Abstract
Background: Median survival in patients with unresectable locally advanced pancreatic cancer lies in the range of 9–15 months. Radiofrequency ablation (RFA) may prolong survival, but data on its safety and efficacy are scarce.
Methods: A systematic literature search was performed in PubMed, EMBASE and the Cochrane Library with the syntax ‘(radiofrequency OR RFA) AND (pancreas OR pancreatic)’ for studies published until 1 January 2012. In addition, a search of the proceedings of conferences on pancreatic disease that took place during 2009–2011 was performed. Studies with fewer than five patients were excluded as they were considered to be case reports. The primary endpoint was survival. Secondary endpoints included morbidity and mortality.
Results: Five studies involving a total of 158 patients with pancreatic cancer treated with RFA fulfilled the eligibility criteria. These studies reported median survival after RFA of 3–33 months, morbidity related to RFA of 4–37%, mortality of 0–19% and overall morbidity of 10–43%. Pooling of data was not appropriate as the study populations and reported outcomes were heterogeneous. Crucial safety aspects included ensuring a maximum RFA tip temperature of < 90 °C and ensuring minimum distances between the RFA probe and surrounding structures.
Conclusions: Radiofrequency ablation seems to be feasible and safe when it is used with the correct temperature and at an appropriate distance from vital structures. It appears to have a positive impact on survival. Multicentre randomized trials are necessary to determine the true effect size of RFA and to minimize the impacts of selection and publication biases.
Introduction
Pancreatic cancer is the fourth leading cause of cancer-related death in Western societies.1 At the time of diagnosis, 20% of patients present with a resectable tumour, 40% with an unresectable locally advanced tumour and 40% with metastatic disease.2,3 After resection, 5-year overall survival rates are 17–24%.4 Median survival in patients with unresectable locally advanced pancreatic cancer lies in the range of 9–15 months, whereas in patients with distant metastasis, median survival is 6 months.4,5
In patients with unresectable locally advanced pancreatic cancer, chemotherapy and radiotherapy provide minimal survival benefits. Gemcitabine gives a modest survival benefit of 3 months and trials on chemoradiation therapy show a marginal effect.6,7 Therefore, there is a clear need for novel, effective therapies in these patients.
Radiofrequency ablation (RFA) has been proposed as a new treatment option for unresectable locally advanced pancreatic cancer. This treatment may lead to prolonged survival, but data on its safety and efficacy are scarce. The aim of this systematic review was to evaluate the safety and survival benefit of RFA in unresectable locally advanced pancreatic cancer.
Materials and methods
A systematic literature search was performed in PubMed, EMBASE and the Cochrane Library for studies published in English up to 1 January 2012. In addition, a search of the proceedings of conferences on pancreatic disease (European Pancreatic Club, Pancreas Club, International Hepato-Pancreato-Biliary Association) in 2009, 2010 and 2011 was performed. Search terms were (radiofrequency OR RFA) AND (pancreas OR pancreatic), and were restricted to the title, abstract and keywords. All titles and abstracts of studies identified in the initial search were screened to identify those reporting on patients with unresectable locally advanced pancreatic cancer undergoing RFA. Subsequently, full-text papers of the selected studies were screened independently by two authors to assess eligibility.
Inclusion criteria required the study population to consist of patients with unresectable locally advanced pancreatic cancer defined as stage III according to the American Joint Committee on Cancer (AJCC) tumour–node–metastasis (TNM) classification, who underwent a surgical RFA procedure. Exclusion criteria ruled out any study with a very small cohort (fewer than five patients) and any study reporting on RFA of tumours other than pancreatic adenocarcinoma. All cross references were screened for potentially relevant studies not identified in the initial literature search.
Data extraction
The following variables were extracted, where available, from the included articles: number of patients; demographic data (sex and age); extent of disease; RFA device used; RFA temperature used; distance of the RFA probe from surrounding structures; number of RFA probes used; duration of ablation; power at which the ablation was performed; number of ablations/number of passes of the probe; whether cooling was used, and the way cooling was generated.
Results
The results of the literature search are summarized in Fig. 1. Of 29 articles reporting on RFA of unresectable locally advanced pancreatic cancer, 22 were excluded for the following reasons: using a cohort of fewer than five patients (seven studies); using pain as an outcome rather than survival, morbidity and mortality (one study); describing a review or overview of the technique (four studies); describing RFA combined with intraoperative 125-iodine seed implantation influencing outcome (one study); describing tumours other than pancreatic adenocarcinoma (four studies); describing a non-surgical RFA procedure (one study); being written in a language other than English (three studies), and comprising a letter to the editor (one study). The remaining seven studies were considered eligible. However, of these seven studies,8–10 three reported results in overlapping cohorts. For this reason, two studies were excluded although they had been appraised as eligible.8–10,12–15 The remaining five studies were included in the present review.8–15 Four studies were prospective cohort studies10,12,14,15 and one study was a retrospective cohort study.13 The characteristics of the five included studies are summarized in Table 1.
