Abstract
Study Objective:
Patients with excessive daytime sleepiness (EDS) are at high risk for driving accidents, and physicians are concerned by the effect of alerting drugs on driving skills of sleepy patients. No study has up to now investigated the effect of modafinil (a reference drug to treat EDS in patients with hypersomnia) on on-road driving performance of patients suffering from central hypersomnia.
The objective is to evaluate in patients with central hypersomnia the effect of a wake-promoting drug on real driving performance and to assess the relationship between objective sleepiness and driving performance.
Design and Participants:
Randomized, crossover, double-blind placebo-controlled trial conducted among 13 patients with narcolepsy and 14 patients with idiopathic hypersomnia. Patients were randomly assigned to receive modafinil (400 mg) or placebo for 5 days prior to the driving test. Each condition was separated by at least 3 weeks of washout.
Measurements:
Mean number of Inappropriate Line Crossings, Standard Deviation of Lateral Position of the vehicle and mean sleep latency in the Maintenance of Wakefulness Test were assessed.
Results:
Modafinil reduced the mean number of Inappropriate Line Crossings and Standard Deviation of Lateral Position of the vehicle compared to placebo (F(1,25) = 4.88, P < 0.05 and F(1,25) = 3.87, P = 0.06 tendency). Mean sleep latency at the Maintenance of Wakefulness Test significantly correlated with the mean number of Inappropriate Line Crossings (r = -0.41, P < 0.001).
Conclusions:
Modafinil improves driving performance in patients with narcolepsy and idiopathic hypersomnia. The Maintenance of Wakefulness Test is a suitable clinical tool to assess fitness to drive in this population.
Citation:
Philip P; Chaufton C; Taillard J; Capelli A; Coste O; Léger D; Moore N; Sagaspe P. Modafinil improves real driving performance in patients with hypersomnia: a randomized double-blind placebo-controlled crossover clinical trial. SLEEP 2014;37(3):483-487.
Keywords: Automobile driving, idiopathic hypersomnia, modafinil, MWT, narcolepsy, sleepiness
INTRODUCTION
Sleepiness at the wheel is a well-known cause of traffic accidents in western societies.1–4 These accidents are caused by sleep deprivation among healthy drivers5 and are also well documented in patients with obstructive sleep apnea syndrome (OSAS).3,6,7 Narcolepsy and idiopathic hypersomnia (IH) induce severe excessive daytime sleepiness but have been less studied for driving risk than OSAS. Evidence exists that narcolepsy and IH increase the risk of sleep related accidents.3,8–10
Even though epidemiological studies show associations between behavioral sleep deprivation or sleep disorders and accident risk, experimental studies are needed to confirm the relationship between sleepiness and risk of accidents. One such study11 demonstrated that patients with narcolepsy and OSAS have impaired driving performance on a simulated driving task compared to controls.
Countermeasures to sleepiness exist and their effect on driving risk has been demonstrated. Naps, caffeine intake, or exposure to continuous blue light have a positive effect on real-life driving performance in sleep deprived healthy subjects,12,13 and continuous positive airway pressure improves driving skills in patients with OSAS.14,15 Modafinil is a first-line pharmacological treatment for daytime sleepiness in narcolepsy and IH. One study investigated its beneficial effects on simulated driving performance in patients with narcolepsy,16 and no study has demonstrated in on-road conditions the efficacy of alerting drugs, used in narcolepsy or IH, on driving performance.
We have clearly shown that untreated patients with OSAS have altered performance in real driving conditions,17 and that Maintenance of Wakefulness Test (MWT) can predict this driving impairment. However, no study has yet evaluated the relationship between MWT scores and real driving performance in patients with hypersomnia.
We therefore designed a double-blind crossover study (modafinil versus placebo) to test the hypothesis that a wakefulness-promoting drug will improve on-road driving performance in patients with narcolepsy and IH. Our secondary objective was to assess the relationship between objective sleepiness and driving performance in these patients.
