Abstract
Objective
Evidence for the adverse effects of prepregnancy obesity on offspring’s neurodevelopmental outcomes has begun to emerge. We examined the association between prepregnancy obesity and children’s behavior problems and if the association would differ by race.
Methods
This observational study used a total of 3395 White (n = 2127) and African American (n = 1268) children aged 96 – 119 months from the National Longitudinal Survey of Youth. Behavior Problem Index (BPI) total and subscale scores were used to measure children’s behavior problems. The association between maternal prepregnancy obesity and the BPI scores for each racial group was examined using multivariate linear and logistic regressions, controlling for prenatal, child, maternal, and family background factors.
Results
Maternal prepregnancy obesity was independently associated with an increase in the BPI total scores among the White sample only. Among the African Americans, prepregnancy obesity was not associated with the BPI scores. Subsample analyses using externalizing and internalizing subscales also revealed similar trends. Among the White sample, children born to obese women were more socially disadvantaged than those born to non-obese women, whereas no such trend was observed in children of African American obese and non-obese women.
Conclusion
The impact of maternal prepregnancy obesity on children’s behavior problems differed by racial groups. Obesity-related metabolic dysregulations during the intrauterine period may not contribute to later children’s behavior problems. Social and psychological factors seem to play key roles in the association between prepregnancy obesity and childhood behavior problems among Whites.
Keywords: prepregnancy obesity, neurodevelopment, children’s behavior problems, racial difference, NLSY
INTRODUCTION
Research over the past two decades has established a robust relation between the intrauterine environment and the development of various human biological systems, particularly those important for metabolic and cardiovascular function (i.e., heart, pancreas).1 More recent work has begun to document the effects of the intrauterine environment on the central nervous system (CNS).2,3 Prepregnancy obesity and weight gain during pregnancy are two factors that have been associated with the development of adult chronic disease,4 but the CNS effects of maternal obesity are less clear. Because of the high prevalence of obesity (body mass index: BMI ≥ 30 kg/m2) among reproductive-aged women,5 understanding the possible health effects of maternal prepregnancy obesity on long-term CNS function is a high priority.
Recent work has examined the possible effects of prepregnancy maternal obesity on child cognition and behavioral problems. A handful of studies have demonstrated that maternal prepregnancy obesity is associated with offspring’s cognition,6–8 but fewer studies examined maternal weight status and the child’s psycho-behavior problems. Traditionally, one’s behavior is thought to be shaped in the post-natal environments. Indeed contributions from social scientists have shown strong evidence that economic disadvantage has harmful effects on children’s development.9,10 The effects of poverty on children’s mental and emotional health are often mediated through home environment, parental skills, and maternal depression.11,12 The current study helps to fill the gap by examining the relation between prepregnancy weight status and child behavior problems.
Animal studies have demonstrated that maternal obesity prior to conception, coupled with a high-fat diet (HFD) during pregnancy and lactation, is associated with altered offspring’s memory and learning of young mice.13,14 Bilbo et al.14 found that adult offspring of a HFD- induced obese rodent exhibited anxiety-like behavior and increased inflammatory markers in the brain. In humans, epidemiological studies examining childhood behavior problems and maternal prepregnancy weight status have produced mixed results. Studies using Nordic cohorts have shown that children born to obese women are at a higher risk of having attention deficit. hyperactivity disorder (ADHD) symptoms compared to those born to women with normal weight. 15,16 In another study, Brion et al.17 using two European cohorts found no consistent associations between prepregnancy overweight/obesity and behavior problem scores at preschool age or at primary school age across the cohorts. No study has examined the association between prepregnancy BMI and offspring’s behavior problems using racial groups other than European White.
The purpose of the current study is twofold: (1) to examine the association between maternal prepregnancy obesity and children’s behavior problems using children from the United States (US) and (2) to test the hypothesis that the association is similar across racial differences. A recent study using a mixed racial/ethnic group of children from the US found no evidence for a differential impact of race/ethnicity on the association between maternal prepregnancy BMI and children’s cognitive function.7 In the current study, we use the term race as a social construct.18 If maternal prepregnancy obesity adversely influences children’s behavioral development purely through a pathway involving obesity-related metabolic mechanisms during intrauterine period, one would expect the association between prepregnancy obesity and a measure representing children’s behavior to demonstrate a similar trend regardless of racial differences.
METHODS
A descriptive observational study design was employed using longitudinal data. Data were obtained from a longitudinal cohort in the United States, the National Longitudinal Survey of Youth (NLSY), Mother and Child file. The NLSY originally included a nationally representative sample of 12686 men and women who were between 14 and 21 years old when the survey began in 1979. Annual interviews were conducted from 1979 through 1994, then biennially thereafter. Starting in 1986, biennial surveys on the biological children of the NLSY female respondents began and continued to date on a variety of subjects.
Subjects
The current study was based on primary school-aged children between 96 and 119 months old (n = 7280), using NLSY surveys from 1986 through 2008. Primary school-aged children were chosen because behavior problems are more recognized during this period than at earlier ages and the results could be compared to previous studies.15–17 All age-eligible children were pooled from different survey years, with birth years of children eligible for the study spanning 1976 to 2000. Inclusion criteria for the current study were: White or African American children, term births (gestational age 37–42 weeks), and birth weight 2500 grams or greater. The last two criteria were used to minimize influences from prematurity and low birth weight on subsequent behavioral problems. This resulted in a total of 4183 children born to 2400 mothers. Final sample included a total of 3395 children born to 2080 mothers (81.2% of the eligible sample: Whites = 2127 or 82.3% eligible sample born to 1307 mothers; African Americans = 1268 or 79.3% or eligible sample born to 773 mothers) with complete data and biologically plausible BMI values according to the Centers for Disease Control and Prevention (CDC) growth chart program.
