Abstract
Evidenced-based-wound management continues to be a cornerstone for advancing patient care. The purpose of this article is to review the use of whirlpool as a wound treatment in light of evidence, outcomes, and potential harm. Whirlpool was initially harnessed as a means to impart biophysical energy to a wound or burn to enhance mechanical debridement and cleansing. Other credible single-patient-use technologies which provide an alternative to whirlpool in wound care are presented.
Keywords: Wound care modalities, Biophysical energies for debridement, Whirlpool, Biofilm, Cross contamination
Overview
Evidence-based practice (EBP) involves clinical reasoning in three major domains: best-available scientific evidence, clinical judgment (experience), and patient's perspective (Figure 1). Evidenced-based wound care seeks to integrate clinical wisdom with the best available science to optimize patient care with safety, statistical power and efficacy brought to bear on the problem at hand, the wound(s).1 This paper provides perspective primarily in the domain of best-available scientific evidence as it pertains to whirlpool (WP) use in wound care.
Figure 1.
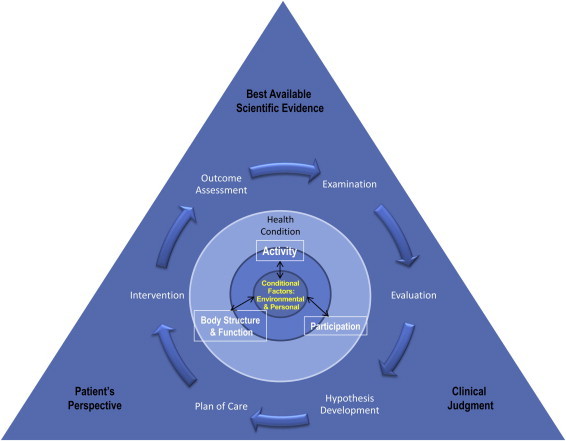
Clinical reasoning with EBP.
Whirlpool, one of the oldest types of hydrotherapy, was originally used by physical therapists (PTs) to treat patients with burns in need of extensive debridement. In many areas of the United States, WP remains an active component of wound care as a means for the removal of necrotic cellular debris and contamination. With the advent of other options, using water as a cleansing agent, it is important to critically analyze the literature reporting the effects of WP. The following summarizes the evidence pertaining to both the goals and the adverse events associated with WP therapy.
The full-body WP (Figure 2), and the Hubbard tank, quickly spearheaded the development of smaller extremity tanks (Figure 3).2,3 The shared goals of WP therapy are to remove gross contaminants and toxic debris including surface bacterial, increase local circulation, decrease wound pain, decrease suppuration, decrease fever, help soak and gently remove dressings, and ultimately accelerate healing.2,4 Typically, it is prescribed for non-healing wounds or to remove a substantial amount of necrotic tissue. The limb or extremity is submersed for 10–20 minutes in water at 92°–96 °F, with or without agitation and antimicrobial agents.5
Figure 2.

Lo Boy whirlpool photo.
Figure 3.

Extremity whirlpool.
The presence of bacteria and/or biofilm can both be obstacles to healing. All wounds have some level of contamination which does not equate to ‘infection’. Critical bacterial colonization occurs when the number of microbes and/or their byproducts exceed the capability of the host to generate a healing response significant enough to effect wound closure.
An additional obstacle to wound closure and cross-contamination is biofilm. Biofilms are structured, highly-organized, communities of microorganisms.6-8 Biofilm poses a challenge by allowing heterogenic bacterial colonies to evade host defense mechanisms under a protective polysaccharide covering, serving both to evade host defense mechanisms and provide a climate ripe for genetic cassette exchange to promulgate antibiotic resistance.9 Biofilm, in the case of the wound environment, presents challenges for the host in terms of clearing pathogens, and subsequently requires advanced wound healing techniques.10 Biofilm adheres not only to wounds and living tissues, but also to medical equipment for example, WP surfaces and catheters, where biofilms allow bacteria to evade antiseptics, antimicrobials, and sterilization procedures.9 Biofilm formation can singularly prove devastating for healing progression both from the perspective of providing a source for potential patient cross contamination as well as delaying individual wound healing.
