Abstract
Object
Microsurgical resection of supratentorial cavernomas associated with intractable epilepsy is performed frequently. Despite its common occurrence, little is known about patient perceptions of microsurgical resection for cavernomas. This survey study was performed to investigate patient perceived outcome after surgery for cavernomas associated with intractable epilepsy.
Methods
The authors’ surgical database was searched for cavernoma resection performed between 1971 and July of 2006. Of the initial 173 patients identified, 102 met criteria for medically intractable seizures. These 102 patients were then mailed a survey to determine follow-up and patient satisfaction. Thirty-nine surveys were returned as undeliverable, and 30 (48%) of the remaining 63 patients responded.
Results
The average age at surgery for patients responding to this survey was 40 ± 16 years compared with 35 ± 15 years for all 102 patients. At prolonged follow-up, 87% of patients reported being seizure-free. Of those with seizures, 2 (7%) reported being nearly seizure-free (rare disabling seizures), 2 (7%) believed they had a worthwhile improvement in seizure frequency, and no patient (0%) in this series believed they did not have a worthwhile improvement in seizure frequency. Ninety percent of responders stated they definitely, and 10% probably, would have surgery again. No patient responded that they probably or definitely would not have epilepsy surgery. Mean clinical follow-up was 36 ± 8 months and survey follow-up was 97 ± 13 months for these 30 patients. Use of the mail-in survey increased follow-up length 2.7 times longer compared with clinical follow-up.
Conclusions
It is clear from this select group of survey responders that patients undergoing surgery for cavernomas associated with medically intractable epilepsy are happy they underwent surgery (100%) and had excellent surgical outcomes (87% seizure-free) at prolonged follow-up of 97 ± 13 months. These survey results support that microsurgical resection for cavernomas is highly effective and significantly improves these patients’ quality of life.
Keywords: cavernoma, epilepsy, survey, patient outcome, postal questionnaire
Cavernomas (cavernous hemangiomas) present in a relatively diverse fashion in the CNS. Infratentorial lesions typically present with stepwise deterioration in neurological function as the result of hemorrhage. Supratentorial lesions may present incidentally with hemorrhage, or most typically, with seizures (40%–70%).1,12 Previously, we have reported outcomes of supratentorial cavernomas in patients presenting with intractable seizures.20 These outcomes, as in all studies to date, are based on clinician assessment of the patient’s last clinic presentation.1,2,5–9,12,13,15,19,20,22
As government interests and insurance control become slowly integrated into health care in the US and globally, it is clear that patient-centered comparative effectiveness research outcomes will be used to guide payment decisions.10 Comparative effectiveness research or patient-assessed satisfaction/outcome is a relatively soft concept (subjectively evaluated) and infrequently reported in relation to neurosurgical procedures. There is no current literature regarding microsurgical resection of cavernous hemangiomas and patient-assessed satisfaction. Therefore, this study was undertaken to detail patient-assessed outcomes and satisfaction in microsurgical resection of cavernomas associated with epilepsy.
Methods
Inclusion Criteria
This study was approved by the Mayo Clinic Institutional Review Board. The Mayo Clinic surgical databases contained records on 173 patients who underwent cavernoma resection between 1971 and July of 2006. All records were screened for neuropathological confirmation of cavernous hemangioma and then determined to meet criteria for medically intractable seizures (failure to control seizures while receiving 2 antiepileptic medications at therapeutic dosing). Of the initial 173 patients, 102 met criteria for medically intractable seizures. These 102 patients were then mailed a survey to determine follow-up and patient satisfaction; 39 were returned as undeliverable. Thirty patients responded, giving a response rate of 48% (30 of 63 possible).
Demographic Evaluation
Patient sex, age at operation, lobular lesion location, and size were abstracted from the clinical charts.
