Abstract
Study Objectives:
To examine the relationship between functional health literacy (FHL) and obstructive sleep apnea (OSA), its diagnosis, related risk factors, and comorbidities.
Design:
Population cohort study.
Setting:
Adelaide, South Australia, 2011-12.
Participants:
1,021 Men Androgen Inflammation Lifestyle Environment and Stress Study participants aged ≥ 40 years, of whom 627 were identified with OSA by self-report (n = 184 previously diagnosed) or with in-home polysomnography in 837 randomly selected participants without self-reported OSA (n = 443 previously undiagnosed).
Interventions:
The Newest Vital Sign assessed FHL in 88% of participants. Full in-home unattended polysomnography (Embletta X100) was scored by 2007 AASM (alternative) criteria.
Measurements and Results:
FHL was adequate in 75.3% (n = 122) of previously diagnosed and 68.3% (n = 261) of previously undiagnosed OSA. Not having a previous diagnosis was independently associated with inadequate FHL (odds ratio [OR]:2.84, 95% confidence interval [CI]:1.25-6.45) and workforce participation (OR = 2.04, 95%CI = 1.01-4.00), and inversely associated with previous snoring (OR = 0.48, 95%CI = 0.29-0.81), obesity (OR = 0.35, 95%CI = 0.15-0.81), and cardiovascular disease (OR = 0.45, 95%CI = 0.24-0.85).
In polysomnography participants, inadequate FHL was independently associated with previously undiagnosed OSA (OR = 2.43, 95%CI = 1.40-4.20). In undiagnosed men, less than adequate FHL was independently associated with sedentary lifestyle (OR = 2.42, 95%CI = 1.36-4.29), and depression (OR = 2.50, 95%CI = 1.23-5.09) and inadequate FHL was associated with current smoking (OR = 2.87, 95%CI = 1.21-6.84). The depression association was attenuated after additional adjustment for comorbidities and general health (OR = 2.04, 95%CI = 0.93-4.49, P = 0.076). In previously diagnosed OSA, less than adequate FHL was independently associated with cardiovascular disease (OR = 2.76, 95%CI = 1.09-7.01).
Conclusions:
Limited functional health literacy was independently associated with obstructive sleep apnea (OSA), OSA diagnosis, lifestyle factors and comorbidities, highlighting the importance of developing and promoting national disease-specific health literacy policies.
Citation:
Li JJ; Appleton SL; Wittert GA; Vakulin A; McEvoy RD; Antic NA; Adams RJ. The relationship between functional health literacy and obstructive sleep apnea and its related risk factors and comorbidities in a population cohort of men. SLEEP 2014;37(3):571-578.
Keywords: Health literacy, obstructive sleep apnea, diagnosis, cardiovascular disease, Newest Vital Sign, cohort study, depression, men
INTRODUCTION
Prevalence studies have shown that obstructive sleep apnea (OSA) is relatively common,1–3 and three-quarters of OSA remains undiagnosed.4 The problem of under-diagnosis has significant implications given that OSA is independently associated with incident hypertension, coronary syndromes, stroke and diabetes5,6 and all-cause mortality.7–9
To date, no studies have examined the association between health literacy and sleep disorders, and Hackney et al.10 speculate that health literacy is likely to impact upon constant positive airway pressure therapy adherence and the diagnosis and management of restless legs syndrome and insomnia. Health literacy is a broad multidimensional concept that adversely affects health outcomes via causal mechanisms such as the ability to understand medical information related to health care, disease prevention, and health promotion.11 Functional Health literacy (FHL), identified with validated instruments including the Newest Vital Sign (NVS), is a more limited concept defined as the extent to which an individual can read, calculate and act on basic healthcare information (such as that entailed on prescription bottles, appointment slips, discharge instructions) in order to make informed health decisions.12 Poor FHL is highly prevalent in developed countries, with data from the United States of America and Australia suggesting that approximately half of adults have less than adequate FHL.13–15 Health literacy affects health system use/costs,13,16,17 disease knowledge and self-management behaviors,10,16,18 and health outcomes,16,19 and is broadly related to health status.16
The aim of this study therefore was to investigate the relationship between FHL (as assessed with the NVS) and OSA, its diagnosis and related risk factors and comorbidities in men participating in The Men Androgen Inflammation Lifestyle Environment and Stress (MAILES) Study, a biomedical population cohort study of men aged 40 years and over.
METHODS
Study Participants
The previously described MAILES Study20 which aims to determine factors associated with diabetes and cardiovascular disease outcomes including OSA, consists of eligible male participants from 2 concurrent longitudinal biomedical cohorts, which are largely representative of the demographics in the State of South Australia: the Florey Adelaide Male Ageing Study (FAMAS)21 and the North West Adelaide Health Study (NWAHS).22 Most data for the current study was acquired in 2010-12, from follow-up assessments; however, self-reported snoring, snorting, and choking data were acquired in 2005-2007 (MAILES Stage 1). Both FAMAS and NWAHS used the same methodology for random population sampling, and biomedical assessment was conducted in 2 hospital-based clinics, using standardized and reproducible study protocols including administration of the Newest Vital Sign (NVS, see below), blood pressure measurement, anthropometry, and a fasting blood sample drawn for lipids and glucose. Body mass index (kg/m2) was categorized according to international criteria: underweight/normal ≤ 24.9, overweight 25.0-29.9, and obesity: ≥ 30.0. Central obesity was identified using the measure of waist circumference (WC), defined as a WC ≥ 102 cm. A self-completed questionnaire collected detailed demographic information self-reported comorbidities, health-related quality of life by the SF-36, and risk factor information.