Figure 1.
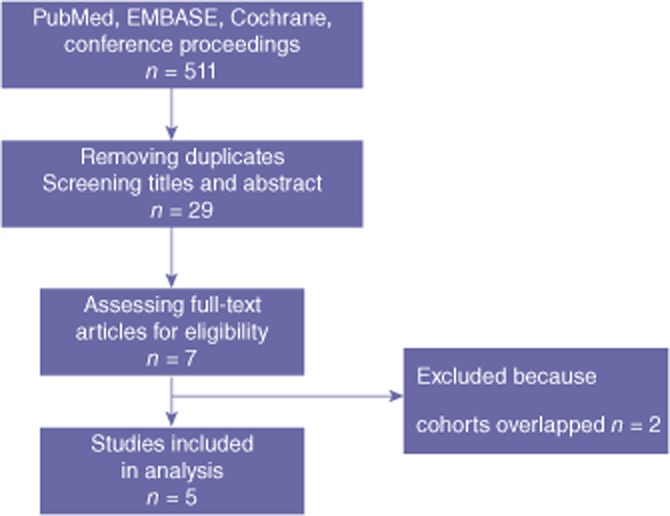
Study selection
Table 1.
Study characteristics
| Authors | Year | Patients, n | Study design | RFA device | RFA temperature | Distance of RFA probea, mm | RFA duration, min | Power | Ablations, n | Cooling with saline |
|---|---|---|---|---|---|---|---|---|---|---|
| Girelli et al.10 | 2011 | 100 | Prospective cohort | Rita | 90 °C | 5–10 | 5–10 | 250 | 1–2 | Area Duodenum, vena cava |
| Singh et al.12 | 2011 | 10 | Prospective cohort | Berchtold | – | – | – | 40–60 | – | – |
| Spiliotis et al.13 | 2007 | 12 | Retrospective cohort | Radionics | 90 °C | – | 5–7 | – | 1–3 | Area |
| Wu et al.14 | 2006 | 16 | Prospective cohort | Radionics | 30–90 °C | 5 | 12 and 1b | 0–200 | 2–5 | – |
| Matsui et al.15 | 2000 | 20 | Prospective cohort | Omron | 50 °C | – | 15 | 500 | 1–15 | – |
Distance of RFA probe from duodenum or portomesenteric vessels.
12 min at 30 °C and 1 min at 90 °C.
RFA, radiofrequency ablation.
Patient characteristics
The five studies included a total of 158 patients who underwent RFA for unresectable ductal pancreatic adenocarcinoma. The number of patients per study ranged from 10 to 100. Patient characteristics are summarized in Table 2. The male : female ratio in the pooled data was 1.3 : 1. Ages ranged between 45 years and 72 years. Radiofrequency ablation was performed in 138 patients with stage III locally advanced pancreatic cancer and in 20 patients with metastatic pancreatic disease.
Table 2.
Patient characteristics
| Authors | Year | Patients, n | Male/female, n | Age, years | Extent of disease, n | |
|---|---|---|---|---|---|---|
| Locally advanced | Metastatic | |||||
| Girelli et al.10 | 2011 | 100 | 55/45 | Median: 64 | 100 | – |
| Singh et al.12 | 2011 | 10 | – | Range: 45–72 | 10 | – |
| Spiliotis et al.13 | 2007 | 12 | 6/6 | Median: 66 | 8 | 4 |
| Wu et al.14 | 2006 | 16 | 10/6 | Median: 67 | 11 | 5 |
| Matsui et al.15 | 2000 | 20 | 12/8 | Median: 59 | 9 | 11 |
Characteristics of RFA
The characteristics of the 158 RFA procedures are summarized in Table 1. In two studies,13,14 an RFA device manufactured by Radionics, Inc. (Burlington, MA, USA) was used. One study12 used a generator manufactured by Berchtold GmbH & Co. KG (Tuttlingen, Germany), one study15 used a generator manufactured by Omron Co. Ltd (Kyoto, Japan) and one study10 used a Generator 1500X manufactured by Rita Medical Systems, Inc. (Mountain View, CA, USA). Four studies10.13–15 reported the RFA temperature used; in two studies,10,13 a temperature of 90 °C was used during the whole RFA procedure. In one study,14 RFA was performed for 12 min at a temperature of 30 °C and for 1 min at a temperature of 90 °C. In one study,15 an RFA temperature of 50 °C was used during the whole procedure. Only two studies10,14 reported the distance of the RFA probe from surrounding structures. In one study15 the distance of the RFA probe was 10 mm from the duodenum and 5 mm from the portomesenteric vessels. In the other study,10 RFA was performed only at the site of the portomesenteric vessels at a distance of 5 mm. The duration of ablation was reported in four studies10,13–15 and varied in all of them, ranging from 5 min to 15 min. The power at which RFA was performed was reported in four studies10,12,14,15 and also varied across studies,10,13–15 ranging from 40 W to 500 W. Four studies reported the number of passes of the RFA probe, which ranged from 1 to 15. The use of cooling was reported in two studies.10,13 In one study,10 the RFA area was cooled with cold saline administered directly with a syringe, a cold wet gauze was placed over the inferior vena cava to protect it from heat and the duodenum was perfused continuously with cold saline solution through a nasogastric tube placed in the second part of the duodenum. In the other study,10 only the ablation area was cooled with cold saline.
