Abstract
Introduction:
Legislation requires the U.S. Food and Drug Administration (FDA) to release information to the public about harmful constituents in tobacco and tobacco smoke. To inform these efforts, we sought to better understand how smokers and nonsmokers think about tobacco constituents.
Methods:
In October 2012, 300U.S. adults aged 18–66 years completed a cross-sectional Internet survey. The questions focused on 20 harmful tobacco constituents that the FDA has prioritized for communicating with the public.
Results:
Most participants had heard of 7 tobacco constituents (ammonia, arsenic, benzene, cadmium, carbon monoxide, formaldehyde, and nicotine), but few participants had heard of the others (e.g., acrolein). Few participants correctly understood that many constituents were naturally present in tobacco. Substances that companies add to cigarette tobacco discouraged people from wanting to smoke more than substances that naturally occur in cigarette smoke (p < .001). Ammonia, arsenic, carbon monoxide, and formaldehyde being in cigarettes elicited the most discouragement from smoking. Constituents elicited greater discouragement from wanting to smoke if respondents were nonsmokers (β = −.34, p < .05), had negative images of smokers (i.e., negative smoker prototypes; β = .19, p < .05), believed constituents are added to tobacco (β = .14, p < .05), or were older (β = .16, p < .05).
Conclusions:
Our study found low awareness of most tobacco constituents, with greater concern elicited by additives. Efforts to communicate health risks of tobacco constituents should consider focusing on ones that elicited the most discouragement from smoking.
INTRODUCTION
Cigarette smoking causes around one of five deaths in the United States, or more than 440,000 deaths per year, primarily from cardiovascular disease, cancer, and respiratory disease (Centers for Disease Control and Prevention, 2012a; Mokdad, Marks, Stroup, & Gerberding, 2004). Most of the harms from smoking come from tobacco constituents that are naturally present in tobacco (Hecht, 2012). Manufacturers also add substances, called additives, such as flavors. Some substances, like ammonia and nicotine, are classified as constituents because they are naturally present in tobacco but are also sometimes added to tobacco products by tobacco manufacturers (Wayne & Carpenter, 2009).
Tobacco products and cigarette smoke contain more than 5,000 constituents, many of which are toxic to human health (Rodgman & Perfetti, 2008; Talhout et al., 2011; U.S. Food and Drug Administration, 2012b). Carcinogenic constituents include 1,3-butadiene, formaldehyde, nicotine-derived nitrosamine ketone (NNK), N-nitrosonornicotine, and benzene (Biener, Nyman, Stepanov, & Hatsukami, 2013; Fowles & Dybing, 2003; Hecht, 2012; International Agency for Research on Cancer, 2004). Acrolein and acetaldehyde are two of the most harmful constituents to respiratory health, and arsenic and hydrogen cyanide pose great cardiovascular health risk (Fowles & Dybing, 2003). In addition to direct health effects, some of these constituents (e.g., nicotine) may cause indirect harm to consumers by hindering cessation or leading to higher intensity or frequency of tobacco use (U.S. Food and Drug Administration, 2011).
Federal law requires the U.S. Food and Drug Administration (FDA) to disseminate information about tobacco constituents. The 2009 Family Smoking Prevention and Tobacco Control Act grants FDA broad authority to regulate tobacco products, including helping the public to better understand the harms of constituents present in tobacco products (United States Public Laws, 2009). The FDA identified 93 such constituents in tobacco products and tobacco smoke (U.S. Food and Drug Administration, 2012a) and later released an abbreviated list of 20 high-priority harmful tobacco constituents (U.S. Food and Drug Administration, 2012b). In 2012, FDA required manufacturers to submit quantities of constituents for their cigarette brands on the abbreviated list (U.S. Food and Drug Administration, 2012b; United States Public Laws, 2009). In 2013, FDA is required to release this information to the public in a way that is both “understandable” and “not misleading” (U.S. Food and Drug Administration, 2011). This event will mark the first time that smokers will ever see brand-specific constituent information.
Investigating awareness of and attitudes toward constituents can inform strategies to effectively communicate the health risks associated with harmful and potentially harmful constituents to smokers and nonsmokers. However, very little is known about the public’s perception of tobacco constituents and whether they discourage smoking. For example, it is unclear whether lesser-known constituents elicit more fear and concern among the public than commonly known constituents that might be perceived as overly familiar or “worn-out.” To our knowledge, this is the first study to assess the extent to which tobacco constituents discourage people from smoking. Several countries, including Australia, Canada, Spain, and the United Kingdom, have incorporated information about constituents in tobacco product warnings (Hammond, 2009). If the United States follows suit, it will be even more important to understand how the public responds to information about harmful constituents. Thus, our study sought to (a) characterize adults’ awareness of 20 constituents on FDA’s priority list of harmful tobacco constituents, (b) identify the extent to which these 20 constituents discourage adults from wanting to smoke, and (c) identify factors that influence whether constituents discourage people from wanting to smoke.
