Abstract
Background
The impact of overweight among men of reproductive-age may affect fertility. Abdominal fat, more than body mass index, is an indicator of higher metabolic risk, which seems to be involved in decreasing sperm quality.
This study aims to assess the relationship between abdominal fat and sperm DNA fragmentation and the effect of abdominal fat loss, among 6 men in subfertile couples.
Methods
Sperm DNA fragmentation, abdominal fat and metabolic and hormonal profiles were measured in the 6 men before and after dietary advices. Seminal oxidative stress and antioxidant markers were determined.
Results
After several months of a lifestyle program, all 6 men lost abdominal fat (patient 1: loss of 3 points of abdominal fat, patient 2: loss of 3 points, patient 3: loss of 2 points, patient 4: loss of 1 point, patient 5: loss of 4 points and patient 6: loss of 13 points). At the same time, their rate of sperm DNA fragmentation decreased: 9.5% vs 31%, 24% vs 43%, 18% vs 47%, 26.3% vs 66%, 25.4% vs 35% and 1.7% vs 25%. Also, an improvement in both metabolic (significant decrease in triglycerides and total cholesterol; p = 0.0139) and hormonal (significant increase in testosterone/oestradiol ratio; p = 0.0139) blood profiles was observed after following the lifestyle program. In seminal plasma, the amount of SOD2 has significantly increased (p = 0.0139) while in parallel carbonylated proteins have decreased. Furthermore, all spouses got pregnant. All pregnancies were brought to term.
Conclusion
This study shows specifically that sperm DNA fragmentation among men in subfertile couples could be affected by abdominal fat, but improvement of lifestyle factor may correct this alteration. The effect of specific abdominal fat loss on sperm quality needs further investigation. The reduction of oxidative stress may be a contributing factor.
Introduction
Infertility affects about 15% of couples in reproductive age. A male factor, usually of unknown origin, is involved in 40% of cases [1].
The high prevalence of overweight and obesity is significantly contributing to the overall burden of diseases worldwide, including infertility. In women, deleterious effects of obesity on reproductive functions are well documented and extensively published, dealing especially with higher frequency of ovulatory disorders and menstrual irregularities [2], [3]. Within this context, abdominal fat accumulation contributes to reproductive dysfunction [4], [5].
Although there are still controversies about the effect on males, we recently show an increased risk of azoospermia or oligozoospermia in male with high body mass index (BMI) [6], [7]. Overweight or obesity may also alter sperm function, as an increase in sperm DNA fragmentation has been observed [8], [9], [10], [11]. Abdominal fat accumulation appears to be a better indicator of high risk for developing an abnormal metabolic profile than body mass index. A recent study showed that central adiposity, defined by a high waist circumference [12], negatively affects sperm concentration and total motile sperm count.
Indeed, adipose tissue accumulation is associated with increased oxidative stress, one of the potential mechanisms to explain sperm damages in obese patients [13], [14]. Decreased seminal plasma antioxidant and increased ROS production can be responsible for idiopathic male infertility [15].
Protein carbonyls, formed by a variety of oxidative mechanisms, are sensitive indices and the most general and commonly used biomarker of oxidative injury [16]. By contrast, it is interesting to evaluate SOD2, a ROS scavenger.
In women, abdominal fat loss results in an improvement of fertility [17], [18]. In men, only one publication is available and suggests an improvement of sperm parameters following weight loss [19].
The aim of this report is to investigate the association between abdominal fat loss in subfertile men and sperm quality. We also report the achievement of pregnancy following dietary advices in six subfertile men and analysis improvement of their sperm parameters, seminal antioxidant and oxidative stress markers and metabolic and hormonal profiles after abdominal fat loss.
Materials and Methods
Subjects
A cohort of couples attending an infertility centre for a primary idiopathic infertility (n = 36) was recruited for the ALIFERT study. ALIFERT study's criteria imply that patients do not have or did not have a metabolic disease (dyslipidemia, high blood pressure, hyperglycemia, diabetes...) nor a digestive disease. A sub-cohort of men was asked to participate to a personalized dietary program, including individualized nutritional advice aiming at reducing intra-abdominal fat and increasing exercise.
In this sub-cohort, we selected non smoking men, presenting with a percentage of sperm DNA fragmentation ≥25%, with abdominal fat ≥4 as measured by impedancemetry (see below) and still in a facto relationship.
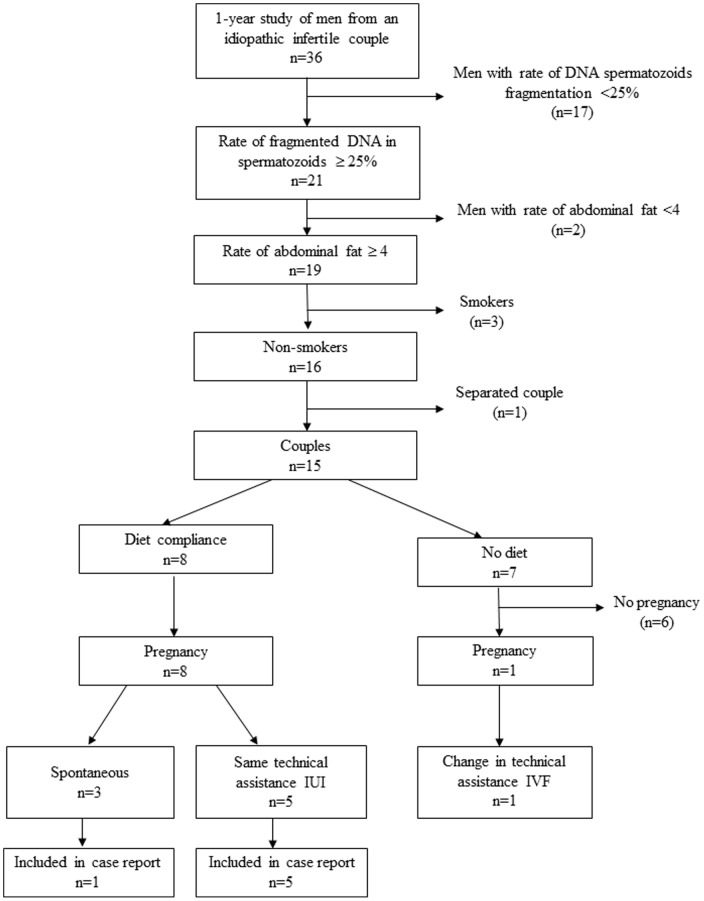
Out of 15 men responding to the above criteria, 8 accepted to follow the dietary program. Among them, only 6 agreed to provide samples before and after the intervention (Figure 1).