Infection occurs when the concentration of pathogenic microorganisms exceeds a tolerable level for normal wound healing to occur. Clinically, an infection is defined as exceeding the “critical level” of 100,000 pathogenic microorganisms per gram of tissue.11,12 Infection delays angiogenesis and granulation, thereby delaying wound healing.12,13 Another barrier to normal wound healing is the presence of eschar, which acts as a physical barrier to impede epithelialization and facilitates wound infection by providing a nutrition source for bacteria.12
An acute wound defines a wound that heals normally (typically complete within 21–41 days) with predictable progression through the phases of healing. The term chronic wound defines a wound that does not heal within the expected time frame and does not exhibit orderly progression of healing phases.2,14,15 The wound halts in a pro-inflammatory state and presents with uncoordinated phases of healing such that different areas within the same wound are found in different phases of healing.13 For normal wound healing to occur, the following are needed: early, appropriate intervention,16 functioning immune system,17-19 adequate blood flow,20 control of bacterial bioburden,21 chronic disease management,22,23 and understanding of expected timing of the process.9,13,24-29
The evidence using WP as a means to facilitate the healing process, while addressing the removal of biofilm, debris and eschar while simultaneously mitigating pain is presented below.
Evidence on Whirlpool: Goals
Removing gross contaminants and toxic debris, diluting bacterial content
Removing gross contaminants and toxic debris, as well as diluting surface bacterial content are the premise of WP's cleansing effects. While this is theoretically sound, there are no double-blind, randomized studies to demonstrate these effects.2,30 In 1982, Bohannan31 found that WP therapy and rinse removed up to four times more bacteria than WP itself in a venous stasis ulcer. However this study was a single-subject-pilot-study that was not followed up. In 1975 Niederhuber et al32 found that maximum reduction of bacteria was associated with 20-minute immersion in water at 37.7 °C and agitation. However this study did not incorporate high-quality randomization nor specify the use of antimicrobial additives.2
Increasing local circulation, helping soak and gently removing dressings
Evidence to support WP's effects on increasing local circulation and helping soak and gently remove dressings are anecdotal at best. In a 2003 review of mechanical adjuncts to wound care, Hess et al2 state that water temperatures around 35.5–39.0 °C promote circulation to the wound surface, but do not cite a source or scientific method to justify this conclusion.
The same review cites only personal communication with a colleague to suggest its benefit with allowing dressings to be soaked slowly and gently removed. This reference further states that WP may be good for patients with crush injuries, venous and arterial insufficiency (although the remainder of review does not support this), pyoderma gangrenosum, animal bites, and occasionally Diabetes mellitus.2
Decreasing wound pain, suppuration, fever, accelerated healing
The claim that WP decreases wound pain, suppuration and fever, and accelerates healing was made by Langenbeck,33 over 100 years ago. Since then, only one RCT published by Burke et al30 in 1998 has supported WP's effect on accelerated wound healing. In the study by Burke, patients with grade III and IV pressure ulcers were randomly assigned to conservative treatment (n = 18) and conservative treatment plus whirlpool (n = 24) groups. Conservative treatment was defined as saline moistened wet-to-wet dressings. Using wound dimension as an outcome, they found that more ulcers in the WP plus conservative treatment group showed improvement (p < 0.05).
Evidence on Whirlpool: Adverse Events
Pseudomonas aeruginosa
Pseudomonas aeruginosa (P. aeruginosa) is a highly evolved pathogen that is prevalent in hospital environments and recognized as a common cause of nosocomial infections, especially with hydrotherapy.34-36 These infections may lead to sepsis/septic shock, folliculitis, bacteremia, and pneumonia. Presence of more developed P. aeruginosa can be extremely fatal, with a 33–80% mortality rate.34-36 Many accurate laboratory methods exist to identify and match bacterial strains in a wound to its source (e.g., WP).37-39 Several studies have reported cases of WP-associated P. aeruginosa infection; below is a summary of two reported hospital outbreaks.