Characteristics of White children who were included in the current study were not different from those excluded. Among African Americans, children who were excluded differed from those included in the study sample in that they were more likely to have mothers with lower Armed Forces Qualification Test (AFQT) scores and come from families with lower income.
Measures
Children’s behavior problems
The Behavior Problems Index (BPI) was developed by Zill and Peterson19 based on Children’s Behavior Checklist 20 and other preexisting children’s behavior scales to measure behavior problems of children aged 4 years and older. Numerous studies have shown that the BPI has acceptable reliability (e.g., α-reliability = 0.91 for adolescent data from the 1981 Child Health Supplement 21). The completion rate for the BPI in this cohort has been above 90%. Mothers rated scores on 28 questions, which were based on their children’s behavior exhibited for the past three months. A higher score represents a higher level of behavioral problems.
Children’s behavior problems were assessed using the BPI total scores as well as externalizing and internalizing subscale scores. The age-based population-normed standardized scores (mean = 100, standard deviation [SD] = 15) as well as percentile scores were calculated by the NLSY analyst and included in the data set. For the externalizing and internalizing subscales, population-normed scores were only available for the survey years in 1994 and thereafter. For the survey years between 1986 and 1992, we constructed the variable using the raw scores of each item included in the subscales. The population-normed scores were then derived using the 1981 National Health Interview survey results as a norm population.
Prepregnancy weight status
Mothers were asked to report their weight just before pregnancy at their first interview after each birth of their child. Self-reported height for each mother was collected in 1981, 1982 and 1985 interviews. The first reported height from these interview years and weight just before each pregnancy were used to calculate their prepregnancy BMI. The World Health Organization adult BMI criteria were used to categorize weight status into underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2 BMI ≤ 25 kg/m2), overweight (25 kg/m2 ≤ BMI < 30 kg/m2), and obese (30 kg/m2≤BMI).
Other covariates
Other covariates were grouped into four factors: prenatal factors, maternal factors, home background factors, and child factors. Prenatal factors included child’s birth weight, gestational age, and mother’s smoking during pregnancy. Birth weight and gestational age of the children were reported by their mothers and expressed in kilograms and weeks, respectively. Mothers also reported whether or not they smoked during each pregnancy, and expressed in dichotomous measure (yes or no).
Maternal factors that may influence children’s development included age at childbirth, education, intellectual ability. Maternal education was expressed as the maximum years of education completed. Mother’s AFQT scores (percentile) was used as a general measure of intellectual ability.
Home background factors included child’s home environment, household income, and marital status of their mothers. Emotional support at home was measured using the Home Observation for the Measurement of Environment Short Form (HOME-SF) emotional support subscale. Developed by Caldwell and Bradley,22 HOME-SF, a shorter version of HOME, was designed to measure quality of stimulation and support provided by family caregivers, and has shown high correlations with children’s cognitive and behavioral development.23 Wording of some items in the scale differs according to developmental age groups. Examples of emotional subscale questions include: “About how many times do you spank your children?” and “If your child got so angry that he/she hit you, what would you do?” Age-based internally normed standardized scores (mean = 100 and SD = 15) were determined by the NLSY analyst. We created a permanent measure of emotional support at home by calculating a mean score of all available HOME-SF emotional support scores of a child from birth to age 119 months.
A permanent household per capita income of a child was derived from averaging household per capita incomes from his/her entire observation period. At each interview, mothers reported their family net incomes and the number of people in their families. Per capita income, deflated to 2008 US dollars, was calculated from family net income divided by the number of family members. A permanent measure of maternal marital status was also constructed by averaging the number of years that child’s mother being married with spouse present over the child’s entire observation period, and expressed as “percent time mother was married with spouse present”.
Finally, child factors included child’s race (mother-reported racial assignment, i.e. white or African American), gender (male or female), birth order, child’s age in month, and child’s weight status at the time of BPI assessment. Child’s weight status was determined by the CDC growth chart program, and categorized according to BMI percentile for age and gender: underweight (>5th percentiles), normal weight (5th – 84.99th percentiles), overweight (85th – 94.99th percentiles), and obese (≥95th percentiles). BMIz-scores were also used to compare group difference.
Maternal weight status categories when children were aged 96–119 months (thereafter called “maternal contemporaneous weight status”) instead of prepregnancy weight status categories were used in the analytical model to assess timing of maternal obesity in relation to children’s behavior problem. These variables were selected through reviews of existing literature. To achieve parsimony of the statistical model, only those that were statistically significantly associated with the dependent variable in the linear model using whole sample. Both maternal education and AFQT scores, which represent maternal intellectual ability, have been considered important factor for children’s behavioral development. However, due to high correlation between the two variables (r=0.54, p>0.0001), decision was made to keep only maternal education in the model.
Statistical Analysis
Characteristics of the samples by racial groups were compared using the t test (normally distributed variables), Wilcoxon-Mann-Whitney test (non-normally distributed variables), and χ2 test (categorical variables). We used both multivariate linear and logistic regressions to examine the association between maternal prepregnancy weight status and children’s behavior problem scores, adjusting for other specified variables. We first tested a linear regression model that included both White and African American children. While none of the maternal BMI categories was associated with children’s behavior problem scores using the whole cohort, the interaction for White race by maternal prepregnancy obesity was significant (data not shown). Therefore, we proceeded to examine the association separately by racial groups. We then repeated the analyses using maternal contemporaneous weight status in place for prepregnancy BMI categories. Second, we used logistic regression models to estimate the odds of a child having “a high level of behavior problems” using the BPI total percentile scores. “A high level of behavior problem” was defined as having the total (or subscale) score equal or greater than 90th percentile. We also ran logistic regression using a high level of externalizing or internalizing behavior as outcome measures using the sample of children who had those scores available, which resulted in a total of 2071 White and 1230 African American children for externalizing behavior subscale, and 2072 White and 1231 African American children for internalizing behavior subscale. Characteristics of these subsamples of children did not differ from those of the study sample described in Table 1.
