Abstract
Introduction: A left lateral section is the first choice for a laparoscopic anatomic liver resection. The objective of this case–control study was to assess the surgical outcome after a laparoscopic left lateral resection for benign liver lesions compared with the open approach.
Methods: From January 2004 to April 2011, 31 laparoscopic left lateral resections were matched with 31 open left lateral resections by selection based on pathology of the lesion, size of the lesion, American Society of Anesthesiologists (ASA) grade, body mass index (BMI), age and gender of the patient.
Results: Duration of the operation (laparoscopic: 182 ± 71 versus open: 244 ± 105 min; P = 0.04), blood loss (223 ± 281 versus 455 ± 593 ml; P = 0.03), duration of hospital stay (4.1 ± 1.7 versus 8.1 ± 4.4 days; P < 0.001) and total cost of hospitalization (7475 ± 2679 versus 11504 ± 7776 Euros; P < 0.001) were significantly lower in the laparoscopic group.
Conclusions: This matched case–control study demonstrated procedural safety, excellent post-operative outcomes and economic benefits for a laparoscopic liver resection. A laparoscopic left lateral liver sectionectomy is recommended as a gold standard for benign liver lesions.
Introduction
Over the past two decades, laparoscopic surgery has evolved to become the standard approach for many abdominal procedures. The laparoscopic approach for a cholecystectomy was rapidly adopted around the world in the 1990s and now is the gold standard.1 Lesser pain, better cosmetic results, and a shorter hospital stay combined with decreased morbidity and mortality expanded the scope of laparoscopic procedures to hernia repair, splenectomy, adrenalectomy, antireflux surgery and bariatric surgery.2 Although the first laparoscopic liver resection was described by Reich et al. in 1991,3 the evolution of the laparoscopic liver resection has been considerably restricted. This may reflect the lack of expertise owing to the higher level of complexity involved in laparoscopic liver procedures or the limited dissemination of advanced laparoscopic techniques among a majority of liver surgeons.4 Of the procedures of liver resection, the left lateral segment of the liver is seen as the first choice for a laparoscopic anatomic resection because of its peripheral location, the thin parenchyma along the ligamentum venosum groove, the minimal requirement for hilar biliary dissection and easy control of the left hepatic vein with a vascular stapler. This case–control study evaluates a left lateral sectionectomy for benign liver tumours.
Patients and methods
From January 2004 to April 2011, 92 left lateral resections were performed in this department: 55 were open and 37 were done using the laparoscopic approach. Left lateral resections for the malignant indications and for living donor liver transplantation were excluded from both groups. Thirty-one laparoscopic left lateral liver resections for benign lesions were matched with 31 open left lateral resections for benign lesions by strict selection based on histopathology of the lesion, size of the lesion, American Society of Anesthesiologists (ASA) grade, body mass index (BMI), age and gender of the patient. In the matched group, the main reason for the open approach was the lack of experienced laparoscopic surgeons and these laparoscopic resections were mainly performed before 2008 (Fig. 1). For benign tumours, the indications for a resection were large adenoma (>5 cm), symptomatic haemangioma or a focal nodular hyperplasia (FNH) including pedunculated or large lesions with associated compression of adjacent organs. Some patients with FNH (n = 3) were operated with a false pre-operative diagnosis of adenoma, owing to the fat content (n = 2) or the absence of a central hypodense scar (n = 1) on imaging.5,6
Figure 1.
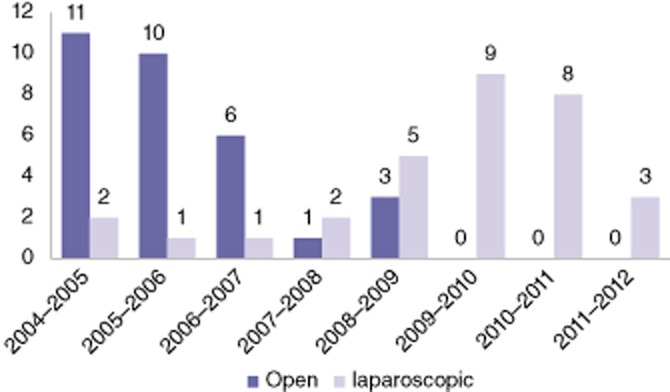
Distribution between an open and laparoscopic left lateral sectionectomy for benign liver lesions according to the year of resection
Data on the demographic profile, BMI, past medical history, ASA grade, pathology of the lesion, details of the operation, post-operative course and cost of the hospital stay were collected from a prospectively maintained database. Total costs of the procedure included the operating room component cost (operative time, anaesthesia and specific material) and hospital stay cost (room and board, and pharmacy).