A 1992 study involving burn victims by Tredget et al34 found that despite weekly surveillance cultures of equipment and standardized protocols for disinfection, a significant lethal strain of P. aeruginosa was found in hydrotherapy (WP) equipment. They associated hydrotherapy use with P. aeruginosa infections, substantial morbidity, and higher mortality rates. The study concluded that there is a significant benefit to managing these patients without hydrotherapy, as it resulted in significant elimination of skin donor site infections.
A 2000 study by Berrouane et al35 supports some of the previous claims made by Tredget et al. This study investigated a recent outbreak of P. aeruginosa at the University of Iowa Hospital, despite infection control measures. These bacteria can be present in hoses, pipes, and filters despite use of disinfectant, and can proliferate rapidly if disinfectant levels are below recommended concentration. All 7 affected patients in the hospital during the 14-month period were male and ill (indicating likely low WBC and albumin); four died. The authors concluded that these infections were highly associated with the WP tubs. Patients who are immunocompromised are at significantly higher risk for P. aeruginosa infection.35
Damage to granulation tissue, hindrance of migrating epidermal cells, maceration
Hess et al2 report that 6 psi of force can help cleanse healthy granulation tissue. However, pressure delivered to the wound surface through WP therapy can vary and be difficult to monitor and control. Higher unspecified and unregulated pressures may damage developing granulation tissue, hinder migrating epidermal cells2 and neutrophils, known to be key to the innate immune response,40 and cause maceration.2
Venous hypertension and vascular congestion
Using WP for the lower extremity places the extremity in a dependent position. This has been shown to increase venous hypertension and vascular congestion of that limb, both of which physiologically decrease the efficiency of wound healing, especially in those patients with venous insufficiency.2,41 These effects have not been studied in the upper extremity.
Alternative Treatments to Whirlpool
Several alternatives to WP therapy exist for treating acute and chronic wounds. Below are summaries of a few alternatives identified in the literature that address several of the purported goals of WP therapy. The most current, acceptable systematic reviews and pertinent high-level studies were reviewed in order to summarize the following treatment modalities.
Pulsed lavage with vacuum (also known as lavage, jet lavage, mechanical lavage, mechanical irrigation, high-pressure irrigation)
Pulsed lavage with vacuum (PLWV) is increasingly gaining favor over WP as the optimal mode for wound cleansing. This single-patient-use-technique utilizes an irrigating solution delivered under pressure via a powered device.2,12 A pressure of 10–15 psi is generally accepted as most efficient to remove debris, decrease bacterial colonization, and prevent clinical infection.2,12 Future studies are required to determine the optimal delivery pressure and mode (continuous vs. intermittent/pulsed) for wound healing. Nonetheless, PLWV has demonstrated improved rates of tissue granulation (12.2%/week), a rate significantly faster than WP therapy (4.8%/week)2,12 Further studies must compare the effectiveness of PLWV to WP in other aspects of wound healing (e.g., healing rate, bacterial concentration, cost-effectiveness).12
Theoretically, PLWV risks the potential promotion of infection (e.g., bacteremia). However, no studies demonstrate increased risk with different pressures. Currently, it is recommended pressures be maintained below 15 psi to prevent theoretical spread of infection, until additional studies are conducted.12 Overall, the benefits of PLWV for wound cleansing are promising. This technique is currently recommended over WP therapy by recent reviews.2,12
Ultrasound (1 and 3 MHz frequencies)
Ultrasound remains a controversial modality in wound care. It transmits thermal and non-thermal waves through tissue by converting electrical waves into sound waves. Historically, thermal waves have been used for late stages of wound healing to improve scar/wound outcome.2 Non-thermal waves have been used in early stages exploiting cavitation to change cell permeability and improve diffusion.2 Various lab-based studies have supported its effects which include: improved cell recruitment, collagen synthesis, increased collagen tensile strength, angiogenesis, wound contraction, fibroblast and macrophage stimulation, fibrinolysis, reduced inflammatory phase/promoting proliferative phase healing.2 Compared with PLWV, clinical outcomes were not as definitive: some studies show improvement in venous stasis wounds over placebo, while others do not. Clinical studies with pressure ulcers were less promising.2