Table 1.
Characteristics of study samples from Children of the NLSY79
| Whole Cohort
|
White
|
African American
|
|||||
|---|---|---|---|---|---|---|---|
| (n = 3 395) | (n = 2 127) | (n = 1 268) | Sig. | ||||
| mean | (SD) | mean | (SD) | mean | (SD) | p value | |
| Child | |||||||
| BPI total standardized score | 105.2 | (15.0) | 104.2 | (14.8) | 107.0 | (15.1) | <0.0001 |
| Gender (female) | 49.3% | 48.2% | 51.0% | 0.1160 | |||
| Birth order (First-born) | 44.6% | 46.7% | 41.1% | 0.0014 | |||
| BMI z-score | 0.37 | (1.18) | 0.30 | (1.15) | 0.49 | (1.2) | <0.0001 |
| Birth weight (kg) | 3.46 | (0.47) | 3.54 | (0.46) | 3.32 | (0.44) | <0.0001 |
| Mother | |||||||
| Prepregnancy weight status | 0.0026 | ||||||
| Underweight | 7.2% | 7.2% | 7.2% | ||||
| Overweight | 17.0% | 15.5% | 19.3% | ||||
| Obese | 9.5% | 8.7% | 10.7% | ||||
| Contemporaneous weight status | |||||||
| Underweight | 3.0% | 3.4% | 2.1% | ||||
| Overweight | 26.8% | 25.0% | 29.9% | ||||
| Obese | 23.9% | 17.9% | 33.9% | ||||
| Smoking during pregnancy (Yes) | 31.1% | 32.9% | 28.4% | 0.0060 | |||
| Maternal education (year) | 13.5 | (2.2) | 13.7 | (2.3) | 13.1 | (2.0) | <0.0001 |
| AFQT score | 42.6 | (28.4) | 54.3 | (26.1) | 23.0 | (19.9) | <0.0001 |
| Age at childbirth (year) | 25.4 | (5.4) | 26.3 | (5.2) | 24.0 | (5.4) | <0.0001 |
| Family background | |||||||
| HOME-SF emotional support | 97.9 | (12.3) | 102.2 | (9.5) | 90.6 | (13.0) | <0.0001 |
| Per capita income (2008 US $1000) | 16.5 | (19.8) | 20.3 | (22.3) | 10.1 | (12.2) | <0.0001 |
The p values shown are from the results of comparisons between White and African American children using t tests, Mann-Whitney-Wilcoxon tests, and χ2 tests.
Presence of secular year trends for the BPI scores over time was tested entering year-dummy variables. We found little evidence of secular trends for the BPI scores. In addition, including year dummies in the model resulted in little change in the effects of maternal prepregnancy weight status on BPI scores. Clustering of standard errors by sibling correlation was corrected using the Huber-White sandwich method. Comparisons of characteristics of White and African American children whose mothers were obese before pregnancy were done against those of non-obese mothers using t test, Wilcoxon-Mann-Whitney test, and χ2 test. All analyses were conducted using Stata 11 (StataCorp, College Station, TX).
RESULTS
Characteristics of the study samples are shown in Table 1. Overall, the mean BPI total score of the study sample was slightly higher than a normative sample. Gender ratio was the same in the whole group and each racial group. Approximately 10% of the children had mothers who were obese before becoming pregnant. The maternal obesity rate increased to 24% when children were primary school-aged. About one half of children (50.9%) had mothers with high school diploma, 27.5% had mothers with some college, and 21.6% had mothers with at least 16 years of education.
There were noticeable differences in characteristics between the two racial groups in all but gender ratios. African American children had approximately a 3-unit higher mean BPI total score (p < 0.0001) than White children. Mean birth weight was approximately 200 grams lower among African American children than White children (p < 0.0001), but the mean BMI at age 8–9 years was higher among African American children than among White children (p < 0.0001). A greater proportion of African American children had mothers who were overweight and obese before pregnancy than did White children (χ2 = 14.24, p = 0.0026). Maternal smoking prevalence during pregnancy was lower among the African American sample than the White sample (χ2 = 7.55, p = 0.0060). In addition, income, HOME-SF scores, maternal age, education, and AFQT were all lower among the African American sample than the White sample (Table 1).
Linear Association between Maternal Obesity and Children’s BPI Total Scores
The results of multivariate linear regressions using BPI total scores are shown in Table 1 (Models 1 and 2). In the linear model for the White children (Model 1), maternal prepregnancy obesity was associated with an average 4.3-unit increase in the BPI total scores compared to having mothers who were normal weight before pregnancy, holding other factors constant. Maternal prepregnancy overweight was marginally associated with the BPI total scores holding other factors constant (p=0.062). In an unadjusted linear model, maternal prepregnancy underweight showed a positive association with the BPI total scores (β = 3.69, 95%CI = 1.37 – 6.04). However, inclusion of maternal age and prenatal smoking in the model reduced the magnitude and strength of the association to non-significant level. On the other hand, among African American children, prepregnancy obesity was not only non-significant factor for the BPI total scores but also the direction of the coefficient was opposite from that of Whites (Model 2). Neither maternal prepregnancy overweight nor underweight was associated with children’s BPI total scores. Interestingly, only the coefficient for maternal prepregnancy underweight bore positive sign.