Figure 1. Design of the study.
Before and after the dietary program, anthropometric measures, abdominal fat, sperm parameters and sperm DNA fragmentation were evaluated. Hormonal and metabolic profiles could be obtained. Occurrence and outcome of pregnancies, obtained either spontaneously or following Assisted Reproductive Technology, were recorded.
The men received no incentives and participation was conditional to written and informed consent. The local ethics committee (Comité de Protection des Personnes) approved the study.
Anthropometric assessment
Height was measured to the nearest 5 mm, without shoes, using a metric, by the same trained investigator. Waist circumference was measured at the narrowest point between the lower border of the ribs and the iliac crest. Weight and body composition were evaluated using the Tanita BC-420MA Analyzer. The bioelectrical impedance measurement combines a digital scale with stainless steel pressure-contact foot-pad electrodes for standing impedance and body weight measurements [20]. Details of the validation and performance characteristics of this bioimpedance analysis model have been reported previously [21]. The bioimpedance supplies a level of visceral fat: the purpose is to be as close to 1; rating from 1 to 4 indicates a low level of visceral fat; rating 5 to 12 indicates a high level of visceral fat; >12 indicates a very excessive level.
Semen analysis
Sperm samples were collected at the laboratory after 3–5 days of sexual abstinence. After semen liquefaction, semen analysis was performed according to World Health Organization guidelines (WHO, 2010) assessing semen volume, sperm concentration, sperm motility. Total sperm count (TSC) was calculated.
Determination of sperm DNA integrity
To evaluate sperm nuclear DNA integrity, the TUNEL (Terminal Uridine Nick End Labeling) technique [22], [23] was performed on semen samples using In Situ Cell Death Detection Kit (In situ Cell Death Detection kit, Fluorescein, Roche Applied Science). Briefly, after trypsinization, spermatozoa were fixed in Carnoy solution (2∶1 methanol/acetic acid) and stored at −20°C. Spermatozoon pellets were permeabilised for 20 minutes with 0,1% Triton X-100 in sodium citrate solution and washed with PBS. Then cells were incubated with dUTP FITC-labelled and terminal deoxyribonucleotidyl tranferase (TdT) (TUNEL solution). The positive control sample was treated with 100 µl of DNase (0,5 mM) for one hour at 37°C before incubation with the TUNEL solution and the TdT enzyme was omitted for the negative control. Cells were then washed twice in PBS and spread out over slides. Slides were dried at room temperature in the dark and DAPI solution was added over the spermatozoa. Slides were examined using fluorescence microscopy. At least 200 spermatozoa were counted and total sperm DNA fragmentation rate was calculated as the number of FITC-positive cells from the total number of sperm nuclei (labelled with DAPI). Two investigators blinded to the exposure and other covariates performed twice the analyses.
Seminal markers assays
Liquefied semen was centrifuged to separate sperm from seminal plasma. Seminal plasma was immediately stored in aliquots at −80°C for further analysis without freezing–thawing.
Superoxide dismutase
SOD2 was quantified by ELISA using the “Human Superoxyde Dismutase 2 ELISA” kit (Abfrontier) according to manufacturer's instructions.
Detection of carbonylated proteins
Carbonylated proteins were labeled with CyDyeTM hydrazides (GE Healthcare) as described previously [24]. Briefly, samples were homogenized using a lysis buffer (10 mM tris-HCl (pH 7.4), 8 M urea, 2 M thiourea, 4% (w/v) CHAPS, 10 mM dithiothreitol (DTT)) and clarified by centrifugation. Protein quantification was performed by the Bradford method (Bio-Rad protein assay), using BSA as standard. Carbonylated proteins were labeled with Cy5 hydrazides (GE Healthcare) and total proteins were precipitated using the 2-D Clean-Up kit (GE Healthcare), following the manufacturer instructions. Protein precipitates were resuspended in loading buffer and separated by SDS-PAGE (4-20%). Total proteins were post-stained with ProteinGOLD (gel company). Fluorescent scanning was performed using Ettan Dalt system (GE Healthcare) at excitation and emission wavelengths of 635/680 for the Cy5 hydrazide and 390/595 for total proteins, respectively. Semiquantification of carbonylated proteins were performed on digitalized images by densitometric analysis using total protein staining as loading control.
Dietary program
All participants received individualized dietary advice by a nutritionist after a complete nutritional assessment. Program was based on a healthy, balanced diet, aiming for reduction in abdominal fat according to the French national nutrition and health programme. They were encouraged to practice 1 h of weekly exercise. Spouses did not change neither their diet nor their lifestyle.
Blood collection
Blood samples were used to estimate fasting glucose, lipid profile (triglycerides (TG), total cholesterol, HDL and LDL) and for sex hormone assays (FSH, LH, oestradiol and testosterone). The testosterone/oestradiol (T/E) ratio was calculated.