Moist dressings
Moist dressings provide a moist wound surface to allow infiltration of phagocytic cells and eventual epithelialization.42 Moist dressings also theoretically protect the wound from infection, but there is conflicting clinical evidence regarding its efficacy for reducing infection rates.14 Despite an abundance of clinical trials, there is no definitive evidence to support one particular type of moist dressing. However, hydrocolloid dressings have been established to be superior to wet-to-dry dressings.14
Negative pressure wound therapy
Negative pressure wound therapy (NPWT) uses sub-atmospheric pressure to convert an open wound to a controlled closed wound. Medical-grade open-cell polyurethane ether foam is cut and placed within the wound, filling the wound defect. Continuous or intermittent pressure of 100–125 mmHg is then applied. NPWT theoretically improves blood flow, removes interstitial fluid, reducing edema, and decreasing interstitial diffusion distance, thereby improving wound oxygenation.2 Animal studies by Morykwas et al43 demonstrated that NPWT promotes granulation tissue formation greater than 103%. Furthermore, wounds treated with NPWT remained under standards for bacterial levels of infection, while wounds treated with dressings reached clinically infected levels by day 11.2,16
Some clinical complications may arise with NPWT including discomfort and minor bleeding during dressing changes, initial patient discomfort with negative pressure, and rare instances of pressure necrosis when placed over bone or ischemic wounds.2 Nonetheless, NPWT has demonstrated significant clinical success with chronic wounds.2
Discussion
“As with any treatment modality, we must, thus, weigh the use of therapy time and effort against objective evidence that supports its use for [wound care].”30
A primary goal of wound care is to create a healing environment enabling the wound to complete self-repair. To that end wound cleaning, including the removal of excess bacteria, eschar and necrotic tissue through cleansing, debriding, while maintaining moisture to facilitate autolytic debridement, all remain key ingredients. Cleansing refers to the use of fluid to remove loosely attached cellular debris, surface pathogens, and residual topical agents from the wound surface.12 Debridement refers sharp, mechanical, autolytic or chemical means to remove adherent material from the wound.12
Whirlpool seeks to address the reduction of bacterial bioburden while simultaneously loosening slough and foreign debris with emulsification of adherent fibrin. However, when used in the treatment of extremities, the resulting vascular impact can be one of edema, due in part to the dependent position of the extremity, with a corresponding increase in venous hypertension.41 Physiologically, at the cellular level, cooling, super hydration and maceration occur, with a noted decrease in antimicrobial peptide levels, macrophage and neutrophil presence. Newly formed granulation tissue is often fragile and easily disrupted. A potential unintended consequence of using WP jets or agitation to dislodge debris, may be the reduction of granulation tissue. In addition, there are documented risks for patient cross contamination with the WP proven to be the vehicle.34,35,44
Insubstantial evidence exists to unequivocally support the role of WP therapy in wound healing. Many claims are based in anecdotal accounts.2 Studies lack quality (e.g., no randomization or blinding) and are outdated by over 20 years.2,30-33 Only one recent high quality study demonstrated its benefits over a control with no hydrotherapy,30 however, this study did not compare WP benefits to other modalities.30 Concurrently, a pool of studies associating WP therapy with nosocomial infections and delayed wound healing exists.2,34-36,41
Several single-patient-use-WP alternatives are readily available and which have literature support and a documented lower risk of adverse events. PLWV is an example of a technique that has been directly compared with WP therapy and is more efficient for wound cleansing. Other examples include NPWT, compression, moist dressings, and perhaps ultrasound. These are only a few of the technologies available for wound cleansing, disruption of biofilm and debridement.
There are some limitations to this report. Some articles regarding WP therapy were inaccessible by online database but were summarized by several systematic reviews herein. Another limitation is the use of articles with data from different types of wounds (e.g., burn wounds, chronic wounds, pressure ulcers, venous leg ulcers). While it is acknowledged that these wounds arise from varied etiologies, nonetheless they progress through the same phases of healing. The conclusions from this report should support its ability to be generalized to all wound types.