Morbidity and mortality
The outcomes as reported in the studies are shown in Table 3. Rates of RFA-related morbidity ranged from 10% to 37%. Complications related to RFA included pancreatic fistulae, portal vein thrombosis, gastrointestinal bleeding and acute pancreatitis. Rates of RFA-related mortality ranged from 0% to 19%. The RFA-related complications that resulted in patient deaths included gastrointestinal bleeding and sepsis. Rates of overall complications ranged from 10% to 43%. The types of complication reported varied widely and included pneumonia, peritoneal cavity abscess, acute renal failure, transient ascites, hepatic insufficiency, pseudomembrane colitis, haemoperitoneum, abdominal fluid collection, gastric bypass fistula, gastric ulcer and choledocholithiasis.
Table 3.
Radiofrequency ablation (RFA)-related morbidity, mortality and survival after RFA
| Authors | Year | Patients, n | Extent of disease, n | Bypass surgery, n | Overall complications | RFA-related morbidity | RFA-related mortality | Median survival, months | |
|---|---|---|---|---|---|---|---|---|---|
| Locally advanced | Metastatic | ||||||||
| Girelli et al.10 | 2011 | 100 | 100 | – | 53 | 26% | 15% | 3% | 20 |
| Singh et al.12 | 2011 | 10 | 10 | – | 0 | 10% | 10% | 0% | 9–36 |
| Spiliotis et al.13 | 2007 | 12 | 8 | 4 | 12 | 25% | 16% | 0% | 33 |
| Wu et al.14 | 2006 | 16 | 11 | 5 | 2 | 43% | 37% | 19% | – |
| Matsui et al.15 | 2000 | 20 | 9 | 11 | – | 10% | 10% | 5% | 3 |
Survival
One of the five studies14 included did not report survival after RFA. Of the remaining four studies, three10,13,15 reported median survival and one12 reported the range of survival.
Median survival after RFA in patients with stage III unresectable locally advanced pancreatic cancer ranged from 20 months to 33 months. The study12 that reported survival lengths rather than median survival cited a range of 9–36 months. One study15 reported median survival in patients with unresectable locally advanced pancreatic cancer and patients with metastatic pancreatic disease without stratifying the data for the respective patient groups; median survival in this study was 3 months.
Discussion
This study reviewed the safety and survival benefits of RFA of locally advanced pancreatic cancer. Radiofrequency ablation appears to be an attractive treatment for locally advanced pancreatic cancer. Rates of RFA-related morbidity ranged from 10% to 37%. Rates of RFA-related mortality ranged from 0% to 19%. Median survival after RFA in patients with stage III locally advanced pancreatic cancer lay in the range of 20–33 months. One study12 did not report median survival, but cited a range of survival of 9–36 months. One study15 reported a median survival of 3 months after RFA in a combined sample of patients with unresectable locally advanced pancreatic cancer and patients with distant metastases.