METHODS
Participants and Procedures
In October 2012, we recruited a convenience sample of 300U.S. cigarette smokers and nonsmokers aged 18 or older to complete a survey about the chemicals found in cigarettes and cigarette smoke. The recruitment message encouraged smokers to participate with text that read, “We are especially hoping for smokers and tobacco users to take our survey, although this is not required.” As health warnings can prevent smoking initiation among nonsmokers and promote cessation among smokers (Hammond, 2011), we included both smokers and nonsmokers. Recruitment happened through Amazon Mechanical Turk (MTurk), a web-based platform commonly used for social science and experimental research (Berinsky, Huber, & Lenz, 2012; Buhrmester, Kwang, & Gosling, 2011; Paolacci, Chandler, & Ipeirotis, 2010; Rand, 2012). MTurk advertises human intelligence tasks (HITs) to users who are invited to complete the HIT and receive a reward for successful completion. Our quality control procedure specified that we would reject a HIT if fewer than 95% of the questions were answered, but no HITs met this threshold for exclusion. We completed recruitment within 2hr of posting the announcement. After providing informed consent, participants completed a 130-item online questionnaire (mean time to completion: 20min). Participants received $5 USD after completing the survey. The University of North Carolina at Chapel Hill Institutional Review Board approved this study.
Measures
Awareness, Worry, and Discouragement
The survey assessed awareness, worry, and discouragement for constituents in cigarette smoke. The 20 constituents appear on FDA’s abbreviated list of harmful and potentially harmful constituents to be reported by tobacco product manufacturers (U.S. Food and Drug Administration, 2011), though two constituents (arsenic and cadmium) are on the priority list for smokeless tobacco, roll-your-own tobacco, and cigarette filler but not for cigarette smoke. The survey introduced the topic as being about “ingredients sometimes found in tobacco.” The survey assessed constituent awareness by asking participants if they had heard of each constituent. The survey assessed worry by asking “how much would [constituent] being in cigarettes make you feel worried about the harms of smoking?” The 5-point response scale ranged from “not at all” (coded as 1) to “very” (coded as 5). To assess discouragement, the survey asked participants “how much would [constituent] being in cigarettes discourage you from wanting to smoke cigarettes?” The 5-point response scale read “not at all” (1), “a little bit” (2), “somewhat” (3), “quite a bit” (4), and “very much” (5). The three questions appeared as a block for each constituent, with a different random order of blocks for each participant to minimize confounding due to order effects. We created a discouragement score, averaged across the 20 items (α = .97).
Beliefs About Sources of Constituents
The survey assessed participants’ beliefs about sources of constituents in cigarettes using two methods: spontaneous recall and recognition of the constituent when presented. The survey stated, “Some chemicals or ingredients are naturally in smoke from burning cigarettes. Tobacco also has ‘additives,’ which are chemicals or ingredients that cigarette companies add.” The survey asked participants to list some of the chemicals or ingredients they think are naturally in cigarette smoke and to list some of chemicals or ingredients they think companies add to cigarette tobacco. Then, the survey listed the 20 constituents and asked participants to select whether they believed the constituent is naturally in tobacco smoke, added to cigarette tobacco, or both. We created variables for the count of the numbers of constituents respondents thought were naturally present and added to tobacco.
Smoker Prototype
The survey included a 12-item smoker prototype scale to measure participants’ attitudes toward smokers (McCool, Cameron, & Petrie, 2004; McCool, Cameron, & Robinson, 2011; Pepper et al., 2013). The main question stem asked participants to what extent they thought that 12 adjectives described a typical person who smokes. The 5-point response scale ranged from “not at all” (1) to “very much” (5). For each participant, we calculated an average score for the seven positive characteristics (stylish, tough, cool, sexy, intelligent, independent, and classy; α = .86) and for the five negative characteristics (immature, inconsiderate, self-centered, trashy, and unattractive; α = .85). Previous studies have shown smoker prototypes as being highly predictive of smoking-related attitudes and behavior. Specifically, those who have negative perceptions of the “typical smoker” are less likely to smoke (Gibbons & Eggleston, 1996; Gibbons, Helweg-Larsen, & Gerrard, 1995). A more recent study found that having more negative beliefs about the typical smoker was associated with lower willingness to try e-cigarettes (Pepper et al., 2013). Similarly, we hypothesized that adults with negative images of smokers would be more discouraged from smoking by constituents while those with positive images of smokers would be less discouraged.
Demographics and Tobacco Use
The survey assessed age, sex, education, race and ethnicity, area of residence (rural, suburban, or urban), and annual household income. We also measured sexual orientation; gays, lesbians, and bisexuals are an important and understudied vulnerable group because they are much more likely to smoke than their heterosexual counterparts. (Centers for Disease Control and Prevention, 2012a; Lee, Griffin, & Melvin, 2009). We measured health literacy using the Newest Vital Sign, a six-item screening tool to identify individuals at risk for low literacy (Weiss et al., 2005). Consistent with the definition used by the Centers for Disease Control and Prevention, we defined current smokers as those who reported having smoked at least 100 cigarettes during their lifetime and reported smoking every day or some days at the time of the survey (Centers for Disease Control and Prevention, 2012a). For use of other tobacco products, we created a composite variable to capture whether participants had ever used: hookah or water pipe; traditional cigar, cigarillo or little cigar; dissolvable tobacco; or electronic cigarettes. The survey instrument is available online: www.unc.edu/~ntbrewer.
Data Analysis
We first calculated descriptive statistics, including the percentage of the sample that had ever heard of each constituent and the mean score for worry and discouragement from smoking for each constituent. We then used McNemar’s test to determine whether the proportion of people who believe that each constituent is added to cigarettes differed from the proportion of people who believe that the constituent naturally occurs in tobacco smoke. Next, we identified correlates of discouragement from wanting to smoke for each constituent. Finally, we conducted bivariate linear regressions to examine predictors of discouragement from wanting to smoke across all constituents. We then entered variables with p values <.10 into a single multivariate model. Analyses used SPSS Statistics version 19.0 with two-tailed tests and a critical α of .05.
