.1 | 1.00 (reference) |
| Former smokers at cancer diagnosis | 545 | 270(49.5%) | 1944 | 3.6 | 5.9 | 71.4 | 76.9 | 44.2 | 14.3 | 0.97 (0.79–1.19) |
| Current smokers at cancer diagnosis | 747 | 491(65.7%) | 3331 | 4.5 | 4.2 | 67.0 | 70.5 | 47.9 | 21.2 | 1.13 (0.91–1.41) |
| Cancer patients who were current smokers at cancer diagnosis and survived until the next annual follow-up interview | ||||||||||
| Quitters after cancer diagnosis (r=0) | 214 | 120 (56.1%) | 696 | 3.3 | 4.4 | 68.9 | 74.3 | 51.9 | 12.6 | 1.00 (reference) |
| Intermittent smokers after cancer diagnosis (r >0 and r <1) | 336 | 223 (66.4%) | 2152 | 6.4 | 7.1 | 65.8 | 74.7 | 48.5 | 25.9 | 0.89 (0.70–1.12) |
| Continued smokers after cancer diagnosis (r=1) | 197 | 148 (75.1%) | 482 | 2.4 | 2.1 | 67.0 | 59.4 | 42.6 | 22.3 | 1.76 (1.37–2.27) |
Person-years at risk began at one year after cancer diagnosis (see details in the Methods)
All Cox models were adjusted for age at diagnosis (continuous), level of education (primary school, middle school, or college or above), cumulative number of pack-year of smoking prior to diagnosis (continuous), treatment modalities: surgery (yes/no), chemotherapy (yes/no), and radiation therapy (yes/no), and cancer site.
The median survival of patients who continued to smoke after diagnosis was 2.1 years, which was more than 50% shorter than quitters with a median survival of 4.4 years (Table 1). Among all current smokers at cancer diagnosis, the Kaplan-Meier curves showed that persistent smokers had inferior overall survival compared with quitters (Plog-rank = 0.009) and intermittent smokers (Plog-rank <0.001) (Figure 2). After adjusting for age at diagnosis, education, cumulative number of pack-years of pre-diagnosis smoking, cancer site, as well as treatment modalities, patients who continued smoking after cancer diagnosis persistently experienced a substantial 76% (95% CI = 37% – 127%) increased risk of death compared with patients who quit smoking and remained nonsmoking after cancer diagnosis. Although intermittent smokers were observed with higher median survival time (7.1 years) and better overall survival shown on the Kaplan-Meier curve, the lower hazard of death of these patients, compared with quitters, was not statistically significant after adjusting for age at diagnosis, cumulative exposure of smoking, and other prognostic factors (Table 1). This artificial effect could be explained by the fact that these patients were diagnosed at a younger age and smoked less before diagnosis (Supplemental Table 1).
Figure 2.
Kaplan-Meier survival curves by smoking status after cancer diagnosis for eligible cancer patients who were current smokers at diagnosis, the Shanghai Cohort Study 1986–2010
Table 2 shows HRs of death for all cancer patients and selected cancer-specific patients associated with the changing of smoking status after diagnosis using the time-dependent approach. For all patients, a statistically significant 59% (95% CI = 36% – 86%) increased mortality risk was associated with smoking relative to nonsmoking after cancer diagnosis. When analyzed separately for cancer-specific patients, the multivariate-adjusted HRs (95% CIs) of death for smoking relative to nonsmoking after cancer diagnosis was 1.92 (1.41–2.60) for lung cancer patients, 1.76 (1.11–2.79) for stomach cancer patients, 1.65 (1.14–2.38) for colorectal cancer patients, and 3.66 (1.56–8.60) for bladder cancer patients. Similar analyses for current smokers at cancer diagnosis revealed that smoking after cancer diagnosis was associated with a statistically significant 79% increased risk of death (95% CI = 49%–116%) relative to nonsmoking after cancer diagnosis for all patients. Among cancer-specific patients, the HRs (95% CIs) of death for smoking versus nonsmoking after cancer diagnosis was 2.36 (1.63–3.42) in lung cancer patients, 1.63 (0.98–2.73) in stomach cancer patients, 2.31 (1.40–3.81) in colorectal cancer patients, 2.95 (1.09–7.95) in bladder cancer patients, 2.27 (0.40–12.80) in prostate cancer patients, and 1.34 (0.96–1.80) in all other cancer patients. Hazard ratios for intermittent smokers relative to quitters varied by cancer site and were not statistically significant after adjusting for all potential prognostic factors (Table 2).