A left lateral resection (sectionectomy) is defined as the resection of Couinaud’s segments 2 and 3. Post-operative complications were graded with the Clavien–Dindo classification.7 Operative mortality was defined as in-hospital death or death within 90 days of surgery.
Operative technique
Laparoscopic procedure
The patient was placed in a supine position, with the legs slightly abducted and the left arm tucked along the body. The surgeon stood between the legs and the assistant on the left side (Fig. 2). A pneumoperitoneum was created using an open technique. Generally four trocars (Fig. 2) were used and a 10-mm operating trocar was placed through the umbilicus, a 10-mm optical trocar for a 30 degree laparoscope was inserted in the left hypochondrium and two 5-mm trocars in the left subcostal area and the right hypochondrium for aspiration, traction and dissection. Hepatic pedicle control was not undertaken routinely and the falciform ligament was not sectioned, allowing the traction on the transection plane. The transection line was marked on the capsule using diathermy. The parenchymal transection was performed using an ultrasonic dissector (Dissectron; Satelec Medical, Merignac, France), and haemostasis and biliostasis were achieved with harmonic shears (Harmonic; Ethicon, Issy les Moulineaux, France) or bipolar cautery coagulation. After partial transection of the parenchyma, the portal pedicles of segments 3 and 2 were exposed and sectioned, respectively, with an endovascular stapler (45 mm, Ethicon Endosurgery; Johnson & Johnson, New Brunswick, NJ, USA) without any previous control in the hepatic hilum. After transection of the segment 3 pedicle, the left triangular ligament was sectioned before exposure of the hepatic vein to facilitate its control. The hepatic vein was identified and transected with the same recharged endovascular stapler (45 mm) or in some cases with the endovascular stapler (60 mm) to avoid a partial section and inadvertent bleeding.
Figure 2.
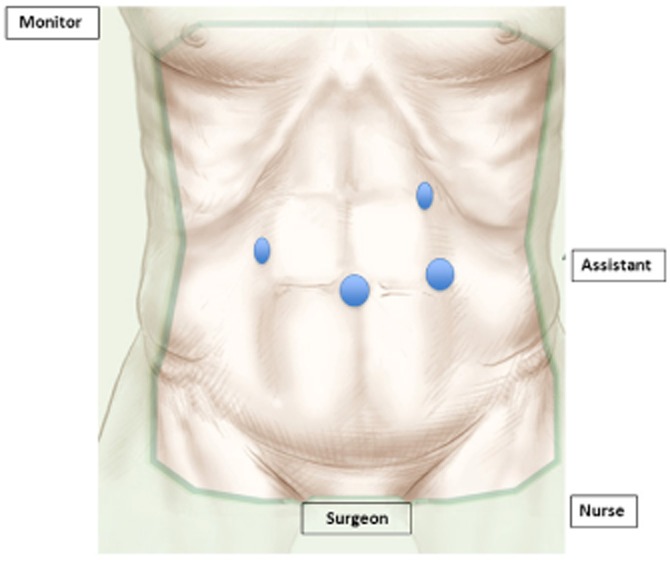
Surgical team and trocars position: two 10-mm trocars were inserted in the umbilicus (operator) and the left hypochondrium (optic) and another two 5-mm trocars are inserted as indicated
The resected liver was placed in a plastic bag and extracted without any fragmentation through a horizontal suprapubic incision or any previous abdominal scar (e.g. McBurney incision). The cut surface and the hepatic stump were inspected for any bleeding while the pressure of the pneumoperitoneum was lowered. Abdominal drainage was not used routinely.
The hand-assisted technique was used in patients with extensive lesions, in close proximity or adherence to the stomach, the spleen, the diaphragm or the hepatic vein. In this situation, mobilization of the left liver or the control of the hepatic vein can be dangerous. Using the hand-assisted technique, a left liver resection can be performed more safely in these patients, who would otherwise be candidates for open surgery.
Open procedure
The technique of an open left lateral liver resection has been described in detail elsewhere.8
Statistical methods
Continuous variables were summarized as mean and categorical variables were summarized as frequency and percentage. Statistical comparison between qualitative variables was performed with the χ2 test, and between quantitative variables with Student’s t-test. All P-values were based on a two-sided test of statistical significance. Significance was accepted at a P-value less than 0.05. All analyses were performed by SPSS software for Windows (Version 18.0; SPSS, Inc., Chicago, IL, USA).