Survey Design
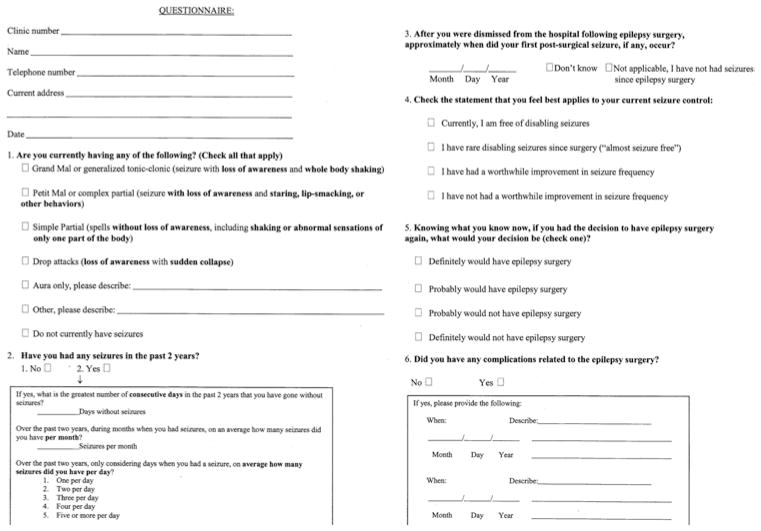
A 2-page survey (Fig. 1) designed to assess seizure type (based on semiology), outcome from epilepsy surgery (based on Engel classification and International League Against Epilepsy outcome scale score), and patient perceived satisfaction was used.21 The survey was designed with the goal of creating a useful tool for outcome follow-up that would not represent a significant burden for patients to respond. The 2-page survey was sent by US mail to all patients.
Fig. 1.
Survey form used in the study.
Analysis of Follow-Up
Follow-up was determined by date of initial surgery to date of clinic follow-up or survey follow-up postal marking. Follow-up calculations were based on a 360-day year and a 30-day month. Furthermore, Engel seizure outcome classifications were based on last clinic visit with a neurologist subspecializing in epilepsy. Our Engel classification of these patients has been previously described.20
Results
Patient Demographics
The average age of the patients responding to this survey (survey group) was 40 ± 16 years old compared with 35 ± 15 years old in all 102 patients asked to participate (total patient pool). In the survey group, 14 (47%) of 30 were women compared with 57 (56%) of 102 in the total patient pool. Average lesion sizes were 1.9 ± 1 cm in the survey group compared with 1.8 ± 1 cm in the total patient pool. In the survey group there were 13 left-sided lesions (43%) versus 51 (50%) in the total patient pool. Table 1 lists the locations of resected cavernomas in the survey and total patient pool groups.
TABLE 1.
Location of cavernomas according to group
| No. in Each Group (%)
|
||
|---|---|---|
| Lesion Location | Survey | Total Patient Pool |
| temporal | 17 (57) | 61 (60) |
| mesial | 8 (27) | 35 (34) |
| neocortical | 9 (30) | 26 (25) |
| frontal | 6 (20) | 21 (20) |
| parietal | 5 (17) | 14 (14) |
| occipital | 2 (7) | 6 (6) |
| total | 30 | 102 |
Surgical Procedure
All patients undergoing resection outside the temporal lobe underwent lesionectomy alone. Two patients are currently not seizure free. One patient harbored a frontal lesion bordering motor cortex, and he has experienced an improvement in seizure status and further resection would result in weakness. The second patient has a parietal lesion residing in sensory cortex abutting motor cortex, and further surgery would result in a worsening of present deficits; these patients have elected to continue medical therapy. Eight patients underwent resection of mesial temporal lobe cavernomas. Of these 8 patients, 6 underwent anterior temporal lobectomy with amygdalohippocampectomy, and 2 underwent lesionectomy alone. Nine patients harbored neocortical temporal cavernomas. Seven of these 9 patients underwent lesionectomy alone, and 2 did not have prolonged seizure-free status and required repeat surgery (detailed below).
