Abstract
Objective:
To evaluate the mortality rate in patients with narcolepsy.
Design:
Data were derived from a large database representative of the US population, which contains anonymized patient-linked longitudinal claims for 173 million individuals.
Setting:
Symphony Health Solutions (SHS) Source Lx, an anonymized longitudinal patient dataset.
Patients/Participants:
All records of patients registered in the SHS database between 2008 and 2010.
Interventions:
None
Measurements and Results:
Identification of patients with narcolepsy was based on ≥ 1 medical claim with the diagnosis of narcolepsy (ICD-9 347.xx) from 2002 to 2012. Dates of death were acquired from the Social Security Administration via a third party; the third party information was encrypted in the same manner as the claims data such that anonymity is ensured prior to receipt by SHS. Annual all-cause mortality rates for 2008, 2009, and 2010 were calculated retrospectively for patients with narcolepsy and patients without narcolepsy in the database, and standardized mortality ratios (SMR) were calculated. Mortality rates were also compared with the general US population (Centers for Disease Control data). SMRs of the narcolepsy population were consistent over the 3-year period and showed an approximate 1.5-fold excess mortality relative to those without narcolepsy. The narcolepsy population had consistently higher mortality rates relative to those without narcolepsy across all age groups, stratified by age decile, from 25-34 years to 75+ years of age. The SMR for females with narcolepsy was lower than for males with narcolepsy.
Conclusions:
Narcolepsy was associated with approximately 1.5-fold excess mortality relative to those without narcolepsy. While the cause of this increased mortality is unknown, these findings warrant further investigation.
Citation:
Ohayon MM; Black J; Lai C; Eller M; Guinta D; Bhattacharyya A. Increased mortality in narcolepsy. SLEEP 2014;37(3):439-444.
Keywords: Narcolepsy, mortality
INTRODUCTION
Narcolepsy is a disabling disorder characterized by pathologic daytime sleepiness manifested by recurrent periods of profound sleep propensity that frequently triggers inadvertent naps or lapses into sleep throughout the day. Additionally, cataplexy, sudden episodes of loss of muscle tone triggered by emotions, can be present.
Narcolepsy is rare, affecting approximately 26 to 50 individuals per 100,000 habitants worldwide.1 Typically, symptoms of narcolepsy first appear in late adolescence or early adulthood,2,3 and since it is a chronic disease often requiring life-long medical treatment, it can have a profound impact on functioning, quality of life, and health care costs.4–7 Furthermore, a recent study on the societal effects of narcolepsy not only reported a substantial economic burden resulting from high health care costs and reduced income for both patients and their partners, but also found that the economic consequences of narcolepsy could be observed up to 11 years before diagnosis.8 Narcolepsy has also been linked to an increased risk of motor vehicle accidents.6,9
Hypersomnia disorders carry overall a heavy burden of illness with a large number of associated medical and psychiatric conditions.10 Patients with narcolepsy are among the most severely affected relative to the general population with high rates of comorbid conditions.11,18 As many as 15% of patients with narcolepsy have restless legs syndrome, and an estimated 25% of patients with narcolepsy have sleep apnea.12–14 Psychiatric disorders are also very common among patients with narcolepsy, especially affective disorders (depression and anxiety); comorbid medical conditions such as chronic pain, gastrointestinal disorders, hypercholesterolemia, and hypertension are also very frequent.15–19
Despite the characterization of associated comorbidities, some of which are known to be associated with increased mortality, mortality rates among patients with narcolepsy have not been explored in large databases. The objective of this study was to use a large, integrated database to characterize the mortality rate in narcolepsy relative to those who do not have narcolepsy.
METHODS
Data Source
Data for this study were derived from a large database maintained by Wolters Kluwer Pharma Solutions (WKPS) currently known as Symphony Health Solutions (SHS) Source Lx. Source Lx contains anonymized patient-linked longitudinal claims from the time of database initiation, January 2002. Data captured for this study include pharmacy, hospital, and physician service utilization acquired from medical and hospital claims, intelligent network services (switches), and via direct contracts with providers.
Patient information is encrypted prior to receipt of the data, and the encrypted values are used to link and match patients across time and location of care. The data are quality controlled and HIPAA (Health Insurance Portability and Accountability Act of 1996) compliant. The study was reviewed and approved by the Stanford University Institutional Review Boards (IRB).