Conclusion
Limited evidence supporting WP usage exists when contrasting the intended goals and patient physiological response. Of greater concern are several reported adverse events, including contamination from P. aeruginosa,2,34-36 damage to developing granulation tissue, hindrance of migrating epidermal cells, maceration,2,3 and increased venous hypertension and vascular congestion.2,41
Evidenced-based-wound management continues to increase and along with that the evaluation and re-evaluation of biophysical energies in light of evidence, outcomes, and potential harm. Whirlpool, initially harnessed as a physical energy, which could simultaneously do mechanical debridement and cleansing, does not have sufficient evidence to remain among viable choices for patient care, especially when one considers the options of single-patient-use-interventions which eliminate the potential for cross-contamination. Our responsibility as health care practitioners is to minimize risks for our patients. Based on the evidence, utilizing readily accessible modalities and alternatives to WP therapy in wound care is the most credible option.
Clinical recommendation
The risk of nosocomial infection associated with WP therapy is too significant to overcome the limited evidence supporting its benefits in wound care. In the presence of several treatment alternatives (e.g., PLWV), evidence-based practice (via best-available scientific evidence) does not support the use of WP for wound care.
Footnotes
Conflict of interest: None of the authors have any conflicts of interest. No financial support was requested or received in the course of this review.
References
- 1.Bolton L.L., Baine W.B. Using science to advance wound care practice: lessons from the literature. Ostomy Wound Manage. 2012;58(9):16–31. [PubMed] [Google Scholar]
- 2.Hess C.L., Howard M.A., Attinger C.E. A review of mechanical adjuncts in wound healing: hydrotherapy, ultrasound, negative pressure therapy, hyperbaric oxygen, and electrostimulation. Ann Plast Surg. 2003;51(2):210–218. doi: 10.1097/01.SAP.0000058513.10033.6B. [DOI] [PubMed] [Google Scholar]
- 3.Frantz R.A. Adjuvant therapy for ulcer care. Clin Geriatr Med. 1997;13(3):553–564. [PubMed] [Google Scholar]
- 4.Gogia P.P., Hurt B.S., Zirn T.T. Wound management with whirlpool and infrared cold laser treatment. A clinical report. Phys Ther. 1988;68(8):1239–1242. [PubMed] [Google Scholar]
- 5.McCulloch J., Kloth L. Wound care management. Rehab Manag. 1997;10(3):46, 50, 58. [PubMed] [Google Scholar]
- 6.Costerton JW. The Society for Investigative Dermatology, Inc; 2007.
- 7.Costerton J.W., Stewart P.S., Greenberg E.P. Bacterial biofilms: a common cause of persistent infections. Science. 1999;284:1318–1322. doi: 10.1126/science.284.5418.1318. [DOI] [PubMed] [Google Scholar]
- 8.Costerton J.W., Veeh R., Shirtliff M., Pasmore M., Post C., Ehrlich G. The application of biofilm science to the study and control of chronic bacterial infections. J Clin Invest. 2003;112:1466–1477. doi: 10.1172/JCI20365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ammons M.C. Anti-biofilm strategies and the need for innovations in wound care. Recent Pat Antiinfect Drug Discov. 2010;5(1):10–17. doi: 10.2174/157489110790112581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolcott R.D., Rumbaugh K.P., James G. Biofilm maturity studies indicate sharp debridement opens a time-dependent therapeutic window. J Wound Care. 2010;19(8):320–328. doi: 10.12968/jowc.2010.19.8.77709. [DOI] [PubMed] [Google Scholar]