Statistical analysis
To determine whether there is an overall difference in pre- and post-intervention, anthropometric and sperm parameters, metabolic and sex hormones values were compared between the pre-test and the post-test using the Wilcoxon test. Value of 0.05 or less was considered statistically significant.
Results
The characteristics of the six patients at baseline and after diet are presented in Table 1 and Figure 2.
Table 1. Anthropometric parameters, semen characteristics, seminal antioxidant markers, metabolic and hormonal profiles and pregnancy outcome at baseline and after dietary advices.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Wilcoxon test | |||||||
| baseline | after diet | baseline | after diet | baseline | after diet | baseline | after diet | baseline | after diet | baseline | after diet | signification (alpha s) | |
| Anthropometry | |||||||||||||
| age (years) | 30 | 29 | 33 | 28 | 27 | 44 | |||||||
| height (m) | 1.86 | 1.82 | 1.89 | 1.73 | 1.88 | 1.89 | |||||||
| weight (kg) | 87.5 | 86.2 | 93.7 | 87.7 | 160.6 | 146.7 | 79.5 | 78.4 | 96.2 | 94.7 | 111.6 | 109 | 0.0139* |
| BMI (kg/m2) | 25.3 | 24.9 | 28.3 | 26.5 | 44.9 | 41.1 | 26.6 | 26.2 | 27.2 | 26.8 | 31.2 | 30.7 | 0.0139* |
| waist circunference (cm) | 103 | 90 | 90 | 89 | 142 | 121 | 83 | 80 | 96 | 94 | 125 | 114 | 0.0139* |
| intra-abdominal fat | 6 | 3 | 4 | 3 | 26 | 13 | 6 | 3 | 7 | 5 | 13 | 9 | 0.0139* |
| Sperm analysis | |||||||||||||
| total sperm count (M) | 28.4 | 16.9 | 76.2 | 31.9 | 35.6 | 87 | 74 | 199.6 | 29 | 176.6 | 21.9 | 32 | 0.1244 |
| progressive sperm motility (%) | 40 | 40 | 30 | 30 | 8 | 10 | 40 | 25 | 25 | 45 | 8 | 35 | 0.1367 |
| normal spermatozoa (%) | 31 | 27 | 14 | 15 | 11 | 21 | 26 | 19 | 7 | 14 | 11 | 16 | 0.2068 |
| sperm fragmentation (%) | 31 | 9.5 | 66 | 26.3 | 25 | 1.7 | 43 | 24 | 47 | 18 | 35 | 25.4 | 0.0139* |
| Seminal plasma analysis | |||||||||||||
| superoxide dismutase protein 2 (pg/ml) | 1191.5 | 2741.5 | 809 | 3621.5 | 1819 | 3311.5 | 4191.5 | >4399 | 754 | 3499 | 2939 | 4484 | 0.0139* |
| Biological parameters | |||||||||||||
| fasting glucose (g/l) | 0.9 | 0.83 | 0.82 | 1.01 | 0.94 | 0.92 | 0.88 | 0.87 | 0.95 | 0.97 | 0.97 | 0.83 | 0.3766 |
| triglycerides (g/l) | 0.82 | 0.7 | 0.89 | 0.59 | 1.87 | 1.39 | 1.02 | 0.7 | 1.21 | 1.1 | 3.07 | 2.19 | 0.0139* |
| total cholesterol (g/l) | 2.01 | 1.72 | 2.2 | 1.64 | 1.75 | 1.62 | 2.01 | 1.69 | 1.86 | 1.64 | 3.17 | 2.63 | 0.0139* |
| HDL (g/l) | 0.46 | 0.37 | 0.52 | 0.37 | 0.43 | 0.54 | 0.47 | 0.38 | 0.51 | 0.5 | 0.62 | 0.5 | 0.0865 |
| LDL (g/l) | 1.4 | 1.21 | 1.51 | 0.95 | 0.96 | 0.97 | 1.35 | 1.17 | 1.11 | 1.52 | 2.11 | 1.52 | 0.1244 |
| HDL/LDL ratio | 0.33 | 0.31 | 0.34 | 0.39 | 0.45 | 0.56 | 0.35 | 0.32 | 0.46 | 0.33 | 0.29 | 0.33 | |
| FSH (UI/l) | 4.6 | 3.2 | 4.6 | 4.5 | 3.6 | 3.2 | 2.1 | 2.3 | 45 | 4.1 | 2.6 | 2.3 | 0.0374* |
| LH (UI/l) | 5.3 | 2.7 | 4.9 | 4.8 | 3.9 | 2.7 | 3 | 2.7 | 3.3 | 2.9 | 2.3 | 2.7 | 0.0865 |
| oestradiol (pg/ml) | 51.7 | 36 | 37.4 | 22 | 34.6 | 32.8 | 32.8 | 26 | 30.3 | 28 | 26.7 | 18.1 | |
| testosterone (ng/ml) | 2.31 | 5.2 | 1.81 | 5.52 | 1.83 | 2.78 | 5.07 | 5.82 | 2.07 | 3.8 | 1.53 | 2.06 | |
| testo/oestra ratio | 44.6 | 144.4 | 48.4 | 250.9 | 52.9 | 87.76 | 154.6 | 223.8 | 68.3 | 135.7 | 57.3 | 113.8 | 0.0139* |
| Assisted reproductive treatment | 1 stim 1 IUI | 1 IUI | 1 stim | 1 IUI | 2 stim 1 IUI | 1 IUI | 1 stim 3 IUI | 1 IUI | 2 stim | None | 3 IUI | 1 IUI | |
| Outcome | No pregnancy | Live birth | No pregnancy | Live birth | No pregnancy | Live birth | No pregnancy | Live birth | No pregnancy | Live birth | No pregnancy | Live birth | |
