Abstract
Purpose
To compare the complication rate of posterior capsule rupture (PCR) with vitreous loss during phacoemulsification at an ambulatory surgical center with published results as a clinical audit for quality control.
Methods
A retrospective chart review of 3,339 consecutive patients who underwent routine phacoemulsification by four experienced private practice surgeons from January 1, 2011 to June 30, 2012 at The Surgical Suites, Honolulu, HI, USA. All cases with PCR and vitreous loss were identified and selected for the study. Risk factors of this complication were further examined. Data were sent to John H Stroger Jr Hospital of Cook County, Division of Ophthalmology, for literature review, analysis, and write-up.
Results
Twenty-three of the 3,339 cases incurred PCR and vitreous loss during phacoemulsification, for an incidence rate of 0.68%. Miosis, shallow chamber, restlessness, pseudoexfoliation syndrome, floppy iris syndrome, and zonulopathy were the main causes. In addition, surgeon volume (number of cases) was inversely correlated with PCR.
Conclusion
The rate of PCR with vitreous loss during phacoemulsification in this study may be lower than other published results done at academic centers. However, there was no compatible study available for comparison, as existing studies performed at academic centers included resident cases. This study identified risk factors for PCR/vitreous loss both preoperatively and postoperatively that may assist in application of preventive measures to decrease rates of PCR/vitreous loss.
Keywords: phacoemulsification complications, posterior capsule rupture, vitreous loss, vitrectomy, miosis, pseudoexfoliation, floppy iris syndrome, zonulopathy
Introduction
One of the major complications from cataract surgery is posterior capsule rupture (PCR) with vitreous loss. Serious morbidities, including retinal detachment, cystoid macular edema, uveitis, glaucoma, and dislocated intraocular lenses (IOLs) are associated with PCR.1 For quality assessment and improvement, an audit was conducted to evaluate the rate of PCR during phacoemulsification at The Surgical Suites (Honolulu, HI, USA) and to compare this rate to that from the current literature.
After PCR, the vitreous body often prolapses and may require anterior vitrectomy to reduce the rate of complications. The vitreous humor is 98%–99% water and the rest is made up of fine collagen bundles and mucopolysaccharide hyaluronic acid. A small amount of traction can be absorbed by the vitreous humor, but larger amounts may be transferred to the posterior and peripheral retina, causing retinal tears or macular edema.2 Retinal detachment occurs after 0.5%–1.0% of phacoemulsification procedures; while it is more common after PCR with vitreous prolapse, thorough anterior vitrectomy can mitigate this complication.3
Method
This research was approved by the Institutional Review Board of the University of Hawaii. The charts of 3,339 consecutive cases of routine phacoemulsification performed by four experienced private practice surgeons from January 1, 2011 to June 30, 2012 at the Surgical Suites, Honolulu, Hawaii were retrospectively reviewed. Inclusion criteria included the use of topical anesthesia and performance at an outpatient surgical center; patients requiring additional anesthesia and those who were operated on in a hospital setting were excluded. Charts documenting PCR requiring anterior vitrectomy were identified. The causative factors leading to rupture were also noted (Table 1).
Table 1.
Causative factors for PCR from 23 cases
| Restlessness | Miosis | Shallow chamber | Pseudoexfoliation | Small eye | Floppy iris | Zonular dehiscence | |
|---|---|---|---|---|---|---|---|
| Number of cases | 6 | 7 | 8 | 5 | 1 | 6 | 5 |
| Percent | 26% | 30% | 35% | 22% | 4% | 26% | 22% |
Abbreviation: PCR, posterior capsule rupture.