- 11.Robson M.C., Heggers J.P. Bacterial quantification of open wounds. Mil Med. 1969;134(1):19–24. [PubMed] [Google Scholar]
- 12.Luedtke-Hoffmann K.A., Schafer D.S. Pulsed lavage in wound cleansing. Phys Ther. 2000;80(3):292–300. [PubMed] [Google Scholar]
- 13.Li J., Chen J., Kirsner R. Pathophysiology of acute wound healing. Clin Dermatol. 2007;25(1):9–18. doi: 10.1016/j.clindermatol.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Bradley M., Cullum N., Nelson E.A., Petticrew M., Sheldon T., Torgerson D. Systematic reviews of wound care management: (2). Dressings and topical agents used in the healing of chronic wounds. Health Technol Assess. 1999;3(17 Pt 2):1–35. [PubMed] [Google Scholar]
- 15.Phillips S.J. Physiology of wound healing and surgical wound care. ASAIO J. 2000;46(6):S2–S5. doi: 10.1097/00002480-200011000-00029. [DOI] [PubMed] [Google Scholar]
- 16.Hess C.T. 5th ed. Lippincott Williams & Wilkins; Philadelphia: 2005. Wound Care. [Google Scholar]
- 17.Jones S.G., Edwards R., Thomas D.W. Inflammation and wound healing: the role of bacteria in the immuno-regulation of wound healing. Int J Low Extrem Wounds. 2004;3(4):201–208. doi: 10.1177/1534734604271810. [DOI] [PubMed] [Google Scholar]
- 18.Roupe K.M., Nybo M., Sjobring U., Alberius P., Schmidtchen A., Sorensen O.E. Injury is a major inducer of epidermal innate immune responses during wound healing. J Invest Dermatol. 2010;130(4):1167–1177. doi: 10.1038/jid.2009.284. [DOI] [PubMed] [Google Scholar]
- 19.Koch A.E., Volin M.V., Woods J.M. Regulation of angiogenesis by C-X-C chemokines interleukin-8 and epithelial neutrophil activating peptide 78 in the rheumatoid joint. Arthritis Rheum. 2001;44:31–40. doi: 10.1002/1529-0131(200101)44:1<31::AID-ANR5>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 20.Bartolucci R. 1st ed. Nuova Editrice Grafica; Rome, Italy: 2002. Critical Lower Limb Ischemia: Principles and Practice. [Google Scholar]
- 21.Wolcott R.D., Ehrlich G.D. Biofilms and chronic infections. JAMA. 2008;299:2682–2684. doi: 10.1001/jama.299.22.2682. [DOI] [PubMed] [Google Scholar]
- 22.Chow I., Lemos E.V., Einarson T.R. Management and prevention of diabetic foot ulcers and infections: a health economic review. Pharmacoeconomics. 2008;26(12):1019–1035. doi: 10.2165/0019053-200826120-00005. [DOI] [PubMed] [Google Scholar]
- 23.Connor H. Some historical aspects of diabetic foot disease. Diabetes Metab Res Rev. 2008;24(suppl 1):S7–S13. doi: 10.1002/dmrr.838. [DOI] [PubMed] [Google Scholar]
- 24.Bates-Jensen B.M. Chronic wound assessment. Nurs Clin North Am. 1999;34(4):799–845. [v] [PubMed] [Google Scholar]
- 25.Bates-Jensen B.M., McNees P. Toward an intelligent wound assessment system. Ostomy Wound Manage. 1995;41(7A suppl):80S–86S. [discussion 87S] [PubMed] [Google Scholar]
- 26.Beitz J.M., Bates-Jensen B. Algorithms, critical pathways, and computer software for wound care: contemporary status and future potential. Ostomy Wound Manage. 2001;47(4):33–40. [quiz 41–32] [PubMed] [Google Scholar]
- 27.Guo S., Dipietro L.A. Factors affecting wound healing. J Dent Res. 2010;89(3):219–229. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.James D.W. Wound healing. Med World. 1958;89(2):122–126. [PubMed] [Google Scholar]
- 29.Lazarus G.S., Cooper D.M., Knighton D.R., Percoraro R.E., Rodeheaver G., Robson M.C. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994;2(3):165–170. doi: 10.1046/j.1524-475X.1994.20305.x. [DOI] [PubMed] [Google Scholar]