METHODS
Twenty-seven patients (age = 33.8 ± 11.1 y, range = 18-65 y, four males) suffering from central hypersomnia were evaluated: 13 patients with narcolepsy (seven with cataplectic attacks) and 14 patients with IH, diagnosed according to the criteria of the current International Classification of Sleep Disorders (ICSD-2, 2005).18 Eligible subjects were recruited over the 2 y preceding the inclusion period through two different means: (1) consultation with a physician in the reference center for rare hypersomnias of Pellegrin Hospital, Bordeaux; and (2) advertising in patients' association. Patients with comorbidities (including another cause of excessive daytime sleepiness) were excluded from the study. For this patient group, age at disease onset was 25.1 ± 11.1 y, range = 12-52 y. The mean Epworth Sleepiness Scale score was 14.3 ± 3.9 (range, 8-22). Anticataplectic medication was maintained for patients treated for narcolepsy.
Each patient received modafinil (400 mg/day) or placebo for 5 consecutive days in a randomized double-blind placebo-controlled crossover design (Figure 1). The placebo was of the same appearance (color and size of the capsule) and taste as the trial medication; it was prepared by the Central Pharmacy of the University Hospital Center of Bordeaux. Modafinil and placebo administrations were separated by a 3-week washout period. Treatment was administrated at 08:00 (modafinil 2×100 mg) and 12:30 (modafinil 2×100 mg). For the first 3 days, the subjects stayed at home where they were instructed to maintain their habitual sleep/wake schedules assessed by actigraphy and sleep diary. The length of this period was choosen due to the half-life of modafinil (15 h); 3 days are required to eliminate the drug. Prior to the start of the study, all patients were treated with modafinil when taking a stimulant medication except one patient treated with modafinil and methylphenidate; during the entire protocol, this patient received only modafinil to match the other patients. At the beginning of the protocol, all patients received either modafinil (400 mg) or placebo for a 3-day period before entering the test sessions the next 2 days. At the end of the day 3, patients were called back in the laboratory to perform an overnight polysomnography (PSG) (night 4). The next day (day 4) patients underwent an MWT to assess their level of objective sleepiness and a second overnight PSG (night 5). The last day (day 5), patients performed an on-road driving session. Patients were paid 400 euros for their involvement in the study.
Figure 1.
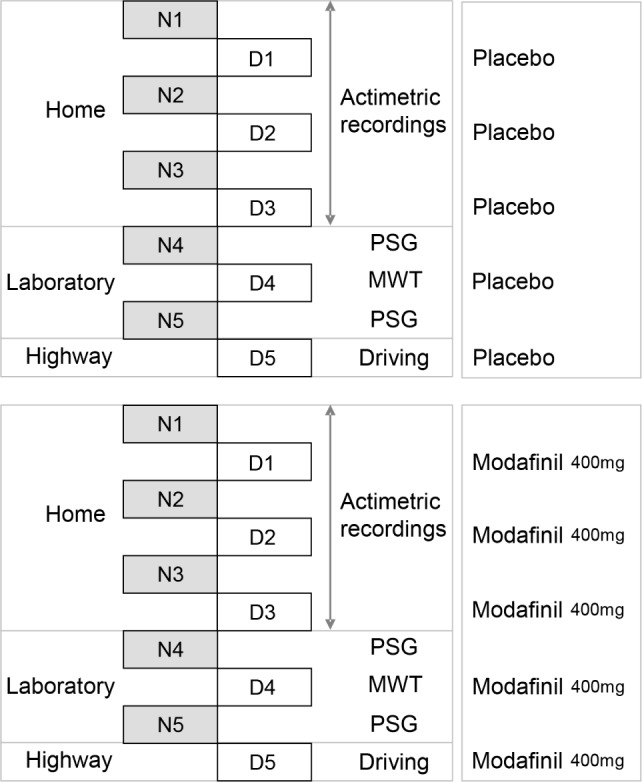
Overview of protocol design. A placebo condition (top panel) and a modafinil condition (400 mg/day) (lower panel) for 5 consecutive days separated by a 3-week washout period were administered in a randomized crossover double-blind placebo-controlled design in patients with narcolepsy and idiopathic hypersomnia (IH). The length of the 3-day period at home was chosen due to the half-life of modafinil (15 h); 3 days are required to eliminate the drug. Treatment was administrated at 08:00 (modafinil 2×100 mg) and 12:30 (modafinil 2×100 mg). In each condition, a period of 3 days at home with actigraphic recordings and sleep diary was followed by successive 36 h with 2 polysomnography (PSG) nights (nights 4 and 5) and 2 days to perform a 4 × 40-min Maintenance of Wakefulness Test (MWT) (day 4) and a 2-h on-road driving session (day 5).