Diabetes was defined by self-report of a previous doctor diagnosis, a fasting plasma glucose ≥ 7.0 mmol/L, or glycated hemoglobin ≥ 6.5%. Nocturia was defined as voiding urine ≥ 2 times per night,23 identified by Question 7 of the International Prostate Symptom Score (“Over the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning?”). Depression was defined as a score > 12 on the Beck Depression Inventory24 (for FAMAS males) or a score ≥ 21 on the Center for Epidemiological Studies Depression Scale (for NWAHS males). Hypertension was defined as systolic blood pressure ≥ 140 mm Hg and/or diastolic ≥ 90 mm Hg, or treatment with antihypertensive medications. Cardiovascular disease was defined as self-reported myocardial infarction, angina, stroke, or transient ischemic attack. General health was measured utilizing Question 1 of the MOS Short-Form 36 Health Survey.25
No selection bias was detected at baseline,26 but due to participant attrition, the participants at follow-up are slightly better educated and self-report better general health than the general population.27
Polysomnography and Definition of OSA
MAILES study participants completed a Computer-Assisted Telephone Interview (CATI) survey in August 2010 (n = 1,629). Figure S1 in the supplemental material shows the flow of participants through the study. This survey included questions regarding demographical, biographical and comorbidities information. Subjects reporting “yes” to “Have you ever been diagnosed with obstructive sleep apnea with a sleep study?” (n = 184) were considered to have previously diagnosed OSA and were not asked to undertake a further sleep study. The subjects reporting “no” to the same question were invited to undergo a sleep study, with 75.2% (1,087 out of 1,445) agreeing. Of these, a random sample (n = 857) undertook an 8-channel in-home unattended polysomnography (PSG) (Embletta X100, Embla Systems, Colorado), the equipment for which was set up and attached by trained staff. The PSG measured EEG, EOG, EMG, nasal pressure, thoracic and abdominal effort, oximetry, body position, and limb movements. Failed PSGs were repeated where possible. The Epworth Sleepiness Scale (ESS)28 was administered, and measures of height, weight, and WC were also taken. Any necessary clinical follow-up was coordinated by a physician investigator, the results were made available to participants and, if the participant consented, results were sent to their primary care practitioner.
All PSGs were manually scored by a single experienced sleep technician, according to the 2007 American Academy of Sleep Medicine (AASM) (alternative) criteria.29 Apneas were defined as cessations of nasal flow lasting ≥ 10 seconds. Hypopneas were defined as > 50% decrease in nasal flow (or in both thoracic and abdominal excursions) and associated with either ≥ 3% oxygen desaturation or an EEG arousal. An apneahypopnea index (AHI) ≥ 10 events per hour of sleep by these criteria has been shown to be approximately equivalent to an AHI of at least 5/h of sleep used in earlier studies3,30 and so was the definition used in this study.
Newest Vital Sign (NVS)
The Newest Vital Sign (NVS) is a validated screening tool used to identify individuals at risk of limited functional health literacy.31,32 It can be administered in 3 minutes and was designed for use in primary care. The NVS asks patients to read and interpret a standardized nutrition label derived from an ice cream container, about which they are asked 6 standardized questions. There is only one correct answer per question resulting in a score ranging from 0 to 6. A score of 4-6 almost always indicates adequate FHL (“adequate”), while a score of 2-3 indicates the possibility of limited FHL (“at risk”), and a score of 0-1 indicates ≥ 50% likelihood of limited FHL (“inadequate”). A score of 0-3, which indicates inadequate or at risk FHL, is described in this article as “less than adequate.”31 A standardized approach to the administration of the NVS was taken by the 2 clinic staff, and coaching was not permitted.
Statistical Analysis
Data were analyzed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Univariate associations of FHL with demographics, risk factors, and comorbidities were determined using the χ2 test. To determine factors independently associated with not being diagnosed with OSA in the all OSA population (consisting of the previously diagnosed and previously undiagnosed), a multivariable logistic regression model was constructed containing all variables found to have a univariate association of χ2 P-value ≤ 0.25, including age, income and education, BMI, plus daytime sleepiness, which is traditionally believed to be associated with OSA despite a P-value > 0.25 in our cohort. Only previous snoring was included in the model as a measure of previous symptoms, because other symptomatology largely identified the same men.
In the men who undertook polysomnography, the logistic regression model assessing the association of FHL with undiagnosed OSA was adjusted for age, income, education, and BMI. In men with previously undiagnosed OSA (Table 3) and previously diagnosed OSA (Table 4), the logistic regression models determining associations of less than adequate FHL with OSA-related risk factors and comorbidities (which included BMI) were adjusted for age, income, and education.
Table 3.