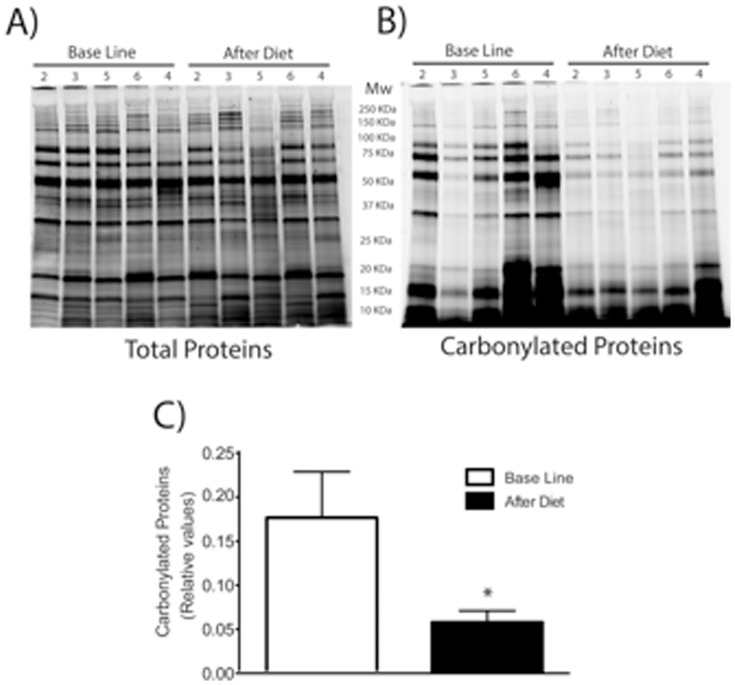
Figure 2. Oxidized damaged proteins before (Basal Line) and after treatment (After Diet).
SDS-PAGE (4–20%) pattern of total proteins post-stained with ProteinGOLDTM (A), or carbonylated proteins pre-labeled with C5Hz (B). Semiquantification of carbonylated proteins were performed by densitometric analysis, expressed as relative values and shown as mean±S.D (n = 5) and analyzed using Student's t-test; * P = 0.06 (C).
Patient 1
Patient 1 was a 30-year-old man with a 21-month history of primary idiopathic infertility. His partner was 30 years old and had a BMI at 26.3 kg/m2; her ovulatory status, hormonal profile and pelvic examination were within normal values.
At the time of the visit, male BMI was 25.3 kg/m2, abdominal fat was 6, sperm DNA fragmentation rate was 31% and sperm parameters were: TSC 28.4×106, progressive motility 40% and 31% normal spermatozoa. In seminal plasma concentration of SOD2 was 1191.5 pg/ml. Ratio of sex hormones was: T/E 44.6 and lipid profile: TG 0.82 g/l and total cholesterol 2.01 g/l. The couple had previously benefited from one ovarian stimulation, and one intrauterine insemination (IUI) without any pregnancy.
After 3 months on the dietary program, a pregnancy was obtained following the second IUI. At this time, male BMI was 24.9 kg/m2, abdominal fat was at 3, sperm DNA fragmentation rate was 9.5% and sperm parameters were: TSC 16.9×106, progressive motility 40% and 27% normal spermatozoa. In seminal plasma concentration of SOD2 was 2741.5 pg/ml. Ratio of sex hormones was: T/E 144.4 and lipid profile: TG 0.7 g/l and total cholesterol 1.72 g/l.
Patient 2
Patient 2 was a 28-year-old man with a 36-months history of primary idiopathic infertility. His partner was 31 years old and had a BMI at 19 kg/m2; her ovulatory status, hormonal profile and pelvic examination were within normal values.
At the time of the visit, male BMI was 26.6 kg/m2, abdominal fat was at 6, sperm DNA fragmentation rate was 43% and sperm parameters were: TSC 74×106, progressive motility 40% and 26% normal spermatozoa. In seminal plasma concentration of SOD2 was 809 pg/ml. Ratio of carbonylated proteins to total proteins was 0.16. Ratio of sex hormones was: T/E 154.6 and lipid profile: TG 1.02 g/l and total cholesterol 2.01 g/l. The couple had previously benefited from one ovarian stimulation cycle and three IUI without any pregnancy.
After 4 months on the dietary program, a pregnancy was obtained following the fourth IUI. At this time, male BMI was 26.2 kg/m2, abdominal fat was at 3, sperm DNA fragmentation rate was 24% and sperm parameters were: TSC 199.6×106, progressive motility 25% and 19% normal spermatozoa. In seminal plasma concentration of SOD2 was 3621.5 pg/ml. Ratio of carbonylated proteins to total proteins was 0.06. Ratio of sex hormones was: T/E 223.8 and lipid profile: TG 0.7 g/l and total cholesterol 1.69 g/l.
Patient 3
Patient 3 was a 27-year-old man with an 18-months history of primary idiopathic infertility. His partner was 31 years old and had a BMI at 27.7 kg/m2; her ovulatory status, hormonal profile and pelvic examination were within normal values.
At the time of the visit, male BMI was 27.2 kg/m2, abdominal fat was at 7, sperm DNA fragmentation rate was 47% and sperm parameters were: TSC 29×106, progressive motility 25% and 7% normal spermatozoa. In seminal plasma concentration of SOD2 was 1819 pg/ml. Ratio of carbonylated proteins to total proteins was 0.04. Ratio of sex hormones was: T/E 68.3 and lipid profile: TG 1.21 g/l and total cholesterol 1.86 g/l. The couple had previously benefited from 2 ovarian stimulations without any pregnancy.