Results
Patients’ characteristics
Both groups were strictly matched for age, gender, BMI, ASA status, comorbidities, pathology and size of the lesion as shown in Table 1. The mean age of the patients in the open group was 43.4 ± 13.2 years [mean ± standard deviation (SD)] as compared with 41.7 ± 12.2 years in the laparoscopic group (P = 0.55). The number of females and males in both groups was similar (23 versus 27 and 8 versus 4; P = 0.19). In both groups, the BMI was similar (25.8 ± 5.7 versus 24.3 ± 4.5, P = 0.15). Patients in both groups had similar comorbidities and ASA status (P = 0.43). Cystic lesions (including hydatid, mucinous and biliary cysts) and FNH were common indications in the open group and adenoma and FNH in the laparoscopic group. The mean size of lesions was 6.8 ± 3.1 cm in the open group and 8.1 ± 3.8 cm in the laparoscopic group (P = 0.50).
Table 1.
Matching characteristics of open and laparoscopic groups
| Open approach n = 31 | Laparoscopic approach n = 31 | P | |
|---|---|---|---|
| Age (mean ± SD) years | 43.4 ± 13.2 | 41.7 ± 12.2 | 0.55 |
| Gender (female/male) | 23/8 | 27/4 | 0.19 |
| BMI (mean ± SD) | 25.8 ± 5.7 | 24.3 ± 4.5 | 0.15 |
| ASA (no. of patients) I/II | 18/13 | 21/10 | 0.43 |
| Past medical history | 13 | 10 | 0.43 |
| Size of lesion (cm) | 6.8 ± 3.1 | 8.1 ± 3.8 | 0.50 |
| Indications | 0.10 | ||
| Adenoma | 4 | 12 | NS |
| Haemangioma | 3 | 2 | NS |
| Cystic lesion | 13 | 7 | NS |
| FNH | 11 | 10 | NS |
ASA, American Society of Anesthesiologists; BMI, body mass index; FNH, focal nodular hyperplasia; NS, not significant.
Intra-operative results
‘Pure laparoscopic’ procedures were performed in 23 (74.2%) patients, hand assisted in four (12.9%) patients and pure procedures converted to hand assisted in four patients (12.9%). The reason for conversion was bleeding in two patients and a technical difficulty in two patients. Retrieval of the specimen was done through a Pfannenstiel incision (5 cm) in 18 patients, through a hand port incision (7 cm) in eight patients and through a previous abdominal scar in five patients. With experience, the number of patients operated with the hand-assisted technique has decreased and during the past 2 years, no patient was operated using this approach.
Open procedures were performed through the bilateral subcostal incision in 15 (48.4%) patients, a midline incision in 13 (41.9%) and a J-shaped incision in three (9.7%) patients.
Operative parameters between the two groups are compared in Table 2. The duration of the operation was significantly shorter in the laparoscopic group (182 ± 71 versus 244 ± 105 min; P = 0.04). Pedicle clamping was used in 10 patients in each group (P = 1.000). However, the blood loss was significantly lower in the laparoscopic group. There was no difference between the two groups regarding blood transfusion. Intra-operative adverse events were seen in six patients in the open group and two patients in the laparoscopic group. Adverse events seen in the open group were bleeding from a right liver cyst fenestration, inferior vena cava or peri-hepatic varicosities. Two of these patients had significant blood loss necessitating a blood transfusion. In the laparoscopic group, two patients had bleeding from hepatic and diaphragmatic veins during parenchymal transection and liver mobilization, respectively, which were controlled through the hand port access.
Table 2.
Operative results in open and laparoscopic groups
| Open approach n = 31 | Laparoscopic approach n = 31 | P | |
|---|---|---|---|
| Duration of operation (min) | 244 ± 105 | 182 ± 71 | 0.04 |
| Clamping of pedicle (no. of patients) | 10 | 10 | 1.00 |
| Blood loss (ml) | 455 ± 593 | 223 ± 281 | 0.03 |
| Associated liver procedure | 5 | 4 | 0.12 |
| Blood transfusion (no. of patients) | 3 | 2 | 0.64 |
| Abdominal drainage (no. of patients) | 15 | 1 | <0.001 |
| Specimen weight (mg) | 414.3 ± 265.6 | 332.5 ± 180.6 | 0.05 |
Post-operative outcome
The post-operative outcome is summarized in Table 3. According to the Clavien–Dindo classification, six patients in the open group had post-operative complications compared with three patients in the laparoscopic group (P = 0.27). Severe morbidity (grade III) was seen in one patient from each group. In the open group, one patient required reoperation for a cardiac effusion (IIIb) and one patient in the laparoscopic group required tapping of a pleural effusion (IIIa). No Grade IV and V complications were seen in both groups. There was a significant difference in favour of the laparoscopic approach regarding intensive care unit duration, hospital stay (4.1 ± 1.7 versus 8.1 ± 4.4 days, P < 0.001) and the total cost of hospitalization (7475 ± 2679 versus 11504 ± 7776 Euros, P < 0.001).