We then tested the effects of maternal contemporaneous obesity on children’s BPI total scores (results not shown). We used the same covariates as the models specified before. We found that among Whites, maternal contemporaneous obesity was independently associated with an approximately 2-unit increase in the BPI total scores (β = 2.04, p=0.044) compared to children with normal weight mothers. Removing children whose mothers were obese before pregnant with them resulted in null association between maternal obesity at child’s aged 96–119 months and the BPI total scores (n=1942, β=0.14, p = 0.907). Among African Americans, on the other hand, maternal contemporaneous obesity was not associated with the BPI total (β = −0.25, p = 0.830). Removing children whose mothers were obese before becoming pregnant with them did not change the results among African Americans.
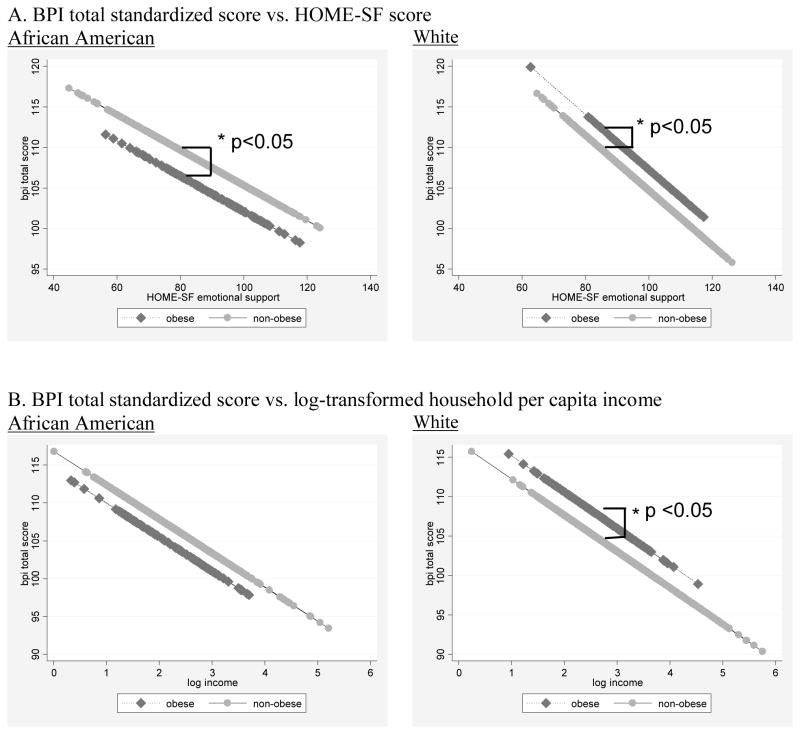
Across racial groups, the effects of maternal and family background factors on the BPI scores were similar, although the magnitudes and strengths of the associations differed slightly. However, a close examination of some of family background factors showed differences between racial groups by maternal prepregnancy obesity status. For example, unadjusted associations between HOME-SF scores and the BPI scores showed a systematic increase in the BPI total scores by maternal prepregnancy obesity among White children, while there was a systematic decrease in the BPI scores by maternal prepregnancy obesity among African American children (Figure, Panel A). A similar relation was present between income and the BPI scores (Figure, Panel B).
Figure.
Unadjusted relations between BPI total standardized score and selected family and maternal factors stratified by maternal prepregnancy obese status. Dark-shaded lines showing regression lines of the BPI total scores for children of women who were obese before pregnancy; light- shaded lines for those of women who were non-obese before pregnancy.
Odds of Having a High Level of Behavior Problems
The Models 3 to 8 in Table 2 show results of logistic regression estimating the odds of a child having “a high level of behavior problems” using the BPI total (Models 3 &4), externalizing (Models 5 & 6), and internalizing subscale (Models 7 & 8) percentile scores. Among the White sample, maternal prepregnancy obesity was associated with 78% higher odds of having a child with a higher level of behavior problems than prepregnancy normal weight category holding everything else constant (Model 3). The results using externalizing and internalizing subscales were similar except that strengths and magnitude of relationship were slightly weaker than those results using the total score (Models 5 & 7). Among the African American sample, the odds of having a child with a high level of behavior problems were very similar across all categories of maternal prepregnancy weight status (Models 4, 6, & 8).
Table 2.