FHL [% (n)] in relation to comorbidities and risk factors in men with previously undiagnosed OSA (n = 382), with adjusted odds ratios† for less than adequate levels of FHL
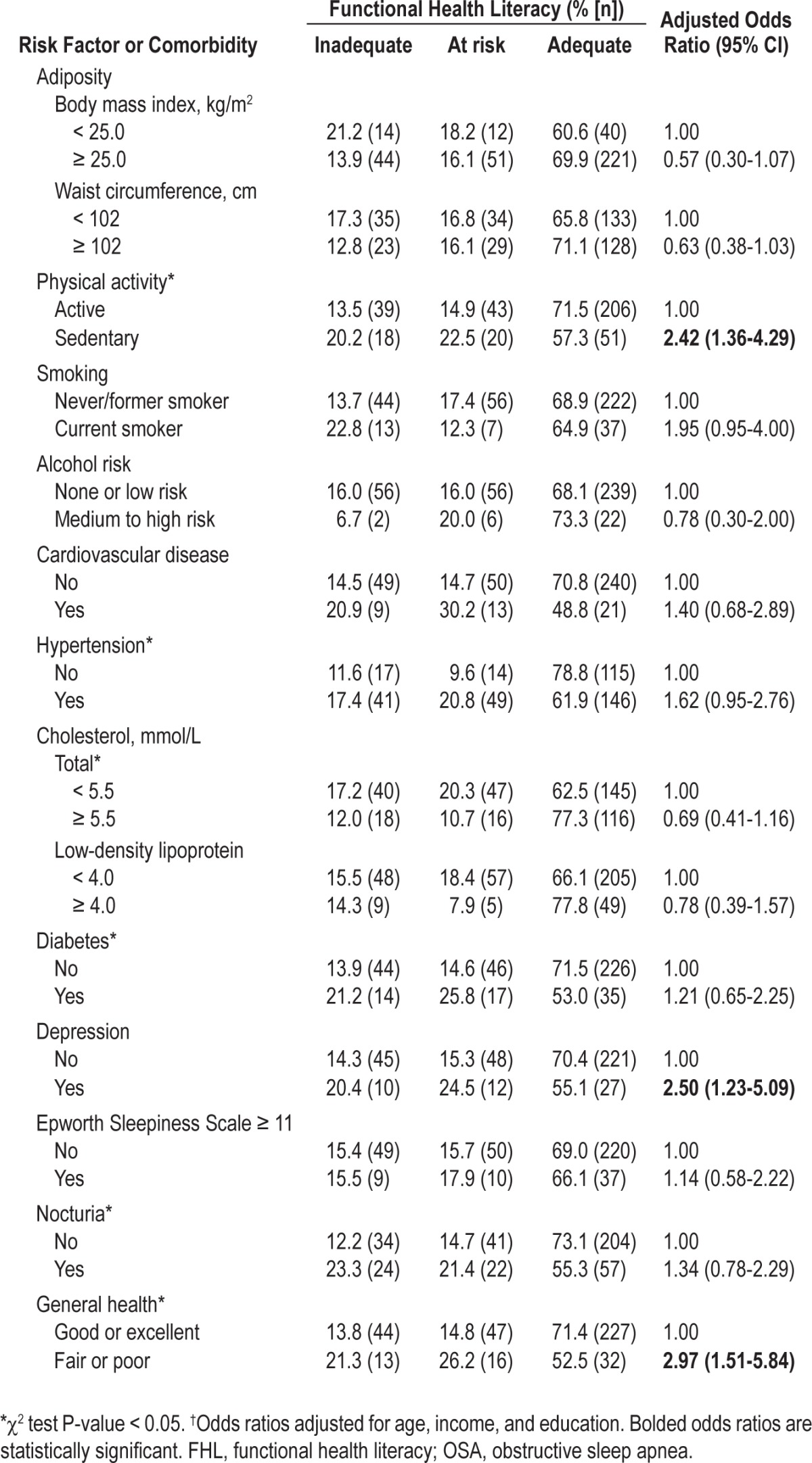
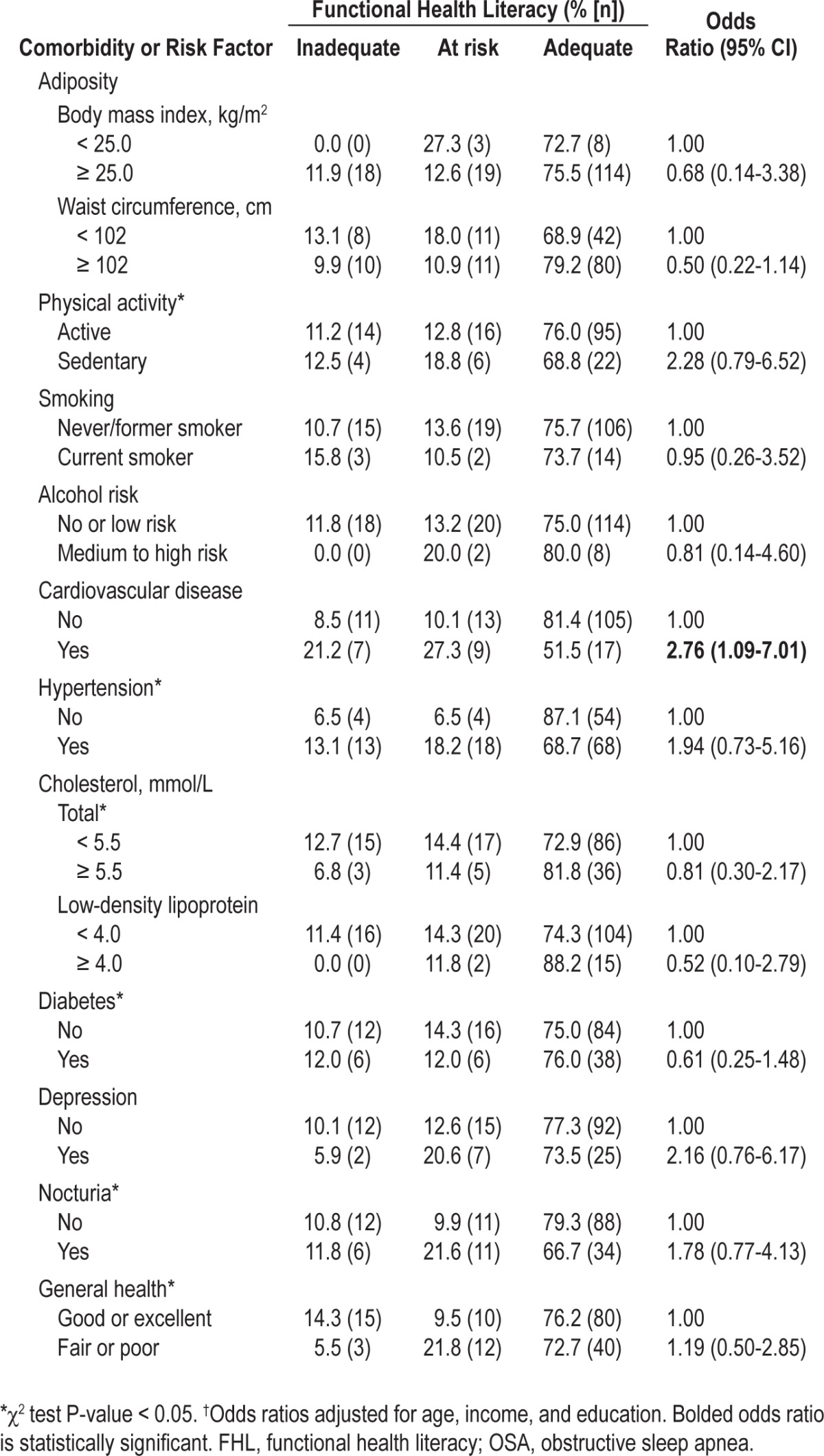
Table 4.