Fourteen healthy control participants (age = 46 ± 9 y, range = 30-59 y, 13 males) were recruited outside of the sleep clinic. Each control participant underwent a clinical interview and examination by a sleep medicine specialist, and completed the Epworth Sleepiness Scale19 (ESS = 5 ± 3, range = 1-9). The presence of any sleep disorders in control participants was exclusion criteria. Each control subject had a polygraphic recording (Embletta; ResMed, Poway, CA) and an actigraphic recording (Actiwatch; Cambridge Neurotechnology, Cambridge, United Kingdom) to rule out any breathing disorders and to estimate their total sleep time (415 min ± 28) and their sleep efficiency (90% ± 3).
Control participants were paid 100 euros for their involvement in the study.
All participants provided written informed consent, and the local ethics committee (Comité de Protection des Personnes [CPP Sud-Ouest et Outre Mer III]) approved the study. The study was declared as a clinical trial (ClinicalTrials.gov identifier: NCT00916253).
Participants drove a 230-km round trip between 14:00 and 16:00 on an open highway. Participants were instructed to maintain a constant speed (130 kph [80 mph]), to drive in the center of the lane, and to not cross the painted lines separating the lanes except to pass a slower vehicle. A professional driving instructor was ready to take control of the car (which was equipped with dual controls) if needed.
Outcome Measures
Driving Performance
Driving Performance was identified by a Continental Automotive (Toulouse, France) video system (Figure 2), recording the lateral position (cm) of the car (10 times/sec) from the right lateral lane marker of the road. Inappropriate Line Crossings (ILC) were recorded when the car crossed a right or left lateral lane marker except to pass a slower vehicle. All ILC were confirmed manually by video recording analysis. The scorer of video recordings was blinded to the driving condition. Standard Deviation of Lateral Position (SDLP) of the car, derived from the lateral position, indicates weaving of the car.
Figure 2.
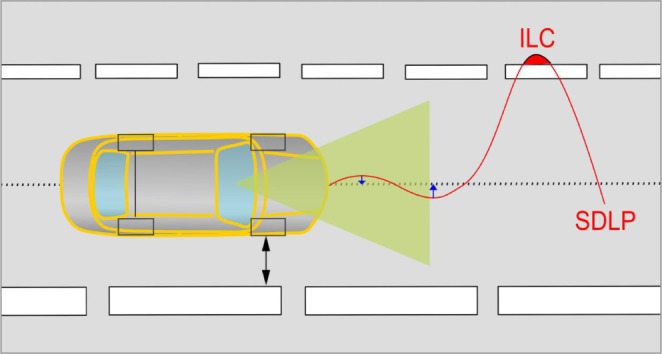
Schematic representation of the on-road driving test. A Continental system continuously records the actual position of the car within the traffic lane by tracking the relative distance of the car from the delineated stripe in the right of the road. Primary outcomes are Inappropriate Line Crossings (ILC) and Standard Deviation of Lateral Position (SDLP) (cm).
Objective Sleepiness
Objective sleepiness was assessed with four 40-min MWT trials, which were completed at 10:00, 12:00, 14:00, and 16:00, as recommended by the American Academy of Sleep Medicine (AASM) practice parameters.20 The patient was asked to fight against sleepiness in a soporific condition. Electroencephalograms (F3/A2, C3/A2, O1/A2), electromyograms, and electrooculograms were recorded according to the recommendations of AASM.21 Data were recorded and manually analyzed in 30-sec epochs. Sleep onset was defined as the first epoch of greater than 15 sec of cumulative sleep in a 30-sec epoch. The test was ended after three continuous epochs of stage N1 or 1 epoch of any other sleep stage to avoid interfering with the sleep homeostasis process.20 Patients who did not sleep during a trial were assigned a value of 40 min. Patients were video monitored during the whole test. The mean sleep latency of the four MWT trials was then calculated.