Results
Of the 3,339 cases of routine phacoemulsification under topical anesthesia, 23 had PCR with vitreous loss, for an incidence rate of 0.68%. Ten were male and 13 were female, aged 60–86 years (mean 73±3 years). Miosis, shallow chamber, restlessness, pseudoexfoliation, floppy iris syndrome, and zonulopathy were the risk factors for PCR. PCR/vitreous loss was most commonly seen in eyes with shallow chamber (Table 1). Five of the 23 patients did not have sufficient support to place a posterior chamber or sulcus IOL and required placement of anterior chamber IOLs. Table 2 shows that there was an inverse correlation between PCR during phacoemulsification and the number of cases performed by the consultant surgeons: the surgeon with the lowest number of cases (411) had the highest rate of PCR (3.75%).
Table 2.
Comparison of PCR/vitreous loss rates by surgeon
| Surgeon | Total cases | PCR/vitreous loss rate |
|---|---|---|
| 1 | 536 | 0.37% |
| 2 | 1,056 | 0.28% |
| 3 | 1,336 | 0.29% |
| 4 | 411 | 3.75% |
Note: The PCR/vitreous loss rate for surgeon 4 was significantly higher than rates for the other surgeons, P<0.0001.
Abbreviation: PCR, posterior capsule rupture.
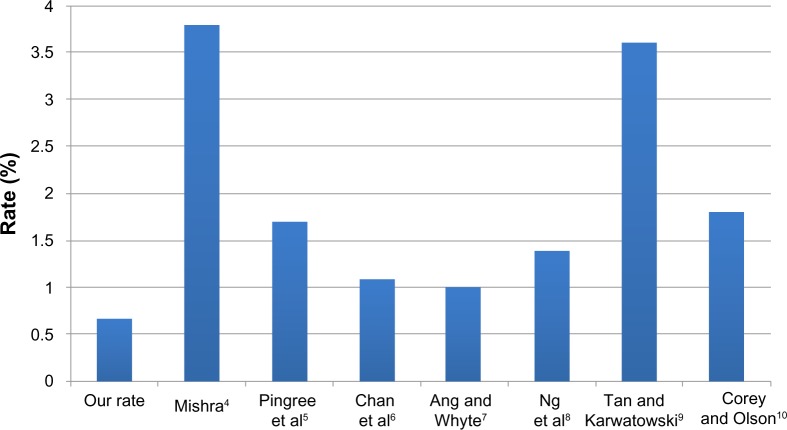
Mishra4 demonstrated a rate of PCR requiring anterior vitrectomy of 3.8% in 7,008 cases, of which 14%–15% of surgeries were performed by residents. Pingree et al5 reported 44 cases of PCR in 1,729 cataract surgeries (2.54%), with 29 (1.68%) requiring anterior vitrectomy over an 18-month period. A clinical audit performed by Chan et al6 out of Singapore in 2003 showed that PCR occurred in 155 of 8,230 consecutive eyes (1.9%) that had extracapsular cataract extraction or phacoemulsification; of those, 91 eyes (1.1%) had concurrent vitreous loss. A 2006 study from the United Kingdom showed that over a 2-year period, 2,727 cataract extractions were performed with a PCR rate of 1.7% and a vitreous loss rate of 1.0%.7 A prospective study conducted in Australia demonstrated a rate of posterior capsule tears with vitreous loss of 1.4% in 1,000 cases.8 Surgeons at the Leicester Royal Infirmary performed a total of 2,538 phacoemulsification cataract extractions, 92 (3.6%) of which required anterior vitrectomy for PCR.9 Corey and Olson10 conducted a resident performance study out of Salt Lake City, Utah that showed a vitreous loss rate of 1.8% in 396 cases (Figures 1–3).
Figure 1.
The rate of PCR with vitreous loss in our center versus that in academic centers.
Abbreviation: PCR, posterior capsule rupture.
Figure 3.