After 5 months on the dietary program, a spontaneous pregnancy was obtained. At this time, male BMI was 26.8 kg/m2, abdominal fat was at 5, sperm DNA fragmentation rate was 18% and sperm parameters were: TSC 176.6×106, progressive motility 45% and 14% normal spermatozoa. In seminal plasma concentration of SOD2 was 3311.5 pg/ml. Ratio of carbonylated proteins to total proteins was 0.05. Ratio of sex hormones was: T/E 135.7 and lipid profile: TG 1.1 g/l and total cholesterol 1.64 g/l.
Patient 4
Patient 4 was a 29-year-old man with a 25-month history of primary idiopathic infertility. His partner was 29 years old and had a BMI at 25.7 kg/m2; her ovulatory status, hormonal profile and pelvic examination were within normal values.
At the time of the visit, male BMI was 28.3 kg/m2, abdominal fat was at 4, DNA fragmentation rate was 66% and sperm parameters were: TSC 76.2×106, progressive motility 30% and 14% normal spermatozoa. In seminal plasma concentration of SOD2 was 4191.5 pg/ml. Ratio of carbonylated proteins to total proteins was 0.26. Ratio of sex hormones was: T/E 48.4 and lipid profile: TG 0.89 g/l and total cholesterol 2.2 g/l. The couple had previously benefited from one ovarian stimulation cycle without any pregnancy.
After 4.5 months on the dietary program, a pregnancy was obtained following the first IUI. At this time, male BMI was 26.5 kg/m2, abdominal fat was at 3, sperm DNA fragmentation rate was 26.3% and sperm parameters were: TSC 31.9×106, progressive motility 30% and 15% normal spermatozoa. In seminal plasma concentration of SOD2 was more than 4399 pg/ml. Ratio of carbonylated proteins to total proteins was 0.12. Ratio of sex hormones was: T/E 250.9 and lipid profile: TG 0.59 g/l and total cholesterol 1.64 g/l.
Patient 5
Patient 5 was a 44-year-old man with a 36-months history of primary idiopathic infertility. His partner was 37 years old and had a BMI at 28.5 kg/m2; her ovulatory status, hormonal profile and pelvic examination were normal.
At the time of the visit, male BMI was 31.2 kg/m2, abdominal fat was at 13, sperm DNA fragmentation rate was 35% and sperm parameters were: TSC 21.9×106, progressive motility 8% and 11% normal spermatozoa. In seminal plasma concentration of SOD2 was 754 pg/ml. Ratio of carbonylated proteins to total proteins was 0.10. Ratio of sex hormones was: T/E 57.3 and lipid profile: TG 3.07 g/l and total cholesterol 3.17 g/l. The couple had previously benefited from 3 IUI without any pregnancy.
After 8 months on the dietary program, a pregnancy was obtained following the fourth IUI. At this time, male BMI was 30.7 kg/m2, abdominal fat was at 9, sperm DNA fragmentation rate was 25.4% and sperm parameters were: TSC 32×106, progressive motility 35% and 16% normal spermatozoa. In seminal plasma concentration of SOD2 was 3499 pg/ml. Ratio of carbonylated proteins to total proteins was 0.04. Ratio of sex hormones was: T/E 113.8 and lipid profile: TG 2.19 g/l and total cholesterol 2.63 g/l.
Patient 6
Patient 6 was a 33-year-old man with a 24-months history of primary idiopathic infertility. His partner was 31 years old and had a BMI at 29.6 kg/m2; her ovulatory status, hormonal profile and pelvic examination were within normal values.
At the time of the visit, male BMI was 44.9 kg/m2, abdominal fat was at 26, sperm DNA fragmentation rate was 25% and sperm parameters were: TSC 35.6×106, progressive motility 8% and 11% normal spermatozoa. In seminal plasma concentration of SOD2 was 2939 pg/ml. Ratio of carbonylated proteins to total proteins was 0.32. Ratio of sex hormones was: T/E 52.9 and lipid profile: TG 1.87 g/l and total cholesterol 1.75 g/l. The couple had previously benefited from 2 ovarian stimulations and one IUI without any pregnancy.
After 8 months on the dietary program, a pregnancy was obtained after the third IUI. At this time, male BMI was 41.1 kg/m2, abdominal fat was at 13, sperm DNA fragmentation rate was 1.7% and sperm parameters were: TSC 87×106, progressive motility 10% and 21% normal spermatozoa. In seminal plasma concentration of SOD2 was 4484 pg/ml. Ratio of carbonylated proteins to total proteins was 0.06. Ratio of sex hormones was: T/E 87.8 and lipid profile: TG 1.39 g/l and total cholesterol 1.62 g/l.
General comment: All participants lost abdominal fat (in terms of body composition and waist circumference) with no change of BMI categories after following the lifestyle program. Furthermore, there was no substantial change in conventional sperm parameters, whereas a significant improvement of sperm DNA integrity was observed for all patients (p = 0.0139). In seminal plasma we observed a large increase of SOD2 protein and a decrease of carbonylated proteins.
At baseline, none had impaired fasting glucose while increased triglycerides were observed for the two obese men with concomitant increase in total cholesterol for one of them. All men except one had decreased levels of testosterone. An improvement in both metabolic (significant decrease in triglycerides and total cholesterol; p = 0.0139) and hormonal (significant increase in testosterone/oestradiol ratio; p = 0.0139) profiles was observed after following the dietary/lifestyle program.
All female partners achieved pregnancy and delivered a healthy child. Delivery and neonatal characteristics are presented in Table 2.