Multiple linear regression and logistic regression models predicting children’s behavioral problems
| Linear Regression | Logistic Regression | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| BPI total§ | BPI total§§ | Externalizing§§ | Internalizing§§ | |||||
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
|
|
||||||||
| white | African American | white | African American | white | African American | white | African American | |
|
|
||||||||
| β | β | OR | OR | OR | OR | OR | OR | |
| Prepregancy weight status¶ | ||||||||
| Underweight | 1.89 [−0.40,4.19] | 0.56 [−2.87,4.00] | 1.24 [0.75,2.07] | 0.93 [0.51,1.68] | 1.23 [0.73,2.05] | 1.13 [0.63,2.04] | 1.01 [0.56,1.81] | 0.80 [0.41,1.53] |
| Normal weight | reference | reference | reference | reference | reference | reference | reference | reference |
| Overweight | 1.71 [−0.09,3.50] | −0.36 [−2.83,2.10] | 1.24 [0.87,1.77] | 1.14 [0.75,1.73] | 1.16 [0.81,1.65] | 1.06 [0.71,1.59] | 1.06 [0.71,1.56] | 1.11 [0.74,1.66] |
| Obese | 4.27*** [1.75,6.79] | −1.74 [−4.82,1.34] | 1.78** [1.16,2.73] | 0.94 [0.54,1.62] | 1.62* [1.04,2.52] | 1.11 [0.66,1.87] | 1.51 [0.96,2.39] | 1.04 [0.61,1.77] |
| Birth weight (kg) | −2.06** [−3.50,−0.63] | −0.61 [−2.62,1.39] | 0.88 [0.64,1.20] | 1.07 [0.76,1.51] | 0.81 [0.59,1.09] | 1.09 [0.77,1.52] | 0.91 [0.67,1.24] | 0.83 [0.58,1.19] |
| Gestational age (week) | 0.59* [0.03,1.14] | 0.23 [−0.54,1.00] | 1.08 [0.97,1.21] | 1.03 [0.88,1.19] | 1.06 [0.94,1.19] | 1.00 [0.86,1.15] | 1.14* [1.00,1.29] | 1.06 [0.91,1.23] |
| Prenatal smoking | ||||||||
| did not smoke | reference | reference | reference | reference | reference | reference | reference | reference |
| smoked | 2.33** [0.74,3.91] | 2.17* [0.08,4.25] | 1.46* [1.09,1.97] | 1.25 [0.88,1.79] | 1.53** [1.15,2.04] | 1.18 [0.83,1.66] | 1.40* [1.02,1.92] | 1.11 [0.77,1.59] |
| Age at childbirth (yr) | −0.49*** [−0.64,−0.35] | −0.25** [−0.44,−0.07] | 0.94*** [0.91,0.97] | 0.99 [0.96,1.02] | 0.94*** [0.92,0.97] | 0.98 [0.95,1.01] | 0.95** [0.92,0.98] | 1.01 [0.98,1.04] |
| Highest education mother completed (yr) | 0.09 [−0.25,0.43] | −0.44 [−0.99,0.11] | 1.01 [0.94,1.08] | 0.88* [0.80,0.98] | 1.00 [0.94,1.07] | 0.93 [0.85,1.03] | 1.04 [0.96,1.13] | 0.94 [0.86,1.03] |
| HOME-sf emotional support score | −0.30*** [−0.37,−0.22] | −0.18*** [−0.26,−0.11] | 0.96*** [0.94,0.97] | 0.98** [0.97,0.99] | 0.96*** [0.95,0.97] | 0.98** [0.97,0.99] | 0.97*** [0.96,0.98] | 0.99 [0.97,1.00] |
| Per capita income¶¶ | −0.03 [−0.05,0.00] | −0.09** [−0.16,−0.03] | 0.99 [0.98,1.00] | 0.98 [0.96,1.01] | 1.00 [0.99,1.00] | 0.97* [0.95,1.00] | 0.99 [0.98,1.01] | 0.99 [0.97,1.01] |
| Child sex | ||||||||
| male | reference | reference | reference | reference | reference | reference | reference | reference |
| female | −3.58*** [−4.79,−2.38] | −2.45** [−4.15,−0.76] | 0.62*** [0.48,0.81] | 0.61** [0.45,0.82] | 0.53*** [0.41,0.70] | 0.50*** [0.37,0.67] | 0.87 [0.66,1.14] | 1.03 [0.76,1.40] |
| Child weight status¶¶¶ | ||||||||
| Underweight | −0.04 [−2.54,2.46] | 2.74 [−1.21,6.68] | 0.81 [0.43,1.54] | 1.69 [0.89,3.24] | 0.90 [0.50,1.61] | 1.61 [0.86,3.00] | 0.94 [0.49,1.79] | 1.58 [0.83,3.04] |
| Normal weight | reference | reference | reference | reference | reference | reference | reference | reference |
| Overweight | 2.63** [0.92,4.33] | 2.19 [−0.05,4.43] | 1.54* [1.10,2.17] | 1.11 [0.73,1.67] | 1.45* [1.03,2.04] | 1.00 [0.66,1.53] | 1.34 [0.94,1.92] | 0.78 [0.49,1.24] |
| Obese | 2.04 [−0.14,4.23] | 1.87 [−0.20,3.94] | 1.55* [1.05,2.29] | 0.93 [0.61,1.42] | 1.17 [0.78,1.78] | 1.00 [0.68,1.47] | 1.60* [1.08,2.37] | 0.93 [0.61,1.42] |
|
|
||||||||
| N | 2127 | 1268 | 2127 | 1268 | 2071 | 1230 | 2072 | 1231 |
| R2 | 0.126 | 0.082 | ||||||
β = beta coefficient; OR = odds ratio; 95% confidence intervals in brackets
BPI total standardized score used as outcome variable
the scores equal or greater than 90th percentile used as “high behavioral score” for each category
prepregnancy weight status categories as follows: underweight (18.5 kg/m2 >BMI), normal weight (18.5 kg/m2 ≤BMI<25 kg/m2), overweight (25 kg/m2≤BMI<30 kg/m2), and obese (30 kg/m2≤BMI)
per capita income deflated to 2008 US dollars and expressed in the unit of $1000
child weight status categories by BMI percentile for age and gender: underweight (5th percentile>BMI), normal weight (5th percentile ≤BMI <85th percentile), overweight (90th ≤BMI<95th percentile), and obese (95th percentile ≤BMI)
p < 0.05,
p < 0.01,
p < 0.001
Comparison of Obese vs. Non-obese Characteristics by Racial Groups
Comparison of sample characteristics by maternal prepregnancy obesity status is shown in Table 3. Among Whites, the maternal prepregnancy obese group had lower HOME-SF scores and lower household income than the non-obese group. In contrast, among African Americans, the HOME-SF scores and household income did not differ between obese and non-obese groups. On average, obese African American mothers had longer years of education than non-obese mothers. The gender ratio for the children of obese African American women prompted an examination of gender-separate linear regression models for this racial group. No evidence was found for the gender ratio altering the positive association between maternal prepregnancy obesity and BPI total scores of African American children (result not shown).