RESULTS
About half of participants were female (54%) and most were aged 30 or older (61%). Our sample was mostly non-Hispanic (95%) and White (83%). Most participants had at least some college education (85%) and had an annual household income of at least $30,000 per year (69%). About of half of participants (51%) lived in a suburban area; the remainder of the sample lived either in a rural area (25%) or an urban area (24%). Almost a third of participants were current smokers (30%), 25% were former smokers, and the remaining 44% were nonsmokers. About two thirds of the sample (66%) had ever used a tobacco product besides cigarettes.
Awareness
Most participants reported that they had heard of ammonia (99%), arsenic (97%), benzene (75%), cadmium (66%), carbon monoxide (100%), formaldehyde (94%), and nicotine (100%) (Table 1). Fewer than 30% were aware of four constituents, and awareness was in the single digits for the remaining nine constituents. Participants tended to report higher levels of worry and discouragement from smoking when asked about constituents they recognized. For example, the highest levels of worry and discouragement from smoking were associated with constituents that at least 90% of participants had heard of (ammonia, arsenic, carbon monoxide, and formaldehyde).
Table 1.
Tobacco Constituent Awareness, Attitudes, and Beliefs
| Awareness | Worry | Discourages wanting to smoke | Spontaneously mentioned | Recognized in list | |||||
|---|---|---|---|---|---|---|---|---|---|
| Added | Naturally occurring | Added | Naturally occurring | ||||||
| (%) | (mean) | (mean) | (%) | (%) | p value | (%) | (%) | p value | |
| 1,3-Butadiene | 9 | 3.48 | 3.49 | – | – | 75 | 13 | <.001 | |
| 1-Aminonaphthalene | 7 | 3.46 | 3.50 | – | – | 76 | 13 | <.001 | |
| 2-Aminonaphthalene | 6 | 3.45 | 3.46 | – | – | 74 | 15 | <.001 | |
| 4-Aminobiphenyl | 6 | 3.49 | 3.47 | – | – | 76 | 12 | <.001 | |
| Acetaldehyde | 23 | 3.66 | 3.60 | – | – | 78 | 12 | <.001 | |
| Acrolein | 6 | 3.38 | 3.38 | – | – | 73 | 15 | <.001 | |
| Acrylonitrile | 8 | 3.49 | 3.50 | – | – | 76 | 13 | <.001 | |
| Ammonia | 99 | 4.39 | 4.34 | 12 | 8 | .20 | 74 | 23 | <.001 |
| Arsenic | 97 | 4.65 | 4.61 | 12 | 6 | .01 | 72 | 25 | <.001 |
| Benzene | 75 | 3.86 | 3.86 | 5 | 2 | .03 | 74 | 21 | <.001 |
| Benzo[a]pyrene | 25 | 3.57 | 3.58 | – | – | 75 | 15 | <.001 | |
| Cadmium | 66 | 3.62 | 3.59 | – | – | 62 | 30 | <.001 | |
| Carbon monoxide | 100 | 4.16 | 4.13 | – | – | 23 | 73 | <.001 | |
| Crotonaldehyde | 4 | 3.52 | 3.54 | – | – | 77 | 11 | <.001 | |
| Formaldehyde | 94 | 4.45 | 4.38 | 16 | 3 | <.001 | 82 | 12 | <.001 |
| Isoprene | 21 | 3.37 | 3.40 | – | – | 69 | 19 | <.001 | |
| Nicotine | 100 | 3.44 | 3.46 | 35 | 52 | <.001 | 32 | 76 | <.001 |
| NNK | 6 | 3.57 | 3.58 | – | – | 66 | 24 | <.001 | |
| NNN | 4 | 3.49 | 3.50 | – | – | 66 | 27 | <.001 | |
| Toluene | 29 | 3.55 | 3.57 | – | – | 72 | 17 | <.001 | |
Note. NNK = nicotine-derived nitrosamine ketone; NNN = N-nitrosonornicotine. Elements in bold indicate constituents that elicit the highest discouragement; (–) indicates that <2% of respondents spontaneously mentioned the constituent. N = 300.
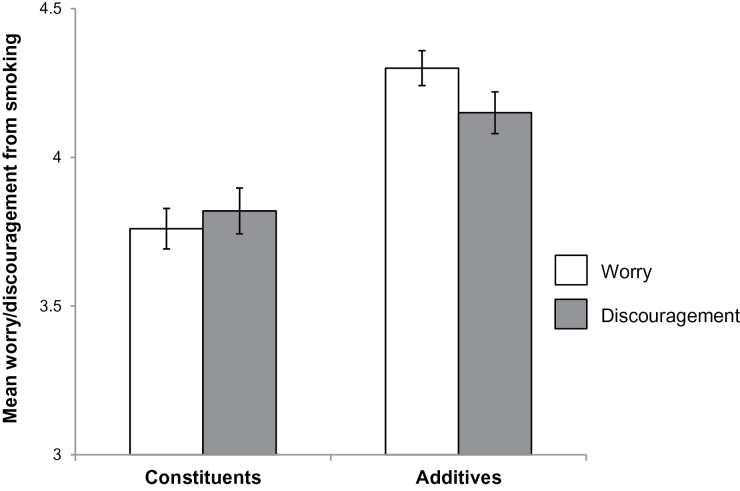
Constituents Versus Additives
Chemicals that companies add to cigarette tobacco (i.e., additives) made participants more worried about the harms of smoking than chemicals that naturally occur in cigarette smoke (p < .001; Figure 1). Similarly, cigarette tobacco additives caused more discouragement from wanting to smoke than chemicals that naturally occur in cigarette smoke (p < .001).