Table 2. Delivery and neonatal characteristics.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | |
| amenorrhea weeks | 39.5 | 40 | 40 | 37 | 38 | 41 |
| baby weight (kg) | 3230 | 3070 | 3580 | 2750 | 3300 | 3750 |
| size (cm) | 47 | 49 | 53 | 45 | 47 | 50 |
| APGAR | 10 | 10 | 10 | 10 | 10 | 10 |
| sex | girl | girl | boy | girl | girl | girl |
Discussion
Although some studies failed to link BMI and semen analyses [25], [26], [27], most of them reported a detrimental impact of male BMI on sperm parameters, notably a decrease in sperm concentration [6], [7], [9], [10]. Consequently, the possibility to improve semen quality through weight reduction was also considered. Improvement of hormonal status was mainly observed after weight loss [28], [29]. Furthermore, a positive impact on semen parameters was observed by Hakonsen et al. [30].
However, abdominal fat, regardless of BMI, is a reliable predictor of individual risk of comorbidities such as metabolic syndrome [31], [32], [33]. Likewise, abdominal fat could be a good indicator to assess the risk of altered semen parameters. Until now, only 2 studies have shown a negative impact of abdominal fat (measured by waist circumference) on conventional semen parameters [12], [34] and none have assessed the impact of abdominal fat loss on male reproductive function.
Our report suggests, for the first time, that reduction of abdominal fat is associated with sperm DNA integrity improvement, regardless of BMI. Fat loss was also associated with an improvement of metabolic and sex steroid profiles. All 8 non smoking patients who followed the dietary program (6 agreed to provide samples after the intervention and 2 did not) have lost weight and their WC have decreased. Of the 7 patients who wished not to participate on the dietary program, no anthropometric change was observed.
Sperm DNA integrity is essential for a successful pregnancy [35]. High rates of sperm DNA fragmentation are associated with lower implantation rates and higher miscarriage rates [36], [37]. In this report, a successful pregnancy was obtained for the six couples after sperm DNA integrity improvement. The 2 other couples whose male partners followed the dietary program conceived healthy children. After one year, of the 7 patients who did not participate, six could not achieve pregnancy and one conceived a child after IVF. Information about sperm quality was not available.
Abdominal fat is associated with increased oxidative stress [38], [39]. Although, seminal plasma and sperm contain antioxidants, these defense systems can be overwhelmed [40]. Oxidative stress is known to impact male fertility. ROS (reactive oxygen species) can alter sperm membrane and sperm nucleus leading to sperm DNA damage [41], [42], [43]. Decreased SOD might be involved in abnormal semen quality [44]. Several studies in humans and in mice have established a link between being overweight or obese and oxidative stress and sperm DNA damages [45], [46]. In the present study, significantly higher levels of SOD2 protein have been observed in seminal plasma after the dietary program. Moreover an important decrease of carbonylated proteins has been evidenced, indicating an increased quality of the seminal proteome. Whether an improvement of the balance between oxidative/anti-oxidative substances in the seminal plasma due to the dietary program remains to be determined in future studies.
Moreover, an improvement of the testosterone/oestradiol ratio was observed in parallel with decreased abdominal fat. Central adiposity has been associated with lower levels of testosterone [47], and oestradiol levels positively correlate with visceral fat, but not with subcutaneous, adipose tissue. Therefore, visceral adipose tissue strongly correlates with testosterone/oestradiol ratio [48]. Based on an experimental mouse model, obesity, inflammation and visceral fat concentrations of aromatase appear to be linked [49]. The aromatization process, leading to the conversion of testosterone into oestradiol, is mediated by visceral fat inflammation. Obesity is associated with elevated of pro-inflammatory molecules that are known to induce the aromatase gene transcription and the aromatase activity [50], [51]
Conclusion
In conclusion, even a limited number of patients, these original findings suggest that abdominal fat loss may improve sperm DNA integrity, blood hormonal profile and pregnancy outcome. Oxidative stress should be involved in this phenomenon since an increase of SOD2 level and a decrease of oxidatively damaged proteins have been evidenced in seminal plasma of these patients after the dietary program.
Further prospective controlled interventional studies are needed to observe the effect of loosing abdominal fat on sperm quality in a larger cohort of infertile men with high sperm fragmentation and imbalance between oxidative and anti-oxidative substances in semen. If these results were confirmed, future prevention of subfertility should target abdominal fat and oxidative stress mainly in men with high sperm fragmentation.
Further studies are also needed to understand mechanisms and the effect on fertility outcome.
Acknowledgments
The authors want to acknowledge and thank all the patients who participated in the study. Thanks and appreciation to AC Marty for performing the second lecture of sperm DNA fragmentation and C Camelin and L Edinburgh who were involved in the paper review.