Table 2.
Time-dependent hazard ratio (95% confidence interval) of all-cause death for smoking after cancer diagnosis for all cancer patients and for current smokers at cancer diagnosis, by cancer sites, The Shanghai Cohort Study 1986–2010
| All patients | Lung Cancer | Stomach Cancer | Colorectal Cancer | Bladder Cancer | Prostate Cancer | Other Cancers | |
|---|---|---|---|---|---|---|---|
| All cancer patients | |||||||
| No. of cases | 1632 | 288 | 362 | 248 | 107 | 132 | 495 |
| No. of deaths (%) | 931(57.0%) | 229 (79.5%) | 159 (43.9%) | 152 (61.3%) | 40 (37.4%) | 47 (35.6%) | 304 (61.4%) |
| Person-years at risk | 6971 | 838 | 1805 | 1077 | 669 | 445 | 2137 |
| Average person-years | 4.3 | 2.9 | 5.0 | 4.3 | 6.3 | 3.4 | 4.3 |
| Average age at diagnosis | 68.8 | 68.1 | 69.6 | 67.9 | 69.2 | 73.3 | 67.9 |
| Median survival time (year) | 5.4 | 2.1 | 10.9 | 4.0 | 15.0 | 8.4 | 5.2 |
| HR (95%CI)-time dependent smoking status* | 1.59 (1.36–1.86) | 1.92 (1.41–2.60) | 1.76 (1.11–2.79) | 1.65 (1.14–2.38) | 3.66 (1.56–8.60) | 1.94 (0.79–4.73) | 1.17 (0.87–1.58) |
| Cancer Patients who were current smokers at cancer diagnosis and survived until the next annual follow-up interview | |||||||
| No. of cases | 747 | 184 | 135 | 114 | 49 | 32 | 233 |
| No. of deaths (%) | 491 (65.7) | 151 (82.1) | 72 (53.3%) | 73 (64.0%) | 23 (46.9%) | 15 (46.9%) | 157 (67.4%) |
| Person-years at risk | 3331 | 547 | 647 | 581 | 311 | 118 | 1126 |
| Average person-years | 4.5 | 3.0 | 4.8 | 5.1 | 6.4 | 3.7 | 4.8 |
| Average age at diagnosis | 67.0 | 66.9 | 69.4 | 65.4 | 67.7 | 70.1 | 65.9 |
| Median survival time (year) for all patients | 4.1 | 2.1 | 7.3 | 4.1 | 12.4 | 6.3 | 4.3 |
| Median survival time (year) for quitters (r=0) | 4.4 | 2.1 | 3.8 | 7.9 | N/A ‡ | 9.8 | 3.3 |
| Median survival time (year) for intermittent smokers (0<r<1.0) | 7.1 | 2.8 | 10.9 | 9.1 | 12.4 | 6.0 | 7.7 |
| Median survival time (year) for continued smokers (r=1) | 2.1 | 1.7 | 3.8 | 2.1 | 2.9 | 11.1 | 2.1 |
| HR (95%CI)-intermittent smokers vs.quitters † | 0.89 (0.70–1.12) | 0.91 (0.59–1.39) | 0.69 (0.38–1.27) | 1.35 (0.68–2.67) | 1.75 (0.28–11.01) | 2.88 (0.22–37.20) | 0.76 (0.49–1.17) |
| HR (95%CI)-continued smokers vs. quitters † | 1.76 (1.37–2.27) | 1.89 (1.18–3.02) | 1.36 (0.70–2.67) | 3.46 (1.69–7.10) | 17.29 (2.25–132.64) | 0.93 (0.08–11.24) | 1.49 (0.92–2.40) |
| HR (95%CI)-time dependent smoking status* | 1.79 (1.49–2.16) | 2.36 (1.63–3.42) | 1.63 (0.98–2.73) | 2.31 (1.40–3.81) | 2.95 (1.09–7.95) | 2.27 (0.40–12.80) | 1.34 (0.96–1.88) |
Derived from a yearly based time-dependent variable of smoking status (yes versus no) after cancer diagnosis with the adjustment for age at diagnosis (continuous), level of education (primary school, middle school, or college or above), cumulative number of pack-year of smoking prior to diagnosis (continuous), and treatment for cancer: surgery (yes/no), chemotherapy (yes/no), and radiation therapy (yes/no). Cox models for all patients were additionally adjusted for cancer site.