The data are captured at the “point of service” and are therefore considered an open dataset. Patients may enter the dataset because they use a healthcare provider whose claims WKPS has access to. It covers all payer types, including commercial, Medicare, Managed Medicare, Medicaid, Assistance Program, and cash. As a result it covers a wide cross-section of US population. The advantage of this structure includes the ability to capture a large, representative portion of the US population.
For the current analysis, dates of death were acquired from a third party who acquires the data from the Social Security Administration (SSA). The third party encrypts its patient information in a manner consistent with SHS' claims providers and patients common to both datasets are matched and linked utilizing encrypted information. SHS' patient matching and linking process leveraged encrypted and scrubbed attributes such as name, date of birth, and gender. All patient information is encrypted and anonymized prior to receipt by SHS. At the time of the analysis, the SSA database included complete data through 2010. The combined dataset was used to calculate mortality rates.
Population
Identification of patients with narcolepsy was based on the presence of at least one medical claim with the diagnosis of narcolepsy, according to the Ninth Revision of the International Classification of Disease code (ICD-9 347.xx), between January 2002 and January 2012, the date of the database query.
Annual all-cause mortality rates for each of the calendar years 2008, 2009, and 2010 were calculated for the patients with narcolepsy and those without narcolepsy. For the patients with narcolepsy, the denominator for the mortality-rate calculation was the total number of narcolepsy patients with a healthcare claim in a given year or the prior year. These patients were considered the “active” narcolepsy group. This procedure ensured that individuals who died in a given year without having healthcare claims during the year of death had an opportunity to be counted in the active sample and included in the denominator for that year. The numerator was the number of narcolepsy patients who died in that year and were considered “active.” For patients without narcolepsy, individuals who had a healthcare claim in the reporting year or the prior year were considered the “active sample.” The annual mortality rate for this population was estimated based on the number of individuals without narcolepsy who died during that year and were considered “active” divided by the total number of individuals without narcolepsy who were “active.”
In both populations, patients who died in a given year were removed from the active sample for the subsequent year. Patients who were left out of the active sample due to not having any claim in the year and the prior year were not included in either the denominator or the numerator for mortality rate calculation. Mortality rates were also stratified by age group and gender.
Analyses
Estimated mortality rates for both populations were compared with those for the general US population obtained from the Centers for Disease Control (CDC).20 Standardized mortality ratios (SMR) with their 95% confidence intervals (95% CI) were calculated. SMR is calculated as the ratio of observed deaths over the expected deaths derived from the mortality rates for the total database population, which is a representative sample of the US general population. Confidence interval was calculated using Mid-P and Fisher exact test. SMR values greater than 1 and having a lower limit of its 95% CI that exceeds 1 indicates significant excess mortality.
RESULTS
From 2008 to 2010, the narcolepsy population in the database varied from 59,528 to 77,616 patients and the non-narcolepsy population varied from 172,577,116 to 177,935,082 (Table 1). Demographic characteristics of the sample are presented in Table 2 based on 2010 data.
Table 1.
Mortality in the narcolepsy and non-narcolepsy populations of the Source Lx Database
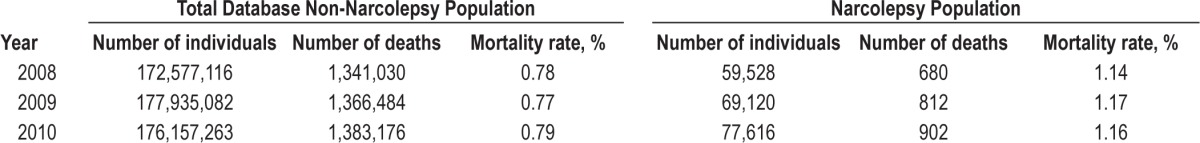
Table 2.