Functional health literacy [FHL, %, (n)] in relation to comorbidities and risk factors in previously diagnosed OSA (n = 162), and adjusted odds ratios† for less than adequate levels of FHL
All protocols herein were approved by the Research Ethics Committees of the Royal Adelaide Hospital and the North West Adelaide Health Service. All participants gave written informed consent.
RESULTS
Complete NVS data were available in 162 of the 184 participants (88.0%) with a previous diagnosis of OSA. The NVS was completed in 740 of 837 participants who undertook a PSG (88.4%). Of these 740 men, an AHI ≥ 10 was demonstrated in 382 (51.6%) who were termed “previously undiagnosed OSA.” FHL was adequate in 75.3% (n = 122) of previously diagnosed and 68.3% (n = 261) of previously undiagnosed OSA.
Factors Associated with Previously Undiagnosed OSA
Table 1 shows the FHL, demographic and biomedical characteristics of men with OSA in relation to diagnosis of their OSA. In univariate analyses, compared to the men who self-reported a previous diagnosis of OSA, men with OSA identified in this study by PSG (i.e. previously undiagnosed) were significantly more likely to be younger, report higher annual income, be workforce participants, and were less likely to report previous snoring or have comorbidities including obesity, cardiovascular disease (CVD), diabetes, and depression. These associations largely persisted in logistic regression analysis (except age, income, and depression), and men with previously undiagnosed OSA were also more likely to have inadequate FHL.
Table 1.
Functional health literacy, demographic and biomedical characteristics [% (n)] of men with OSA in relation to diagnosis, and adjusted odds ratios* of factors associated with previously undiagnosed OSA
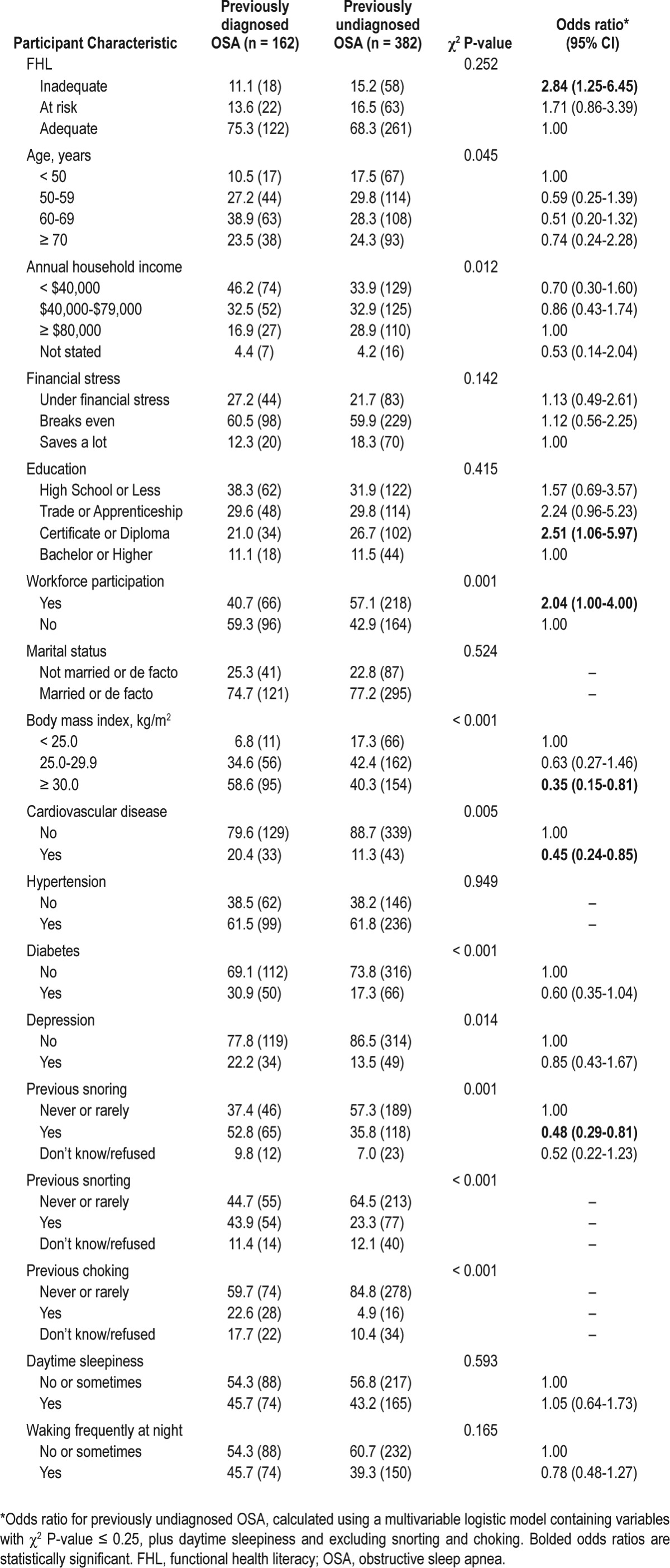
It was unclear what criteria were used to diagnose the men who self-reported OSA, and in order to account for a possible diagnostic bias of a more severe OSA presentation in these men, we also performed the above analysis comparing moderate-to-severe previously undiagnosed OSA (AHI ≥ 20 events/h) with previously diagnosed OSA (Table S1, supplemental material). In the logistic regression model, men with moderate-to-severe previously undiagnosed OSA had an increased likelihood of having inadequate FHL (OR 2.41, 95% CI 0.97-6.00), though this was of borderline significance (P = 0.059) and be significantly less likely to report previous snoring and have diabetes.