All Cox models were adjusted for age at diagnosis (continuous), level of education (primary school, middle school, or college or above), cumulative number of pack-year of smoking prior to diagnosis (continuous), and treatment modalities: surgery (yes/no), chemotherapy (yes/no), and radiation therapy (yes/no). Cox models for all patients were additionally adjusted for cancer site.
Median survival (50% of the patients died) was not reached in this group of bladder cancer patients.
Discussion
The present prospective study of 1,632 eligible male cancer patients in Shanghai, China demonstrated a substantial poorer prognosis for patients who continued smoking than those who quit after cancer diagnosis. Among the 747 current smokers at diagnosis, compared with patients who stopped smoking after diagnosis, those who continued smoking experienced a statistically significant 79% increased risk of mortality. In these smokers at diagnosis, patients diagnosed with lung, colorectal, or bladder cancers may have a more than 2 fold increased risk of death from all cause if they continued smoking after diagnosis.
Epidemiological studies evaluating the impact of smoking after cancer diagnosis on survival of cancer patients are sparse. A few hospital-based studies found no significant difference in survival rates between persistent smokers and quitters in surgically treated patients with lung cancer among smokers (12, 15, 18, 19), while others found poor survival rates in smokers at 2 years after diagnosis (11, 12). Overall, these studies involved small number of patients and suffered from cross-sectional or retrospective study designs with single assessment of smoking status after diagnosis or limited time period of follow-up. To our knowledge, the present study is the first population-based study with long-term follow-up for cancer survivors and multiple annual assessment of smoking status after diagnosis, and the first to report evidence on increase mortality associated with post-diagnosis smoking in many cancer sites. Findings of the present study underscore the importance of smoking cessation intervention on cancer patients that could improve their survival.
Several factors may contribute to the poor survival in cancer patients who continued to smoke after diagnosis. Studies showed that in lung or head and neck cancer patients, smoking after cancer diagnosis was associated with increased risks of unfavorable post-treatment consequences, including anesthesia and surgery complications, delayed wound healing, toxicity and side effects of treatment, immune suppression, infection, cancer recurrence, or occurrence of a second primary cancer (12, 18, 24–28). Lower quality of life, worse performance status, higher level of usual pain, and poorer general health and social functioning were also reported in smokers compared with nonsmokers (13, 29–31). These adverse outcomes are likely to render high mortality risk in patients who smoke. In addition, tobacco substances may continue to cause genetic mutations that lead to the progression of cancer via carcinogenic pathways (32), which explains the increased mortality risk in patients with smoking-related cancer (e.g., lung, stomach, colorectal, and bladder) but not in non-smoking-related cancers (e.g., prostate) in our study. In the present study, 85.8% of patient deaths occurred were due to the primary cancer. We found no association between post-diagnosis smoking and risk of death from cardiovascular (4.9% of deaths), respiratory (1.7% of deaths), and other diseases (data not shown). Therefore, it is highly likely that post-diagnosis smoking was associated with poor survival by exacerbating the tumor progression or response to cancer therapy.
Our findings provide important public health implications for cancer survivors, healthcare providers, and policy makers. After the diagnosis of cancer, smokers are expected to show great interest and motivation to quit smoking (33, 34). However, patients face tremendous physical, psychological, and social stresses (35) which result in no reduction of the smoking prevalence in cancer patients (36, 37), given smoking as a possible means for stress relief. Moreover, physicians are pessimistic to help patients quit smoking (38), especially to patients with smoking-related cancers that are believed it was too late to quit smoking given the smoking-induced damages had been occurred (39). In the U.S., less than 50% smokers received formal smoking cessation counseling at diagnosis, during treatment, or on follow-up visits (20). Therefore, there is noticeable room for the improvement of self-managed or healthcare provider-assisted smoking cessation in the clinical setting for cancer patients. Message of inferior survival associated with post-diagnosis smoking should be conveyed to patients and their families and included in guidelines and evidence-based clinical practices. In addition, smoking cessation is considered cost-effective in the general population (40) as well as for lung cancer patients who have had surgery (41). It is worth promoting effective and sufficient cancer-tolerable smoking cessation interventions and disease management strategies for cancer patients.