Figure 1.
Worry and discouragement from wanting to smoke elicited by tobacco additives and tobacco smoke constituents.
When asked to spontaneously recall constituents found in cigarettes, participants commonly mentioned nicotine, and they occasionally mentioned ammonia, arsenic, benzene, and formaldehyde. Less than 2% of the sample mentioned any of the remaining 15 constituents (Table 1). Of the five constituents that at least 2% of respondents spontaneously mentioned, it was more common for participants to erroneously believe that arsenic, benzene, and formaldehyde were added to cigarette tobacco than that they were naturally occurring in cigarette smoke (p < .05 for all three constituents). However, participants were more likely to report that nicotine was naturally occurring than to report that it was added to cigarettes (p < .001).
When asked about the 20 constituents by name, few respondents believed that constituents naturally occurred in cigarette smoke (Table 1), and most believed they were added to cigarette tobacco. More respondents believed 18 of the constituents were added to cigarette tobacco than believed they were naturally occurring in cigarette smoke (each p < .001; Table 1). The opposite was true for carbon monoxide and nicotine: more participants believed that these two constituents were naturally occurring in cigarette smoke than that they were added to cigarette tobacco (p < .001).
Discouragement From Wanting to Smoke
The mean discouragement across all constituents was 3.70 (SD = 0.98). This corresponds to being between “somewhat” (=3) and “quite a bit” (=4) discouraged from wanting to smoke. The constituents that elicited the highest mean discouragement were ammonia (4.34, SD = 1.00), arsenic (4.61, SD = 0.81), carbon monoxide (4.13, SD = 1.23), and formaldehyde (4.38, SD = 1.02; Table 1, elements in bold). Smokers and nonsmokers rated these same four constituents as causing the most discouragement from smoking (data not shown; please refer to Supplementary Table 1). Nicotine elicited the lowest mean discouragement among smokers (2.42, SD = 1.38).
Bivariate analyses used discouragement elicited by each constituent as the outcome. For example, the first cell of Table 2 indicates that the correlation between belief that tobacco companies add butadiene to tobacco and discouragement from wanting to smoke elicited by butadiene is .15. The strongest bivariate correlate of discouragement was worry (mean r = .89; Table 2). For all but two constituents, negative smoker prototype was a stronger correlate (mean r = .30) than positive smoker prototype (mean r = −.18). We grouped former smokers with nonsmokers because they reported similar levels of constituents discouraging them from smoking (p = .98). Smokers had lower discouragement for all constituents than nonsmokers (mean r = −.36). Smoking status was not correlated with awareness for any of the constituents, and smoking was weakly correlated with belief that companies add constituents to tobacco for only 4 of the 20 constituents (data not shown; please refer to Supplementary Table 2).
Table 2.
Correlates of Discouragement From Wanting to Smoke, by Tobacco Constituent
| Belief that tobacco companies add constituents to tobacco (r) | Awareness (r) | Prototype of smoker as good (r) | Prototype of smoker as bad (r) | Smoking status (r) | Worry (r) | |
|---|---|---|---|---|---|---|
| 1,3-Butadiene | .15* | .23* | −.19* | .31* | −.38* | .90* |
| 1-Aminonaphthalene | .12* | .14* | −.17* | .28* | −.39* | .90* |
| 2-Aminonaphthalene | .05 | .18* | −.13* | .34* | −.33* | .88* |
| 4-Aminobiphenyl | .13* | .13* | −.14* | .28* | −.30* | .92* |
| Acetaldehyde | .09 | .22* | −.22* | .33* | −.35* | .87* |
| Acrolein | .14* | .22* | −.12* | .25* | −.28* | .89* |
| Acrylonitrile | .05 | .20* | −.16* | .33* | −.36* | .87* |
| Ammonia | .04 | .04 | −.22* | .30* | −.34* | .88* |
| Arsenic | −.05 | .28* | −.20* | .26* | −.34* | .83* |
| Benzene | .09 | .23* | −.24* | .37* | −.41* | .89* |
| Benzo[a]pyrene | .11 | .29* | −.13* | .28* | −.29* | .89* |
| Cadmium | .15* | .13* | −.16* | .25* | −.36* | .93* |
| Carbon monoxide | .20* | .05 | −.27* | .25* | −.40* | .88* |
| Crotonaldehyde | .03 | .07 | −.17* | .30* | −.38* | .88* |
| Formaldehyde | .03 | .22* | −.28* | .26* | −.33* | .85* |
| Isoprene | .11 | .21* | −.14* | .26* | −.36* | .90* |
| Nicotine | .18* | .02 | −.17* | .32* | −.47* | .90* |
| NNK | .16* | .06 | −.13* | .30* | −.34* | .91* |
| NNN | .20* | .15* | −.09 | .30* | −.39* | .90* |
| Toluene | .11 | .29* | −.17* | .31* | −.36* | .89* |
| Mean r | .10 | .17 | −.18 | .30 | −.36 | .89 |
Note. NNK = nicotine-derived nitrosamine ketone; NNN = N-nitrosonornicotine. Elements in bold indicate constituents that elicit the highest discouragement. Correlation coefficients (rs) characterize the bivariate relationship between the variables in each column and discouragement from wanting to smoke elicited by the constituent in each row. N = 300.
