Abstract
Cerebellar injury is an important complication of preterm birth with far-reaching neuropsychiatric sequelae. We have previously shown a significant association between isolated injury to the premature cerebellum and subsequent impairment of regional volumetric growth in the contralateral cerebrum. In the current study, we examine the relationship between these remote regional impairments of cerebral volumetric growth and domain-specific functional deficits in these children. In 40 ex-preterm infants with isolated cerebellar injury, we performed neurodevelopmental evaluations and quantitative magnetic resonance imaging (MRI) studies at a mean age of 34 months. We measured cortical gray matter volumes in 8 parcellated regions of each cerebral hemisphere, as well as right and left cerebellar volumes. We show highly significant associations between early signs of autism and dorsolateral prefrontal cortex volume (P < 0.001); gross motor scores and sensorimotor cortical volumes (P < 0.001); and cognitive and expressive language scores and premotor and mid-temporal cortical volumes (P < 0.001). By multivariate analyses, each unit increase in the corresponding regional cerebral volume was associated with lower odds of abnormal outcome score, adjusted for age at MRI and contralateral cerebellar volume. This is the first report linking secondary impairment of remote cerebral cortical growth and functional disabilities in survivors of prematurity-related cerebellar brain injury.
Keywords: cerebellum, cerebral cortex, magnetic resonance imaging, outcome, preterm
Introduction
Survivors of prematurity are at significant risk of adverse neurodevelopmental outcome originating from brain injury sustained in the newborn period (Hoekstra et al. 2004; Himmelmann et al. 2005; Dyet et al. 2006; Msall 2006; Dubois et al. 2008; Kesler et al. 2008; Volpe 2009; Smith et al. 2011). Until recently, the predilection of the premature cerebellum to injury was under-recognized (Limperopoulos, Benson, et al. 2005). The majority of prematurity-related cerebellar injuries occur in the late second trimester, (Limperopoulos, Benson, et al. 2005; Maddalena and Gibbins 2008; Steggerda et al. 2009; Biran et al. 2011; McCarthy et al. 2011) prior to a critical period of brain, and particularly cerebral cortical, development (Bystron et al. 2008). In previous reports, we characterized the prevalence of prematurity-related cerebellar injury, as well as the structural and functional outcomes in survivors (Limperopoulos, Benson, et al. 2005; Limperopoulos, Soul, et al. 2005; Limperopoulos et al. 2007, Limperopoulos et al. 2010). More recently, our studies have focused on the effects of cerebellar injury on subsequent brain development. In addition to later disturbances in the development of the injured cerebellum, we have shown that volumetric development of the uninjured contralateral cerebral hemisphere may be impaired and that this remote growth effect is largely confined to cerebral regions known to be activated in the mature brain by afferent pathways from the contralateral cerebellum (Limperopoulos et al. 2010). Such cerebellar projection areas of the cerebral cortex include the dorsolateral prefrontal, premotor, sensorimotor, and mid-temporal regions (Limperopoulos et al. 2010). In addition, we have shown through comprehensive neuropsychological testing that the long-term functional phenotype of prematurity-related cerebellar injury includes prominent deficits in “higher order” domains previously considered cerebral, and usually cortical, in origin including deficits in cognitive, emotional, and behavioral function (Limperopoulos et al. 2007).
In the current study, we extend our investigations in survivors of prematurity-related cerebellar injury by addressing the following question: When controlling for the extent of cerebellar injury, is there an association between regional impairments of volumetric development of the cerebral cortex and domain-specific long-term functional deficits in these children?
Materials and Methods
As part of a prospective study, we recruited preterm infants (<32 weeks gestational age) born between January 1998 and December 2005, with isolated cerebellar injury (i.e., the absence of associated supratentorial parenchymal lesions) diagnosed in the neonatal period by cranial ultrasound and confirmed by magnetic resonance imaging (MRI). These conventional neonatal MRI studies were reviewed to confirm the diagnosis of cerebellar parenchymal injury and to exclude infants with cerebral parenchymal injury. Detailed inclusion and exclusion criteria have been previously described (Limperopoulos et al. 2010). Children underwent follow-up quantitative MRI studies and standardized neurodevelopmental outcome testing. The study was approved by the Committee for Clinical Investigation at Children's Hospital Boston, and informed written consent was obtained in all cases.
MRI Acquisitions
The MRI studies were performed on a 1.5-T General Electric Signa System magnetic resonance scanner (Milwaukee, WI, United States of America), using an 8-channel phased array head coil. MRI sequences included conventional, spin-echo T1-weighted, fast spin-echo T2-weighted images, multiplanar gradient-recalled echo susceptibility sensitive sequence, 3-dimensional Fourier-transform spoiled gradient-recalled sequence (1.5-mm coronal slices; flip angle: 45°; repetition time: 35 ms; echo time: 3 ms; field of view: 20 cm; matrix: 256 × 256; 116 slices), and double-echo (proton density and T2-weighted), spin-echo sequence (3-mm axial slices; repetition time: 5000 ms; echo time: 50 ms; field of view: 20 cm; matrix: 256 × 256, interleaved acquisition; 58 slices).
MRI Analyses
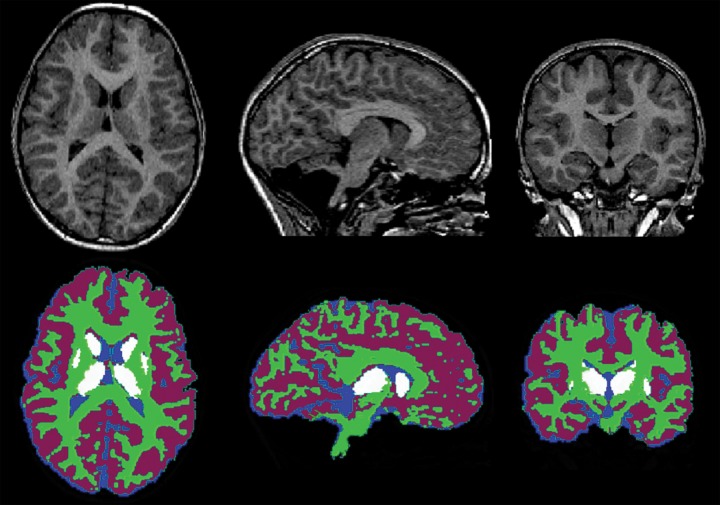
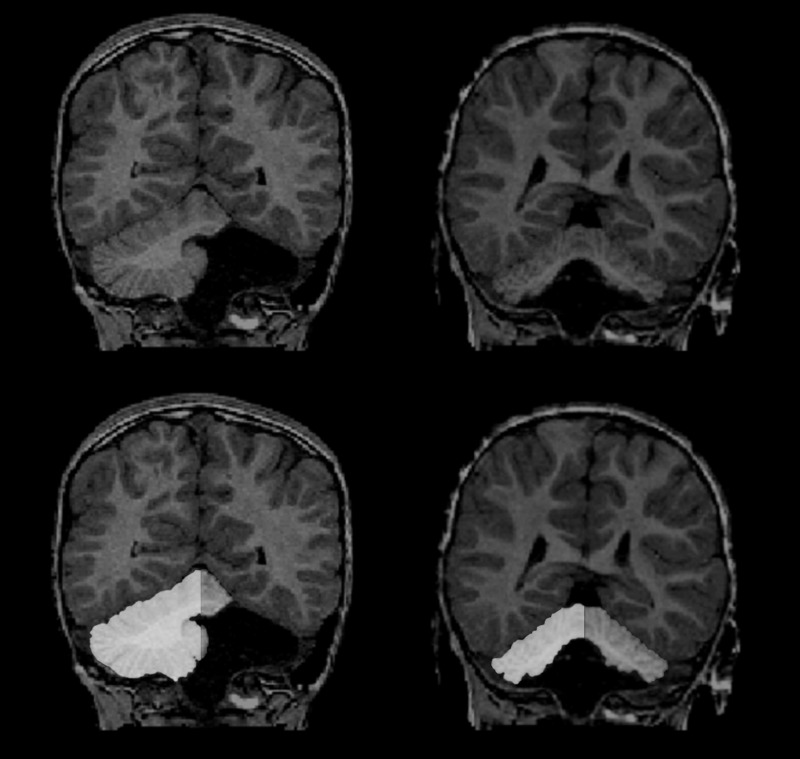