The primary end points were the mean number of ILC and mean SDLP of the vehicle. The secondary end points included the mean sleep latency at 4 × 40-min MWT trials.
Statistical Analysis
Group data are expressed as mean ± standard error (SE). Driving-related variables were analyzed with three-way analyses of variance (ANOVAs) with repeated factors “Treatment” (modafinil versus placebo) and “Driving sessions” (first versus second), and between subject-factor “Pathology” (narcolepsy versus hypersomnia). ILC were also analyzed with two-way ANOVAs with between subject-factors “Group” (controls versus placebo and controls versus modafinil) and with repeated factor “Driving sessions” (first versus second). Objective sleepiness scores were analyzed with three-way ANOVAs with repeated factors “Treatment” (modafinil versus placebo) and “Trials” (10H, 12H, 14H, 16H), and between-subject factor (narcolepsy versus hypersomnia). Objective sleepiness scores were also analyzed with two-way ANOVAs with between-subject factors “Group” (controls versus placebo and controls versus modafinil) and with repeated-factor “Trials” (10H, 12H, 14H, 16H). Planned comparisons were performed to localize statistical differences in significant main effect or interaction.
Spearman correlations were computed between MWT scores and driving performance (ILC and SDLP).
The alpha risk threshold was set at P = 0.05. Statistica® (StatSoft Inc. 2010, Statistica for Windows, Maisons-Alfort, France, Version 9.1) was used.
RESULTS
Objective Sleepiness (Sleep Latency on MWT)
Sleep latencies on the 4 × 40-min MWT in patients and controls are presented in Table 1.
Table 1.
Sleep latencies (mean ± standard deviation) on the 4 × 40-min Maintenance of Wakefulness Tests (10H, 12H, 14H, and 16H) and mean sleep latency in patients suffering from narcolepsy or idiopathic hypersomnia under placebo and under Modafinil, and in the healthy control group.

Sleep Latency on MWT in Patients
Mean sleep latencies on the MWT did not differ between patients suffering from narcolepsy or IH (25.0 min ± 2.4 versus 25.4 min ± 2.3) (F(1,25) = 0.019, not significant [NS]). Patients treated with modafinil suffering from narcolepsy or IH had longer mean sleep latencies than when under placebo (30.8 min ± 1.9 versus 19.7 min ± 1.8) (F(1,25) = 44.95, P < 0.001). Mean sleep latencies in patients under modafinil or placebo did not differ between trials (10H: 26.7 min ± 1.7, 12H: 25.8 min ± 2.0, 14H: 22.5 min ± 1.9, 16H: 25.7 min ± 1.9) (F(3,75) = 2.56, NS). No interaction was significant.
Sleep Latency on MWT in Patients Versus Controls
Patients suffering from narcolepsy or IH when under placebo had shorter mean sleep latencies than controls (19.7 ± 1.8 vs. 39.6 ± 2.0) (F(1,39) = 63.48, P < 0.001). The interaction Group × Trials did not yield any significance.
Patients suffering from narcolepsy or IH treated with modafinil had shorter mean sleep latencies than controls (30.8 ± 1.9 vs. 39.6 ± 2.0) (F(1,39) = 11.13, P < 0.01). The interaction Group × Trials did not yield any significance.
Driving Performance
All patients performed their entire driving session (230 km) without interrupting driving in both conditions.
Inappropriate Line Crossings
ILC in Patients
The number of ILC did not differ between patients suffering from narcolepsy or IH (2.0 ± 0.7 versus 1.3 ± 0.6) (F(1,25) = 0.55, NS). Patients treated with modafinil suffering from narcolepsy or IH made fewer ILC than when under placebo (1.1 ± 0.3 versus 2.1 ± 0.7) (F(1,25) = 4.88, P < 0.05) (Figure 3). Patients did not make more ILC on the second session than on the first session (1.6 ± 0.5 versus 1.6 ± 0.5) (F(1,25) = 0.054, NS). No interaction was significant.
Figure 3.