- 30.Burke D.T., Ho C.H., Saucier M.A., Stewart G. Effects of hydrotherapy on pressure ulcer healing. Am J Phys Med Rehabil. 1998;77(5):394–398. doi: 10.1097/00002060-199809000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Bohannon R.W. Whirlpool versus whirlpool rinse for removal of bacteria from a venous stasis ulcer. Phys Ther. 1982;62(3):304–308. doi: 10.1093/ptj/62.3.304. [DOI] [PubMed] [Google Scholar]
- 32.Niederhuber S.S., Stribley R.F., Koepke G.H. Reduction of skin bacterial load with use of the therapeutic whirlpool. Phys Ther. 1975;55(5):482–486. doi: 10.1093/ptj/55.5.482. [DOI] [PubMed] [Google Scholar]
- 33.Kellogg J.H. F.A. Davis; 1904. Rational Hydrotherapy: A Manual of the Physiological and Therapeutic Effects of Hydriatic Procedures, and the Technique of Their Application in the Treatment of Disease. [Google Scholar]
- 34.Tredget E.E., Shankowsky H.A., Joffe A.M. Epidemiology of infections with Pseudomonas aeruginosa in burn patients: the role of hydrotherapy. Clin Infect Dis. 1992;15(6):941–949. doi: 10.1093/clind/15.6.941. [DOI] [PubMed] [Google Scholar]
- 35.Berrouane Y.F., McNutt L.A., Buschelman B.J. Outbreak of severe Pseudomonas aeruginosa infections caused by a contaminated drain in a whirlpool bathtub. Clin Infect Dis. 2000;31(6):1331–1337. doi: 10.1086/317501. [DOI] [PubMed] [Google Scholar]
- 36.Hatchette T.F., Gupta R., Marrie T.J. Pseudomonas aeruginosa community-acquired pneumonia in previously healthy adults: case report and review of the literature. Clin Infect Dis. 2000;31(6):1349–1356. doi: 10.1086/317486. [DOI] [PubMed] [Google Scholar]
- 37.Speert D.P., Campbell M.E., Farmer S.W., Volpel K., Joffe A.M., Paranchych W. Use of a pilin gene probe to study molecular epidemiology of Pseudomonas aeruginosa. J Clin Microbiol. 1989;27(11):2589–2593. doi: 10.1128/jcm.27.11.2589-2593.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Vos D., Lim A., Jr., Pirnay J.P. Direct detection and identification of Pseudomonas aeruginosa in clinical samples such as skin biopsy specimens and expectorations by multiplex PCR based on two outer membrane lipoprotein genes, oprI and oprL. J Clin Microbiol. 1997;35(6):1295–1299. doi: 10.1128/jcm.35.6.1295-1299.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Feizabadi M.M., Majnooni A., Nomanpour B. Direct detection of Pseudomonas aeruginosa from patients with healthcare associated pneumonia by real time PCR. Infect Genet Evol. 2010;10(8):1247–1251. doi: 10.1016/j.meegid.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 40.Segal A.W. How neutrophils kill microbes. Annu Rev Immunol. 2005;23:197–223. doi: 10.1146/annurev.immunol.23.021704.115653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McCulloch J., Boyd V.B. The effects of whirlpool and the dependent position on lower extremity volume. J Orthop Sports Phys Ther. 1992;16(4):169–173. doi: 10.2519/jospt.1992.16.4.169. [DOI] [PubMed] [Google Scholar]
- 42.Werdin F., Tennenhaus M., Schaller H.E., Rennekampff H.O. Evidence-based management strategies for treatment of chronic wounds. Eplasty. 2009;9:e19. [PMC free article] [PubMed] [Google Scholar]
- 43.Morykwas M.J., Argenta L.C., Shelton-Brown E.I., McGuirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38(6):553–562. doi: 10.1097/00000637-199706000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Stanwood W., Pinzur M.S. Risk of contamination of the wound in a hydrotherapeutic tank. Foot Ankle Int. 1998;19(3):173–176. doi: 10.1177/107110079801900312. [DOI] [PubMed] [Google Scholar]