The study by Wu et al. reported the highest rates of RFA-related morbidity (38%, 6 of 16 patients) and mortality (19%, 3 of 16 patients).14 In this study, RFA was applied at a distance of 5 mm from the portomesenteric vessels in 16 patients with locally advanced pancreatic cancer. Three patients developed a pancreatic fistula which healed smoothly within 10 days, and three patients had massive gastrointestinal bleeding as a result of portal vein thrombosis leading to portal hypertension. The three patients with massive gastrointestinal bleeding all died, resulting in an RFA-related mortality rate of 19%. Wu et al. reported that a minimum distance of 5 mm between the RFA site and major peripancreatic vessels might not be enough to avoid injury to the major peripancreatic vessels.14
The largest series, reported by Girelli et al.,10 cited an RFA-related morbidity of 15% and an RFA-related mortality of 3% in 100 patients with unresectable locally advanced pancreatic cancer.8–11 Girelli et al.8 treated the first 25 patients with RFA at a temperature of 105 °C; at this temperature a high complication rate was seen.8–10 Thereafter, the authors decreased the RFA temperature to 90 °C, resulting in a significant reduction in the rate of complications, particularly in rates of mesenteric and portal thrombosis, which represent typical thermal vein damage,8 and duodenal damage.11 In the study by Singh et al., no major procedure-related morbidity or mortality occurred; one patient developed a 2-cm asymptomatic pseudocyst.12 Spiliotis et al. reported biliary leak after RFA in two patients.13 Matsui et al. reported cyst formation in two patients and the development of an abscess in the peritoneal cavity in one patient, who died of sepsis 21 days after treatment.15
With respect to survival after RFA, the largest series, that reported by Girelli et al., cited a median survival of 20 months.10 In this study, half of the patients were treated first with RFA and then with radiochemotherapy or systemic or intra-arterial chemotherapy or a combination of all of these. In the other half of the patients, RFA was performed after other primary treatments (radiochemotherapy or systemic or intra-arterial chemotherapy or a combination of all of these). This may have led to a selection bias in some patients who received second-line RFA, who must have benefited from an earlier treatment in order to receive RFA later.10 Spiliotis et al. reported a median survival of 33 months after RFA.13 This study included patients with either stage III or IV pancreatic cancer. Patients with stage III unresectable locally advanced pancreatic cancer receiving RFA were all alive at the time of publication of the study and reached a maximum survival of 38 months.13 Singh et al. reported survival after RFA in the range of 9–36 months.12 Of the 10 patients included, 8 received post-RFA chemotherapy.12 Matsui et al. reported a median survival of 3 months.15 However, their series included 11 patients with distant metastases and 9 patients with unresectable locally advanced pancreatic cancer and did not stratify for the two different groups. As most of these patients had distant metastases, the survival benefit of RFA in patients with unresectable locally advanced pancreatic cancer may be underestimated in this study.15
The largest series reported in this review was that of Girelli et al.10 However, that the other smaller studies reported comparable results is important because it shows that the data were reproducible in other centres. In most studies, rates of RFA-related morbidity lay in the range of 10–15%, mortality in the range of 0–5% and overall complications in the range of 10–26% (Table 3). The only exception to this concerns the study by Wu et al., which showed RFA-related morbidity of 37%, mortality of 19% and overall complications of 43%.14 Wu et al. demonstrated the importance of distance as they performed RFA at a distance of 5 mm from major peripancreatic vessels.14 Radiofrequency ablation at this distance resulted in a higher complication rate. With respect to survival, the results of the studies are similarly comparable, other than those observed in the study by Matsui et al.,15 which included both stage III and stage IV patients. This indicates that stage IV patients should not be treated with RFA.
The studies reviewed show that there are some important factors for safety. To prevent the occurrence of complications, the temperature at which RFA is performed should not exceed a maximum of 90 °C. Moreover, the distance between the RFA probe and surrounding structures should be > 5 mm with reference to the portomesenteric vessels and > 10 mm with reference to the duodenum. Furthermore, thermal damage to the duodenum can be prevented by intraluminal duodenal cooling.
Although the studies reviewed here appear to show RFA to be an attractive treatment option in unresectable locally advanced pancreatic cancer, this review is subject to some limitations. Patient populations across the different studies were heterogeneous; some studies included patients with either stage III or stage IV disease, and pre-and post-RFA treatments differed across studies and within each study. Another limitation refers to the fact that the RFA devices and RFA settings (temperature, ablation duration, power etc.) used in the various studies differed. Because of these limitations, it was not appropriate to pool the data. Furthermore, there are no randomized controlled trials (RCTs) of RFA in locally advanced pancreatic cancer.
In conclusion, RFA is a feasible and safe procedure when it is used with the right setting. Radiofrequency ablation in combination with chemotherapy and/or radiotherapy may have a positive impact on survival. A large, multicentre RCT is necessary to determine the true effect size of RFA and to minimize the impact of selection and publication biases. Preparations for such a study are underway.
Acknowledgments
SF is supported by a grant from the Netherlands Organization for Scientific Research [Nederlandse Organisatie voor Wetenschappelijk Onderzoek (NWO)] (no. 017.007.133).