Repeat Surgery
Two patients in this series received repeat operations (1 man and 1 woman). The lesions were 1.2- and 5-cm cavernomas, respectively. The first patient was seizure-free for 4 years until recurrence, then after a medication trial underwent mesial structure resection. She is currently seizure free. The second patient experienced a partial reduction in seizures during the first year after surgery, but was considered Engel Class IV. After repeat surgery, he was seizure-free after surgery for 35 days and now continues to experiences seizures, but these have been simple partial seizures without generalization. Both patients’ cavernomas were left neocortical temporal. Their repeat operation was a completion anterior temporal lobectomy with amygdalohippocampectomy. Neither patient underwent electrocorticography at the time of their initial surgery.
Survey Responses
In response to the first question on the survey (“Are you currently having any of the following”), 26 (87%) did not currently have seizures, 3 (10%) had complex partial seizures, and 1 (3%) had simple partial seizures (Table 2). In response to the second question (“Have you had any seizures in the past 2 years?”), 26 (87%) said no. Of the 4 (13%) that said yes, their greatest number of days without a seizure over the last 2 years was 120, 35, 50, and 21 days, respectively, and their average number of seizures per month was 3, 2, 2, and 8 seizures, respectively. In response to Question 4 (“Check the statement that you feel best applies to your current seizure control”), 26 (87%) were currently free of disabling seizures, 2 (7%) were almost seizure free (rare disabling seizures), 2 (7%) believed they experienced a worthwhile improvement in seizure frequency (Engel Class III), and no patient (0%) in this survey group believed they did not have a worthwhile improvement in seizure frequency. Regarding the fifth question (“Knowing what you know now, if you had the decision to have epilepsy surgery again, what would your decision be?”), 27 (90%) definitely would have surgery again, 3 (10%) probably would have surgery again, and no patient (0%) responded they probably or definitely would not have epilepsy surgery. Lastly, in response to the sixth question (“Did you have any complications related to the epilepsy surgery?”), 4 (13%) believed they suffered a complication related to epilepsy surgery. The write-in responses for what they considered complications were poor facial recall, incisional headache, mild unilateral weakness, and mild unilateral sensory loss (last 2 complications in the same patient).
TABLE 2.
Responses to survey questions
| Survey Question | Percentage |
|---|---|
| are you currently having any of the following: | |
|
| |
| grand mal or generalized tonic-clonic seizure | 0 |
| petit mal or complex partial seizure | 10 |
| simple partial seizure | 3 |
| drop attacks | 0 |
| aura only | 0 |
| other | 0 |
| do not currently have seizures | 87 |
|
| |
| have you had any seizures in the past 2 years: | |
|
| |
| yes | 13 |
| no | 87 |
|
| |
| check the statement that you feel best applies to your current seizure control: | |
|
| |
| currently, I am free of disabling seizures | 87 |
| I have rare disabling seizures since surgery | 7 |
| I have had a worthwhile improvement in seizure frequency | 7 |
| I have not had a worthwhile improvement in seizures | 0 |
|
| |
| would you have epilepsy surgery again: | |
|
| |
| definitely would | 90 |
| probably would | 10 |
| probably would not | 0 |
| definitely would not | 0 |
Follow-Up
Mean clinical follow-up was 36 ± 8 months (range 0–164 months) for these 30 patients. Survey follow-up was 97 ± 13 months (range 9–317 months). Follow-up by mail-in survey increased follow-up duration 2.7 times longer. Of the 30 responders, 6 returned to their home institutions for follow-up and therefore had unknown outcome at our institution. Of 24 patients with known follow-up, 22 were seizure-free (92%) and 2 were not. Of the 6 patients without any known clinical follow-up, 1 reported seizures. Interestingly, 1 of the 24 patients followed clinically reported simple partial seizures. She had been followed clinically for more than 5 years and these “seizures” were determined to be amnestic spells with an unknown cause and negative electroencephalographic findings for epileptiform activity. Agreement was high (κ = 0.78) between reported seizure-free rates and the clinically determined rate.