Demographic characteristics of the sample in 2010
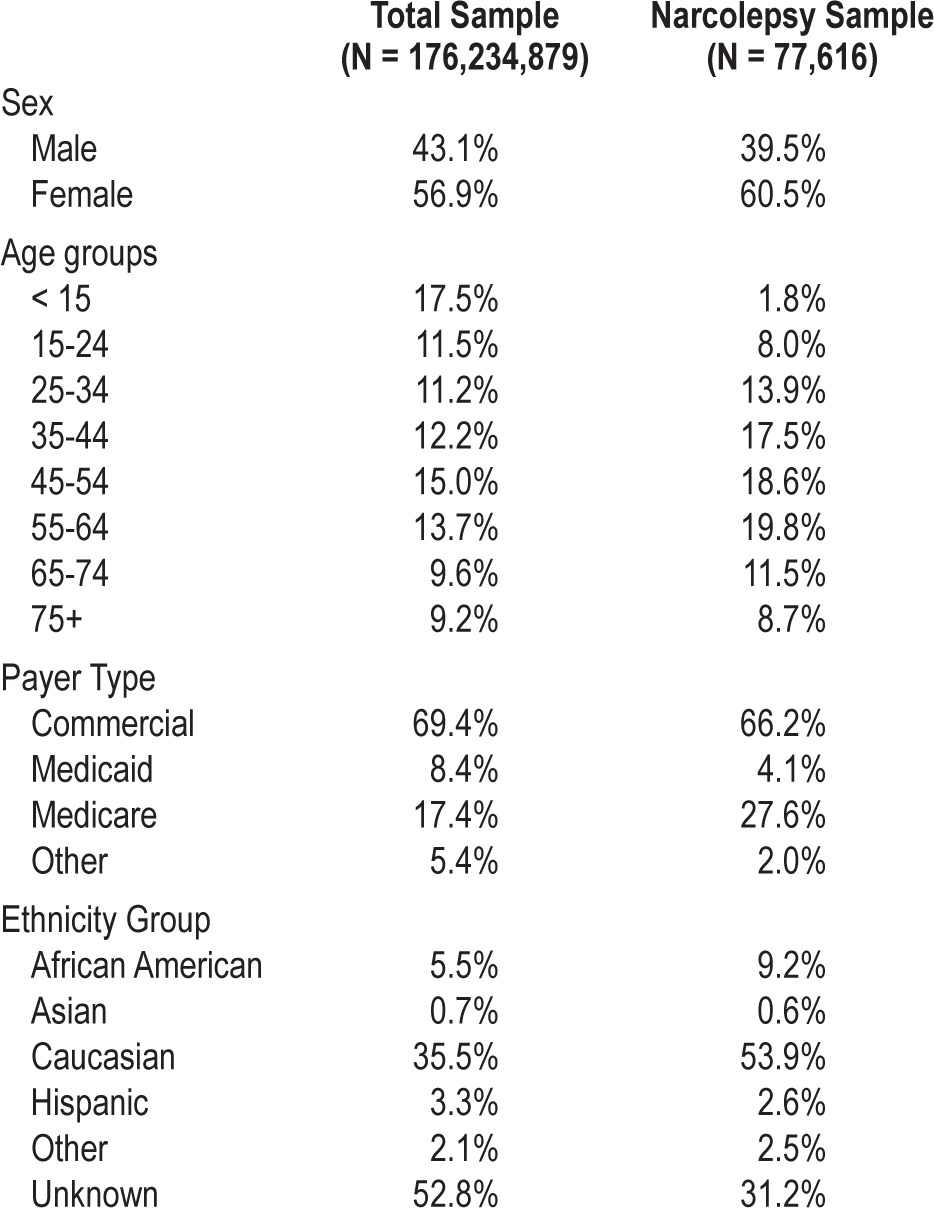
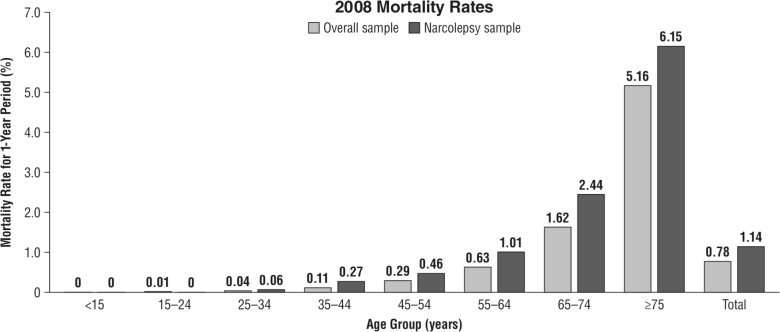
In the narcolepsy population, the mortality rates were consistent across time; 1.14% in 2008, 1.17% in 2009, and 1.16% in 2010. These rates were substantially higher than those estimated for the non-narcolepsy population; 0.78%, 0.77%, and 0.79%, respectively. The mortality rates estimated for the total population in the database were similar to those of the US population published by the CDC for 2008 through 2010, which were 0.81% in 2008 and 0.80% in 2009 and 2010. The SMRs of the narcolepsy population were consistent over the 3-year period (Figure 1), and indicated that there was an approximate 1.5-fold excess mortality that was significant relative to the non-narcolepsy population (P < 0.001).