Table 3.
Comparison of sample characteristics by maternal prepregnancy obese status
| White
|
African American
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-obese (n = 1 942) | Obese (n = 185) | Non-obese (n = 1 132) | Obese (n = 136) | |||||||
| mean | (SD) | mean | (SD) | p | mean | (SD) | mean | (SD) | p | |
| BPI total standardized score | 103.9 | (14.7) | 107.5 | (15.2) | 0.0016 | 107.3 | (15.0) | 104.6 | (15.8) | 0.0482 |
| Gender (%) | 0.9707 | 0.1673 | ||||||||
| Female | 48.3% | 48.1% | 50.4% | 56.6% | ||||||
| BMI z-score | 0.24 | (1.14) | 0.90 | (1.13) | <.0001 | 0.42 | (1.19) | 1.03 | (1.20) | <.0001 |
| Birth weight (kg) | 3.53 | (0.46) | 3.63 | (0.49) | 0.0070 | 3.31 | (0.44) | 3.43 | (0.44) | 0.0022 |
| Prenatal smoking (%) | 0.1967 | <.0001 | ||||||||
| Yes | 33.3% | 28.7% | 30.1% | 14.0% | ||||||
| Mother’s education (year) | 13.7 | (2.33) | 13.7 | (2.42) | 0.9198 | 13.1 | (1.96) | 13.5 | (2.15) | 0.0222 |
| Maternal AFQT score | 54.5 | (26.2) | 52.5 | (25.2) | 0.3160 | 22.5 | (19.3) | 26.8 | (23.6) | 0.1470 |
| Mother’s age at childbirth | 26.0 | (5.14) | 29.0 | (4.85) | <.0001 | 23.5 | (5.18) | 27.3 | (5.62) | <.0001 |
| HOME-SF emotional support score | 102.5 | (9.43) | 99.4 | (9.31) | <.0001 | 90.8 | (13.0) | 88.5 | (12.9) | 0.0507 |
| Household per capita income (2008 US $1000) | 20.6 | (23.1) | 16.3 | (11.6) | 0.0115 | 10.0 | (12.5) | 10.6 | (8.7) | 0.1520 |
Group differences were assessed using t test, Wilcoxon’s non-parametric test, and χ2 test
DISCUSSION
This study was designed to examine the relation between maternal prepregnancy weight status and children’s behavior problems, and to examine if the same relationship holds in different racial groups, using African American and White U.S. children. We found that the association between children’s behavior problem scores and maternal prepregnancy obesity was not consistent across the two racial groups. Maternal prepregnancy obesity was associated with an increase in mother-rated children’s behavior problem scores among White primary school-aged children from term-birth. Among African American children, we found no association between maternal prepregnancy obesity and children’s behavior problems. In addition, contemporaneous maternal obesity was not an independent factor for children’s BPI scores in either racial group, suggesting that the timing of a White woman’s being obese may play an important role in the association. Characteristics of children born to obese women were different from those of non-obese women, although the patterns of difference varied by racial groups in such a way that a wide social gap between obese and non-obese women seemed to exist among Whites but not among African Americans.
With regard to White children, our results are in accordance with those of Rodriguez et al. 15 and Rodriguez,16 in that maternal prepregnancy obesity was an independent factor for increasing children’s behavior problems. However, direct comparisons of these studies may not be possible; the outcome measure in the current study is the mother-rated global behavior problem score, whereas the studies by Rodriguez used the measures to specifically identify ADHD symptoms. Our results are different from those of Brion et al.17 who examined the same association in two different age groups (preschool and primary school) using a similar instrument to the current study but a different analytic strategy. Their use of an analytical method of estimating the probability of a child being in a higher quintile may have been necessary because of the use of raw scores, but their analysis may have been insensitive to detecting small increases in behavior problem scores, which in our study was about 4.4 units of standardized total score (or a 0.3 SD unit).
With regard to African American children, this was the first study examining the association between children’s behavior problem scores and maternal prepregnancy obesity using a large number from a minority racial group. All three of the previous similar studies were conducted in European countries with overwhelming White populations. Our results indicated that maternal prepregnancy obesity in the African American sample was not a factor for their children’s developing behavior problems. This was unexpected. Replication of the study using African American children from a different cohort is warranted to verify our findings.
While prevalence of obesity is higher among populations with low socioeconomic status (SES) and minority racial/ethnic standings,24 obese White women may experience larger social and economic consequences than their African American counterparts. For example, Salsberry and Reagan25 found that both childhood and adult low SES were associated with being obese among middle-aged White women, but this relationship did not exist among African American women. Other studies indicated a larger wage difference between obese and non-obese White women than that between obese and non-obese African American women.26 Using data from the 1981–2000 NLSY79, Cawley26 estimated that an obese White woman would earn 11.9% less wages than her normal-weight counterpart. An inverse relationship between BMI and SES was also found among White female adolescents from the early 2000s in the US, whereas high BMI was more prevalent among African American female adolescents from high SES in the same period.24,27
The psychological impact of obesity also appeared greater among White women than African American women. For example, low self-esteem was more pronounced among obese White women than obese African American women.28 Similarly, quality of life perceived by obese White women was significantly lower than that perceived by obese African American women, though a negative relationship between BMI and perceived quality of life was a general trend in both racial groups.29 It is possible that the significant relationship between children’s behavior problems and maternal prepregnancy obesity observed in Whites in the current study may be because prepregnancy obesity acts as a marker of persistent social disadvantage or stigma related to obesity that exists among White women. This notion is supported by our results among the White sample showing that children’s BMI significantly associated with their own behavior problems. In addition, the null association between children’s BPI scores and contemporaneous maternal obesity may demonstrate distinct characteristics of the White women who were obese before becoming pregnant.