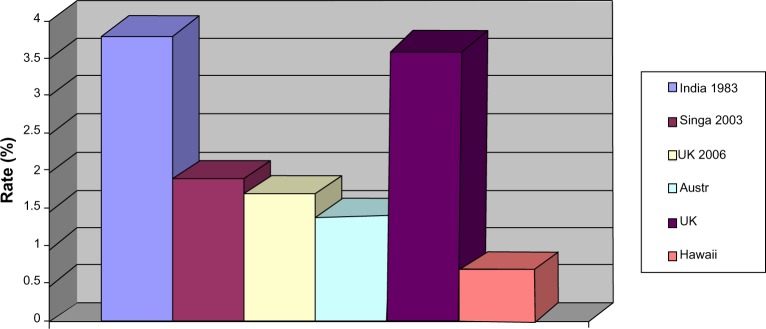
The rate of PCR with vitreous loss in The Surgical Suites versus that in other centers in the world.
Note: All centers except Hawaii were academic centers.
Abbreviations: PCR, posterior capsule rupture; Singa, Singapore; UK, United Kingdom; Austr, Australia.
Discussion
Retinal detachment, cystoid macular edema, uveitis, and glaucoma are associated with the complication of PCR with vitreous loss in cataract extraction. When the vitreous does prolapse, a careful anterior vitrectomy may prevent these complications. However, steps taken to prevent PCR and vitreous prolapse preoperatively are even more important and effective. Risk factors such as miosis, restlessness, zonulopathy, and floppy iris syndrome can be diagnosed preoperatively, and modified surgical plans can be arranged. Preventive measures such as additional 1% atropine drops, intracameral preservative-free epinephrine, viscoelastic, and mechanical pupil-dilation devices may be used to enlarge the pupil intraoperatively for miosis. Restless patients may be managed with appropriate sedation and anesthesia. Laser-assisted cataract surgery, capsular tension rings, capsular hooks, and supranucleus phacoemulsification techniques can secure the integrity of zonules to prevent PCR and vitreous loss.
This study was performed out of a privately-owned, high-volume Hawaiian cataract surgical center staffed with four cataract surgeons, each with an average of 25 years of cataract surgery experience. All four surgeons had similar phacoemulsification techniques using exactly the same phacoemulsifier and microscope. The surgical assistants were the same group. Habib et al11 showed an inverse correlation between PCR during phacoemulsification and the number of cases performed by the consultant surgeon. This is consistent with our results, in that the PCR rate was higher for the surgeon who performed the fewest procedures. There are many similar small cataract surgical centers in the United States and abroad, yet there is a lack of data regarding the PCR rate with vitreous loss at such facilities. On review of the current literature, a total of nine studies on the complication of PCR during cataract surgery were found. The total number of cases in these studies ranged from 396 to 602,553, and spanned nearly three decades, from 1983 to 2011. None of the studies was conducted in a small, privately-owned cataract surgical center similar to this facility.
As far as we know, this is the only study that has established the complication rate of PCR with vitreous loss during phacoemulsification from a small, modern, privately-owned cataract surgical center; as such, it is the only study to compare this rate to that of academic centers in the United States and abroad (Figure 1). The data from this study may be used as a reference for similar cataract surgical centers for auditing and comparison.
This study is an example of a clinical audit. The clinical audit is a cycle and it is the heart of clinical governance. There are five stages in the cycle: audit preparation, selection criteria, performance measurement, improvement implementation, and improvement sustainment. The cycle should be completed until success is achieved, and then followed by regular monitoring of performance.
Conclusion
The clinical audit of this cataract surgical center in Hawaii in 2011 had a lower rate of PCR compared to the rates published in previous literature. However, there was no compatible study available for comparison, as existing studies performed at academic centers included resident cases. Nevertheless, we provided the first and the only data available for other similar private cataract surgical centers to compare their audits on PCR with vitreous loss. The risk factors of PCR were found to be similar to those reported in the literature. All these risk factors can be carefully managed before and during phacoemulsification to reduce the PCR rate.
Figure 2.