The MRI studies were examined by an experienced pediatric neuroradiologist (R.L.R.) blinded to the clinical and previous MRI findings, as well as the neurodevelopmental outcome data. The neuroradiologist confirmed our inclusion criterion of the absence of injury to the supratentorial structures and categorized the cerebellar lesions as unilateral or bilateral. Our quantitative volumetric MRI analyses have been previously described (Limperopoulos et al. 2010). Briefly, each MRI study was first automatically segmented into 3 tissue classes: Cortical gray matter, white matter, and cerebrospinal fluid, using a previously validated probabilistic classification method (Zijdenbos and Dawant 1994), while subcortical gray matter was manually delineated, with an intrarater reliability of 0.96 (Limperopoulos et al. 2010) (Fig. 1). To obtain separate measurements for cerebral and cerebellar volumes, total cerebellar volumes (cerebellar gray matter volume + cerebellar white matter volume) were subtracted from the total brain volume by manually outlining the cerebellum onto the ICBM-152 template (Evans et al. 1993; using the Montreal Neurological Institute Display software (www.bic.mni.mcgill.ca/ServicesSoftware); the invert of the nonlinear registration transformation was then applied to resample the cerebellar mask onto the subject's native space. Intrarater reliability for cerebellar manual outlining was 0.96 (Limperopoulos et al. 2010). We did not formally parcellate the cerebellum into specific regions; instead the cerebellar hemispheres and vermis were divided through the midsagittal plane using a previously validated technique (Limperopoulos, Soul, et al. 2005). The midsagittal plane was used to ensure that the vermis was divided using a consistent approach for all MRI studies. This served as a measure of the injury to the left and right cerebellar hemispheres (Fig. 2).
Figure 1.
Brain segmentation illustrating cortical and cerebellar gray matter (purple), cerebral and cerebellar white matter (green), subcortical gray matter (white), and cerebrospinal fluid (blue).
Figure 2.
Examples of a subject with unilateral left cerebellar injury (upper left) and another with bilateral cerebellar injury (upper right), and corresponding cerebellar parcellations: Right cerebellar hemisphere (white) and left cerebellar hemisphere (gray).
Regional comparisons in the cerebrum were made using a previously described and validated Talairach scheme (Peterson et al. 2000). Each cerebral hemisphere was divided into 8 anatomical regions (Fig. 3): Dorsolateral prefrontal, orbitofrontal, premotor, subgenual, sensorimotor, mid-temporal, parieto-occipital, and inferior occipital using the axial plane passing through the anterior commissure and posterior commissure line and 3 limiting coronal planes. Intrarater reliability for regional volumes was evaluated on 7 MRI studies by a single operator (N.G.) using intraclass correlations and was >0.89 (Limperopoulos et al. 2010). Since we were interested in the furthest downstream effects of potential trophic withdrawal after cerebellar injury, we focused our study on remote cortical growth and not on white matter or subcortical gray matter volume.
Figure 3.
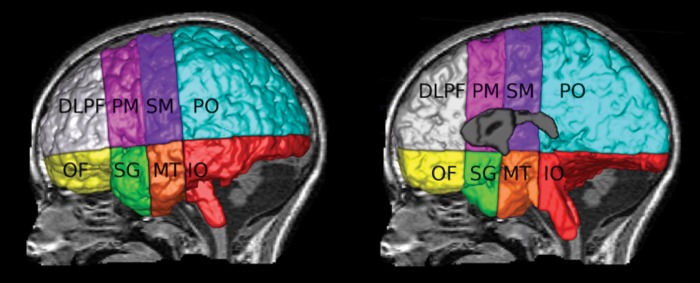
Parcellation of the external (left) and internal cerebral hemispheres (right) into 16 regions (8 right hemisphere and 8 left hemisphere): Dorsolateral prefrontal (DLPF; gray), premotor (PM; pink), sensorimotor (SM; purple), parieto-occipital (PO; blue), orbitofrontal (OF; yellow), subgenual (SG; green), midtemportal (MT; orange), and inferior occipital (IO; red).
Neurodevelopmental Outcome Testing
In our cohort, we explored a broad range of neurodevelopmental functions including gross and fine motor skills, language, cognition, social–behavior, and affect (described below). We adjusted postnatal age to account for prematurity in all subjects <24 months of age at testing. Evaluators were blinded to past medical history, MRI findings, and to each other's clinical findings.
A licensed pediatric psychologist (N.S.) administered the “Mullen Scales of Early Learning” (Mullen) (Mullen 1995), which is a standardized developmental assessment for children from 0 to 69 months of age. The Mullen includes 5 subscales: Gross motor, fine motor, visual reception (i.e., cognition), receptive language and expressive language (mean 50, standard deviation [SD] 10), and a summary measure of general cognitive function underlying all cognitive performances (early learning composite; mean 100, SD 15). A score below 2 SD of the normative mean was defined as abnormal.
A pediatric occupational therapist (C.L.) administered the “Peabody Developmental Motor Scales” (Folio and Fewell 1983), which is a standardized assessment for gross motor and fine motor abilities in children from 0 to 65 months. A score below 2 SD of the normative mean was defined as abnormal.
The “Child Behavior Checklist (CBCL 1.5–5)” was completed by the primary caregiver to determine the frequency of behavioral problems in our cohort. Both externalizing and internalizing problem behavior scores were derived. Internalizing behavior problems include the following scales: Withdrawn, somatic complaints, and anxious and depressed syndromes, and externalizing behavior scales consists of the delinquent and aggressive behavior syndrome. The clinical range is defined as T scores >64, the borderline range as T scores from 60 to 63, and the normal range consists of T scores <60.
The “Modified Checklist for Autism in Toddlers” (M-CHAT) was used to screen all children's behaviors for early signs of autism by parental report (Robins et al. 2001). The M-CHAT is a 23-item yes/no parent report screening instrument for autistic spectrum disorders. Critical items include items concerning joint attention, interest in other children, responding to name, and imitation. Cut-off scores of at least 2 critical items or 3 total items on the checklist are used.
We tested developmental performance in a broad spectrum of domains using standardized instruments. To maintain statistical power we confined our structure–function analyses to selected developmental domains including gross motor skills (Peabody), expressive language skills (Mullen), visual reception skills (Mullen), positive autism screening (M-CHAT), and internalizing behavior problems (CBCL).