Table 3.
Post-operative outcome in the open and laparoscopic groups
| Open approach n = 31 | Laparoscopic approach n = 31 | P | |
|---|---|---|---|
| Mortality | 0 | 0 | |
| Morbidity | 6 | 3 | 0.27 |
| Duration of ICU (mean ± SD) days | 0.83 ± 1.4 | 0.25 ± 0.7 | 0.04 |
| Duration discharge (mean ± SD) days | 8.06 ± 4.4 | 4.1 ± 1.7 | <0.001 |
| Total cost of hospitalization (mean ± SD) Euros | 11504 ± 7776 | 7475 ± 2679 | <0.001 |
ICU, intensive care unit; SD, standard deviation.
Discussion
In this largest series of benign liver lesions only, patients were strictly matched regarding the indication for surgery, the histopathology of the lesion and the physiological status to evaluate the efficacy of the open or laparoscopic left lateral liver resection. This study confirmed the feasibility and the safety of a laparoscopic left lateral liver resection even although these were done without control of the hepatic pedicle since 2007. Intra-operative blood loss was significantly less in laparoscopic liver resections and compares well with the literature, in which the blood loss ranges from 80 to 550 ml.9–16 The duration of the operation was also significantly shorter in laparoscopic liver resections. Lesser operative trauma of a laparoscopic liver resection resulted in the lesser need of abdominal drainage after this procedure. Operative safety of a laparoscopic liver resection translated into a smooth post-operative course with less morbidity observed when compared with the open group. The overall morbidity reported in other series of laparoscopic liver resection ranges from 10–20%,9–16 which is similar to the 10% morbidity in this series and translated into a shorter duration of hospital stay. The total cost of hospitalization for the open group was greater. Even if a laparoscopy is more expensive technically, it is much less expensive than a laparotomy owing to a shorter hospital stay. A laparoscopy appears to be more cost effective and promotes an earlier return to work by rapid recovery.
Recently, Cherqui et al. 17reported 36 laparoscopic lateral left sectionectomies, 20 of which were for malignant lesions. In comparing the first and last 18 procedures, they noted that operative time, use of the Pringle manoeuver and post-operative stay were significantly decreased with experience. In the recent era of laparoscopic liver procedures, other authors have also demonstrated the increased efficiency and safety of the laparoscopic left lateral sectionectomy compared with the open approach.9–16 However, in most of these studies, indications for a left lateral resection were not uniform (benign/malignant) and these studies also have a biased patient selection for the laparoscopic procedures. In the present case–control study, we analysed the efficacy of an open and laparoscopic left lateral resection through strict matching of diagnosis, physiological status and demographic profile of the patients.
Benign liver lesions are commonly seen in young females.6 Females of less than 40 years old constituted 82% of this study population. Cosmesis and body image are important contributors in the post-operative quality of life. Perception of post-operative cosmesis and body image is very high in females. The gender of the patient is an important selection criteria between an open and laparoscopic procedure for many other common procedures such as appendectomy and cholecystectomy.18–20 The large number of young females with a benign liver lesion in the left lateral segment prompted us to increase the utilization of the laparoscopic procedure in recent years. Although we have not studied the post-operative quality of life scores in our patients operated by laparoscopy, during the post-operative follow-up they appear more satisfied with the hidden scar.
Conclusion
Technological advancement during the past two decades has improved the outcomes of liver surgery. When the benefits of laparoscopic surgery are added to liver surgery, the outcome will be further improved. This matched case–control study has demonstrated procedural safety, excellent post-operative outcomes and the economic benefits of a laparoscopic liver resection. A laparoscopic left lateral liver resection is therefore recommended as the gold standard procedure for benign liver lesions.
Conflicts of interest
None declared.