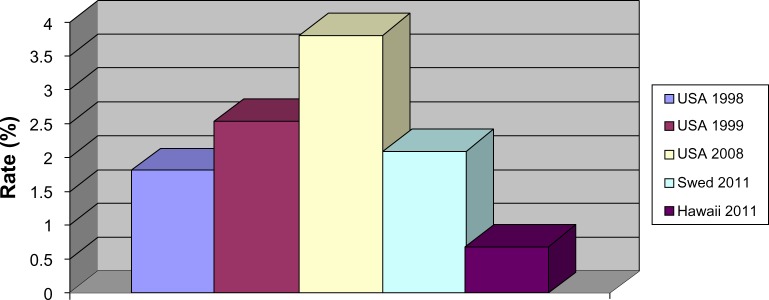
The rate of PCR with vitreous loss in The Surgical Suites versus that in other centers in the USA and Sweden.
Notes: All USA centers were academic centers and most surgeries were performed by residents. The Sweden study was based on 602,553 cataract extractions reported to the NCR of Sweden.
Abbreviations: PCR, posterior capsule rupture; Swed, Sweden; NCR, national capsule rupture.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Johansson B, Lundström M, Montan P, Stenevi U, Behndig A. Capsule complication during cataract surgery: Long-term outcomes: Swedish Capsule Rupture Study Group report 3. J Cataract Refract Surg. 2009;35(10):1694–1698. doi: 10.1016/j.jcrs.2009.05.027. [DOI] [PubMed] [Google Scholar]
- 2.Sebag J. Vitreous biochemistry, morphology, and clinical examination. In: Duane TD, Tasman W, Jaeger EA, editors. Duane’s Foundations of Clinical Ophthalmology. Philadelphia, PA: Lippincott Williams & Wilkins; 1998. pp. 7–15. [Google Scholar]
- 3.Tan JH, Karwatowski WS. Phacoemulsification cataract surgery and unplanned anterior vitrectomy-is it bad news? Eye (Lond) 2002;16(2):117–120. doi: 10.1038/sj.eye.6700015. [DOI] [PubMed] [Google Scholar]
- 4.Mishra RK. Anterior vitrectomy. Indian J Ophthalmol. 1983;31(3):288–289. [PubMed] [Google Scholar]
- 5.Pingree MF, Crandall AS, Olson RJ. Cataract surgery complications in 1 year at an academic institution. J Cataract Refract Surg. 1999;25(5):705–708. doi: 10.1016/s0886-3350(99)00017-6. [DOI] [PubMed] [Google Scholar]
- 6.Chan FM, Mathur R, Ku JJ, et al. Short-term outcomes in eyes with posterior capsule rupture during cataract surgery. J Cataract Refract Surg. 2003;29(3):537–541. doi: 10.1016/s0886-3350(02)01622-x. [DOI] [PubMed] [Google Scholar]
- 7.Ang GS, Whyte IF. Effect and outcomes of posterior capsule rupture in a district general hospital setting. J Cataract Refract Surg. 2006;32(4):623–627. doi: 10.1016/j.jcrs.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 8.Ng DT, Rowe NA, Francis IC, et al. Intraoperative complications of 1000 phacoemulsification procedures: a prospective study. J Cataract Refract Surg. 1998;24(10):1390–1395. doi: 10.1016/s0886-3350(98)80235-6. [DOI] [PubMed] [Google Scholar]
- 9.Tan JH, Karwatowski WS. Phacoemulsification cataract surgery and unplanned anterior vitrectomy – is it bad news? Eye (Lond) 2002;16(2):117–120. doi: 10.1038/sj.eye.6700015. [DOI] [PubMed] [Google Scholar]
- 10.Corey RP, Olson RJ. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J Cataract Refract Surg. 1998;24(1):66–72. doi: 10.1016/s0886-3350(98)80076-x. [DOI] [PubMed] [Google Scholar]
- 11.Habib M, Mandal K, Bunce CV, Fraser SG. The relation of volume with outcome in phacoemulsification surgery. Br J Ophthalmol. 2004;88(5):643–646. doi: 10.1136/bjo.2003.028159. [DOI] [PMC free article] [PubMed] [Google Scholar]