Statistical Analysis
All statistical analyses were performed using SAS 9.2 statistical program. Descriptive statistics were performed to highlight the study participants' main clinical, neurodevelopmental, and MRI characteristics.
Partial correlation analyses were performed to examine the association between cerebral volumes in 8 regions for 2 hemispheres (left and right) separately and neurodevelopmental scores, adjusting for age at MRI and contralateral cerebellar volume. Multiple logistic regression analyses were performed to examine the relationship between dichotomous neurodevelopmental scores (normal vs. abnormal) and cerebral volumes. The logistic regression analysis modeled the probability for an abnormal score on the 5 neurodevelopment outcome measures in 8 regions for 2 hemispheres accounting for the presence of 2 additional covariates (age at MRI and contralateral cerebellar volume).
Simple and multiple linear regression analyses were performed for all 5 neurodevelopmental outcome measures to explore the relationship with cerebral gray matter volumes separately for the right and left hemispheres. Residual plots were inspected to verify linearity, normality, and homoscedasticity assumptions for all univariate and multiple regression models. Additionally, a robust regression was carried out to identify potential outliers and leverage points. Finally, collinearity was assessed based on tolerance, variation of inflation, and eigenvalues. Regression shrinkage (LASSO) and least angle regression methods were applied as a starting point for further analysis to identify parsimonious models for the neurdevelopmental outcome variables.
To test the hypothesis that the associations between neurodevelopmental scores and cerebral volumes would not be different for the right versus left hemispheric regions, the Dunn and Clark test using Fisher's Z transformation was carried out comparing correlated partial correlations. Finally, Fisher's Z transformation was applied to investigate differences in partial correlations between subjects with unilateral and bilateral cerebellar injury. All comparisons were adjusted for multiple testing using the Bonferroni correction.
Results
Characteristics of Our Cohort
Of the 48 ex-preterm subjects that met our inclusion criteria, 5 died in the early postnatal period, and of the available 43 subjects, 3 were lost to follow-up. The remaining 40 subjects (93% recruitment) underwent follow-up MRI studies and developmental testing, of which 25 had unilateral cerebellar injury and 15 had bilateral cerebellar injury. The mean age at MRI and developmental testing was 34.5 ± 8.6 and 33.1 ± 9.1 (range 18–63 months), respectively. None of these subjects had evidence of structural injury to the cerebral hemispheres on conventional MRI, as interpreted by an experienced neuroradiologist (R.L.R.). The clinical characteristics of our cohort are described in Table 1.
Table 1.
Clinical characteristics of the study population (n = 40)
| Clinical characteristics | N (%) |
|---|---|
| Gender | |
| Male | 28 (70.0) |
| Female | 12 (30.0) |
| Number of infants | |
| Singleton | 33 (82.5) |
| Multiple | 7 (17.5) |
| Side of cerebellar injury | |
| Left | 7 (17.5) |
| Right | 18 (45.0) |
| Bilateral | 15 (37.5) |
| Mean (SD) | |
| Gestational age (weeks) | 26.4 (1.9) |
| Birth weight (g) | 746.4 (198.7) |
| Total cerebral volume | 865.1 (109.5) |
| Total cerebral gray matter | 587.7 (68.2) |
| Total cerebral gray matter (right) | 296.7 (40.5) |
| Total cerebral gray matter (left) | 291.0 (38.5) |
| Total cerebellar volume | 59.6 (24.6) |
| Total left/right cerebellar volume | 32.7 (16.6)/26.9 (18.2) |
Developmental Outcomes
Details of the developmental performance on the selected 5 outcome measures are summarized in Table 2. Seventeen (43%) subjects demonstrated significant (<2 SD below the mean) gross and fine motor delays on the Peabody Developmental Motor Scales. Similarly, 17 children experienced expressive language delays (43%), 16 (40%) had visual receptive deficits, and 13 (33%) had receptive language delays on the Mullen. Additionally, 17 (43%) had testing positive for early signs of autism features on the M-CHAT and 15 (38%) had externalizing behavioral problems, while 11 (25%) had externalized behavioral problems on the CBCL.
Table 2.
Developmental outcomes of our cohort (N = 40)
| Developmental scores | N (%) |
|---|---|
| M-CHAT, mean (range) | 4.1 (0–15) |
| Normal | 23 (57.5) |
| Abnormal | 17 (42.5) |
| Internalizing, mean (range) | 54.0 (29–78) |
| Normal | 25 (62.5) |
| Abnormal | 15 (37.5) |
| Peabody_GM, mean (range) | 75.6 (65–95) |
| Normal | 23 (57.5) |
| Abnormal | 17 (42.5) |
| Mullen_VR, mean (range) | 33.8 (20–52) |
| Normal | 24 (60.0) |
| Abnormal | 16 (40.0) |
| Mullen_EL, mean (range) | 33.4 (20–56) |
| Normal | 23 (57.5) |
| Abnormal | 17 (42.5) |
Relationship Between Regional Cerebral Cortical Volumes and Continuous Developmental Outcome Measures
Overall partial correlation analysis results revealed similar patterns of the relationship between left and right regional cerebral volumes and developmental scores. The Dunn and Clark test did not reveal any statistically significant differences between partial correlations of the left and right cerebral hemispheres.
Significant moderate-to-high correlations were observed between M-CHAT scores and gray matter volumes in both the left (rp = −0.81, P < 0.001) and right (rp = −0.70, P < 0.001) dorsolateral prefrontal cortices (Table 3). Similarly, internalizing behavior scores were significantly correlated with regional volumes of both the dorsolateral prefrontal regions (left: rp = −0.66, P < 0.001 and right: rp = −0.75, P < 0.001). Not surprisingly, gross motor scores were significantly correlated with sensorimotor cortical volumes for both the left (rp = 0.66, P < 0.001) and right (rp = 0.74, P < 0.001) hemispheres. Visual reception scores were significantly associated with regional volumes of the premotor and mid-temporal cortical regions for both the left (premotor: rp = 0.68, P < 0.001 and mid-temporal: rp = 0.67, P < 0.001) and right hemispheres (premotor: rp = 0.54, P < 0.001 and mid-temporal: rp = −0.49, P < 0.001). Likewise, expressive language scores were related to premotor and mid-temoral left (premotor: rp = 0.67 and mid-temporal: rp = 0.58, P < 0.001) and right (premotor: rp = 0.52 and mid-temporal: rp = 0.66, P < 0.001) hemispheric volumes.
Table 3.