*p < .05.
The final multivariate analysis used average discouragement across the constituents as the outcome (Table 3). Mean discouragement from wanting to smoke was most strongly associated with being a nonsmoker (β = −.34). The mean discouragement among smokers was 3.04 (SD = 0.93), compared with 3.98 (SD = 0.86) among nonsmokers. Mean discouragement was also associated with greater belief that constituents are added to tobacco (β = .14), having negative smoker prototypes (β = .19), and older age (β = .16). To better understand the association with age, we examined mean discouragement by age categories: age 18–24, mean = 3.54 (SD = 0.84); age 25–39, mean = 3.61 (SD = 0.99); age 40–55, mean = 3.93 (SD = 0.94); and age 55 and older, mean = 3.95 (SD = 1.16). Belief that constituents are added to tobacco was not statistically significant in bivariate regression (p = .09); this variable became statistically significant when we included smoking status in the model (p < .01). The multivariate model did not include worry as it was so highly correlated with discouragement.
Table 3.
Correlates of Discouragement From Wanting to Smoke, Across Tobacco Constituents
| Discouragement | Bivariate | Multivariate | |
|---|---|---|---|
| Mean (SD) | β | β | |
| Belief that constituents are added to tobacco | .10 | .14* | |
| Awareness | .17* | .10 | |
| Prototype of smoker as good | −.21* | −.09 | |
| Prototype of smoker as bad | .36* | .19* | |
| Smoking status | −.44* | −.34* | |
| Current smoker | 3.04 (0.93) | ||
| Nonsmoker | 3.98 (0.86) | ||
| Ever used other tobacco products | −.18* | .03 | |
| Yes | 3.57 (0.98) | ||
| No | 3.94 (0.95) | ||
| Age | .15* | .16* | |
| Sex | .12* | .04 | |
| Male | 3.57 (0.95) | ||
| Female | 3.82 (1.00) | ||
| Sexual orientation | .02 | ||
| Heterosexual | 3.69 (0.99) | ||
| Nonheterosexual | 3.78 (0.83) | ||
| Ethnicity | .00 | ||
| Hispanic | 3.68 (0.74) | ||
| Non-Hispanic | 3.70 (1.00) | ||
| Race | .10 | .08 | |
| White | 3.65 (0.98) | ||
| Non-White | 3.92 (0.97) | ||
| Education | .13* | −.00 | |
| Household income, annual | .15* | .04 | |
| Urbanicity | .03 | ||
| Rural | 3.65 (1.06) | ||
| Urban or suburban | 3.72 (0.96) | ||
| Health literacy | −.11 | −.09 |
Note. Multivariate analysis provided standardized regression coefficients (βs). The regression model included variables with p values <.10 in bivariate analyses. Analyses treated age, education, and income as continuous variables.
*p < .05.
DISCUSSION
Tobacco is likely the most important source of toxic chemical exposure and chemically caused disease (Rodgman & Perfetti, 2008; Talhout et al., 2011). Yet few participants in our study had heard of many of the 20 constituents that the FDA has prioritized for tobacco manufacturers to report to FDA and the public. Nearly all respondents (more than 95%) had heard of nicotine, carbon monoxide, ammonia, and arsenic, and most had heard of benzene, cadmium, and formaldehyde. Studies of smokers and nonsmokers in the United States, Canada, Australia, and the United Kingdom (Borland & Hill, 1997; Environics Research Group, 2008; Hammond, Fong, McNeill, Borland, & Cummings, 2006; Siahpush, McNeill, Hammond, & Fong, 2006; Stockwell, Rutley, & Clark, 1992) have also found that the public has very high awareness of nicotine and carbon monoxide (Hammond et al., 2006; Siahpush et al., 2006; Stockwell et al., 1992), but they are less familiar with arsenic, ammonia, benzene, and formaldehyde (Environics Research Group, 2008). These studies did not ask participants about the other 13 constituents on the FDA’s high priority list, like acetaldehyde, acrolein, or NNK, which few participants in our study had heard of. These previous studies also did not examine how information about tobacco constituents might convey health risks or discourage people from smoking, another novel aspect of our research findings.
One important question is how people perceive constituents they have never heard of compared to constituents with which they are familiar. Our study found that chemicals that most people had heard of tended to cause stronger feelings of worry and discouragement. This finding stands in contrast to research on health warnings that has shown that introducing some novel concepts can be more effective than reinforcing existing knowledge (Borland, 1997; Hammond et al., 2007). This is in part because the impact of tobacco warnings tends to diminish over time (Hammond, 2009). However, to our knowledge, the impact of messages about familiar compared to unfamiliar constituents has not been studied, and merits further research. If future studies corroborate our findings, health communication campaigns to discourage smoking could consider emphasizing widely recognized constituents (e.g., ammonia, carbon monoxide) in their materials and messages, instead of chemicals that most people have not heard of (e.g., NNK, acrolein), at least until the public becomes more aware of them. An alternative is to conduct communication campaigns to raise public awareness of some of these dangerous chemicals to develop their suitability for discouraging smoking.