Figure 1.
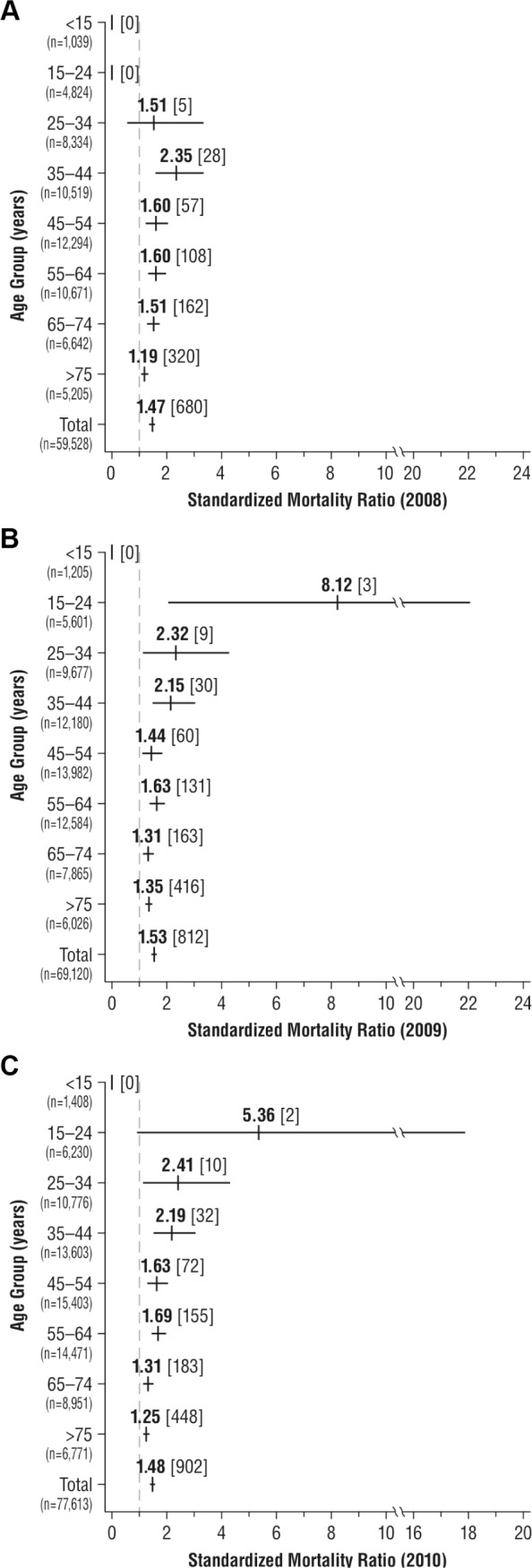
Standardized mortality ratios (95% CI) by age of the narcolepsy population relative to the non-narcolepsy population in the Source Lx Database for the years 2008 (A), 2009 (B), and 2010 (C). Numbers in brackets represent number of deaths in that age group. Numbers in parentheses represent the numbers of individuals of that age.
