Abstract
Although atelectasis is common in children, its persistence or refractoriness to treatment should lead prompt evaluation to identify causal mechanism. We describe the case of a child presenting in first year of life with persistent left upper lobe atelectasis, recurrent wheezing and respiratory infections refractory to medical therapy, submitted to partial lobectomy when he was 3 years old age. Histopathological examination revealed follicular bronchiolitis. Systemic underlying diseases were excluded. Clinical improvement was initially achieved using inhaled corticosteroids, but oral therapy was needed due to clinical relapse, with favorable response.
Follicular bronchiolitis, a rare pulmonary primary lymphoid lesion, consists of numerous reactive lymphoid follicles in a peribonchiolar distribution. Its precise cause is unknown, particularly in children, in which few cases have been reported. Treatment usually includes steroids and prognosis is generally good.
Keywords: Follicular bronchiolitis, Lymphoproliferative disorder, Histopathology, Atelectasis
1. Introduction
Atelectasis consists in collapse of alveolar spaces. It is a common feature in pediatric patients, to which they are particularly prone because of their chest wall compliance and lack of collateral ventilation observed in adults [1]. Its persistence or refractoriness to treatment should lead to prompt evaluation to identify causal mechanism, ensuring an adequate approach.
Although most frequent type of atelectasis described in children is obstructive, mainly as consequence of mucus plugging [1], it is rarely reported as consequence of bronchial obstruction due to hyperplasia of bronchus-associated lymphoid tissue. We report a unique case of a boy presenting with persistent atelectasis, recurrent wheezing and severe respiratory infections, which had follicular bronchiolitis (FB) diagnosis.
2. Case report
A 21-month boy was referred to our consultation because of persistent left upper lobe (LUL) atelectasis. He had a previous history of recurrent wheezing since the first trimester of life, conditioning three previous admissions at local hospital due to dyspnea and respiratory distress (at 2, 8 and 9 months). In latter episode adenovirus and parainfluenza 3 were identified in viral antigen detection on nasopharyngeal swab, and chest X-ray revealed a LUL atelectasis.
Despite clinical improvement verified during acute episodes described above, chronic cough, maintenance of tachypnea and respiratory effort in intercritical period justified chest X-ray reevaluation, which demonstrated persistence of atelectasis previously found, motivating referral to a tertiary care hospital.
In our first observation he was tachypneic, with mild respiratory effort and non-hypoxemic. Pulmonary auscultation revealed reduced respiratory sounds on upper third of left lung with fine crackles on same location.
Additional studies performed included high resolution thoracic computed tomography (CT), which evidenced diffuse ground-glass opacity, LUL atelectasis and mild bronchial dilation. Bronchoscopy revealed airways with normal morphology and purulent bronchorrhea, with no residual obstruction after aspiration.
Blood cell count, allergologic panel and sweat chloride test were normal. Genetic study for cystic fibrosis and protein-chain reaction assay for Mycobacterium tuberculosis in gastric aspirate were negative. Serum analysis of immunoglobulins and evaluation of blood lymphocyte subsets were normal.
During initial follow-up period, he maintained recurrent LUL infection, often requiring hospital admission and need for frequent courses of antibiotic therapy. Cough and recurrent exacerbations persisted. No improvement was achieved with daily physiotherapy, impairing his quality of life.
The case was discussed with cardiothoracic surgery department and considering failure of medical therapy, recurrent respiratory infections, persistent sputum production and chronic cough he was submitted to a LUL lobectomy, when he was three years old. Histopathological examination revealed numerous reactive lymphoid follicles in a peribronchial/peribronchiolar distribution, diagnosing follicular bronchiolitis (Fig. 1).
Fig. 1.
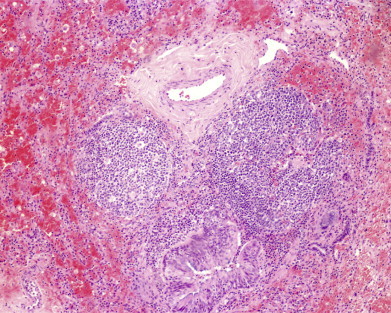
HE (40×). Reactive lymphoid follicles containing germinal centers located between bronchioles and pulmonary arteries.
Underlying diseases were excluded, such as vascular collagen disease as well as primary or secondary immunodeficiency.
In the first six years after surgery pulmonary function tests remained stable, he had few exacerbations marked by bronchospasm controlled with inhaled short acting β2-agonist (salbutamol) and inhaled corticosteroid (fluticasone).
When he was 10 years old he referred mild exertional dyspnea and recurrence of cough. Spirometry showed a mixed pattern with a Forced Vital Capacity (FVC) of 78%, a Forced Expiratory Volume in one second (FEV1) of 65% and a reduced ratio of FEV1/FVC of 74%. A course of oral prednisolone (40 mg/day) was initiated, with gradual clinical and lung function improvement, allowing oral steroid dose tapering six months after.
Actually, at 11 years old, he is kept asymptomatic on daily inhaled corticosteroid.
3. Discussion
FB is a rare disorder and represents hyperplasia of mucosa-associated lymphoid tissue along airways (bronchus associated lymphoid tissue – BALT). It occurs mostly in middle aged adults [2] and rarely reported in children [2,3].