Discussion
Microsurgical resection of cavernomas responsible for intractable epilepsy is evidently a heterogeneous procedure in the literature.5,12,20,22 This is likely due to the ongoing debate as to the extent of tissue surrounding the cavernoma that needs to be removed to achieve the best outcome for the patient.2,5,12,19,20,22 Ultimately, approximately 90% of patients realize a decrease in seizure frequency and 60% to 90% achieve seizure freedom depending on the surgical approach used.2,5,7,12,13,15,19,20 Interestingly, 87% of our survey responders were seizure free, which is imperative when one considers the average follow-up interval of more than 8 years. This data suggests that not only is microsurgical resection of cavernomas successful in the long-term, it likely has a significant impact on the HRQOL. The evaluation of HRQOL is increasingly being accepted as a vital component of clinical care and outcome appraisal. Given that these patients are typically 20 to 40 years of age, the HRQOL impact for society appears to be very significant.
Health-related quality of life has been evaluated in neurosurgery, with the most information available in surgical epilepsy. Stavem et al.18 compared medically and surgically treated patients with focal epilepsy in an age-and sex-matched retrospective cohort, noting seizure-free outcomes and results on the Quality of Life in Epilepsy Inventory 89 questionnaire. In this study, postsurgical patients were seizure-free in 48% of cases (and used less medications) compared with 19% of controls.18 Health-related quality of life was higher in 5 of 17 dimensions and worse in none compared with controls with an average of more than 15 years of follow-up.18 In a long-term outcome study with similar patients, Spencer et al.17 demonstrated HRQOL improved after resection regardless of outcome. These studies support that surgical treatment for focal epilepsy improves HRQOL, as this report implies.
There are currently no data pertaining to the patient’s perception on outcome and satisfaction in relation to CNS cavernomas.1 Furthermore, an extensive literature search reveals no published information on comparative effectiveness research in neurosurgery for any procedure. Perhaps this is due to the subjective nature of the data, but it is becoming more and more important that we begin to consider patients’ feelings regarding their operations postoperatively as this may guide reimbursements in the future. Furthermore, implications beyond seizure freedom such as depression, return to work, and driver’s licensure will need to be documented to justify these procedures.
Patient satisfaction with the procedure performed is also infrequently reported in the literature, but it is present in surgical epilepsy series.3 In a series of 42 children undergoing temporal lobe resection for various pathologies, including 3 cavernomas, evaluation of satisfaction found that most families were very satisfied. Furthermore, of those who were seizure free, all were satisfied with the procedure, and of those with poor Engel classes (III or IV, minimal improvement in seizure control), most were neutral regarding surgery.3 It should be noted that half of these patients underwent tumor resections and therefore it may be difficult to generalize this study to our current study.3 Postsurgically, 82% of these patients were not taking anticonvulsants.3 Other studies have validated that HRQOL in epilepsy patients who underwent surgery is related to seizure-free outcome, medications, and driver status postsurgically.4,11
It is difficult to assess why mailed-in response rates are so low in this study (48%). We were unable to reliably detect whether there was a change in address or if mail was not returned for another reason. Likely due to the prolonged time period of the study, as well as the referral pattern of our hospital, many of our patients were not able to be tracked. Other postal survey outcome studies have experienced similar reported response rates (between 30% and 50%).11,14,16 The relatively low response rate may introduce a reporting bias in which dissatisfied patients did not respond.
Conclusions
It is clear from this select group of survey responders that patients undergoing surgery for cavernomas associated with medically intractable epilepsy are happy they underwent surgery (100%) and had excellent surgical outcomes (87% seizure free) at prolonged follow-up of 97 ± 13 months. These data indicate that microsurgical resection for cavernomas is likely highly effective and supports that the procedure significantly improves the patients’ quality of life.