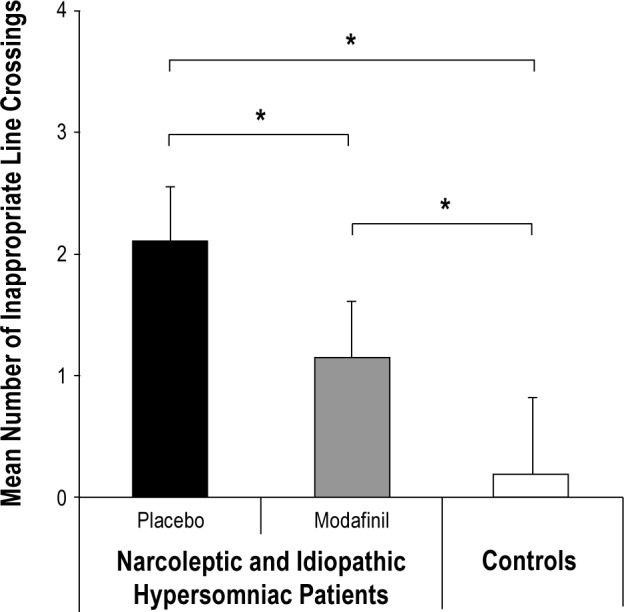
Mean number of Inappropriate Line Crossings (ILC) with on-road driving in patients with narcolepsy and idiopathic hypersomnia (IH) under placebo and modafinil and in healthy controls (mean ± standard error). *P < 0.05.
ILC in Patients Versus Controls
Patients suffering from narcolepsy or IH when under placebo made more ILC than controls (2.1 ± 0.5 versus 0.2 ± 0.7) (F(1,39) = 4.20, P < 0.05) (Figure 3). The interaction Group × Driving sessions did not yield any significance.
Patients suffering from narcolepsy or IH treated with modafinil made more ILC than controls (1.1 ± 0.2 versus 0.2 ± 0.7) (F(1,39) = 4.95, P < 0.05) (Figure 3). The interaction Group × Driving sessions did not yield any significance.
Standard Deviation of Lateral Position
SDLP in Patients
SDLP did not differ between patients suffering from narcolepsy or IH (25.0 cm ± 1.1 versus 23.5 cm ± 1.0) (F(1,25) = 1.10, NS). Patients treated with modafinil suffering from narcolepsy or IH had lower SDLP than when under placebo (23.6 cm ± 0.6 versus 24.9 cm ± 0.9) (F(1,25) = 3.87, P = 0.06 tendency). Patients had higher SDLP on the second session than on the first session (24.7 cm ± 0.7 versus 23.8 cm ± 0.8) (F(1,25) = 4.85, P < 0.05). No interaction was significant.
MWT Scores Versus Driving Performance
Mean sleep latency at the MWT correlated with mean number of ILC in controls and patients under modafinil or placebo (rho = -0.41, P < 0.001). Moreover, mean sleep latency at the MWT correlated with mean number of ILC in patients under modafinil or placebo (rho = -0.26, P = 0.054 tendency). Objective sleepiness (rho = -0.24, NS) did not correlate with mean SDLP in participants taking modafinil or placebo.
DISCUSSION
This study confirms that patients with untreated hypersomnia are at risk of sleep related driving accidents and demonstrates for the first time that modafinil improves on-road driving ability in these patients, although it does not improve lane-keeping to the level of healthy controls drivers.