Results of the current study may have important health, social, and economic implications. When we estimated the odds of a child having a clinically-significant behavior problems (BPI total or subscale scores ≥ 90 %ile), we found that children born to obese White women were associated with 1.6–1.8 times higher risk of having “a high level of behavior problems” compared to those born to normal weight White women. The social and economic burdens of treating these children with behavior problems are high. An annual societal cost for childhood ADHD alone has been estimated over $40 billion in the US.30 For young White women who are especially affected by obesity epidemic, providing them with guidance to nurture successful parenting skills and encouraging them to regain healthy weight status may be necessary for reducing the risk of their children developing severe behavior problems. For young African American women, because high weight status carries high costs for their health, innovative approaches to weight maintenance while preserving its protective effect for children’s behavior problems are imperative.
The current study has strengths and limitations. One of our major strengths is a large number of African American children in our sample, which allowed us to conduct a separate analysis for each racial group. Panel data design also made it possible to construct permanent measures of HOME-SF scores and household income: more accurate measures for family background than those from point-in-time.9 Our study also has limitations. Most data were from mothers’ self-reports, including maternal prepregnancy weight. Individuals at a higher end of weight tend to underestimate and those at a lower end to overestimate their weights.31 Therefore, use of self-reported body weight may have resulted in overestimation of the effects by prepregnancy obesity on children’s BPI score. In other words, our estimates for prepregnancy obesity may represent for those with much higher BMI than the current cut-off for adult obesity (BMI≥30 kg/m2). Unfortunately, low frequency of prepregnancy obesity in our sample (9.5%) did not allow us to examine the effects of different obesity classes (e.g. WHO obesity class I, II, or II).
There may be omitted variables that may be correlated to maternal prepregnancy obesity. One of these may be the effect of maternal depression on children’s behavior problems, which we were unable to demonstrate due to the limitation in the timing of maternal depressive symptom assessment in the NLSY. The scores of the Center for Epidemiologic Studies Depression scales (CES-D) for the mothers were only available from the interviews in 1992 and 1994. This would mean that the assessment for maternal depressive symptoms may have occurred at varying times for each participant, depending on when she became pregnant: time before childbirth, during pregnancy, or after childbirth. While we were aware of this limitation, we ran our analyses including maternal CES-D score and its interaction term. Inclusion of these variables resulted in strengthening of the positive association between maternal prepregnancy obesity children’s BPI scores (β = 5.99, 95%CI = 2.49 – 9.49) among Whites, and in a statistically significant negative association between prepregnancy obesity and children’s BPI score among African Americans (β = −5.6, 95%CI = −9.40 – −1.81), suggesting that maternal depression may have a distinct effect on the relationship between prepregnancy obesity and children’s behavior problems by racial groups.
We may also have introduced sample selection bias. Characteristics of the study sample and those excluded due to missing information were not equally distributed. We realized that disadvantaged African American children were more likely to be excluded, which could have underestimated the effects of income and AFQT scores for this racial group. However, we do not think that it would result in a meaningful change in the association between maternal prepregnancy obesity and children’s behavior problem scores because prepregnancy obesity tends not to bear a signature of social disadvantage among African American women in this sample. Lastly, because of the observational nature of our study design, causal relationship cannot be assumed.
In conclusion, there is little evidence suggesting maternal prepregnancy obesity impact children’s behavior problems through intrauterine mechanisms. The association between maternal prepregnancy obesity and children’s behavior found in White samples in the current as well as previous studies could not be replicated with the African American sample of the NLSY. Our results indicate that the association between maternal prepregnancy obesity and children’s behavior problems may be largely due to disadvantaged social characteristics that are uniquely present among White female population. Culturally sensitive and innovative approaches are needed to reduce the risk of developing childhood behavior problems while encouraging young women of all racial/ethnic backgrounds to maintain healthy weight. The findings of this study add to the growing body of literature documenting the relationship between health outcomes of prepregnancy obesity and racial/ethnic differences. We recommend replication of the study using samples from other racial/ethnic groups.
Acknowledgments
The authors would like to thank Dr. Patricia B. Reagan for her expertise in statistical analyses and critical review of the manuscript, Dr. Muriel Z. Fang for her technical support in data processing and programming, and Mr. Kevin Grandfield for his editorial assistance. This study was supported by the Ruth L. Kirschstein National Research Service Award (NRSA) predoctoral fellowship sponsored by the National Institute of Nursing Research (Grant # 5F31NR012878). Authors declared no conflict of interest.
Footnotes
Conflict of interest: The authors declare no conflict of interest.