The major strength of the present study was that smoking status was recorded in the Shanghai Cohort Study at baseline and updated on an annual basis for all surviving cohort members. The prospective nature of the study with a large population-based samples plus long-term, almost complete follow-up for all cancer patients for their vital status provided an unbiased estimate of mortality for cancer patients. In addition, the time-dependent approach in the analysis captured the dynamic change of smoking on an annual basis over the years after cancer diagnosis.
In spite of the considerable strengths, the present analysis may be subject to potential limitations. One concern is the lack of information on factors especially the clinical extent of disease at diagnosis. In our study, comparable proportion of lifelong nonsmokers, former, and current smokers at diagnosis received surgical treatment and chemotherapy (Ps > 0.05, more data available in Supplemental Table 2). In all analyses, the type of treatments administered to cancer patients was adjusted, which would take into account the potential difference, to some extent, in cancer stage at diagnosis between patients who continued smoking and those who quit smoking after cancer diagnosis. The treatment data available in our study were limited and did not include information on aspects of quality, delays in the timing of care, whether treatment regimens were actually completed, or details on the specific types of surgery, radiation, or chemotherapy agents. Survival differences, especially those we observed between the intermittent smokers and quitters, in these aspects of treatment may exist and may result from either patient or healthcare system issues or from differences in tumor characteristics. Another limitation is that our study included only patients who survived one or more years after cancer diagnosis. Patients who died less than one year after cancer diagnosis (n = 1,591; median survival time = 4.2 months) were excluded from the present study due to lack of updated information on smoking status after cancer diagnosis. Therefore, the findings of the present study may be only applicable to cancer patients with at least one year survival after diagnosis.
In summary, our study shows that continued smoking after cancer diagnosis increased risk of all-cause death in male cancer patients in Shanghai, China by approximately 80%. In current smokers at diagnosis, patients diagnosed with lung, colorectal, or bladder cancers may experience a 2 fold increased risk of death if they continued smoking after diagnosis. These data provide new information regarding smoking and cancer survival, which should inform future research into the contextual and individual-level factors that may result in inadequate attention of smoking among cancer patients in the post-diagnosis setting. Our study provides strong support to a smoking cessation intervention program that targets cancer survivors.
Supplementary Material
Acknowledgments
The authors thank Drs. Beth Virnig, Karen Kuntz, Kristin Anderson, and David Radosevich for their critiques and comments on the draft of this manuscript. We also thank Ms. Xue-Li Wang of the Shanghai Cancer Institute for supervising the field work of the Shanghai Cohort Study, and the Shanghai Cancer Registry for assistance with identification of cancer outcomes in the Shanghai Cohort Study.
This work was supported by United States Public Health Service grants R01 CA034092, R01 CA129534 and R01 CA144034.
Footnotes
Disclosure of potential conflicts of interest:
No potential conflicts of interest were disclosed by the authors.
References
- 1.Tobacco smoke and involuntary smoking. IARC Monogr Eval Carcinog Risks Hum. 2004;83:1–1438. [PMC free article] [PubMed] [Google Scholar]
- 2.He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, et al. Major causes of death among men and women in China. The New England journal of medicine. 2005;353:1124–34. doi: 10.1056/NEJMsa050467. [DOI] [PubMed] [Google Scholar]
- 3.Stewart BW, Kleihues P. World Cancer Report 2003. IARC Press; 2003. [Google Scholar]
- 4.CDC. Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses --- United States, 2000–2004. MMWR. 2008;57:1226–8. [PubMed] [Google Scholar]