Patients with narcolepsy have continual fluctuations of vigilance with attention difficulties22,23 that affect a wide variety of activities of daily living,24 including automobile driving. Modafinil has been shown to significantly improve cognitive performance including executive functions in healthy subjects in normal and sleep deprived conditions.25 Our study is the first to investigate the benefit of a reference wake-promoting drug, i.e., modafinil, on real driving condition in patients suffering from narcolepsy or IH. Modafinil caused a substantial reduction in the number of ILC and SDLP of the vehicle on the highway. This result confirms the beneficial effect of modafinil on driving skills in patients with narcolepsy and IH using validated criteria of driving performance.26
Our selected population was pathologically sleepy according to the MWT scores during the placebo condition. This result confirms the severity of IH and narcolepsy on the objective level of alertness. As expected, modafinil significantly increased mean sleep latency on the MWT but does not improve mean MWT sleep latency to the level of our controls. It is interesting to note that modafinil-treated patients exhibit a mean sleep latency on MWT that is quite similar to results found in healthy subjects: in the precited paper, the AASM reports a value of 30.4 ± 11.2 min.20
Because of the medicolegal issue raised by sleep related accidents, French authorities, as in many other countries, regulate the processing and dispensing of driving licenses of patients suffering from daytime sleepiness. The fitness to drive again for professional drivers is based on the assessment of treatment efficacy, which requires an MWT. In the same way, in its practice parameters for clinical use, the AASM states that a “MWT 40 min protocol may be used to assess an individual's ability to remain awake when his or her inability to remain awake constitutes a public or personal safety issue.”20 However, no evidence supports these guidelines within the specific context of narcolepsy and IH. Our study seems to confirm that MWT could be a good tool to predict driving ability in patients with central hypersomnia. One hundred percent of the worst driving performances were recorded in the MWT sleep latency scores < 19 min. Still, some patients from this group had preserved driving performance. However, all patients presenting with MWT sleep latency scores > 33 min had optimal driving performance. Patients from this group can therefore be defined as safe drivers. It seems reasonable to consider that the most patients presenting with sleep latency under 19 min are unsafe to drive. Physicians should combine objective measures (MWT scores) and clinical evaluation (self-report of sleepiness at the wheel) to provide recommendations about fitness to drive in these sleepy patients.
Regarding the limitations of the current study, different cognitive processes can be involved in specific situations of automobile driving. The vigilance component is usually involved during a prolonged and monotonous situation of driving on highway. If the situation requires more attention (i.e., increased traffic), the driver is then in condition of sustained attention. The driving conditions in our experiment were stimulant though involving a high cognitive load due to heavy traffic. Additional studies will have to verify that patients with hypersomnia do not experience more difficulty in monotonous driving situations involving the vigilance component. It is possible that the vigilance component is more affected than the sustained attention component in these patients during driving. Another limitation of our study is the small sample size. More studies are needed to determine the reproducibility of data. Finally, our control group was not matched in age with the patient group but was older. However, no degradation of driving performance has been observed between young and middle-aged drivers on the highway;27 therefore, our conclusions remain valid.
In conclusion, patients with hypersomnia treated with modafinil should be considered to be at less risk for accidents than untreated patients but at higher risk than controls. MWT scores could help physicians in their decisions about the fitness to drive in these patients.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported by a grant from ANR (Agence Nationale de la Recherche) AUTOSOP - PREDIT (Programme de Recherche et d'Innovations dans les Transports Terrestres). The funding organization had no role in the design and conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript. Dr. Philip has consulted for UCB, Sanofi, Takeda, Vital-Aire, and Bastide. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Maurice Cour (Continental) for his assistance in the analysis of data driving.
REFERENCES