References
- 1.Barker DJ. Fetal origins of coronary heart disease. BMJ. 1995 Jul 15;311(6998):171–174. doi: 10.1136/bmj.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antonow-Schlorke I, Schwab M, Cox LA, et al. Vulnerability of the fetal primate brain to moderate reduction in maternal global nutrient availability. Proc Natl Acad Sci U S A. 2011 Feb 15;108(7):3011–3016. doi: 10.1073/pnas.1009838108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Georgieff MK. Nutrition and the developing brain: nutrient priorities and measurement. Am J Clin Nutr. 2007 Feb;85(2):614S–620S. doi: 10.1093/ajcn/85.2.614S. [DOI] [PubMed] [Google Scholar]
- 4.Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005 Mar;115(3):e290–296. doi: 10.1542/peds.2004-1808. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012 Feb 1;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 6.Neggers YH, Goldenberg RL, Ramey SL, Cliver SP. Maternal prepregnancy body mass index and psychomotor development in children. Acta Obstet Gynecol Scand. 2003 Mar;82(3):235–240. doi: 10.1034/j.1600-0412.2003.00090.x. [DOI] [PubMed] [Google Scholar]
- 7.Tanda R, Salsberry PJ, Reagan PB, Fang MZ. The Impact of Prepregnancy Obesity on Children's Cognitive Test Scores. Matern Child Health J. Feb 17; doi: 10.1007/s10995-012-0964-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krakowiak P, Walker CK, Bremer AA, et al. Maternal Metabolic Conditions and Risk for Autism and Other Neurodevelopmental Disorders. Pediatrics. 2012 Apr 9;129(5):e1121–e1128. doi: 10.1542/peds.2011-2583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blau DM. The effect of income on child development. The Review of Economics and Statistics. 1999;81(2):261–276. [Google Scholar]
- 10.Brooks-Gunn J, Duncan GJ. The effects of poverty on children. The Future of children / Center for the Future of Children, the David and Lucile Packard Foundation. 1997 Summer-Fall;7(2):55–71. [PubMed] [Google Scholar]
- 11.Berger LM, Paxson C, Waldfogel J. Income and Child Development. Children and youth services review. 2009 Sep 1;31(9):978–989. doi: 10.1016/j.childyouth.2009.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rijlaarsdam J, Stevens GW, van der Ende J, et al. Economic Disadvantage and Young Children's Emotional and Behavioral Problems: Mechanisms of Risk. J Abnorm Child Psychol. 2012 Jun 27; doi: 10.1007/s10802-012-9655-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tozuka Y, Kumon M, Wada E, Onodera M, Mochizuki H, Wada K. Maternal obesity impairs hippocampal BDNF production and spatial learning performance in young mouse offspring. Neurochem Int. 2010 Oct;57(3):235–247. doi: 10.1016/j.neuint.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 14.Bilbo SD, Tsang V. Enduring consequences of maternal obesity for brain inflammation and behavior of offspring. FASEB J. 2010 Jun;24(6):2104–2115. doi: 10.1096/fj.09-144014. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez A, Miettunen J, Henriksen TB, et al. Maternal adiposity prior to pregnancy is associated with ADHD symptoms in offspring: evidence from three prospective pregnancy cohorts. Int J Obes (Lond) 2008 Mar;32(3):550–557. doi: 10.1038/sj.ijo.0803741. [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez A. Maternal pre-pregnancy obesity and risk for inattention and negative emotionality in children. J Child Psychol Psychiatry. 2010 Feb;51(2):134–143. doi: 10.1111/j.1469-7610.2009.02133.x. [DOI] [PubMed] [Google Scholar]
- 17.Brion MJ, Zeegers M, Jaddoe V, et al. Intrauterine effects of maternal prepregnancy overweight on child cognition and behavior in 2 cohorts. Pediatrics. 2011 Jan;127(1):e202–211. doi: 10.1542/peds.2010-0651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Caprio S, Daniels SR, Drewnowski A, et al. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment: a consensus statement of Shaping America's Health and the Obesity Society. Diabetes Care. 2008 Nov;31(11):2211–2221. doi: 10.2337/dc08-9024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peterson JL, Zill N. Marital disruption, parent-child relationships, and behavior problems in children. Journal of Marriage and Family. 1986;48:295–307. [Google Scholar]
- 20.Achenbach TM, Edelbrock CS. Behavioral problems and competencies reported by parents of normal and disturbed children aged four through sixteen. Chicago, Ill: Published by the University of Chicago Press for the Society for Research in Child Development; 1981. [PubMed] [Google Scholar]
- 21.Zill N. Behavior problems index based on parent report. Washington DC: 1990. [Google Scholar]
- 22.Caldwell B, Bradley R. Home observation for measurement of the environment. Little Rock: University of Arkansas at Little Rock; 1984. [Google Scholar]
- 23.Totsika V, Sylva K. The Home Observation for Measurement of the Environment Revisited. Child and Adolescent Mental Health. 2004;9(1):25–35. doi: 10.1046/j.1475-357X.2003.00073.x. [DOI] [PubMed] [Google Scholar]
- 24.Gordon-Larsen P, Adair LS, Popkin BM. The relationship of ethnicity, socioeconomic factors, and overweight in US adolescents. Obes Res. 2003 Jan;11(1):121–129. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- 25.Salsberry PJ, Reagan PB. Comparing the Influence of Childhood and Adult Economic Status on Midlife Obesity in Mexican American, White, and African American Women. Public Health Nursing. 2009;26(1):14–22. doi: 10.1111/j.1525-1446.2008.00751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cawley J. The Impact of Obesity on Wages. Journal of Human Resources. 2004 Spring;39(2):451–474. 2004. [Google Scholar]
- 27.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006 Oct;84(4):707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 28.Averett S, Korenman S. Black-white differences in social and economic consequences of obesity. Int J Obes Relat Metab Disord. 1999 Feb;23(2):166–173. doi: 10.1038/sj.ijo.0800805. [DOI] [PubMed] [Google Scholar]
- 29.Cox T, Ard J, Beasley T, et al. Examining the Association Between Body Mass Index and Weight Related Quality of Life in Black and White Women. Applied Research in Quality of Life. :1–14. doi: 10.1007/s11482-011-9160-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pelham WE, Foster EM, Robb JA. The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. J Pediatr Psychol. 2007 Jul;32(6):711–727. doi: 10.1093/jpepsy/jsm022. [DOI] [PubMed] [Google Scholar]
- 31.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002 Aug;5(4):561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]