Few people in our study correctly understood that constituents are naturally present in tobacco, and many instead believed they are added by tobacco companies. Furthermore, substances people perceived as added to cigarettes by tobacco companies elicited more discouragement from wanting to smoke than substances they perceived as naturally occurring in tobacco. Additives also made participants more worried about the harms of smoking than chemicals that naturally occur in cigarette smoke. The tobacco industry has consistently marketed certain brands of cigarettes as “natural” and “additive-free,” which can create the false perception that additive-free cigarettes are safer than regular cigarettes (Wilkenfeld, Henningfield, Slade, Burns, & Pinney, 2000). A national survey of U.S. adult smokers found that 73% incorrectly believed that cigarettes with additives are more harmful than cigarettes that do not have additives (Cummings et al., 2004). Communications campaigns that focus on constituents may face multiple challenges, as people may misunderstand tobacco constituents to be less harmful than additives and find constituents less motivating than additives. Thus, health communication efforts might be more effective if they emphasize that all cigarettes—even so-called “natural” and “additive-free” cigarettes—are irrevocably dangerous because they contain harmful components.
In adjusted analyses, nonsmokers were more likely than smokers to report that constituents discouraged them from smoking. This finding is consistent with research indicating differences in attitudes and beliefs according to smoking status (Poland et al., 2000). Smokers are more resistant than nonsmokers to information on the health risks of smoking and, as a result, more extensively underestimate their health risks (Cameron, Pepper, & Brewer, in press; Harris, Cohen, Wyrwich, & Luke, 2011; Strecher, Kreuter, & Kobrin, 1995). One reason is that some smokers may spend less time looking at risk information than nonsmokers (Loeber et al., 2011). Consequently, efforts to communicate information about constituents should design messages carefully with the understanding that smokers are likely to be less attentive to the warnings. These findings support the use of vivid cigarette pack warnings to increase the chance of drawing the attention of smokers to the key messages.
In our study, respondents with more negative images of smokers (i.e., prototypes) were more likely to report that constituents discouraged them from smoking. Research has found that individuals’ perceptions of a “typical smoker” are strong predictors of attitudes and behavior (Gibbons & Eggleston, 1996; Gibbons & Gerrard, 1995; Pepper et al., 2013). One cessation study found that smokers were more likely to relapse if they had positive perceptions of the typical smoker (Gibbons & Eggleston, 1996). Another recent study found that adolescent nonsmokers with negative images of smokers were significantly less willing to try e-cigarettes than those with positive images of smokers (Pepper et al., 2013). Thus, images of smokers may be an important predictor of smoking-related attitudes and behavior. In the context of this study, our data suggest that adults with negative images of smokers might be more receptive to constituent-related health information than those who have positive images of smokers.
Study strengths include gathering highly novel data on beliefs about tobacco constituents and our national sample that included both smokers and nonsmokers. Study limitations include the cross-sectional study design, which limits our ability to infer causal relations among variables. The nonprobability sampling approach and low inclusion of minority respondents may limit the generalizability of our findings. As communication about and discussion of tobacco constituents grows, the patterns of relationships we found among variables may also evolve.
This early look at how Americans think about constituents should be replicated with a larger and more diverse population to better understand how subgroups that experience smoking-related health disparities (e.g., by race, income, sexual orientation) respond to information about constituents. Youth and adolescents are of particular interest as this group is at highest risk of smoking initiation (Centers for Disease Control and Prevention, 2012b; The Substance Abuse and Mental Health Services Administration, 2011). Future studies should examine the effectiveness of different methods of conveying constituent information to consumers (e.g., numerical vs. descriptive information) (Gallopel-Morvan et al., 2011; Hammond, 2009), as well as the extent to which FDA’s constituent-related dissemination efforts are understandable to the public. Previously, consumers have misconstrued information about tar and nicotine levels, perceiving certain products as less harmful than others (Cohen, 1996; Pollay & Dewhirst, 2001). Likewise, as constituent levels differ by cigarette product and brand (Wu, Zhang, Jain, Ashley, & Watson, 2005), FDA must anticipate possible unintended consequences of releasing new constituent information. Therefore, future studies should investigate the potential unintended consequences of publicizing information about constituents. Our results can inform efforts by FDA and others organizations as they develop health communications campaigns, for example as FDA develops new cigarette pack warnings. Future research should develop and evaluate warning messages that convey information about tobacco constituents.
SUPPLEMENTARY MATERIAL
Supplementary Tables 1 and 2 can be found online at http://www.ntr.oxfordjournals.org
FUNDING
This work was supported by Comprehensive Cancer Control Collaborative of North Carolina (4CNC): Moving Evidence into Action, a collaborating site in the Cancer Prevention and Control Research Network (U48/DP001944), funded by the Centers for Disease Control and Prevention and the National Cancer Institute.
DECLARATION OF INTERESTS
None declared.
Supplementary Material
ACKNOWLEDGMENT
We would like to acknowledge the Comprehensive Cancer Control Collaborative of North Carolina (4CNC) for supporting this work.