- 1.Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ. 2002;324:1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horne JA, Reyner LA. Sleep related vehicle accidents. BMJ. 1995;310:565–7. doi: 10.1136/bmj.310.6979.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philip P, Sagaspe P, Lagarde E, et al. Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Med. 2010;11:973–9. doi: 10.1016/j.sleep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Blazejewski S, Girodet PO, Orriols L, Capelli A, Moore N. Factors associated with serious traffic crashes: a prospective study in southwest France. Arch Intern Med. 2012;172:1039–41. doi: 10.1001/archinternmed.2012.1695. [DOI] [PubMed] [Google Scholar]
- 5.Connor J, Whitlock G, Norton R, Jackson R. The role of driver sleepiness in car crashes: a systematic review of epidemiological studies. Accid Anal Prev. 2001;33:31–41. doi: 10.1016/s0001-4575(00)00013-0. [DOI] [PubMed] [Google Scholar]
- 6.George CF, Smiley A. Sleep apnea and automobile crashes. Sleep. 1999;22:790–5. [PubMed] [Google Scholar]
- 7.Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 8.Aldrich MS. Automobile accidents in patients with sleep disorders. Sleep. 1989;12:487–94. doi: 10.1093/sleep/12.6.487. [DOI] [PubMed] [Google Scholar]
- 9.Powell NB, Schechtman KB, Riley RW, Guilleminault C, Chiang RP, Weaver EM. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30:331–42. doi: 10.1093/sleep/30.3.331. [DOI] [PubMed] [Google Scholar]
- 10.Kotterba S, Müller N, Steiner G, Mayer G. Narkolepsy und Fahrtauglichkeit. Akt Neurol. 2004;31:273–8. [Google Scholar]
- 11.George CF, Boudreau AC, Smiley A. Comparison of simulated driving performance in narcolepsy and sleep apnea patients. Sleep. 1996;19:711–7. doi: 10.1093/sleep/19.9.711. [DOI] [PubMed] [Google Scholar]
- 12.Philip P, Taillard J, Moore N, et al. The effects of coffee and napping on nighttime highway driving: a randomized trial. Ann Intern Med. 2006;144:785–91. doi: 10.7326/0003-4819-144-11-200606060-00004. [DOI] [PubMed] [Google Scholar]
- 13.Taillard J, Capelli A, Sagaspe P, Anund A, Akerstedt T, Philip P. In-car nocturnal blue light exposure improves motorway driving: a randomized controlled trial. PLoS One. 2012;7:e46750. doi: 10.1371/journal.pone.0046750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George CF, Boudreau AC, Smiley A. Effects of nasal CPAP on simulated driving performance in patients with obstructive sleep apnoea. Thorax. 1997;52:648–53. doi: 10.1136/thx.52.7.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mazza S, Pepin JL, Naegele B, et al. Driving ability in sleep apnoea patients before and after CPAP treatment: evaluation on a road safety platform. Eur Respir J. 2006;28:1020–8. doi: 10.1183/09031936.06.00112905. [DOI] [PubMed] [Google Scholar]
- 16.Kotterba S, Mueller N, Leidag M, et al. Comparison of driving simulator performance and neuropsychological testing in narcolepsy. Clin Neurol Neurosurg. 2004;106:275–9. doi: 10.1016/j.clineuro.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 17.Philip P, Sagaspe P, Taillard J, et al. Maintenance of Wakefulness Test, obstructive sleep apnea syndrome, and driving risk. Ann Neurol. 2008;64:410–6. doi: 10.1002/ana.21448. [DOI] [PubMed] [Google Scholar]
- 18.American Academy of Sleep Medicine. International classification of sleep disorders. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. diagnostic and coding manual. [Google Scholar]
- 19.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 20.Littner MR, Kushida C, Wise M, T, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28:113–21. doi: 10.1093/sleep/28.1.113. [DOI] [PubMed] [Google Scholar]
- 21.Iber C, Ancoli-Israel S, Chesson A, Quan SF for the American Academy of Sleep Medicine. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 22.Rieger M, Mayer G, Gauggel S. Attention deficits in patients with narcolepsy. Sleep. 2003;26:36–43. [PubMed] [Google Scholar]
- 23.Naumann A, Bellebaum C, Daum I. Cognitive deficits in narcolepsy. J Sleep Res. 2006;15:329–38. doi: 10.1111/j.1365-2869.2006.00533.x. [DOI] [PubMed] [Google Scholar]
- 24.Bayon V, Leger D, Philip P. Socio-professional handicap and accidental risk in patients with hypersomnias of central origin. Sleep Med Rev. 2009;13:421–6. doi: 10.1016/j.smrv.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Muller U, Rowe JB, Rittman T, Lewis C, Robbins TW, Sahakian BJ. Effects of modafinil on non-verbal cognition, task enjoyment and creative thinking in healthy volunteers. Neuropharmacology. 2013;64:490–5. doi: 10.1016/j.neuropharm.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verster JC, Roth T. Vigilance decrement during the on-the-road driving tests: The importance of time-on-task in psychopharmacological research. Accid Anal Prev. 2012;58:244–8. doi: 10.1016/j.aap.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 27.Sagaspe P, Taillard J, Chaumet G, Moore N, Bioulac B, Philip P. Aging and nocturnal driving: better with coffee or a nap? A randomized study. Sleep. 2007;30:1808–13. doi: 10.1093/sleep/30.12.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]