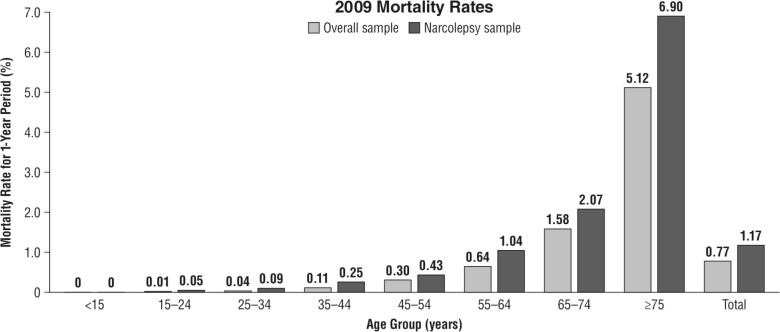
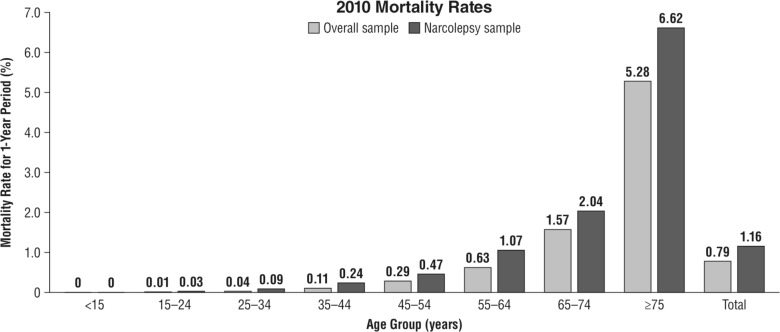
For 2008, the narcolepsy population had higher mortality rates for all age groups when stratified by age decile from 25-34 years to 75+ years of age compared with the non-narcolepsy population (Figure 2). Similar patterns of higher mortality rates were observed for the years 2009 and 2010 (Figures 3 and 4). SMRs show that there was excess mortality in all age groups except those < 15 years, and those 15-24 years in 2008. The lowest excess mortality was observed in the older age groups, where the death rates increased substantially in both the narcolepsy and the non-narcolepsy populations. The greatest excess mortality was observed in younger age groups, although these groups also had the widest 95% CIs (Figure 1).
Figure 2.
Narcolepsy and non-narcolepsy population mortality rates for 2008 by age in the Source Lx Database.
Figure 3.
Narcolepsy and non-narcolepsy population mortality rates for 2009 by age in the Source Lx Database.
Figure 4.
Narcolepsy and non-narcolepsy population mortality rates for 2010 by age in the Source Lx Database.
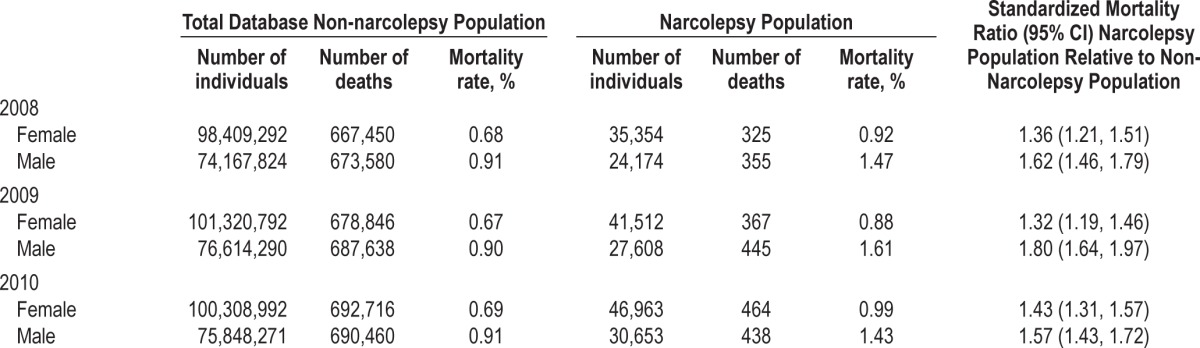
For both females and males, all SMRs indicated significant excess mortality relative to the non-narcolepsy population (Table 3).
Table 3.