Funding Statement
This study was supported by National Biomedical Research: ALIFERT. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Wong WY, Thomas CM, Merkus JM, Zielhuis GA, Steegers-Theunissen RP (2000) Male factor subfertility: possible causes and the impact of nutritional factors. Fertil Steril 73: 435–442. [DOI] [PubMed] [Google Scholar]
- 2. Rich-Edwards JW, Goldman MB, Willett WC, Hunter DJ, Stampfer MJ, et al. (1994) Adolescent body mass index and infertility caused by ovulatory disorder. Am J Obstet Gynecol 171: 171–177. [DOI] [PubMed] [Google Scholar]
- 3. Zain MM, Norman RJ (2008) Impact of obesity on female fertility and fertility treatment. Womens Health (Lond Engl) 4: 183–194. [DOI] [PubMed] [Google Scholar]
- 4. Zaadstra BM, Seidell JC, Van Noord PA, te Velde ER, Habbema JD, et al. (1993) Fat and female fecundity: prospective study of effect of body fat distribution on conception rates. BMJ 306: 484–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pasquali R, Gambineri A, Pagotto U (2006) The impact of obesity on reproduction in women with polycystic ovary syndrome. Bjog 113: 1148–1159. [DOI] [PubMed] [Google Scholar]
- 6. Sermondade N, Faure C, Fezeu L, Levy R, Czernichow S (2012) Obesity and increased risk for oligozoospermia and azoospermia. Arch Intern Med 172: 440–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sermondade N, Faure C, Fezeu L, Shayeb AG, Bonde JP, et al. (2012) BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum Reprod Update [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fariello RM, Pariz JR, Spaine DM, Cedenho AP, Bertolla RP, et al. Association between obesity and alteration of sperm DNA integrity and mitochondrial activity. BJU Int [DOI] [PubMed] [Google Scholar]
- 9. Chavarro JE, Toth TL, Wright DL, Meeker JD, Hauser R (2010) Body mass index in relation to semen quality, sperm DNA integrity, and serum reproductive hormone levels among men attending an infertility clinic. Fertil Steril 93: 2222–2231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kort HI, Massey JB, Elsner CW, Mitchell-Leef D, Shapiro DB, et al. (2006) Impact of body mass index values on sperm quantity and quality. J Androl 27: 450–452. [DOI] [PubMed] [Google Scholar]
- 11. Dupont C, Faure C, Sermondade N, Boubaya M, Eustache F, et al. (2013) Obesity leads to higher risk of sperm DNA damage in infertile patients. Asian J Androl 15: 622–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hammiche F, Laven JS, Twigt JM, Boellaard WP, Steegers EA, et al. (2012) Body mass index and central adiposity are associated with sperm quality in men of subfertile couples. Hum Reprod [DOI] [PubMed] [Google Scholar]
- 13. Tremellen K (2008) Oxidative stress and male infertility—a clinical perspective. Hum Reprod Update 14: 243–258. [DOI] [PubMed] [Google Scholar]
- 14. Ebisch IM, Peters WH, Thomas CM, Wetzels AM, Peer PG, et al. (2006) Homocysteine, glutathione and related thiols affect fertility parameters in the (sub)fertile couple. Hum Reprod 21: 1725–1733. [DOI] [PubMed] [Google Scholar]
- 15. Alkan I, Simsek F, Haklar G, Kervancioglu E, Ozveri H, et al. (1997) Reactive oxygen species production by the spermatozoa of patients with idiopathic infertility: relationship to seminal plasma antioxidants. J Urol 157: 140–143. [PubMed] [Google Scholar]
- 16. Dalle-Donne I, Rossi R, Giustarini D, Milzani A, Colombo R (2003) Protein carbonyl groups as biomarkers of oxidative stress. Clin Chim Acta 329: 23–38. [DOI] [PubMed] [Google Scholar]
- 17. Thomson RL, Buckley JD, Noakes M, Clifton PM, Norman RJ, et al. (2008) The effect of a hypocaloric diet with and without exercise training on body composition, cardiometabolic risk profile, and reproductive function in overweight and obese women with polycystic ovary syndrome. J Clin Endocrinol Metab 93: 3373–3380. [DOI] [PubMed] [Google Scholar]
- 18. Kuchenbecker WK, Groen H, van Asselt SJ, Bolster JH, Zwerver J, et al. (2011) In women with polycystic ovary syndrome and obesity, loss of intra-abdominal fat is associated with resumption of ovulation. Hum Reprod 26: 2505–2512. [DOI] [PubMed] [Google Scholar]
- 19. Hakonsen LB, Thulstrup AM, Aggerholm AS, Olsen J, Bonde JP, et al. Does weight loss improve semen quality and reproductive hormones? Results from a cohort of severely obese men. Reprod Health 8: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nunez C, Gallagher D, Visser M, Pi-Sunyer FX, Wang Z, et al. (1997) Bioimpedance analysis: evaluation of leg-to-leg system based on pressure contact footpad electrodes. Med Sci Sports Exerc 29: 524–531. [DOI] [PubMed] [Google Scholar]
- 21. Pietrobelli A, Rubiano F, St-Onge MP, Heymsfield SB (2004) New bioimpedance analysis system: improved phenotyping with whole-body analysis. Eur J Clin Nutr 58: 1479–1484. [DOI] [PubMed] [Google Scholar]
- 22. Gorczyca W, Gong J, Darzynkiewicz Z (1993) Detection of DNA strand breaks in individual apoptotic cells by the in situ terminal deoxynucleotidyl transferase and nick translation assays. Cancer Res 53: 1945–1951. [PubMed] [Google Scholar]
- 23. La Vignera S, Condorelli RA, Vicari E, Calogero AE (2012) Negative effect of increased body weight on sperm conventional and nonconventional flow cytometric sperm parameters. J Androl 33: 53–58. [DOI] [PubMed] [Google Scholar]
- 24. Baraibar MA, Ladouce R, Friguet B (2013) Proteomic quantification and identification of carbonylated proteins upon oxidative stress and during cellular aging. J Proteomics [DOI] [PubMed] [Google Scholar]
- 25. Duits FH, van Wely M, van der Veen F, Gianotten J (2009) Healthy overweight male partners of subfertile couples should not worry about their semen quality. Fertil Steril 94: 1356–1359. [DOI] [PubMed] [Google Scholar]