REFERENCES
- Berinsky A. J., Huber G. A., Lenz G. S. (2012). Evaluating online labor markets for experimental research: Amazon.com’s Mechanical Turk. Political Analysis, 20, 351–368. 10.1093/pan/mpr057 [Google Scholar]
- Biener L., Nyman A. L., Stepanov I., Hatsukami D. (2013). Public education about the relative harm of tobacco products: An intervention for tobacco control professionals. Tobacco Control. [Epub ahead of print] 10.1136/tobaccocontrol-2012–050814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R. (1997). Tobacco health warnings and smoking-related cognitions and behaviours. Addiction (Abingdon, England), 92, 1427–1435. 10.1111/j.1360-0443.1997.tb02864.x [PubMed] [Google Scholar]
- Borland R., Hill D. (1997). Initial impact of the new Australian tobacco health warnings on knowledge and beliefs. Tobacco Control, 6, 317–325. 10.1136/tc.6.4.317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M., Kwang T., Gosling S. D. (2011). Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6, 3–5. 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Cameron L. D., Pepper J. K., Brewer N. T. (2013). Responses of young adults to graphic warning labels for cigarette packages. Tobacco Control. [Epub ahead of print]. 10.1136/tobaccocontrol-2012-050645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2012a). Current cigarette smoking among adults - United States, 2011. MMWR. Morbidity and Mortality Weekly Report, 61, 889–894. 10.1001/jama.2012.114523 [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2012b). Youth and tobacco use. Retrieved April 1, 2013, from http://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/
- Cohen J. B. (1996). Smokers’ knowledge and understanding of advertised tar numbers: Health policy implications. American Journal of Public Health, 86, 18–24. 10.2105/AJPH.86.1.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings K. M., Hyland A., Giovino G. A., Hastrup J. L., Bauer J. E., Bansal M. A. (2004). Are smokers adequately informed about the health risks of smoking and medicinal nicotine? Nicotine & Tobacco Research, 6(Suppl. 3), S333–S340. 10.1080/14622200412331320734 [DOI] [PubMed] [Google Scholar]
- Environics Research Group (2008). Wave 13 Surveys: The Health Effects of Tobacco and Health Warning Messages on Cigarette Packages. Survey of Adults and Adult Smokers. Toronto, Canada: Health Canada [Google Scholar]
- Fowles J., Dybing E. (2003). Application of toxicological risk assessment principles to the chemical constituents of cigarette smoke. Tobacco Control, 12, 424–430. 10.1136/tc.12.4.424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallopel-Morvan K., Moodie C., Hammond D., Eker F., Beguinot E., Martinet Y. (2011). Consumer understanding of cigarette emission labelling. European Journal of Public Health, 21, 373–375. 10.1093/eurpub/ckq087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons F. X., Eggleston T. J. (1996). Smoker networks and the “typical smoker”: A prospective analysis of smoking cessation. Health Psychology, 15, 469–477. 10.1037/0278-6133.15.6.469 [DOI] [PubMed] [Google Scholar]
- Gibbons F. X., Gerrard M. (1995). Predicting young adults’ health risk behavior. Journal of Personality and Social Psychology, 69, 505–517. 10.1037/0022-3514.69.3.505 [DOI] [PubMed] [Google Scholar]
- Gibbons F. X., Helweg-Larsen M., Gerrard M. (1995). Prevalence estimates and adolescent risk behavior: Cross-cultural differences in social influence. The Journal of Applied Psychology, 80, 107–121. 10.1037/0021-9010.80.1.107 [DOI] [PubMed] [Google Scholar]
- Hammond D.(2009). Tobacco labelling and packaging toolkit. Retrieved December 10, 2012, from http://www.tobaccolabels.ca/toolkit .
- Hammond D. (2011). Health warning messages on tobacco products: A review. Tobacco Control, 20, 327–337. 10.1136/tc.2010.037630 [DOI] [PubMed] [Google Scholar]
- Hammond D., Fong G. T., Borland R., Cummings K. M., McNeill A., Driezen P. (2007). Communicating risk to smokers: The impact of health warnings on cigarette packages. American Journal of Preventive Medicine, 32, 202. 10.1016/j.amepre.2006.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D., Fong G. T., McNeill A., Borland R., Cummings K. M. (2006). Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: Findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control, 15(Suppl. 3), iii19–25. 10.1136/tc.2005.012294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris J. K., Cohen E. L., Wyrwich K. W., Luke D. A. (2011). Differences in smokers and nonsmokers’ assessments of an educational campaign about tobacco use. Health Education and Behavior, 38, 574–583. 10.1177/1090198110385894 [DOI] [PubMed] [Google Scholar]
- Hecht S. S. (2012). Research opportunities related to establishing standards for tobacco products under the Family Smoking Prevention and Tobacco Control Act. Nicotine & Tobacco Research, 14, 18–28. 10.1093/ntr/ntq216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (2004). Tobacco Smoke and Involuntary Smoking. Lyon, France: IARC Press [Google Scholar]
- Lee J. G., Griffin G. K., Melvin C. L. (2009). Tobacco use among sexual minorities in the USA, 1987 to May 2007: A systematic review. Tobacco Control, 18, 275–282. 10.1136/tc.2008.028241 [DOI] [PubMed] [Google Scholar]
- Loeber S., Vollstädt-Klein S., Wilden S., Schneider S., Rockenbach C., Dinter C., Kiefer F. (2011). The effect of pictorial warnings on cigarette packages on attentional bias of smokers. Pharmacology, Biochemistry, and Behavior, 98, 292–298. 10.1016/j.pbb.2011.01.010 [DOI] [PubMed] [Google Scholar]