Mortality in the narcolepsy and non-narcolepsy populations of the Source Lx Database stratified by sex
DISCUSSION
To our knowledge, this is the first study to report on the relationship between narcolepsy and mortality, and thus it is important to highlight some of the features of the database used in the analysis. The database population is large, containing information on more than 173 million individuals within the US and from all payer types. The mortality rates of the total database population during the years evaluated paralleled very closely those reported by the CDC for the general US population, suggesting that the database is reliably representative of the general population. Moreover, the proportion of narcoleptic patients in this database is similar to the prevalence reported in epidemiological studies; we observed an overall narcolepsy prevalence of 0.039%, which is well within the range of that of the general population (0.026%-0.05%).1
Within the database, narcolepsy was associated with a 1.5-fold increase in all-cause mortality for each of the three consecutive years studied. While elevated mortality rates have not been reported previously, many studies have identified a higher rate of comorbid medical conditions associated with narcolepsy; consistently reported comorbidity includes obesity, obstructive sleep apnea, cognitive deficits, and psychiatric disorders, especially depression.11,14–18,21–23 Furthermore, recent work suggests that additional medical conditions may be common in narcolepsy.18 Many of these conditions impart a known increased mortality risk; pathologic sleepiness, a symptom common to all patients with narcolepsy, carries its own elevated mortality risk, especially among the elderly.24–26 Excessive daytime sleepiness may also be associated with an increased risk of suicide ideation, especially in the presence of depression.27
It is possible that the increased mortality observed in the narcolepsy population results from complications of the condition of narcolepsy, from the comorbid conditions that carry their own increased mortality risk, or from a combination of narcolepsy and the comorbid medical conditions. Thus, the question remains as to whether narcolepsy exerts an independent effect on the cause of death or if the presence of other factors such as obesity, medical conditions, or psychiatric disorders may explain some of the variance in the association between narcolepsy and mortality. Although narcolepsy has been increasingly studied in recent years, there have been surprisingly few studies on medical conditions and psychiatric disorders associated with narcolepsy, and even fewer studies on the long-term evolution of narcolepsy.
As expected, mortality rates increased with age in both groups (narcoleptics and non-narcoleptics). However, we observed the presence of a peak in the relative mortality risk in the age groups 25-34 and 35-44 years, along with a higher relative mortality risk in the younger age groups relative to the older groups. Narcolepsy generally develops in late adolescence or early adulthood and takes an average of 7 to 10 years to diagnose after the appearance of the first symptoms.28 Some studies have reported a poorer health-related quality of life, as measured with the SF-36, in narcoleptic patients compared to the general population.6 However, it has also been reported that health-related quality of life tends to improve over time in patients with narcolepsy,29,30 perhaps as a result of adaptation strategies that enable patients to cope with the impact of the disease later in life when patients are past their peak productivity. It may be thus hypothesized that at least some of the early mortality may be a result of suicide, potentially resulting from the combination of reduced health-related quality of life and comorbid depression. Support for this hypothesis is that sleep disturbances including excessive daytime sleepiness represent risk factors for suicide among adolescents,31,32 and may likely also be a factor in the 25- to 34-year and 35- to 44-year age groups. This hypothesis found some validity in a morbidity and mortality longitudinal study on 322 narcoleptic individuals, which reported narcolepsy to be associated with a 7.35 fold increase in mortality due to suicide for the overall sample.33
One of the main limitations of this study is that it was not possible to identify the cause of death for the database subjects. There was also limited information available for subjects, and therefore it was not possible to adjust the mortality rates for possible confounding factors such as obesity or other medical conditions that may impart an independent effect on the outcome. We did not have either information on medical and/or psychiatric comorbid conditions. Moreover, meaningful evaluation of the interaction of distinct subtypes of narcolepsy, such as narcolepsy with or without cataplexy, on mortality was not possible with this database. Analysis of the differences in mortality between narcolepsy with or without cataplexy, would require a database in which all patients were definitively categorized. The narcolepsy population in this study was inadequately characterized to facilitate a more detailed analysis. Additionally, no information within the database was available regarding the clinical condition or diagnostic evaluation of those diagnosed with narcolepsy. Therefore, the accuracy of the diagnosis cannot be confirmed. Nonetheless, the prevalence of narcolepsy diagnosis within this extensive database is similar to that known to exist in the US population. It is therefore likely that the majority of patients are appropriately diagnosed. If misdiagnosis with other conditions of pathological sleepiness were common in this database, a much larger prevalence of narcolepsy would be found. Moreover, the patients identified with a narcolepsy diagnosis within the database are those who have a claim related to narcolepsy and therefore represent a clinically relevant population of patients for whom mortality information is clinically meaningful.
Research needs to address the question of whether or not features of the disorder may be responsible for the increased mortality rate: cataplexy, somnolence, disrupted sleep, a combination of these, or other disease-related factors. However, it is important to highlight that narcolepsy is a hypersomnolence disorder in classification systems. We do not understand the factors that underlie this increased rate of mortality but we think that the information is valuable for clinicians and researchers.