- 5.Gu D, Kelly TN, Wu X, Chen J, Samet JM, Huang JF, et al. Mortality attributable to smoking in China. The New England journal of medicine. 2009;360:150–9. doi: 10.1056/NEJMsa0802902. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. The Health Benefits of Smoking Cessation. U.S. Department of Health and Human Services. Public Health Service. Centers for Disease Control. Center for Chronic Disease Prevention and Health Promotion. Office on Smoking and Health; 1990. DHHS Publication No.(CDC) 90–8416. [Google Scholar]
- 7.Godtfredsen NS, Holst C, Prescott E, Vestbo J, Osler M. Smoking reduction, smoking cessation, and mortality: a 16-year follow-up of 19,732 men and women from The Copenhagen Centre for Prospective Population Studies. Am J Epidemiol. 2002;156:994–1001. doi: 10.1093/aje/kwf150. [DOI] [PubMed] [Google Scholar]
- 8.Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. Bmj. 2000;321:323–9. doi: 10.1136/bmj.321.7257.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Warren GW, Kasza KA, Reid ME, Cummings KM, Marshall JR. Smoking at diagnosis and survival in cancer patients. Int J Cancer. 2013;132:401–10. doi: 10.1002/ijc.27617. [DOI] [PubMed] [Google Scholar]
- 10.Sardari Nia P, Weyler J, Colpaert C, Vermeulen P, Van Marck E, Van Schil P. Prognostic value of smoking status in operated non-small cell lung cancer. Lung Cancer. 2005;47:351–9. doi: 10.1016/j.lungcan.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 11.Videtic GM, Stitt LW, Dar AR, Kocha WI, Tomiak AT, Truong PT, et al. Continued cigarette smoking by patients receiving concurrent chemoradiotherapy for limited-stage small-cell lung cancer is associated with decreased survival. J Clin Oncol. 2003;21:1544–9. doi: 10.1200/JCO.2003.10.089. [DOI] [PubMed] [Google Scholar]
- 12.Bergman B, Sorenson S. Smoking and effect of chemotherapy in small cell lung cancer. Eur Respir J. 1988;1:932–7. [PubMed] [Google Scholar]
- 13.Baser S, Shannon VR, Eapen GA, Jimenez CA, Onn A, Lin E, et al. Smoking cessation after diagnosis of lung cancer is associated with a beneficial effect on performance status. Chest. 2006;130:1784–90. doi: 10.1378/chest.130.6.1784. [DOI] [PubMed] [Google Scholar]
- 14.Nakaya N, Saito-Nakaya K, Akizuki N, Yoshikawa E, Kobayakawa M, Fujimori M, et al. Depression and survival in patients with non-small cell lung cancer after curative resection: a preliminary study. Cancer Sci. 2006;97:199–205. doi: 10.1111/j.1349-7006.2006.00160.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston-Early A, Cohen MH, Minna JD, Paxton LM, Fossieck BE, Jr, Ihde DC, et al. Smoking abstinence and small cell lung cancer survival. An association. Jama. 1980;244:2175–9. [PubMed] [Google Scholar]
- 16.Shiba M, Kohno H, Kakizawa K, Iizasa T, Otsuji M, Saitoh Y, et al. Ki-67 immunostaining and other prognostic factors including tobacco smoking in patients with resected nonsmall cell lung carcinoma. Cancer. 2000;89:1457–65. doi: 10.1002/1097-0142(20001001)89:7<1457::aid-cncr7>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 17.Saito-Nakaya K, Nakaya N, Fujimori M, Akizuki N, Yoshikawa E, Kobayakawa M, et al. Marital status, social support and survival after curative resection in non-small-cell lung cancer. Cancer Sci. 2006;97:206–13. doi: 10.1111/j.1349-7006.2006.00159.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tucker MA, Murray N, Shaw EG, Ettinger DS, Mabry M, Huber MH, et al. Second primary cancers related to smoking and treatment of small-cell lung cancer. Lung Cancer Working Cadre. J Natl Cancer Inst. 1997;89:1782–8. doi: 10.1093/jnci/89.23.1782. [DOI] [PubMed] [Google Scholar]
- 19.Yoshida T, Matsui K, Masuda N, Kusunoki Y, Takada M, Yana T, et al. Risk of second primary cancer in two-year survivors of small cell lung cancer. Nihon Kyobu Shikkan Gakkai Zasshi. 1996;34:741–6. [PubMed] [Google Scholar]
- 20.Burke L, Miller LA, Saad A, Abraham J. Smoking behaviors among cancer survivors: an observational clinical study. J Oncol Pract. 2009;5:6–9. doi: 10.1200/JOP.0912001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ross RK, Yuan JM, Yu MC, Wogan GN, Qian GS, Tu JT, et al. Urinary aflatoxin biomarkers and risk of hepatocellular carcinoma. Lancet. 1992;339:943–6. doi: 10.1016/0140-6736(92)91528-g. [DOI] [PubMed] [Google Scholar]
- 22.Yuan JM, Ross RK, Wang XL, Gao YT, Henderson BE, Yu MC. Morbidity and mortality in relation to cigarette smoking in Shanghai, China. A prospective male cohort study. Jama. 1996;275:1646–50. [PubMed] [Google Scholar]