- McCool J. P., Cameron L., Petrie K. (2004). Stereotyping the smoker: Adolescents’ appraisals of smokers in film. Tobacco Control, 13, 308–314. 10.1136/tc.2003.006791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCool J., Cameron L. D., Robinson E. (2011). Do parents have any influence over how young people appraise tobacco images in the media? The Journal of Adolescent Health, 48, 170–175. 10.1016/j.jadohealth.2010.06.012 [DOI] [PubMed] [Google Scholar]
- Mokdad A. H., Marks J. S., Stroup D. F., Gerberding J. L. (2004). Actual causes of death in the United States, 2000. JAMA: The Journal of the American Medical Association, 291, 1238–1245. 10.1001/jama.291.10.1238 [DOI] [PubMed] [Google Scholar]
- Paolacci G., Chandler J., Ipeirotis P. (2010). Running experiments on Amazon Mechanical Turk. Judgment and Decision Making, 5, 411–419 [Google Scholar]
- Pepper J. K., Reiter P. L., McRee A. L., Cameron L. D., Gilkey M. B., Brewer N. T. (2013). Adolescent males’ awareness of and willingness to try electronic cigarettes. The Journal of Adolescent Health, 52, 144–150. 10.1016/j.jadohealth.2012.09.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poland B. D., Cohen J. E., Ashley M. J., Adlaf E., Ferrence R., Pederson L. L., Raphael D. (2000). Heterogeneity among smokers and non-smokers in attitudes and behaviour regarding smoking and smoking restrictions. Tobacco Control, 9, 364–371. 10.1136/tc.9.4.364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollay R. W., Dewhirst T. (2001). Marketing Cigarettes with Low Machine-Measured Yields (pp. 199–235). Bethesda, MD: U.S. Department of Health and Human Services [Google Scholar]
- Rand D. G. (2012). The promise of Mechanical Turk: How online labor markets can help theorists run behavioral experiments. Journal of Theoretical Biology, 299, 172–179. 10.1016/j.jtbi.2011.03.004 [DOI] [PubMed] [Google Scholar]
- Rodgman A., Perfetti T. A. (2008). The Chemical Components of Tobacco and Tobacco Smoke. Boca Raton, FL: CRC Press [Google Scholar]
- Siahpush M., McNeill A., Hammond D., Fong G. T. (2006). Socioeconomic and country variations in knowledge of health risks of tobacco smoking and toxic constituents of smoke: Results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tobacco Control, 15(Suppl. 3), iii65–70. 10.1136/tc.2005.013276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockwell T. R., Rutley R., Clark K. (1992). Pesticides and other chemicals in cigarette tobacco. The Medical Journal of Australia, 157, 68. [DOI] [PubMed] [Google Scholar]
- Strecher V. J., Kreuter M. W., Kobrin S. C. (1995). Do cigarette smokers have unrealistic perceptions of their heart attack, cancer, and stroke risks? Journal of Behavioral Medicine, 18, 45–54. 10.1007/BF01857704 [DOI] [PubMed] [Google Scholar]
- Talhout R., Schulz T., Florek E., van Benthem J., Wester P., Opperhuizen A. (2011). Hazardous compounds in tobacco smoke. International Journal of Environmental Research And Public Health, 8, 613–628. 10.3390/ijerph8020613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Substance Abuse and Mental Health Services Administration (2011). Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings (HHS Publication No. (SMA) 11-4658). Rockville, MD: Substance Abuse and Mental Health Services Administration [Google Scholar]
- U.S. Food and Drug Administration (2011). Guidance for Industry and FDA Staff: “Harmful and Potentially Harmful Constituents” in Tobacco Products as Used in Section 904(e) of the Federal Food, Drug, and Cosmetic Act. Rockville, MD: U.S. Department of Health and Human Services, Food and Drug Administration, Center for Tobacco Products [Google Scholar]
- U.S. Food and Drug Administration (2012a). Harmful and potentially harmful constituents in tobacco products and tobacco smoke; established list. Federal Register, 77, 20034–20037 [Google Scholar]
- U.S. Food and Drug Administration (2012b). Reporting Harmful and Potentially Harmful Constituents in Tobacco Products and Tobacco Smoke Under Section 904(a)(3) of the Federal Food, Drug, and Cosmetic Act. Rockville, MD: U.S. Department of Health and Human Services, Food and Drug Administration, Center for Tobacco Products [Google Scholar]
- United States Public Laws (2009). Family Smoking Prevention and Tobacco Control Act (Public Law 111–31 [H.R. 1256]). [Google Scholar]
- Wayne G. F., Carpenter C. M. (2009). Tobacco industry manipulation of nicotine dosing. Handbook of Experimental Pharmacology (Vol. 192, pp. 457–485). 10.1007/978-3-540-69248-5_16 [DOI] [PubMed] [Google Scholar]
- Weiss B. D., Mays M. Z., Martz W., Castro K. M., DeWalt D. A., Pignone M. P., Hale F.A. (2005). Quick assessment of literacy in primary care: The newest vital sign. Annals of Family Medicine, 3, 514–522. 10.1370/afm.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkenfeld J., Henningfield J., Slade J., Burns D., Pinney J. (2000). It’s time for a change: Cigarette smokers deserve meaningful information about their cigarettes. Journal of the National Cancer Institute, 92, 90–92. 10.1093/jnci/92.2.90 [DOI] [PubMed] [Google Scholar]
- Wu W., Zhang L., Jain R. B., Ashley D. L., Watson C. H. (2005). Determination of carcinogenic tobacco-specific nitrosamines in mainstream smoke from U.S.-brand and non-U.S.-brand cigarettes from 14 countries. Nicotine & Tobacco Research, 7, 443–451. 10.1080/14622200500125898 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.