CONCLUSIONS
This retrospective study is the first to identify increased mortality in narcolepsy, although the cause or causes of this increased mortality is unknown. These findings are expected to be representative of the US population; however, additional studies are required to corroborate these results. Of key importance is to develop an understanding of the causes of the increased mortality to enable better care and initiate preventive measures in these patients.
DISCLOSURE STATEMENT
The authors acknowledge the editorial assistance and table and figure formatting by the Curry Rockefeller Group, which was funded by Jazz Pharmaceuticals. The analysis of the data by Symphony Health Solutions was funded by Jazz Pharmaceuticals. Dr. Ohayon was supported by the National Institutes of Health grant R01NS044199 and the Arrillaga Foundation. Drs. Guinta, Lai and Eller are employees of Jazz Pharmaceuticals. Dr. Black is a part-time employee of Jazz Pharmaceuticals. Dr. Bhattacharyya was an employee of Symphony Health Solutions, which was responsible for organizing and analyzing the data. Dr. Ohayon has received honorarium for participation with the advisory board from Jazz Pharmaceuticals.
REFERENCES
- 1.Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev. 2008;12:129–41. doi: 10.1016/j.smrv.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dauvilliers Y, Montplaisir J, Molinari N, et al. Age at onset of narcolepsy in two large populations of patients in France and Quebec. Neurology. 2001;57:2029–33. doi: 10.1212/wnl.57.11.2029. [DOI] [PubMed] [Google Scholar]
- 3.Okun ML, Lin L, Pelin Z, et al. Clinical aspects of narcolepsy-cataplexy across ethnic groups. Sleep. 2002;25:27–35. doi: 10.1093/sleep/25.1.27. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira VG, Faccenda JF, Douglas NJ. Functional status in patients with narcolepsy. Sleep Med. 2004;5:477–83. doi: 10.1016/j.sleep.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Daniels E, King MA, Smith IE, Shneerson JM. Health-related quality of life in narcolepsy. J Sleep Res. 2001;10:75–81. doi: 10.1046/j.1365-2869.2001.00234.x. [DOI] [PubMed] [Google Scholar]
- 6.Ozaki A, Inoue Y, Nakajima T, et al. Health-related quality of life among drug-naive patients with narcolepsy with cataplexy, narcolepsy without cataplexy, and idiopathic hypersomnia without long sleep time. J Clin Sleep Med. 2008;4:572–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Dodel R, Peter H, Walbert T, et al. The socioeconomic impact of narcolepsy. Sleep. 2004;27:1123–8. doi: 10.1093/sleep/27.6.1123. [DOI] [PubMed] [Google Scholar]
- 8.Jennum P, Ibsen R, Petersen ER, et al. Health, social, and economic consequences of narcolepsy: A controlled national study evaluating the societal effect on patients and their partners. Sleep Med. 2012;13:1086–93. doi: 10.1016/j.sleep.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Philip P, Sagaspe P, Lagarde E, et al. Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Med. 2010;11:973–9. doi: 10.1016/j.sleep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Ohayon MM, Dauvilliers Y, Reynolds CF., 3rd Operational definitions and algorithms for excessive sleepiness in the general population: implications for DSM-5 nosology. Arch Gen Psychiatry. 2012;69:71–9. doi: 10.1001/archgenpsychiatry.2011.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jennum P, Ibsen R, Knudsen S, Kjellberg J. Comorbidity and mortality of narcolepsy: a controlled retro- and prospective national study. Sleep. 2013;36:835–40. doi: 10.5665/sleep.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Plazzi G, Ferri R, Antelmi E, et al. Restless legs syndrome is frequent in narcolepsy with cataplexy patients. Sleep. 2010;33:689–94. doi: 10.1093/sleep/33.5.689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plazzi G, Ferri R, Franceschini C, et al. Periodic leg movements during sleep in narcoleptic patients with or without restless legs syndrome. J Sleep Res. 2012;21:155–62. doi: 10.1111/j.1365-2869.2011.00942.x. [DOI] [PubMed] [Google Scholar]