Relationship between regional cortical volumes and continuous developmental outcome measures
| IO | MT | SG | DLPF | PO | PM | SM | OF | |
|---|---|---|---|---|---|---|---|---|
| Left hemisphere | ||||||||
| M-CHAT | −0.09 (−0.40 to 0.24 | −0.48 (−0.70 to −0.19) | −0.18 (−0.47 to 0.15) | −0.81 (−0.90 to −0.67) | −0.37 (−0.62 to −0.06) | −0.49 (−0.70 to −0.20) | −0.39 (−0.63 to −0.08) | −0.35 (−0.60 to 0.03) |
| Internalizing | −0.11 (−0.42 to 0.21) | −0.29 (−0.56 to 0.03 | −0.03 (−0.35 to 0.29 | −0.67 (−0.81 to −0.44) | −0.06 (−0.37 to 0.27) | −0.35 (−0.60 to −0.04) | −0.28 (−0.55 to 0.04) | −0.23 (−0.51) to 0.10) |
| Peabody_GM | 0.15 (−0.18 to 0.45) | 0.19 (−0.13) to 0.48) | 0.45 (0.16 to 0.67) | 0.21 (−0.12 to 0.49) | 0.13 (−0.20) to 0.43) | 0.05 (−0.27 to 0.37) | 0.66 (0.43 to 0.81) | 0.07 (−0.26 to 0.38) |
| Mullen_VR | 0.19 (−0.14 to 0.48) | 0.67 (0.44 to 0.81) | 0.25 (−0.08 to 0.53) | 0.42 (0.12 to 0.65) | 0.16 (−0.17 to 0.46) | 0.68 (0.46 to 0.82) | 0.21 (−0.12 to 0.49) | −0.20 (−0.49 to 0.12) |
| Mullen_EL | 0.09 (−0.24 to 0.40) | 0.73 (0.54 to 0.85) | 0.23 (−0.10 to 0.51) | 0.43 (0.12 to 0.66) | 0.25 (−0.07 to 0.53) | 0.65 (0.41 to 0.80) | 0.07 (−0.26 to 0.38) | −0.29 (−0.55 to 0.04) |
| Right hemisphere | ||||||||
| M-CHAT | −0.07 (−0.38 to 0.26) | −0.43 (−0.66 to −0.13) | −0.19 (−0.48 to 0.14) | −0.70 (−0.83 to −0.48) | −0.37 (−0.62 to −0.06) | −0.45 (−0.67 to −0.16) | −0.34 (−0.60 to −0.02) | −0.25 (−0.53 to 0.08) |
| Internalizing | −0.18 (−0.47 to 0.15) | −0.29 (−0.56 to 0.03) | −0.03 (−0.35 to 0.29) | −0.60 (−0.77 to −0.35) | −0.08 (−0.39 to 0.25) | −0.34 (−0.60 to −0.03) | −0.26 (−0.54 to 0.06) | −0.15 (−0.45 to 0.18) |
| Peabody_GM | 0.13 (−0.19 to 0.43) | 0.13 (−0.19 to 0.43) | 0.53 (0.26 to 0.73) | 0.15 (−0.18 to 0.45) | 0.26 (−0.07 to 0.53) | −0.04 (−0.35 to 0.29) | 0.75 (0.56 to 0.86) | 0.07 (−0.26 to 0.38) |
| Mullen_VR | 0.05 (−0.27 to 0.37) | 0.49 (0.21 to 0.70) | 0.25 (−0.08 to 0.52) | 0.39 (0.08 to 0.63) | 0.19 (−0.13 to 0.48) | 0.54 (0.27 to 0.73) | 0.22 (−0.11 to 0.50) | −0.19 (−0.48 to 0.14) |
| Mullen_EL | −0.03 (−0.35 to 0.29) | 0.66 (0.43 to 0.81) | 0.22 (−0.11 to 0.50) | 0.35 (0.04 to 0.60) | 0.29 (−0.03 to 0.56) | 0.52 (0.24 to 0.72) | 0.11 (−0.22 to 0.42) | −0.26 (−0.53 to 0.07) |
DLPF: dorsolateral prefrontal; OF: orbitofrontal; PM: premotor; SG: subgenual; SM: sensorimotor; MT: mid-temporal; PO: parieto-occipital; IO: inferior occipital; GM: gross motor; VR: visual reception; EL: expressive language.
Relationship Between Regional Cortical Volumes and Dichotomous Developmental Outcome Measures
Table 4 presents the best logistic regression models selected for each dichotomous (normal/abnormal) developmental outcome measures. The logistic regression analysis modeled the probability of abnormality for each of the developmental scores. Thus, all tested models included the corresponding neurodevelopmental dichotomous outcome measures, main predictor regional cerebral volume, and 2 covariates (age at MRI and contralateral cerebellar volume). The best models were selected based on the most optimal Akaike Information criterion as well as models with discriminate power (area under the receiver operating characteristic [ROC] curve). Interestingly, the relationship between regional cerebral cortex volumes and risk for an abnormal developmental score was not significantly different between the left and right hemispheres. For all presented models, one unit increase in the corresponding cerebral volume was associated with lower odds of having an abnormal developmental score adjusted for age at MRI and contralateral cerebellar volume.
Table 4.
Relationship between regional cortical volumes and dichotomous outcome measures
| Neurodevelopment measure | Hemisphere | Region | Odds ratio |
Area under ROC curve | P-value | |
|---|---|---|---|---|---|---|
| eβ | 95% CI | |||||
| M-CHAT | Right | DLPF | 0.16 | 0.04–0.69 | 0.97 | 0.014 |
| Left | DLPF | 0.11 | 0.02–0.57 | 0.99 | 0.008 | |
| Internalizing behavior problems | Right | DLPF | 0.42 | 0.21–0.84 | 0.94 | 0.013 |
| Left | DLPF | 0.17 | 0.03–0.88 | 0.98 | 0.034 | |
| Gross motor delays (Peabody) | Right | SM | 0.43 | 0.25–0.75 | 0.92 | 0.002 |
| Left | SM | 0.54 | 0.35–0.83 | 0.88 | 0.005 | |
| Cognitive impairments (Mullen_VR) | Right | PM | 0.78 | 0.62–0.97 | 0.86 | 0.023 |
| Left | PM | 0.68 | 0.52–0.89 | 0.88 | 0.004 | |
| Expressive language (Mullen) | Right | MT | 0.65 | 0.47–0.92 | 0.84 | 0.013 |
| Left | MT | 0.55 | 0.37–0.83 | 0.86 | 0.004 | |
VR: visual reception; DLPF: dorsolateral prefrontal; SM: sensorimotor; PM: premotor; MT: mid-temporal.
Multivariate Analysis
Along with main predictors, cerebral gray matter volumes, additional explanatory variables assessed in the initial model were gestational age at birth, age at MRI, and contralateral cerebellar volumes. Results of the multivariate analysis are summarized in Table 5. Predictors included in the final models explained 47–72% of the variation in neurodevelopmental scores in the left cortical regional hemispheric volumes and 35–57% in the right regional cortical volumes. The selected models demonstrated a negative relationship between regional cerebral gray matter volumes with M-CHAT and internalizing behavioral problems on the CBCL, whereas a positive relationship was evident between selected regional cerebral volumes and gross motor (Peabody), visual reception (Mullen), and expressive language (Mullen) scores.
Table 5.