References
- 1.Litynski GS. Erich Muhe and the rejection of laparoscopic cholecystectomy: (1985): a surgeon ahead of his time. JSLS. 1998;2:341–346. [PMC free article] [PubMed] [Google Scholar]
- 2.Payne JH, Jr, Tashima W, Lapschies B, Washecka R, Hariharan A, Duh QY. Advanced laparoscopy: ‘the next generation’. The adrenal, kidney, spleen, pancreas, and liver. Hawaii Med J. 1998;57:710–714. [PubMed] [Google Scholar]
- 3.Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78(5 Pt 2):956–958. [PubMed] [Google Scholar]
- 4.Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009;250:825–830. doi: 10.1097/sla.0b013e3181b3b2d8. [DOI] [PubMed] [Google Scholar]
- 5.Ronot M, Paradis V, Duran R, Kerbaol A, Vullierme MP, Belghiti J, et al. MR findings of steatotic focal nodular hyperplasia and comparison with other fatty tumours. Eur Radiol. 2013;23:914–923. doi: 10.1007/s00330-012-2676-y. [DOI] [PubMed] [Google Scholar]
- 6.Belghiti J, Dokmak S, Vilgrain V, Paradis V. Benign Liver Lesions. Blumgart’s, Surgery of the Liver, Biliary Tract and Pancreas. 5th edn. Philadelphia, PA: Elsevier; 2012. volume 2, Part 7, Chapter 79 A. [Google Scholar]
- 7.Dindo D, Desmartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belghiti J. Liver Resection for Benign Liver Tumors: Its Indications and Results. Vol. 1. Heidelberg: Springer; 1995. [Google Scholar]
- 9.Aldrighetti L, Pulitano C, Catena M, Arru M, Guzzetti E, Casati M, et al. A prospective evaluation of laparoscopic versus open left lateral hepatic sectionectomy. J Gastrointest Surg. 2008;12:457–462. doi: 10.1007/s11605-007-0244-6. [DOI] [PubMed] [Google Scholar]
- 10.Soubrane O, Cherqui D, Scatton O, Stenard F, Bernard D, Branchereau S, et al. Laparoscopic left lateral sectionectomy in living donors: safety and reproducibility of the technique in a single center. Ann Surg. 2006;244:815–820. doi: 10.1097/01.sla.0000218059.31231.b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abu Hilal M, McPhail MJ, Zeidan B, Zeidan S, Hallam MJ, Armstrong T, et al. Laparoscopic versus open left lateral hepatic sectionectomy: a comparative study. Eur J Surg Oncol. 2008;34:1285–1288. doi: 10.1016/j.ejso.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 12.Vanounou T, Steel JL, Nguyen KT, Tsung A, Marsh JW, Geller DA, et al. Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol. 2010;17:998–1009. doi: 10.1245/s10434-009-0839-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Endo Y, Ohta M, Sasaki A, Kai S, Eguchi H, Iwaki K, et al. A comparative study of the long-term outcomes after laparoscopy-assisted and open left lateral hepatectomy for hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech. 2009;19:e171–e174. doi: 10.1097/SLE.0b013e3181bc4091. [DOI] [PubMed] [Google Scholar]
- 14.Tang CN, Tai CK, Ha JP, Siu WT, Tsui KK, Li MK. Laparoscopy versus open left lateral segmentectomy for recurrent pyogenic cholangitis. Surg Endosc. 2005;19:1232–1236. doi: 10.1007/s00464-004-8184-7. [DOI] [PubMed] [Google Scholar]
- 15.Carswell K, Sagias FG, Murgatroyd B, Rela M, Heaton N, Patel AG. Laparoscopic versus open left lateral segmentectomy. BMC Surg. 2009;9:14. doi: 10.1186/1471-2482-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lesurtel M, Cherqui D, Laurent A, Brunetti F, Tayar C, Fagniez PL. Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg. 2003;196:236–242. doi: 10.1016/S1072-7515(02)01622-8. [DOI] [PubMed] [Google Scholar]
- 17.Chang S, Laurent A, Tayar C, Karoui M, Cherqui D. Laparoscopy as a routine approach for left lateral sectionectomy. Br J Surg. 2007;94:58–63. doi: 10.1002/bjs.5562. [DOI] [PubMed] [Google Scholar]
- 18.Bignell M, Hindmarsh A, Nageswaran H, Mothe B, Jenkinson A, Mahon D, et al. Assessment of cosmetic outcome after laparoscopic cholecystectomy among women 4 years after laparoscopic cholecystectomy: is there a problem? Surg Endosc. 2011;25:2574–2577. doi: 10.1007/s00464-011-1589-1. [DOI] [PubMed] [Google Scholar]
- 19.Tzovaras G, Liakou P, Baloyiannis I, Spyridakis M, Mantzos F, Tepetes K, et al. Laparoscopic appendectomy: differences between male and female patients with suspected acute appendicitis. World J Surg. 2007;31:409–413. doi: 10.1007/s00268-006-0335-7. [DOI] [PubMed] [Google Scholar]
- 20.Horstmann R, Tiwisina C, Classen C, Palmes D, Gillessen A. [Laparoscopic versus open appendectomy: which factors influence the decision between the surgical techniques?] Zentralbl Chir. 2005;130:48–54. doi: 10.1055/s-2004-836240. [DOI] [PubMed] [Google Scholar]