- 14.Sansa G, Iranzo A, Santamaria J. Obstructive sleep apnea in narcolepsy. Sleep Med. 2010;11:93–5. doi: 10.1016/j.sleep.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Fortuyn HA, Lappenschaar MA, Furer JW, et al. Anxiety and mood disorders in narcolepsy: a case-control study. Gen Hosp Psychiatry. 2010;32:49–56. doi: 10.1016/j.genhosppsych.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Fortuyn HA, Mulders PC, Renier WO, et al. Narcolepsy and psychiatry: an evolving association of increasing interest. Sleep Med. 2011;12:714–9. doi: 10.1016/j.sleep.2011.01.013. [DOI] [PubMed] [Google Scholar]
- 17.Fortuyn HA, Swinkels S, Buitelaar J, et al. High prevalence of eating disorders in narcolepsy with cataplexy: a case-control study. Sleep. 2008;31:335–41. doi: 10.1093/sleep/31.3.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ohayon MM. Narcolepsy is complicated by high medical and psychiatric comorbidities: a comparison with the general population. Sleep Med. 2013;14:488–92. doi: 10.1016/j.sleep.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Dauvilliers Y, Bayard S, Shneerson JM, et al. High pain frequency in narcolepsy with cataplexy. Sleep Med. 2011;12:572–7. doi: 10.1016/j.sleep.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 20.Miniño AM, Murphy SL, Xu J, Kochanek KD. Deaths: Final data for 2008. National Vital Statistics Report. 2011;59:1–127. [PubMed] [Google Scholar]
- 21.Ohayon MM, Ferini-Strambi L, Plazzi G, et al. How age influences the expression of narcolepsy. J Psychosom Res. 2005;59:399–405. doi: 10.1016/j.jpsychores.2005.06.065. [DOI] [PubMed] [Google Scholar]
- 22.Heier MS, Jansson TS, Gautvik KM. Cerebrospinal fluid hypocretin 1 deficiency, overweight, and metabolic dysregulation in patients with narcolepsy. J Clin Sleep Med. 2011;7:653–8. doi: 10.5664/jcsm.1474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schuld A, Hebebrand J, Geller F, Pollmacher T. Increased body-mass index in patients with narcolepsy. Lancet. 2000;355:1274–5. doi: 10.1016/S0140-6736(05)74704-8. [DOI] [PubMed] [Google Scholar]
- 24.Newman AB, Spiekerman CF, Enright P, et al. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. The Cardiovascular Health Study Research Group. J Am Geriatr Soc. 2000;48:115–23. doi: 10.1111/j.1532-5415.2000.tb03901.x. [DOI] [PubMed] [Google Scholar]
- 25.Empana JP, Dauvilliers Y, Dartigues JF, et al. Excessive daytime sleepiness is an independent risk indicator for cardiovascular mortality in community-dwelling elderly: the three city study. Stroke. 2009;40:1219–24. doi: 10.1161/STROKEAHA.108.530824. [DOI] [PubMed] [Google Scholar]
- 26.Gooneratne NS, Richards KC, Joffe M, et al. Sleep disordered breathing with excessive daytime sleepiness is a risk factor for mortality in older adults. Sleep. 2011;34:435–42. doi: 10.1093/sleep/34.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chellappa SL, Araujo JF. Excessive daytime sleepiness in patients with depressive disorder. Rev Bras Psiquiatr. 2006;28:126–9. doi: 10.1590/s1516-44462006000200010. [DOI] [PubMed] [Google Scholar]
- 28.Rye DB, Dihenia B, Weissman JD, et al. Presentation of narcolepsy after 40. Neurology. 1998;50:459–65. doi: 10.1212/wnl.50.2.459. [DOI] [PubMed] [Google Scholar]
- 29.Bruck D. The impact of narcolepsy on psychological health and role behaviours: negative effects and comparisons with other illness groups. Sleep Med. 2001;2:437–46. doi: 10.1016/s1389-9457(01)00067-3. [DOI] [PubMed] [Google Scholar]
- 30.Vignatelli L, Plazzi G, Peschechera F, et al. A 5-year prospective cohort study on health-related quality of life in patients with narcolepsy. Sleep Med. 2011;12:19–23. doi: 10.1016/j.sleep.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 31.Liu X, Buysse DJ. Sleep and youth suicidal behavior: a neglected field. Curr Opin Psychiatry. 2006;19:288–93. doi: 10.1097/01.yco.0000218600.40593.18. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ohayon MM. A longitudinal study of 322 individuals with narcolepsy. [abstract] Ann Neurol. 2012;72(Suppl S16):52. [Google Scholar]