Summary of multiple regression analysis
| Outcome measure | Final model | Parameter estimates | 95% CI | P-value | R2 |
|---|---|---|---|---|---|
| Left hemisphere | |||||
| M-CHAT_23 | Left_cerebral_DLPF | −1.05 | (−1.27 to −0.83) | <0.001 | 71.8 |
| Internalizing | Left_cerebral_DLPF | −2.97 | (−4.0 to −1.93) | <0.001 | 46.9 |
| Peabody_GM | Left_cerebral_SM | 1.32 | (0.95 to 1.68) | <0.001 | 58.1 |
| Mullen_VR | Left_cerebral_PM | 0.71 | (0.17 to 1.25) | 0.011 | 62.4 |
| Left_cerebral_MT | 0.92 | (0.15 to 1.69) | 0.021 | ||
| Mullen_EL | Left_cerebral_MT | 1.58 | (0.83 to 2.33) | <0.001 | 64.0 |
| Right hemisphere | |||||
| M-CHAT_23 | Right_cerebral_DLPF | −0.80 | (−1.04 to −0.55) | <0.001 | 52.6 |
| Internalizing | Right_cerebral_DLPF | −2.26 | (−3.28 to −1.24) | <0.001 | 34.6 |
| Peabody_GM | Right_cerebral_SM | 1.32 | (0.92 to 1.71) | <0.001 | 54.9 |
| Mullen_VR | Right_cerebral_PM | 1.00 | (0.66 to 1.34) | <0.001 | 48.2 |
| Mullen_EL | Right_cerebral_MT | 1.65 | (1.18 to 2.12) | <0.001 | 56.9 |
GM: gross motor; VR: visual reception; EL: expressive language; DLPF: dorsolateral prefrontal; SM: sensorimotor; PM: premotor; MT: mid-temporal.
Relationship Between Regional Cerebral Cortical Volumes and Developmental Scores in Children with Unilateral Versus Bilateral Cerebellar Injury
A similar pattern of association between regional cerebral cortical volumes and specific developmental measures was noted between subjects with unilateral versus bilateral neonatal cerebellar injury. A comparison of the partial correlation coefficients between unilateral and bilateral groups using Fisher's Z transformation with Bonferroni adjustment did not reveal any statistical differences. Moreover, additional χ2 analysis of the proportions of preterm infants with abnormal developmental scores did not reveal statistical difference between unilateral and bilateral cerebellar injury groups (χ2 ranging 0.06–0.86 and corresponding P-values 0.35–0.80 for 5 developmental measures).
Discussion
We have previously shown that brain injury confined to the cerebellum of the premature newborn is associated with reduced growth in specific regions of the uninjured contralateral cerebral cortex (Limperopoulos, Soul, et al. 2005, Limperopoulos et al. 2010). Importantly, the affected cerebral cortical regions are known in the mature brain to be projection targets of the contralateral cerebellar hemisphere. We extend these observations in the current study by describing a significant association between these regional decreases in cerebral cortical volume and long-term neurodevelopmental outcome in these children. Specifically, we show that the risk of impaired cognitive, language, behavior, and motor performance increases significantly with decreasing regional volumes of the cerebral cortex. Furthermore, by controlling for volumetric growth in the injured cerebellar hemisphere, we show that secondary underdevelopment of cerebral cortical projection regions is an important structural correlate for long-term functional impairment in survivors of prematurity-related cerebellar injury. To our knowledge, this is the first study to examine the long-term functional impact of disturbed structural brain development occurring remote from known prematurity-related brain lesions.
In earlier studies, we showed that ex-premature infants with cerebellar injury are at significant risk for nonmotor higher order neurologic sequelae more typically associated with cerebral cortical dysfunction (Limperopoulos et al. 2007). In adults and older children with cerebellar injury and cerebellar malformations, this spectrum of nonmotor sequelae has been designated the cerebellar cognitive affective syndrome (Levisohn et al. 2000; Schmahmann 2004; Tavano et al. 2007). Our studies have supported the notion of a “developmental cerebellar cognitive affective syndrome” in survivors of prematurity-related cerebellar injury. The data from our current study suggest that the structural basis for such a developmental cerebellar cognitive affective syndrome is secondary disruption during the critical periods of cerebral cortical development in the third trimester and infancy.
In the mature brain, the prefrontal cortex plays a central role in the coordination of complex cognitive functions including the integration of higher order functions such as working memory, judgment, attention, language, planning, and motivational behavior (Barbas and Mesulam 1985; Cavada and Goldman-Rakic 1989; Eblen and Graybiel 1995). In our study, decreased prefrontal gray matter volumes were significantly associated with social and behavioral impairment. Relevant to our findings is the fact that the prefrontal cortex is one of the last cerebral regions to reach full maturation (Chugani et al. 1987). Our previous studies identified a significant prevalence of elevated risk for autistic spectrum behaviors following prematurity-related cerebellar injury (Limperopoulos et al. 2007, 2008). In the current study, positive screening for autism and internalizing behavior traits are associated with reduced volumes in the dorsolateral prefrontal cortex. We also show that impairments in cognitive and expressive language function are significantly related to reduced volumes in the premotor and mid-temporal cortex. Reciprocal circuits between the temporal lobe and cerebellum primarily involve the cortex of the superior temporal sulcus (Schmahmann and Pandya 1991), which is represented in the mid-temporal section of the parcellation scheme used in our study. The characteristic motor sequelae described after injury to the mature cerebellum, such as nystagmus, ataxia, dysmetria, or intention tremor (Schmahmann 2004), are rarely seen in survivors of prematurity-related cerebellar injury. However, hypotonia and delayed motor development are common in this population (Limperopoulos et al. 2007; Messerschmidt et al. 2008; Tam et al. 2011) and, in the current study, there was a significant association between sensorimotor cortex volumes and gross motor disabilities.
In our study, there were several unexpected findings. In the mature brain, the posterior parietal cortex plays an important role in visuo-spatial analysis, focused attention, and vigilance, with injury to these areas associated with visuo-spatial integration deficits, as well as agnosia, apraxia, and language dysfunction (Giovagnoli et al. 2009; Gesierich et al. 2012; Chechlacz et al. 2012; Tankus and Fried 2012). Somewhat unexpectedly, we found no significant association in our current study between volumes of the parietal cortex and functional outcome. Potential reasons for this are discussed below. Likewise, in our study population, the lateralization of the initial cerebellar injury had no significant impact on specific long-term outcome measures. The converse is true in more mature subjects with cerebellar stroke or tumor resection (Beebe et al. 2005), in whom, for example, lesions of the right cerebellar hemisphere are associated with disturbed verbal and literacy skills, while left cerebellar lesions result in nonverbal and visuo-spatial deficits (Scott et al. 2001). The intriguing lack of such lateralizing effects in our study requires further investigation, but likely relates to the early nature of the immature cerebellar injury prior to maturation of cerebellocerebral connectivity, as well as other incompletely understood plasticity factors.
The cerebral cortex and cerebellum of the mature brain are connected by a myriad, closed-loop circuit, with feed-forward and feed-back limbs, forming distinct functional and structural units. The feed-forward limb of each closed-loop projects to a discrete locus in the cerebellum from a specific region of the cerebral cortex, including the premotor, prefrontal, oculomotor, primary motor, and posterior parietal regions (Lynch et al. 1994; Middleton and Strick 1994, 2001; Clower et al. 2001). These cerebral cortical regions in turn become the target of feed-back projection from the principal cerebellar output center, the dentate nucleus (Middleton and Strick 1998). The manner in which the cerebellum effects neurologic function within the context of these loops is less clear. However, several important features support its role as a coordinating and integrating center that modulates rather than generates neural activity (Schmahmann and Pandya 1997a). First, the cerebellum receives afferents from a broad range of functionally diverse regions of the cerebral cortex (Schmahmann and Pandya 1993, 1997b; Clower et al. 2001; Kelly and Strick 2003; Schmahmann 2004). Secondly, the intrinsic circuitry is remarkably uniform across the cerebellar cortex, which suggests a common computational function or “universal cerebellar transform” (Schmahmann 2004), rather than a regional functional specialization of the cerebellar cortex. Finally, the number of inputs to the cerebellum far outnumbers the number of efferents, supporting its role as a functional integration center (Gottwald et al. 2004). Taken together, these features suggest that the functional impact of injury to the mature cerebellum is related more to its connectivity to extracerebellar regions (Bloedel et al. 1993; Schmahmann and Sherman 1998; Ramnani 2006; Ito 2008), rather than to the intrinsic functional topography of the cerebellum itself. In this paradigm, injury to the mature cerebellum would cause a functional disconnection of the cerebellum releasing it from its modulating influence on activity in specific projection areas in the cerebral cortex. Our data suggest that injury to the immature cerebellum may impact neurologic function through mechanisms that disrupt subsequent development of remote regions of the cerebral cortex.