- 26. Li Y, Lin H, Ma M, Li L, Cai M, et al. (2009) Semen quality of 1346 healthy men, results from the Chongqing area of southwest China. Hum Reprod 24: 459–469. [DOI] [PubMed] [Google Scholar]
- 27. Aggerholm AS, Thulstrup AM, Toft G, Ramlau-Hansen CH, Bonde JP (2008) Is overweight a risk factor for reduced semen quality and altered serum sex hormone profile? Fertil Steril 90: 619–626. [DOI] [PubMed] [Google Scholar]
- 28. Kaukua J, Pekkarinen T, Sane T, Mustajoki P (2003) Sex hormones and sexual function in obese men losing weight. Obes Res 11: 689–694. [DOI] [PubMed] [Google Scholar]
- 29. Niskanen L, Laaksonen DE, Punnonen K, Mustajoki P, Kaukua J, et al. (2004) Changes in sex hormone-binding globulin and testosterone during weight loss and weight maintenance in abdominally obese men with the metabolic syndrome. Diabetes Obes Metab 6: 208–215. [DOI] [PubMed] [Google Scholar]
- 30. Hakonsen LB, Thulstrup AM, Aggerholm AS, Olsen J, Bonde JP, et al. (2011) Does weight loss improve semen quality and reproductive hormones? Results from a cohort of severely obese men. Reprod Health 8: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Canoy D, Boekholdt SM, Wareham N, Luben R, Welch A, et al. (2007) Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation 116: 2933–2943. [DOI] [PubMed] [Google Scholar]
- 32. Heber D (2010) An integrative view of obesity. Am J Clin Nutr 91: 280S–283S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee CM, Huxley RR, Wildman RP, Woodward M (2008) Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 61: 646–653. [DOI] [PubMed] [Google Scholar]
- 34. Fejes I, Koloszar S, Szollosi J, Zavaczki Z, Pal A (2005) Is semen quality affected by male body fat distribution? Andrologia 37: 155–159. [DOI] [PubMed] [Google Scholar]
- 35. Santiso R, Tamayo M, Gosalvez J, Meseguer M, Garrido N, et al. (2010) Simultaneous determination in situ of DNA fragmentation and 8-oxoguanine in human sperm. Fertil Steril 93: 314–318. [DOI] [PubMed] [Google Scholar]
- 36. Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, et al. (2007) Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod 22: 174–179. [DOI] [PubMed] [Google Scholar]
- 37. Velez de la Calle JF, Muller A, Walschaerts M, Clavere JL, Jimenez C, et al. (2008) Sperm deoxyribonucleic acid fragmentation as assessed by the sperm chromatin dispersion test in assisted reproductive technology programs: results of a large prospective multicenter study. Fertil Steril 90: 1792–1799. [DOI] [PubMed] [Google Scholar]
- 38. Dandona P, Aljada A, Chaudhuri A, Mohanty P, Garg R (2005) Metabolic syndrome: a comprehensive perspective based on interactions between obesity, diabetes, and inflammation. Circulation 111: 1448–1454. [DOI] [PubMed] [Google Scholar]
- 39. Davi G, Falco A (2005) Oxidant stress, inflammation and atherogenesis. Lupus 14: 760–764. [DOI] [PubMed] [Google Scholar]
- 40. Aitken RJ, De Iuliis GN (2007) Origins and consequences of DNA damage in male germ cells. Reprod Biomed Online 14: 727–733. [DOI] [PubMed] [Google Scholar]
- 41. Ebisch IM, Thomas CM, Wetzels AM, Willemsen WN, Sweep FC, et al. (2008) Review of the role of the plasminogen activator system and vascular endothelial growth factor in subfertility. Fertil Steril 90: 2340–2350. [DOI] [PubMed] [Google Scholar]
- 42. Blumer CG, Fariello RM, Restelli AE, Spaine DM, Bertolla RP, et al. (2008) Sperm nuclear DNA fragmentation and mitochondrial activity in men with varicocele. Fertil Steril 90: 1716–1722. [DOI] [PubMed] [Google Scholar]
- 43. Cocuzza M, Sikka SC, Athayde KS, Agarwal A (2007) Clinical relevance of oxidative stress and sperm chromatin damage in male infertility: an evidence based analysis. Int Braz J Urol 33: 603–621. [DOI] [PubMed] [Google Scholar]
- 44. Alvarez JG, Touchstone JC, Blasco L, Storey BT (1987) Spontaneous lipid peroxidation and production of hydrogen peroxide and superoxide in human spermatozoa. Superoxide dismutase as major enzyme protectant against oxygen toxicity. J Androl 8: 338–348. [DOI] [PubMed] [Google Scholar]
- 45. Bakos HW, Mitchell M, Setchell BP, Lane M (2011) The effect of paternal diet-induced obesity on sperm function and fertilization in a mouse model. Int J Androl 34: 402–410. [DOI] [PubMed] [Google Scholar]
- 46. Tunc O, Bakos HW, Tremellen K (2011) Impact of body mass index on seminal oxidative stress. Andrologia 43: 121–128. [DOI] [PubMed] [Google Scholar]
- 47. Derby CA, Zilber S, Brambilla D, Morales KH, McKinlay JB (2006) Body mass index, waist circumference and waist to hip ratio and change in sex steroid hormones: the Massachusetts Male Ageing Study. Clin Endocrinol (Oxf) 65: 125–131. [DOI] [PubMed] [Google Scholar]
- 48. Gautier A, Bonnet F, Dubois S, Massart C, Grosheny C, et al. (2013) Associations between visceral adipose tissue, inflammation and sex steroid concentrations in men. Clin Endocrinol (Oxf) 78: 373–378. [DOI] [PubMed] [Google Scholar]
- 49. Subbaramaiah K, Howe LR, Bhardwaj P, Du B, Gravaghi C, et al. (2011) Obesity is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prev Res (Phila) 4: 329–346. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 50. Zhao Y, Agarwal VR, Mendelson CR, Simpson ER (1997) Transcriptional regulation of CYP19 gene (aromatase) expression in adipose stromal cells in primary culture. J Steroid Biochem Mol Biol 61: 203–210. [DOI] [PubMed] [Google Scholar]
- 51. Irahara N, Miyoshi Y, Taguchi T, Tamaki Y, Noguchi S (2006) Quantitative analysis of aromatase mRNA expression derived from various promoters (I.4, I.3, PII and I.7) and its association with expression of TNF-alpha, IL-6 and COX-2 mRNAs in human breast cancer. Int J Cancer 118: 1915–1921. [DOI] [PubMed] [Google Scholar]