Conflicts of interest
None declared.
References
- 1.Spinelli GP, Zullo A, Romiti A, Di Seri M, Tomao F, Miele E, et al. Longterm survival in metastatic pancreatic cancer. A case report and review of the literature. J Pancreas. 2006;7:486–491. [PubMed] [Google Scholar]
- 2.Morganti AG, Massaccesi M, La Torre G, Caravatta L, Piscopo A, Tambaro R, et al. A systematic review of resectability and survival after concurrent chemoradiation in primarily unresectable pancreatic cancer. Ann Surg Oncol. 2010;17:194–205. doi: 10.1245/s10434-009-0762-4. [DOI] [PubMed] [Google Scholar]
- 3.Moss RA, Lee C. Current and emerging therapies for the treatment of pancreatic cancer. Oncol Targets Ther. 2010;3:111–127. doi: 10.2147/ott.s7203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cartwright T, Richards DA, Boehm KA. Cancer of the pancreas: are we making progress? A review of studies in the US Oncology Research Network. Cancer Control. 2008;15:308–313. doi: 10.1177/107327480801500405. [DOI] [PubMed] [Google Scholar]
- 5.Vincent A, Herman J, Schulick R, Hruban RH, Goggins M. Pancreatic cancer. Lancet. 2011;378:607–620. doi: 10.1016/S0140-6736(10)62307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu J, Zhao G, Wang HX, Tang L, Xu YC, Ma Y, et al. A meta-analysis of gemcitabine containing chemotherapy for locally advanced and metastatic pancreatic adenocarcinoma. J Hematol Oncol. 2011;4:1–15. doi: 10.1186/1756-8722-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loehrer PJ, Sr, Feng Y, Cardenes H, Wagner L, Brell JM, Cella D, et al. Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an Eastern Cooperative Oncology Group trial. J Clin Oncol. 2011;29:4105–4112. doi: 10.1200/JCO.2011.34.8904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Girelli R, Frigerio I, Salvia R, Barbi E, Tinazzi Martini P, Bassi C. Feasibility and safety of radiofrequency ablation for locally advanced pancreatic cancer. Br J Surg. 2010;97:220–225. doi: 10.1002/bjs.6800. [DOI] [PubMed] [Google Scholar]
- 9.Frigerio I, Alessandro G, Girelli R, Salvia R, Capelli P, Bassi C. Downstaging after radiofrequency ablation of stage III pancreatic cancer can lead to R0 resection. HPB. 2011;13(Suppl. 2):112–113. [Google Scholar]
- 10.Girelli R, Giardino A, Frigerio I, Salvia R, Partelli S, Bassi C. Survival after radiofrequency of stage III pancreatic carcinoma: a wind of change? HBP. 2011;13(Suppl. 2):15. [Google Scholar]
- 11.Cantore M, Girelli R, Mambrini A, Frigerio I, Boz G, Salvia R, et al. Combined modality treatment for patients with locally advanced pancreatic adenocarcinoma. Br J Surg. 2012;99:1083–1088. doi: 10.1002/bjs.8789. [DOI] [PubMed] [Google Scholar]
- 12.Singh V, Varshney S, Sewkani A, Varshney R, Deshpande G, Shaji P, et al. Radiofrequency ablation of unresectable pancreatic carcinoma: 10-year experience from single centre. Pancreatology. 2011;11(Suppl. 1):52. [Google Scholar]
- 13.Spiliotis JD, Datsis AC, Michalopoulos MV, Kekelos SP, Vaxevanidou A, Rogdakis AV, et al. Radiofrequency ablation combined with palliative surgery may prolong survival of patients with advanced cancer of the pancreas. Langenbecks Arch Surg. 2007;392:55–60. doi: 10.1007/s00423-006-0098-5. [DOI] [PubMed] [Google Scholar]
- 14.Wu Y, Tang Z, Fang H, Gao S, Chen J, Wang Y, et al. High operative risk of cool-tip radiofrequency ablation for unresectable pancreatic head cancer. J Surg Oncol. 2006;94:392–395. doi: 10.1002/jso.20580. [DOI] [PubMed] [Google Scholar]
- 15.Matsui Y, Nakagawa A, Kamiyama Y, Yamamoto K, Kubo N, Nakase Y. Selective thermocoagulation of unresectable pancreatic cancers by using radiofrequency capacitive heating. Pancreas. 2000;20:14–20. doi: 10.1097/00006676-200001000-00002. [DOI] [PubMed] [Google Scholar]