Another interesting observation in our study was the gender distribution of our cohort in which 70% were male. Several previous studies (Reiss et al. 2004; van Kooij et al. 2011; Kent et al. 2012; Peacock et al. 2012) have suggested that the incidence of, and response to, prematurity-related brain injury is affected by male gender. In our own earlier studies, we described a significantly greater prevalence of cerebellar hemorrhagic injury among premature males versus females (Limperopoulos, Benson, et al. 2005). Thus, the significantly greater percentage of males in this study reflects the male predilection to the initial injury. Although the subsequent local and remote developmental responses to this initial injury might be influenced by gender, the current study is unable to address this question. It is the focus of ongoing studies in this population.
Our findings have several important implications. First, they provide further support that the long-term neurodevelopmental consequences of injury to the immature brain are due not only to the initial encephaloclastic injury, but also the effects of injury on subsequent brain development. This also calls into question the concept of acquired brain injury as “static” in these infants, given that the remote effects of primary cerebellar injury may continue to influence cerebral development over months to years. Our study focused on the remote functional effects of primary cerebellar injury. However, similar mechanisms are likely to operate following any prematurity-related brain lesions, including periventricular leucomalacia and periventricular hemorrhagic infarction. Furthermore, the current window for preventing primary brain injury in this population is narrow to nonexistent. However, if the secondary delayed effects on brain development are occurring over prolonged periods during which these children are in our care, it is reasonable to expect that future therapeutic interventions may decrease or prevent these secondary mechanisms of disrupted brain development.
Several potential limitations of this study are worthy of note. First, although the Talairach parcellation scheme (Peterson et al. 2000) used in our study has provided valuable insights in the current and in previous studies (Peterson et al. 2003; Thompson et al. 2007; Limperopoulos et al. 2010; Bolduc et al. 2011), the relatively large size of the parieto-occipital compartment in this scheme may have compromised sensitivity to volumetric changes in discrete cerebellar projection areas of the parietal cortex. Although cerebral gray and white matter segmentations and parcellations were performed automatically, subcortical gray matter and cerebellar volumes were carried out manually, which may be a limitation despite our very high intrarater reliability coefficients (0.96 for both structures). In addition, since we did not perform more extensive cerebellar parcellations, we have been limited in our ability to relate specific regions of cerebellar injury to specific functional deficits. Unlike the lesions in the studies of mature subjects (territorial strokes or surgical tumor removal), prematurity-related cerebellar lesions have a prominent hemorrhagic component, often with a major disruption of subsequent cerebellar development, seriously distorting the anatomic landmarks used to parcellate the cerebellum. In recognition of this limitation, we confined our analyses to overall measures of left or right cerebellar volume, or their sum as total cerebellar volume. Finally, give the relatively young age of our cohort and the wide age range at testing (18–63 months), we were unable to further discretely examine the relationship between cortical development and high-order cognitive and social–behavioral functions (e.g., executive function, cognitive–affective disturbances, autism spectrum disorders) that have been described in older children and adults, given that these functions have yet to solidify in preschool-aged children. Long-term follow-up at school age, including formal autism diagnostic testing is currently underway to address this intriguing question.
In conclusion, our study describes for the first time an association between secondary developmental impairment of the cerebral cortex and the known functional disabilities described in survivors of prematurity-related cerebellar injury (Limperopoulos et al. 2007; Messerschmidt et al. 2008). We propose that similar structure–function associations may result following other forms of injury to the immature developing brain. Since such evolving developmental disruption may unfold over months and years during which these children are in our direct care, and therefore at least in theory may become accessible to intervention, it appears imperative that concentrated efforts be made to address the questions raised by this study.
Funding
This work is supported by the Hearst Foundation and the National Institutes of Health (NINDS K24NS057568).
Notes
We thank Marine Bouyssi-Kobar and Cedric Clouchoux for their assistance with manuscript preparation. We are indebted to the children and families for their participation in this study. Conflict of Interest: None declared.
References
- Barbas H, Mesulam MM. Cortical afferent input to the principals region of the rhesus monkey. Neuroscience. 1985;15(3):619–637. doi: 10.1016/0306-4522(85)90064-8. [DOI] [PubMed] [Google Scholar]
- Beebe DW, Ris MD, Armstrong FD, Fontanesi J, Mulhern R, Holmes E, Wisoff JH. Cognitive and adaptive outcome in low-grade pediatric cerebellar astrocytomas: evidence of diminished cognitive and adaptive functioning in National Collaborative Research Studies (CCG 9891/POG 9130) J Clin Oncol. 2005;23(22):5198–5204. doi: 10.1200/JCO.2005.06.117. [DOI] [PubMed] [Google Scholar]
- Biran V, Bodiou AM, Zana E, Gaudin A, Farnoux C, Hovhannisyan S, Alison M, Elmaleh M, Oury JF, Maury L, et al. Cerebellar injury in premature infants less than 30 weeks of gestation. Arch Pediatr. 2011;18(3):261–266. doi: 10.1016/j.arcped.2010.12.016. [DOI] [PubMed] [Google Scholar]
- Bloedel JR, Bracha V, Larson PS. Real time operations of the cerebellar cortex. Can J Neurol Sci. 1993;20(Suppl 3):S7–S18. [PubMed] [Google Scholar]
- Bolduc ME, Du Plessis AJ, Evans A, Guizard N, Zhang X, Robertson RL, Limperopoulos C. Cerebellar malformations alter regional cerebral development. Dev Med Child Neurol. 2011;53(12):1128–1134. doi: 10.1111/j.1469-8749.2011.04090.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bystron I, Blakemore C, Rakic P. Development of the human cerebral cortex: Boulder Committee revisited. Nat Rev Neurosci. 2008;9(2):110–122. doi: 10.1038/nrn2252. [DOI] [PubMed] [Google Scholar]