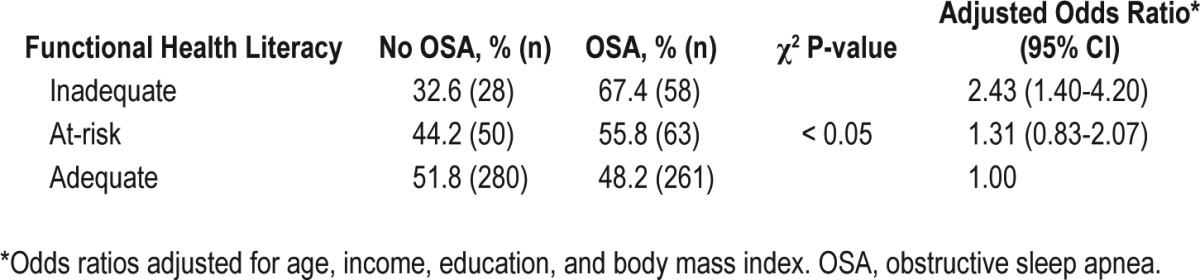
Relationship between FHL and Previously Undiagnosed OSA
In the population of men who underwent a PSG, compared to men with adequate FHL, those with inadequate FHL were significantly more likely to have previously undiagnosed OSA, and this association persisted after adjusting for age, income, education, and BMI (Table 2). No significant association between FHL and OSA severity was observed (P = 0.79).
Table 2.
Association between functional health literacy and previously undiagnosed OSA in men undergoing polysomnography (n = 740), and adjusted odds ratios* for undiagnosed OSA
Factors Associated with Less than Adequate FHL in Previously Undiagnosed OSA
Table 3 shows the relationship between FHL and OSA-related comorbidities and risk factors in the men with OSA identified by PSG (previously undiagnosed). There were significant univariate associations between FHL and CVD, hypertension, total cholesterol, sedentary lifestyle, diabetes, nocturia, and general health. In the adjusted models, associations persisted with depression, poor to fair general health, and sedentary lifestyle, and borderline associations were observed with hyper-tension, current smoking, lower WC, and lower BMI levels. In separate analyses of factors associated with inadequate FHL (data not shown), inadequate FHL (i.e., NVS score of 0-1) was significantly associated with current smoking (OR = 2.87, 95% CI 1.21-6.84), and lower WC (OR 0.52, 95% CI 0.27-0.99).
In the additional logistic regression analyses of depression (data not shown), the significant relationship with less than adequate FHL persisted after additional adjustment for marital status and comorbidities including obesity, CVD, and diabetes (P = 0.016, OR = 2.45, 95% CI 1.18-5.09). However, further additional adjustment for general health was made to account for residual confounding by other health factors. In this final model, the association between less than adequate FHL and depression was attenuated, and of borderline significance (P = 0.076).
Factors Associated with Less than Adequate FHL in Men with a Prior Diagnosis of OSA
Table 4 shows the relationship between FHL and OSA-related comorbidities and risk factors in previously diagnosed OSA. Univariate associations were found between FHL and presence of CVD, hypertension, and general health. After adjusting for age, income, and education, the relationship between less than adequate FHL and CVD persisted. The adjusted odds ratios for the associations between less than adequate FHL and hyper-tension, sedentary lifestyle were elevated, but the associations were not statistically significant.
DISCUSSION
Our results suggest that in men with OSA, those with inadequate functional health literacy are likely to remain undiagnosed. This is the first study to describe this relationship and confirms previous studies that have implicated health literacy as a determinant of health status.16,19 Undiagnosed men are almost three times as likely to have inadequate functional health literacy as diagnosed men, even after adjusting for demographics, symptomatology, and comorbidities. Health literacy is therefore an important determinant in OSA diagnosis. A possible explanation for this may be that the significance of OSA symptoms is not recognized by patients, bed partners, or clinicians. OSA is a unique disease in that bed partners commonly drive the referral and consultation process, and so the health literacy of bed partners may be important to investigate in future research. Snoring is arguably the most important symptom to recognize in patients at risk of sleep apnea, as other common symptoms including daytime sleepiness are not reported in a large proportion of patients.33 As 36% of the undiagnosed men (and 40% of the men with moderate-to-severe undiagnosed OSA) had reported significant snoring at least five years before the diagnosis was made by PSG in this study, it seems likely that the issue of snoring does not get addressed. Furthermore, there is likely to be a lower level of clinical suspicion in men with lower waist circumference and BMI, resulting in a sleep history not being pursued. Therefore a connection between their sleep disordered breathing and other health problems may not be made. If those men also concurrently have inadequate FHL, then they may not recognize the significance of their symptoms and/or not adequately articulate their symptoms or concerns to their primary care practitioners. Their OSA would have thereby remained undiagnosed until they were randomly sampled to undergo PSG for our study. This could explain the association between inadequate FHL and lower waist circumference found in our study, and is supported by the lack of significant association between FHL and WC and BMI in the previously diagnosed men. Public education initiatives and further professional development for clinicians to increase knowledge of the significance of snoring should be investigated, especially given the low sensitivity of the current clinical approach34 and the low uptake of OSA screening tools such as the long-standing Berlin questionnaire35 in primary care. It is unclear whether current screening tools such as the Berlin35 and OSA5036 questionnaires are as clinically useful in people with low FHL as in others, and research on this should be encouraged.