Acknowledgments
The authors would like to thank Karla Crockett for her administrative support of our epilepsy surgery database and tireless patient care, as well as Dr. Aaron Cohen-Gadol for his development of the epilepsy surgery database.
Abbreviation used in this paper
- HRQOL
health-related quality of life
Footnotes
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author contributions to the study and manuscript preparation include the following. Conception and design: all authors. Acquisition of data: Worrell, Van Gompel. Analysis and interpretation of data: Worrell, Van Gompel. Drafting the article: all authors. Critically revising the article: all authors. Reviewed final version of the manuscript and approved it for submission: all authors. Statistical analysis: Van Gompel. Study supervision: Worrell, Marsh, Meyer.
References
- 1.Awad I, Jabbour P. Cerebral cavernous malformations and epilepsy. Neurosurg Focus. 2006;21(1):e7. doi: 10.3171/foc.2006.21.1.8. [DOI] [PubMed] [Google Scholar]
- 2.Baumann CR, Schuknecht B, Lo Russo G, Cossu M, Citterio A, Andermann F, et al. Seizure outcome after resection of cavernous malformations is better when surrounding hemosiderin-stained brain also is removed. Epilepsia. 2006;47:563–566. doi: 10.1111/j.1528-1167.2006.00468.x. [DOI] [PubMed] [Google Scholar]
- 3.Benifla M, Rutka JT, Otsubo H, Lamberti-Pasculli M, Elliott I, Sell E, et al. Long-term seizure and social outcomes following temporal lobe surgery for intractable epilepsy during childhood. Epilepsy Res. 2008;82:133–138. doi: 10.1016/j.eplepsyres.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Buschmann F, Wagner K, Metternich B, Biethahn S, Zentner J, Schulze-Bonhage A. The impact of extratemporal epilepsy surgery on quality of life. Epilepsy Behav. 2009;15:166–169. doi: 10.1016/j.yebeh.2009.02.041. [DOI] [PubMed] [Google Scholar]
- 5.Cappabianca P, Alfieri A, Maiuri F, Mariniello G, Cirillo S, de Divitiis E. Supratentorial cavernous malformations and epilepsy: seizure outcome after lesionectomy on a series of 35 patients. Clin Neurol Neurosurg. 1997;99:179–183. doi: 10.1016/s0303-8467(97)00023-1. [DOI] [PubMed] [Google Scholar]
- 6.Casazza M, Avanzini G, Ciceri E, Spreafico R, Broggi G. Lesionectomy in epileptogenic temporal lobe lesions: preoperative seizure course and postoperative outcome. Acta Neurochir Suppl. 1997;68:64–69. doi: 10.1007/978-3-7091-6513-3_12. [DOI] [PubMed] [Google Scholar]
- 7.Casazza M, Broggi G, Franzini A, Avanzini G, Spreafico R, Bracchi M, et al. Supratentorial cavernous angiomas and epileptic seizures: preoperative course and postoperative outcome. Neurosurgery. 1996;39:26–34. doi: 10.1097/00006123-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Cascino GD, Jack CR, Jr, Parisi JE, Sharbrough FW, Schreiber CP, Kelly PJ, et al. Operative strategy in patients with MRI-identified dual pathology and temporal lobe epilepsy. Epilepsy Res. 1993;14:175–182. doi: 10.1016/0920-1211(93)90022-y. [DOI] [PubMed] [Google Scholar]
- 9.Chang EF, Gabriel RA, Potts MB, Garcia PA, Barbaro NM, Lawton MT. Seizure characteristics and control after microsurgical resection of supratentorial cerebral cavernous malformations. Neurosurgery. 2009;65:31–38. doi: 10.1227/01.NEU.0000346648.03272.07. [DOI] [PubMed] [Google Scholar]