- Cavada C, Goldman-Rakic PS. Posterior parietal cortex in rhesus monkey: II. Evidence for segregated corticocortical networks linking sensory and limbic areas with the frontal lobe. J Comp Neurol. 1989;287(4):422–445. doi: 10.1002/cne.902870403. [DOI] [PubMed] [Google Scholar]
- Chechlacz M, Rotshtein P, Hansen PC, Riddoch JM, Deb S, Humphreys GW. The neural underpinings of simultanagnosia: disconnecting the visuospatial attention network. J Cogn Neurosci. 2012;24(3):718–735. doi: 10.1162/jocn_a_00159. [DOI] [PubMed] [Google Scholar]
- Chugani HT, Phelps ME, Mazziotta JC. Positron emission tomography study of human brain functional development. Ann Neurol. 1987;22(4):487–497. doi: 10.1002/ana.410220408. [DOI] [PubMed] [Google Scholar]
- Clower DM, West RA, Lynch JC, Strick PL. The inferior parietal lobule is the target of output from the superior colliculus, hippocampus, and cerebellum. J Neurosci. 2001;21(16):6283–6291. doi: 10.1523/JNEUROSCI.21-16-06283.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois J, Benders M, Borradori-Tolsa C, Cachia A, Lazeyras F, Ha-Vinh Leuchter R, Sizonenko SV, Warfield SK, Mangin JF, Huppi PS. Primary cortical folding in the human newborn: an early marker of later functional development. Brain. 2008;131(Pt 8):2028–2041. doi: 10.1093/brain/awn137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyet LE, Kennea N, Counsell SJ, Maalouf EF, Ajayi-Obe M, Duggan PJ, Harrison M, Allsop JM, Hajnal J, Herlihy AH, et al. Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics. 2006;118(2):536–548. doi: 10.1542/peds.2005-1866. [DOI] [PubMed] [Google Scholar]
- Eblen F, Graybiel AM. Highly restricted origin of prefrontal cortical inputs to striosomes in the macaque monkey. J Neurosci. 1995;15(9):5999–6013. doi: 10.1523/JNEUROSCI.15-09-05999.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans AC, Collins DL, Mills SR, Brown ED, Kelly RL, Peters TM. 3D statistical neuroanatomical models from 305 MRI volumes. Proc IEEE Nucl Sci Symp Med Imaging Conf. 1993:1813–1817. [Google Scholar]
- Folio R, Fewell R. Peabody development motor scales and activity cards. Austin (TX): DLM Teaching Resources; 1983. [Google Scholar]
- Gesierich B, Jovicich J, Riello M, Adriani M, Monti A, Brentari V, Robinson SD, Wilson SM, Fairhall SL, Gorno-Tempini ML. Distinct neural substrates for semantic knowledge and naming in the temporoparietal network. Cereb Cortex. 2012;22(10):2217–2226. doi: 10.1093/cercor/bhr286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovagnoli AR, Aresi A, Reati F, Riva A, Gobbo C, Bizzi A. The neuropsychological and neuroradiological correlates of slowly progressive visual agnosia. Neurol Sci. 2009;30(2):123–131. doi: 10.1007/s10072-009-0019-9. [DOI] [PubMed] [Google Scholar]
- Gottwald B, Wilde B, Mihajlovic Z, Mehdorn HM. Evidence for distinct cognitive deficits after focal cerebellar lesions. J Neurol Neurosurg Psychiatry. 2004;75(11):1524–1531. doi: 10.1136/jnnp.2003.018093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelmann K, Hagberg G, Beckung E, Hagberg B, Uvebrant P. The changing panorama of cerebral palsy in Sweden. IX. Prevalence and origin in the birth-year period 1995–1998. Acta Paediatr. 2005;94(3):287–294. doi: 10.1111/j.1651-2227.2005.tb03071.x. [DOI] [PubMed] [Google Scholar]
- Hoekstra RE, Ferrara TB, Couser RJ, Payne NR, Connett JE. Survival and long-term neurodevelopmental outcome of extremely premature infants born at 23–26 weeks’ gestational age at a tertiary center. Pediatrics. 2004;113(1 Pt 1):e1–e6. doi: 10.1542/peds.113.1.e1. [DOI] [PubMed] [Google Scholar]
- Ito M. Control of mental activities by internal models in the cerebellum. Nat Rev Neurosci. 2008;9(4):304–313. doi: 10.1038/nrn2332. [DOI] [PubMed] [Google Scholar]
- Kelly RM, Strick PL. Cerebellar loops with motor cortex and prefrontal cortex of a nonhuman primate. J Neurosci. 2003;23(23):8432–8444. doi: 10.1523/JNEUROSCI.23-23-08432.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent AL, Wright IM, Abdel-Latif ME New South Wales and Australian Capital Territory Neonatal Intensive Care Units Audit Group. Mortality and adverse neurologic outcomes are greater in preterm male infants. Paediatrics. 2012;129(1):124–131. doi: 10.1542/peds.2011-1578. [DOI] [PubMed] [Google Scholar]
- Kesler SR, Reiss AL, Vohr B, Watson C, Schneider KC, Katz KH, Maller-Kesselman J, Silbereis J, Constable RT, Makuch RW, et al. Brain volume reductions within multiple cognitive systems in male preterm children at age twelve. J Pediatr. 2008;152(4):513–520. doi: 10.1016/j.jpeds.2007.08.009. 520 e511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levisohn L, Cronin-Golomb A, Schmahmann JD. Neuropsychological consequences of cerebellar tumour resection in children: cerebellar cognitive affective syndrome in a paediatric population. Brain. 2000;123(Pt 5):1041–1050. doi: 10.1093/brain/123.5.1041. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Bassan H, Gauvreau K, Robertson RL, Jr, Sullivan NR, Benson CB, Avery L, Stewart J, Soul JS, Ringer SA, et al. Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors? Pediatrics. 2007;120(3):584–593. doi: 10.1542/peds.2007-1041. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Bassan H, Sullivan NR, Soul JS, Robertson RL, Jr, Moore M, Ringer SA, Volpe JJ, du Plessis AJ. Positive screening for autism in ex-preterm infants: prevalence and risk factors. Pediatrics. 2008;121(4):758–765. doi: 10.1542/peds.2007-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limperopoulos C, Benson CB, Bassan H, Disalvo DN, Kinnamon DD, Moore M, Ringer SA, Volpe JJ, du Plessis AJ. Cerebellar hemorrhage in the preterm infant: ultrasonographic findings and risk factors. Pediatrics. 2005;116(3):717–724. doi: 10.1542/peds.2005-0556. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Chilingaryan G, Guizard N, Robertson RL, Du Plessis AJ. Cerebellar injury in the premature infant is associated with impaired growth of specific cerebral regions. Pediatr Res. 2010;68(2):145–150. doi: 10.1203/PDR.0b013e3181e1d032. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Soul JS, Haidar H, Huppi PS, Bassan H, Warfield SK, Robertson RL, Moore M, Akins P, Volpe JJ, et al. Impaired trophic interactions between the cerebellum and the cerebrum among preterm infants. Pediatrics. 2005;116(4):844–850. doi: 10.1542/peds.2004-2282. [DOI] [PubMed] [Google Scholar]
- Lynch JC, Hoover JE, Strick PL. Input to the primate frontal eye field from the substantia nigra, superior colliculus, and dentate nucleus demonstrated by transneuronal transport. Exp Brain Res. 1994;100(1):181–186. doi: 10.1007/BF00227293. [DOI] [PubMed] [Google Scholar]