Low FHL was independently associated with undiagnosed OSA, and also with sedentary lifestyle and current smoking, factors related to the development of OSA.37 There is evidence that people with low health literacy are less likely to adopt lifestyle changes,38 although it is unclear whether this applies specifically to people with OSA. Our results suggest that education regarding lifestyle modification among people with OSA needs to be formulated with health literacy in mind, with an emphasis on clarity of communication. Although there have been recent improvements, much written information for consumers regarding sleep apnea is beyond the easy comprehension of the majority of adults, and further improvements must still be made.39 Recognition also needs to be given to the problem of low income, often concurrent with FHL limitations, and the effect this can have on the management of OSA.40 While there is a clear gradient of poorer health literacy occurring with decreasing social advantage,14 we have previously shown that even among those with a bachelor degree or higher, around 20% were at risk of limited FHL.13 Thus educational level is a poor proxy measure of health literacy and will misclassify a substantial proportion of people as health literate/illiterate14 and this also needs consideration in the clinical management of OSA when taken together with evidence suggesting that clinicians may overestimate patients' literacy skills.41
We found that less than adequate FHL was associated with depression in men with undiagnosed OSA when adjusted for demographics, marital status, and comorbidities, but not after also adjusting for general health, a similar result to that previously found in an elderly population.42 However, we also found that less than adequate FHL is negatively associated with general health. As such, the direction of causality, if any exists, between the three factors of FHL, depression, and general health is unclear. Nonetheless, depression is highly prevalent in OSA patients,37 and there is some, albeit limited, evidence that poor health literacy adversely affects depression management,43 and is correctable by a health literacy intervention.44
In the men with diagnosed OSA, we found an independent association between less than adequate FHL and cardiovascular disease. Health literacy therefore has management implications given that cardiovascular disease is a major comorbidity of obstructive sleep apnea8,9 and is also a major contributor to all-cause mortality seen in OSA patients.7,8 While there were no other significant associations found in the men with diagnosed OSA, the low sample size (n = 162) of previously diagnosed men may have contributed to a possible type II error. It is unclear whether the elevated, but not statistically significant, odds ratios for the associations between FHL and hypertension, sedentary lifestyle, and depression represent true clinical associations in men with OSA. Further studies with larger sample sizes are required to determine this.
Our study was limited to men and therefore the results of our study cannot be generalized to women. Another possible limitation of this study may have been the chosen measure of functional health literacy. Although the NVS is a validated measure of FHL,31,45 it tends to identify more people with less than adequate FHL when compared to the Test of Functional Health Literacy in Adults (TOFHLA).46 However, commentators have previously suggested that none of the current brief measures of health literacy test for all aspects of health literacy in a comprehensive manner,47,48 and so it is unclear which health literacy measure is superior to the other in that regard. Furthermore, we have previously shown13 that the NVS identifies a similar proportion of the general population with inadequate FHL as the much longer tools used in international literacy comparison studies such as the Adult Literacy and Life Skills Survey.14 In addition, the NVS can be administered in three minutes,31 and a previous study found over 98% of patients agreed to take the NVS during a routine visit, without any significant adverse effect on patient satisfaction.49
The definition of OSA used in the study may also have been a possible limitation. Our definition of OSA as AHI ≥ 10 events/ hour of sleep by the 2007 AASM (alternative) criteria is approximately equivalent to AHI ≥ 530 used in earlier studies,3 and generated a prevalence consistent with the significant increases in modeled prevalence estimates recently reported by Peppard et al.,1 but did not consider whether participants were symptomatic. Furthermore, we did not know what criteria were used by clinicians for the previously diagnosed cases of OSA in our sample. However, our sensitivity analysis utilizing the higher cut-off of AHI ≥ 20 in an attempt to account for a possible diagnostic bias of a more severe OSA presentation in the previously diagnosed men yielded similar results, suggesting the findings are robust. Thus, FHL limitations are likely to be contributing to not being diagnosed with moderate to severe OSA in men despite their high AHI and snoring history in 40% and sleepiness in 47%, although they are without related comorbidity (such as diabetes).
In conclusion, we have demonstrated an independent association between poor functional health literacy and OSA, together with its associated risk factors and comorbidities. The prevalence of obesity, particularly severe obesity, is increasing,50 and is likely to be accompanied by an increase in the prevalence of OSA.51 Our data highlight the importance of public health policy initiatives that aim to increase public awareness of the significance of OSA and its symptoms such as snoring.52–54 Our findings also indicate the need for clinicians to undertake an adequate sleep history using a “universal precautions” approach, with clear and simple communication that avoids complex jargon.
DISCLOSURE STATEMENT
This study was supported by the National Health and Medical Research Council of Australia grant number: 627227; The Resmed Foundation, California, USA. Embla Systems, Colorado contributed a number of Embletta X100 devices.