- 10.Cohen JP, Bridges JFP. Assessing comparative effectiveness research in the US. Appl Health Econ Health Policy. 2009;7:219–224. doi: 10.1007/BF03256155. [DOI] [PubMed] [Google Scholar]
- 11.Elsharkawy AE, May T, Thorbecke R, Ebner A. Predictors of quality of life after resective extratemporal epilepsy surgery in adults in long-term follow-up. Seizure. 2009;18:498–503. doi: 10.1016/j.seizure.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Ferrier CH, Aronica E, Leijten FSS, Spliet WGM, Boer K, van Rijen PC, et al. Electrocorticography discharge patterns in patients with a cavernous hemangioma and pharmacoresistent epilepsy. J Neurosurg. 2007;107:495–503. doi: 10.3171/JNS-07/09/0495. [DOI] [PubMed] [Google Scholar]
- 13.Ferroli P, Casazza M, Marras C, Mendola C, Franzini A, Broggi G. Cerebral cavernomas and seizures: a retrospective study on 163 patients who underwent pure lesionectomy. Neurol Sci. 2006;26:390–394. doi: 10.1007/s10072-006-0521-2. [DOI] [PubMed] [Google Scholar]
- 14.Harris IA, Khoo OK, Young JM, Solomon MJ, Rae H. Lottery incentives did not improve response rate to a mailed survey: a randomized controlled trial. J Clin Epidemiol. 2008;61:609–610. doi: 10.1016/j.jclinepi.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 15.Kivelev J, Niemelä M, Kivisaari R, Dashti R, Laakso A, Hernesniemi J. Long-term outcome of patients with multiple cerebral cavernous malformations. Neurosurgery. 2009;65:450–455. doi: 10.1227/01.NEU.0000346269.59554.DB. [DOI] [PubMed] [Google Scholar]
- 16.Rodriguez HP, von Glahn T, Rogers WH, Chang H, Fanjiang G, Safran DG. Evaluating patients’ experiences with individual physicians: a randomized trial of mail, internet, and interactive voice response telephone administration of surveys. Med Care. 2006;44:167–174. doi: 10.1097/01.mlr.0000196961.00933.8e. [DOI] [PubMed] [Google Scholar]
- 17.Spencer SS, Berg AT, Vickrey BG, Sperling MR, Bazil CW, Haut S, et al. Health-related quality of life over time since resective epilepsy surgery. Ann Neurol. 2007;62:327–334. doi: 10.1002/ana.21131. [DOI] [PubMed] [Google Scholar]
- 18.Stavem K, Bjørnaes H, Langmoen IA. Long-term seizures and quality of life after epilepsy surgery compared with matched controls. Neurosurgery. 2008;62:326–335. doi: 10.1227/01.neu.0000315999.58022.1c. [DOI] [PubMed] [Google Scholar]
- 19.Stavrou I, Baumgartner C, Frischer JM, Trattnig S, Knosp E. Long-term seizure control after resection of supratentorial cavernomas: a retrospective single-center study in 53 patients. Neurosurgery. 2008;63:888–897. doi: 10.1227/01.NEU.0000327881.72964.6E. [DOI] [PubMed] [Google Scholar]
- 20.Van Gompel JJ, Rubio J, Cascino GD, Worrell GA, Meyer FB. Electrocorticography-guided resection of temporal cavernoma: is electrocorticography warranted and does it alter the surgical approach? Clinical article. J Neurosurg. 2009;110:1179–1185. doi: 10.3171/2008.10.JNS08722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wieser HG, Blume WT, Fish D, Goldensohn E, Hufnagel A, King D, et al. ILAE Commission Report. Proposal for a new classification of outcome with respect to epileptic seizures following epilepsy surgery. Epilepsia. 2001;42:282–286. [PubMed] [Google Scholar]
- 22.Yeon JY, Kim JS, Choi SJ, Seo DW, Hong SB, Hong SC. Supratentorial cavernous angiomas presenting with seizures: surgical outcomes in 60 consecutive patients. Seizure. 2009;18:14–20. doi: 10.1016/j.seizure.2008.05.010. [DOI] [PubMed] [Google Scholar]