- Maddalena P, Gibbins S. Cerebellar hemorrhage in extremely low birth weight infants: incidence, risk factors, and impact on long-term outcomes. Neonatal Netw. 2008;27(6):387–396. doi: 10.1891/0730-0832.27.6.387. [DOI] [PubMed] [Google Scholar]
- McCarthy LK, Donoghue V, Murphy JF. Ultrasonically detectable cerebellar haemorrhage in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2011;96(4):F281–F285. doi: 10.1136/adc.2010.183889. [DOI] [PubMed] [Google Scholar]
- Messerschmidt A, Fuiko R, Prayer D, Brugger PC, Boltshauser E, Zoder G, Sterniste W, Weber M, Birnbacher R. Disrupted cerebellar development in preterm infants is associated with impaired neurodevelopmental outcome. Eur J Pediatr. 2008;167(10):1141–1147. doi: 10.1007/s00431-007-0647-0. [DOI] [PubMed] [Google Scholar]
- Middleton FA, Strick PL. Anatomical evidence for cerebellar and basal ganglia involvement in higher cognitive function. Science. 1994;266(5184):458–461. doi: 10.1126/science.7939688. [DOI] [PubMed] [Google Scholar]
- Middleton FA, Strick PL. Cerebellar projections to the prefrontal cortex of the primate. J Neurosci. 2001;21(2):700–712. doi: 10.1523/JNEUROSCI.21-02-00700.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Middleton FA, Strick PL. The cerebellum: an overview. Trends Neurosci. 1998;21(9):367–369. doi: 10.1016/s0166-2236(98)01330-7. [DOI] [PubMed] [Google Scholar]
- Msall ME. Neurodevelopmental surveillance in the first 2 years after extremely preterm birth: evidence, challenges, and guidelines. Early Hum Dev. 2006;82(3):157–166. doi: 10.1016/j.earlhumdev.2005.12.016. [DOI] [PubMed] [Google Scholar]
- Mullen E. Mullen scales of early learning. Circle Pines (MN): American Guidance Services, Inc; 1995. [Google Scholar]
- Peacock JL, Marston L, Marlow N, Calvert SA, Greenough A. Neonatal and infant outcome in boys and girls born very prematurely. Pediatr Res. 2012;71(3):305–310. doi: 10.1038/pr.2011.50. [DOI] [PubMed] [Google Scholar]
- Peterson BS, Anderson AW, Ehrenkranz R, Staib LH, Tageldin M, Colson E, Gore JC, Duncan CC, Makuch R, Ment LR. Regional brain volumes and their later neurodevelopmental correlates in term and preterm infants. Pediatrics. 2003;111(5 Pt 1):939–948. doi: 10.1542/peds.111.5.939. [DOI] [PubMed] [Google Scholar]
- Peterson BS, Vohr B, Staib LH, Cannistraci CJ, Dolberg A, Schneider KC, Katz KH, Westerveld M, Sparrow S, Anderson AW, et al. Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA. 2000;284(15):1939–1947. doi: 10.1001/jama.284.15.1939. [DOI] [PubMed] [Google Scholar]
- Ramnani N. The primate cortico-cerebellar system: anatomy and function. Nat Rev Neurosci. 2006;7(7):511–522. doi: 10.1038/nrn1953. [DOI] [PubMed] [Google Scholar]
- Reiss AL, Kesler SR, Vohr B, Duncan CC, Katz KH, Pajot S, Schneider KC, Makuch RW, Ment LR. Sex differences in cerebral volumes of 8-year-olds born preterm. J Pediatr. 2004;145(2):242–249. doi: 10.1016/j.jpeds.2004.04.031. [DOI] [PubMed] [Google Scholar]
- Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31:131–144. doi: 10.1023/a:1010738829569. [DOI] [PubMed] [Google Scholar]
- Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16(3):367–378. doi: 10.1176/jnp.16.3.367. [DOI] [PubMed] [Google Scholar]
- Schmahmann JD, Pandya DN. Anatomic organization of the basilar pontine projections from prefrontal cortices in rhesus monkey. J Neurosci. 1997b;17(1):438–458. doi: 10.1523/JNEUROSCI.17-01-00438.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmahmann JD, Pandya DN. The cerebrocerebellar system. Int Rev Neurobiol. 1997a;41:31–60. doi: 10.1016/s0074-7742(08)60346-3. [DOI] [PubMed] [Google Scholar]
- Schmahmann JD, Pandya DN. Prelunate, occipitotemporal, and parahippocampal projections to the basis pontis in rhesus monkey. J Comp Neurol. 1993;337(1):94–112. doi: 10.1002/cne.903370107. [DOI] [PubMed] [Google Scholar]
- Schmahmann JD, Pandya DN. Projections to the basis pontis from the superior temporal sulcus and superior temporal region in the rhesus monkey. J Comp Neurol. 1991;308(2):224–248. doi: 10.1002/cne.903080209. [DOI] [PubMed] [Google Scholar]
- Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998;121(Pt 4):561–579. doi: 10.1093/brain/121.4.561. [DOI] [PubMed] [Google Scholar]
- Scott RB, Stoodley CJ, Anslow P, Paul C, Stein JF, Sugden EM, Mitchell CD. Lateralized cognitive deficits in children following cerebellar lesions. Dev Med Child Neurol. 2001;43(10):685–691. doi: 10.1017/s0012162201001232. [DOI] [PubMed] [Google Scholar]
- Smith GC, Gutovich J, Smyser C, Pineda R, Newnham C, Tjoeng TH, Vavasseur C, Wallendorf M, Neil J, Inder T. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann Neurol. 2011;70(4):541–549. doi: 10.1002/ana.22545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steggerda SJ, Leijser LM, Wiggers-de Bruine FT, van der Grond J, Walther FJ, van Wezel-Meijler G. Cerebellar injury in preterm infants: incidence and findings on US and MR images. Radiology. 2009;252(1):190–199. doi: 10.1148/radiol.2521081525. [DOI] [PubMed] [Google Scholar]
- Tam EW, Rosenbluth G, Rogers EE, Ferriero DM, Glidden D, Goldstein RB, Glass HC, Piecuch RE, Barkovich AJ. Cerebellar hemorrhage on magnetic resonance imaging in preterm newborns associated with abnormal neurologic outcome. J Pediatr. 2011;158(2):245–250. doi: 10.1016/j.jpeds.2010.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tankus A, Fried I. Visuomotor coordination and motor representation by human temporal lobe neurons. J Cogn Neurosci. 2012;24(3):600–610. doi: 10.1162/jocn_a_00160. [DOI] [PubMed] [Google Scholar]
- Tavano A, Grasso R, Gagliardi C, Triulzi F, Bresolin N, Fabbro F, Borgatti R. Disorders of cognitive and affective development in cerebellar malformations. Brain. 2007;130(Pt 10):2646–2660. doi: 10.1093/brain/awm201. [DOI] [PubMed] [Google Scholar]
- Thompson DK, Warfield SK, Carlin JB, Pavlovic M, Wang HX, Bear M, Kean MJ, Doyle LW, Egan GF, Inder TE. Perinatal risk factors altering regional brain structure in the preterm infant. Brain. 2007;130(Pt 3):667–677. doi: 10.1093/brain/awl277. [DOI] [PubMed] [Google Scholar]
- van Kooij BJ, van Pul C, Benders MJ, van Haastert IC, de Vries LS, Groenendaal F. Fiber tracking at term displays gender differences regarding cognitive and motor outcome at 2 years of age in preterm infants. Pediatr Res. 2011;70(6):626–32. doi: 10.1203/PDR.0b013e318232a963. [DOI] [PubMed] [Google Scholar]
- Volpe JJ. Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 2009;8(1):110–124. doi: 10.1016/S1474-4422(08)70294-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijdenbos AP, Dawant BM. Brain segmentation and white matter lesion detection in MR images. Crit Rev Biomed Eng. 1994;22(5–6):401–465. [PubMed] [Google Scholar]