- 23.Walker MS, Larsen RJ, Zona DM, Govindan R, Fisher EB. Smoking urges and relapse among lung cancer patients: findings from a preliminary retrospective study. Preventive medicine. 2004;39:449–57. doi: 10.1016/j.ypmed.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 24.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 25.Gritz ER, Dresler C, Sarna L. Smoking, the missing drug interaction in clinical trials: ignoring the obvious. Cancer Epidemiol Biomarkers Prev. 2005;14:2287–93. doi: 10.1158/1055-9965.EPI-05-0224. [DOI] [PubMed] [Google Scholar]
- 26.Silverman S, Jr, Gorsky M, Greenspan D. Tobacco usage in patients with head and neck carcinomas: a follow-up study on habit changes and second primary oral/oropharyngeal cancers. J Am Dent Assoc. 1983;106:33–5. doi: 10.14219/jada.archive.1983.0004. [DOI] [PubMed] [Google Scholar]
- 27.Vladimirov BS, Schiodt M. The effect of quitting smoking on the risk of unfavorable events after surgical treatment of oral potentially malignant lesions. Int J Oral Maxillofac Surg. 2009;38:1188–93. doi: 10.1016/j.ijom.2009.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Kawahara M, Ushijima S, Kamimori T, Kodama N, Ogawara M, Matsui K, et al. Second primary tumours in more than 2-year disease-free survivors of small-cell lung cancer in Japan: the role of smoking cessation. Br J Cancer. 1998;78:409–12. doi: 10.1038/bjc.1998.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duffy SA, Terrell JE, Valenstein M, Ronis DL, Copeland LA, Connors M. Effect of smoking, alcohol, and depression on the quality of life of head and neck cancer patients. Gen Hosp Psychiatry. 2002;24:140–7. doi: 10.1016/s0163-8343(02)00180-9. [DOI] [PubMed] [Google Scholar]
- 30.Asaph JW, Handy JR, Jr, Grunkemeier GL, Douville EC, Tsen AC, Rogers RC, et al. Median sternotomy versus thoracotomy to resect primary lung cancer: analysis of 815 cases. Ann Thorac Surg. 2000;70:373–9. doi: 10.1016/s0003-4975(00)01364-3. [DOI] [PubMed] [Google Scholar]
- 31.Daniel M, Keefe FJ, Lyna P, Peterson B, Garst J, Kelley M, et al. Persistent smoking after a diagnosis of lung cancer is associated with higher reported pain levels. J Pain. 2009;10:323–8. doi: 10.1016/j.jpain.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. pp. 221–353. [PubMed] [Google Scholar]
- 33.Gritz ER, Carr CR, Rapkin D, Abemayor E, Chang LJ, Wong WK, et al. Predictors of long-term smoking cessation in head and neck cancer patients. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 1993;2:261–70. [PubMed] [Google Scholar]
- 34.Gritz ER, Carr CR, Rapkin DA, Chang C, Beumer J, Ward PH. A smoking cessation intervention for head and neck cancer patients: trial design, patient accrual, and characteristics. Cancer Epidemiol Biomarkers Prev. 1991;1:67–73. [PubMed] [Google Scholar]
- 35.McBride CM, Ostroff JS. Teachable moments for promoting smoking cessation: the context of cancer care and survivorship. Cancer Control. 2003;10:325–33. doi: 10.1177/107327480301000407. [DOI] [PubMed] [Google Scholar]
- 36.Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2005;23:8884–93. doi: 10.1200/JCO.2005.02.2343. [DOI] [PubMed] [Google Scholar]
- 37.Coups EJ, Ostroff JS. A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Preventive medicine. 2005;40:702–11. doi: 10.1016/j.ypmed.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 38.Warren GW, Marshall JR, Cummings KM, Toll B, Gritz ER, Hutson A, et al. Practice patterns and perceptions of thoracic oncology providers on tobacco use and cessation in cancer patients. J Thorac Oncol. 2013;8:543–8. doi: 10.1097/JTO.0b013e318288dc96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.U.S. Department of Health and human Services. The Health Benefits of Smoking Cessation. U.S. Department of health and Human Services, Public Health Services, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. DHHS Publication No. (CDC) 90–8416. [Google Scholar]
- 40.Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA : the journal of the American Medical Association. 1997;278:1759–66. [PubMed] [Google Scholar]
- 41.Slatore CG, Au DH, Hollingworth W. Cost-effectiveness of a smoking cessation program implemented at the time of surgery for lung cancer. J Thorac Oncol. 2009;4:499–504. doi: 10.1097/JTO.0b013e318195e23a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.