It is defined by its histological pattern that consists of numerous reactive lymphoid follicles in a peribronchiolar distribution, which can cause airway lumen compression and obstruction because they frequently lie between bronchioles and pulmonary arteries [4,5].
It can be secondary, occurring in patients with underlying collagen vascular disease, in cases of congenital or acquired immunodeficiency or in a heterogeneous group characterized by peripheral eosinophilia [4]. Less frequently it can be idiopathic [6], as in our case.
Although the precise cause is still unknown, it was suggested that it may represent a polyclonal hyperplasia of bronchus associated lymphoid tissue in response to an antigenic stimuli (intrinsic or extrinsic) [4,7]. In our case, previous respiratory infection with adenovirus and parainfluenza 3 might have contributed to development of FB.
Most patients present with cough, dyspnea or recurrent pneumonia, weight loss and fatigue [4]. In children, failure to thrive, recurrent hemoptysis and tachypnea are also possible features [3]. Multiple pulmonary function studies abnormalities have been reported, including obstructive, restrictive and mixed patterns [4,7,8]. Chest X-ray findings usually include bilateral small nodular or reticulonodular infiltrates with intrathoracic adenopathy. TC evidences centrilobular and peribronchial nodules and ground-glass opacity, normally bilateral and diffuse [7,9,10]. Some cases have mild bronchial dilation [7], as in our case.
Despite presence of suggestive clinical, laboratory and radiological findings, definitive diagnosis requires open lung biopsy [6]. Bronchoscopic biopsy is not diagnostic because of the patchy nature of disease, leading to sample error and the amount of tissue obtained by this technique, which is often insufficient [9].
Treatment, although not fully understood, is usually directed to the underlying cause, when recognized. Idiopathic cases generally are treated with bronchodilators and steroids [7]. Macrolide therapy was recently suggested as an alternative approach in some patients and considered in those who remain corticosteroid-dependent [9]. Immunosuppressive agents are generally reserved for refractory cases. As there are few cases reported, experience in treatment options in children is scarce, so we believe our report may be important in establishing a therapeutic plan in cases similar to ours.
Prognosis in unclear, but generally described as favorable, although progressive disease is recognized when it presents in young ages [5,7,9].
Contributor's statement
Ângela Dias – conception and design of the manuscript, drafting of the article.
Joana Jardim – conception of the manuscript, data collection.
Teresa Nunes – manuscript revision.
Conceição Souto Moura – manuscript revision.
Luísa Vaz – manuscript revision and final approval of version to be published.
Disclosure statement
The authors report no biomedical financial interests or other potential conflicts of interest in this manuscript. There were no sponsors in this study.
References
- 1.Finder J. In: Atelectasis in children. UpToDate, Basow D.S., editors. UpToDate; Waltham, MA: 2013. [Google Scholar]
- 2.Nicholson A.G. Pulmonary lymphoproliferative disorders. Curr Diagn Pathol. 2000;6:130–139. [Google Scholar]
- 3.Dai Y.W., Lin L., Tang H.F., Jiang K.W. Follicular bronchiolitis in a child. World J Pediatr. 2011;7(2):176–178. doi: 10.1007/s12519-011-0277-5. [DOI] [PubMed] [Google Scholar]
- 4.Guinee G.D., Jr. Update on pulmonary and pleural lymphoproliferative disorders. Diagn Histopathology. 2008;14(10):474–498. [Google Scholar]
- 5.Travis W.D., Galvin J.R. Non-neoplastic pulmonary lymphoid lesions. Thorax. 2001;56:964–971. doi: 10.1136/thorax.56.12.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benesch M., Kurz H., Eber E., Varga E.M., Gopfrich H., Pfleger A. Clinical and histopathological findings in two Turkish children with follicular bronchiolitis. Eur J Pediatr. 2001;160:223–226. doi: 10.1007/pl00008432. [DOI] [PubMed] [Google Scholar]
- 7.Ryu J.H., Myers J.L., Swensen S.J. Bronchiolar disorders. Am J Respir Crit Care Med. 2003;168(11):1278–1292. doi: 10.1164/rccm.200301-053SO. [DOI] [PubMed] [Google Scholar]
- 8.Yousem S.A., Colby T.V., Carrington C.B. Follicular bronchitis/bronchiolitis. Hum Pathol. 1985;16:700–706. doi: 10.1016/s0046-8177(85)80155-6. [DOI] [PubMed] [Google Scholar]
- 9.Aerni M.R., Vassallo R., Myers J.L., Lindell R.M., Ryu J.H. Follicular bronchiolitis in surgical lung biopsies: clinical implications in 12 patients. Respir Med. 2008;102(2):307–312. doi: 10.1016/j.rmed.2007.07.032. [DOI] [PubMed] [Google Scholar]
- 10.Howling S.J., Hansell D.M., Wells A.U., Nicholson A.G., Flint J.D., Muller N.L. Follicular bronchiolitis: thin-section CT and histologic findings. Radiology. 1999;212:637–642. doi: 10.1148/radiology.212.3.r99se04637. [DOI] [PubMed] [Google Scholar]