Dr. Wittert has received research support from the National Health and Medical Research Council of Australia and The ResMed Foundation and equipment donations from Embla Systems. Dr. Vakulin has received research support from the National Health and Medical Research Council of Australia. Dr. McEvoy has received research support from the National Health and Medical Research Council of Australia, the ResMed Foundation, Philips Respironics, and Fisher and Paykel, equipment donations from ResMed, Philips Respironics and SomnoMed, and lecture fees from Philips Respironics. Dr. Antic has received research support from the National Health and Medical Research Council of Australia, Philips Respironics, and Fisher and Paykel; equipment donations from ResMed, Philips Respironics and SomnoMed; and lecture fees and payment for development of educational presentations from ResMed. Dr. Adams has received research support from the National Health and Medical Research Council of Australia, and The ResMed Foundation, and Equipment donations from Embla Systems. The other authors have indicated no financial conflicts of interest. This work was conducted at The University of Adelaide, Adelaide, South Australia.
SUPPLEMENTAL MATERIAL
The MAILES study: polysomnography (PSG) recruitment, Newest Vital Sign (NVS) completion and participant flow throughout the study. *Reasons for 40 initial failed studies: n = 19 TST not ≥ 3.5 hours from ≥ 5 hours recording; n = 3 poor respiratory signals; n = 2 poor EEG; n = 13 no SaO2; n = 3 All traces/recording failed. Of 23 repeated studies, 20 were valid and 3 failed (n = 2 TST not ≥ 3.5 hours from ≥ 5 hours recording; n = 1 no SaO2) of which 1 was repeated and valid.
Functional health literacy (FHL), demographic and biomedical characteristics (% [n]) of men with obstructive sleep apnea (OSA) in relation to diagnosis, and adjusted odds ratios* of factors associated with moderate-to-severe previously undiagnosed OSA (AHI ≥ 20 events/h)
REFERENCES
- 1.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–14. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindberg E. Epidemiology of OSA. Eur Respir Soc Monograph. 2010;50:51–68. [Google Scholar]
- 3.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 4.Kapur V, Strohl KP, Redline S, Iber C, O'Connor G, Nieto J. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath. 2002;6:49–54. doi: 10.1007/s11325-002-0049-5. [DOI] [PubMed] [Google Scholar]
- 5.Levy P, Tamisier R, Minville C, Launois S, Pepin JL. Sleep apnoea syndrome in 2011: current concepts and future directions. Eur Respir Rev. 2011;20:134–46. doi: 10.1183/09059180.00003111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X, Bi Y, Zhang Q, Pan F. Obstructive sleep apnoea and the risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Respirology. 2013;18:140–6. doi: 10.1111/j.1440-1843.2012.02267.x. [DOI] [PubMed] [Google Scholar]
- 7.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–85. [PMC free article] [PubMed] [Google Scholar]
- 8.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–8. [PMC free article] [PubMed] [Google Scholar]
- 10.Hackney JE, Weaver TE, Pack AI. Health literacy and sleep disorders: a review. Sleep Med Rev. 2008;12:143–51. doi: 10.1016/j.smrv.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Sorensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nielsen-Bohlman L, Panzer AM, Hamlin B, et al. Health literacy: a prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 13.Adams RJ, Appleton SL, Hill CL, Dodd M, Findlay C, Wilson DH. Risks associated with low functional health literacy in an Australian population. Med J Aust. 2009;191:530–4. doi: 10.5694/j.1326-5377.2009.tb03304.x. [DOI] [PubMed] [Google Scholar]
- 14.Australian Bureau of Statistics. Adult Literacy and Life Skills Survey, Summary Results, Australia, 2006 (Reissue) Commonwealth of Australia. 2008 [Google Scholar]
- 15.Kutner M, Greenberg E, Jin Y, Paulsen C. Washington, DC: National Center for Education Statistics; 2006. The health literacy of America's adults: results from the 2003 National Assessment of Adult Literacy. (NCES 2006-483). U.S. Department of Education. [Google Scholar]
- 16.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howard DH, Gazmararian J, Parker RM. The impact of low health literacy on the medical costs of Medicare managed care enrollees. Am J Med. 2005;118:371–7. doi: 10.1016/j.amjmed.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 19.Adams RJ, Appleton SL, Hill CL, Ruffin RE, Wilson DH. Inadequate health literacy is associated with increased asthma morbidity in a population sample. J Allergy Clin Immunol. 2009;124:601–3. doi: 10.1016/j.jaci.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 20.Grant JF, Martin SA, Taylor AW, et al. Cohort Profile: The Men Androgen Inflammation Lifestyle Environment and Stress (MAILES) Study. Int J Epidemiol. 2013 Jun 19; doi: 10.1093/ije/dyt064. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin SA, Haren MT, Middleton SM, Wittert GA. Members of the Florey Adelaide Male Ageing Study. The Florey Adelaide Male Ageing Study (FAMAS): design, procedures & participants. BMC Public Health. 2007;7:126. doi: 10.1186/1471-2458-7-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant JF, Taylor AW, Ruffin RE, et al. Cohort Profile: The North West Adelaide Health Study (NWAHS) Int J Epidemiol. 2008;38:1479–86. doi: 10.1093/ije/dyn262. [DOI] [PubMed] [Google Scholar]
- 23.Weiss JP, Blaivas JG, Bliwise DL, et al. The evaluation and treatment of nocturia: a consensus statement. BJU Int. 2011;108:6–21. doi: 10.1111/j.1464-410X.2011.10175.x. [DOI] [PubMed] [Google Scholar]
- 24.Lasa L, Ayuso-Mateos JL, Vázquez-Barquero JL, Díez-Manrique FJ, Dowrick CF. The use of the Beck Depression Inventory to screen for depression in the general population: a preliminary analysis. J Affect Disord. 2000;57:261–5. doi: 10.1016/s0165-0327(99)00088-9. [DOI] [PubMed] [Google Scholar]
- 25.McHorney CA, Ware JE, Jr., Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Taylor AW, Dal Grande E, Gill T, et al. Do people with risky behaviours participate in biomedical cohort studies? BMC Public Health. 2006;6:11. doi: 10.1186/1471-2458-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor AW, Dal Grande E, Grant J, et al. Weighting of the data and analytical approaches may account for differences in overcoming the inadequate representativeness of the respondents to the third wave of a cohort study. J Clin Epidemiol. 2013;66:461–4. doi: 10.1016/j.jclinepi.2012.06.021. [DOI] [PubMed] [Google Scholar]
- 28.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 29.Iber C, Ancoli-Israel S, Chesson A, Jr, Quan SF. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 30.Ruehland WR, Rochford PD, O'Donoghue FJ, Pierce RJ, Singh P, Thornton AT. The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index. Sleep. 2009;32:150–7. doi: 10.1093/sleep/32.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–22. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rowlands G, Khazaezadeh N, Oteng-Ntim E, Seed P, Barr S, Weiss BD. Development and validation of a measure of health literacy in the UK: the newest vital sign. BMC Public Health. 2013;13:116. doi: 10.1186/1471-2458-13-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ. Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep. 2005;28:472–7. doi: 10.1093/sleep/28.4.472. [DOI] [PubMed] [Google Scholar]
- 34.Rahaghi F, Basner RC. Delayed diagnosis of obstructive sleep apnea: don't ask, don't tell. Sleep Breath. 1999;3:119–24. doi: 10.1007/s11325-999-0119-z. [DOI] [PubMed] [Google Scholar]
- 35.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 36.Chai-Coetzer CL, Antic NA, Rowland LS, et al. A simplified model of screening questionnaire and home monitoring for obstructive sleep apnoea in primary care. Thorax. 2011;66:213–9. doi: 10.1136/thx.2010.152801. [DOI] [PubMed] [Google Scholar]
- 37.Heatley EM, Harris M, Battersby M, McEvoy RD, Chai-Coetzer CL, Antic NA. Obstructive sleep apnoea in adults: A common chronic condition in need of a comprehensive chronic condition management approach. Sleep Med Rev. 2013;17:349–55. doi: 10.1016/j.smrv.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 39.Adams R, Sowden J, Hill C, Visvanathan R, Gill T, Appleton S. Readability assessment of consumer information material on sleep and health from Australian websites. Sleep Biol Rhythms. 2012;10:61. [Google Scholar]
- 40.Bakker JP, O'Keeffe KM, Neill AM, Campbell AJ. Ethnic disparities in CPAP adherence in New Zealand: effects of socioeconomic status, health literacy and self-efficacy. Sleep. 2011;34:1595–603. doi: 10.5665/sleep.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kelly PA, Haidet P. Physician overestimation of patient literacy: a potential source of health care disparities. Patient Educ Couns. 2007;66:119–22. doi: 10.1016/j.pec.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 42.Gazmararian J, Baker D, Parker R, Blazer DG. A multivariate analysis of factors associated with depression: evaluating the role of health literacy as a potential contributor. Arch Intern Med. 2000;160:3307–14. doi: 10.1001/archinte.160.21.3307. [DOI] [PubMed] [Google Scholar]
- 43.Bauer AM, Schillinger D, Parker MM, et al. Health literacy and antidepressant medication adherence among adults with diabetes: the diabetes study of Northern California (DISTANCE) J Gen Intern Med. 2013;28:1181–7. doi: 10.1007/s11606-013-2402-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gulliver A, Griffiths KM, Christensen H, Brewer JL. A systematic review of help-seeking interventions for depression, anxiety and general psychological distress. BMC Psychiatry. 2012;12:81. doi: 10.1186/1471-244X-12-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Osborn CY, Weiss BD, Davis TC, et al. Measuring adult literacy in health care: performance of the newest vital sign. Am J Health Behav. 2007;31(Suppl 1):S36–46. doi: 10.5555/ajhb.2007.31.supp.S36. [DOI] [PubMed] [Google Scholar]
- 46.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 47.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–83. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67:2072–8. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 49.Ryan JG, Leguen F, Weiss BD, et al. Will patients agree to have their literacy skills assessed in clinical practice? Health Educ Res. 2008;23:603–11. doi: 10.1093/her/cym051. [DOI] [PubMed] [Google Scholar]
- 50.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11:441–6. doi: 10.1016/j.sleep.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 52.National Health and Hospitals Reform Commission. A healthier future for all Australians - final report 2009. Commonwealth of Australia. 2009 doi: 10.5694/j.1326-5377.2009.tb02845.x. [DOI] [PubMed] [Google Scholar]
- 53.Rudd R, Kirsch I, Yamamato K. Literacy and Health in America. Princeton, NJ: Educational Testing Service; 2004. [Google Scholar]
- 54.Adams RJ. Improving health outcomes with better patient understanding and education. Risk Manag Health Policy. 2010;3:61–72. doi: 10.2147/RMHP.S7500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The MAILES study: polysomnography (PSG) recruitment, Newest Vital Sign (NVS) completion and participant flow throughout the study. *Reasons for 40 initial failed studies: n = 19 TST not ≥ 3.5 hours from ≥ 5 hours recording; n = 3 poor respiratory signals; n = 2 poor EEG; n = 13 no SaO2; n = 3 All traces/recording failed. Of 23 repeated studies, 20 were valid and 3 failed (n = 2 TST not ≥ 3.5 hours from ≥ 5 hours recording; n = 1 no SaO2) of which 1 was repeated and valid.
Functional health literacy (FHL), demographic and biomedical characteristics (% [n]) of men with obstructive sleep apnea (OSA) in relation to diagnosis, and adjusted odds ratios* of factors associated with moderate-to-severe previously undiagnosed OSA (AHI ≥ 20 events/h)


