Abstract
In recent years, several studies have reported that the prevalence of diabetes mellitus is increasing every year, and also the acute and chronic complications accompanying this disease are increasing. Diabetic nephropathy is one of chronic complications of diabetes mellitus, and food intake which is burden to kidney function should be limited. At the same time, diet restriction could deteriorate quality of life of patient with diabetic nephropathy. According to the results of previous studies, the aggressive management is important for delaying of the progression to diabetic nephropathy. Also, the implementation of a personalized diet customized to individuals is an effective tool for preservation of kidney function. This is a case report of a patient with diabetic nephropathy who was introduced to a proper diet through nutrition education to prevent malnutrition, uremia and to maintain blood glucose levels.
Keywords: Diabetic nephropathies, Diabetes mellitus, Nutrition education
Introduction
According to a recently released 'The Korean Diabetes Research Report 2012' by Korean Diabetes Association, one out of ten adults has diabetes disease, two out of ten have the impaired fasting glucose which is stage of diabetes, and three out of ten adults are threatened by high blood glucose [1]. In addition, the aging society proceeds quickly, thereby the number of diabetes patients are predicted about 6 million in 2050, approximately a 2-fold increase compared to the current number of diabetes patients [1,2]. Also, the incidence of acute and chronic complications associated with diabetes is expected to increase [2,3]. Especially diabetic nephropathy occurs more frequently among the patients suffered from diabetes for a long time. Also, it is a complication that has a large impact on patient's quality of life [4].
A balanced diet was recommended for diabetes mellitus patient as a key component of diet therapy. On the other hand, food intake increases burden to kidney function in diabetic nephropathy patients. Therefore, the patient who proceeded to diabetic nephropathy needs nutrition education to properly manage the disease and to increase the quality of life. [4].
Diabetic nephropathy occurs in 20% to 40% of patients with diabetes, and is a most likely causes of end-stage renal disease reported worldwide [5]. Continuous microalbuminuria (30-299 mg/day) appears in the early stages of diabetic nephropathy with type 1 diabetes, and it is an indicator of nephropathy onset and the development of cardiovascular disease [5]. A patient who had a progression from microalbuminuria to macroalbuminuria (≥300 mg/day) has a high risk of developing end-stage renal disease in few years [5].
According to a recent study, the deterioration of renal function could be delayed by proactive management at the initial diagnosis point, therefore, it is important to implement a personalized diet customized to individuals as soon as possible [6]. In this case report, the nutrition education for one patient with diabetic nephropathy is discussed.
Case
The patient was a 52-year-old woman who was diagnosed with type 2 diabetes mellitus approximately 6 years ago. The patient had been taking oral hypoglycemic agents (Glimepiride) and insulin (Glargine 18-20 IU before breakfast and 4 IU before bed) to control blood glucose level. The patient's 2 hrs postprandial blood level was normally maintained between 280-300 mg/dL, however, the level increased to 300-400 mg/dL, in recent 2-3 weeks and the patient was hospitalized to control high glucose level. In addition to that, the patient had been receiving medical treatment for hypertension and dyslipidemia, and regular blood tests and urine tests were performed to monitor significant changes. The patient had been diagnosed with renal failure and proteinuria one year ago, and at the time of this hospitalization, the patient was diagnosed with stage 4 chronic kidney disease, and was consulted for nutrition education of diabetic nephropathy.
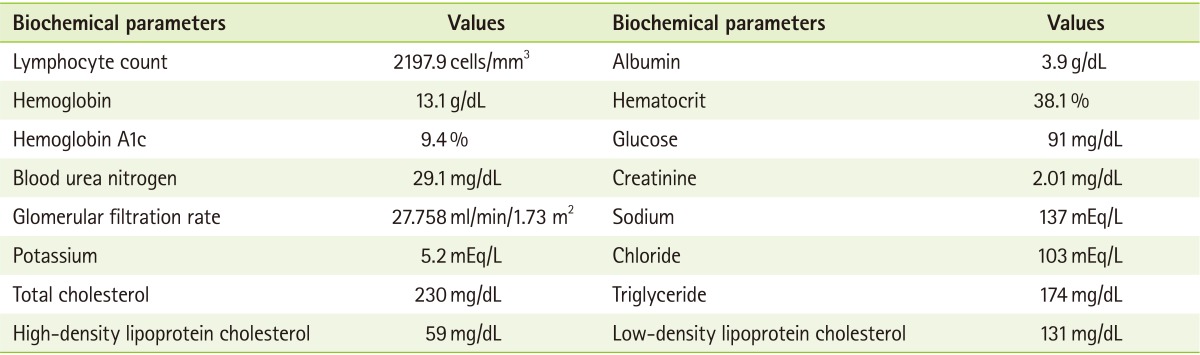
The patient's height and weight were 158 cm and 81.4 kg, respectively, percent of ideal body weight was 155.5%, indicating she was severely obese. Biochemical values of the patient are shown in Table 1.
Table 1.
Biochemical data of the patient at baseline
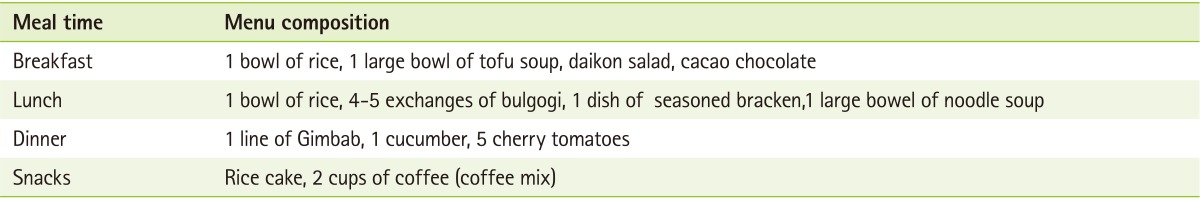
The patient preferred a salty soup and stew, and the actual amount of intake exceeded the recommendation. When eating out once a week, the patient often ate a hamburger or a noodle meal. The patient's diet history was analyzed by the 24-hr recall method using Can Pro 3.0 software (The Korean Nutrition Society, Seoul, South Korea) (Table 2). The patient consumed approximately 1,840 kcal/d with a protein intake of 67.5 g, and the energy ratio from carbohydrate, protein, and fat was 61.7%: 14.4%: 23.9%, respectively. The patient did not take any nutritional supplements, and did not drink alcohol, or smoke. The patient's physical activity was rated to mild level of a homemaker; she participated in weight training or bowling for 2 hrs (3 times a week). The patient had never received nutrition education.
Table 2.
Diet composition consumed by the patient
The patient was prescribed the nutritional regimen as follows.
-
- Energy: 1,600 kcal (30 kcal/kg x 52.4 kg ideal body weight [IBW])
- Protein: 40 g/d (0.8 g/kg × 52.4 kg [IBW])
- Sodium: 2,000 mg/d
- Potassium: 2,000 mg/d
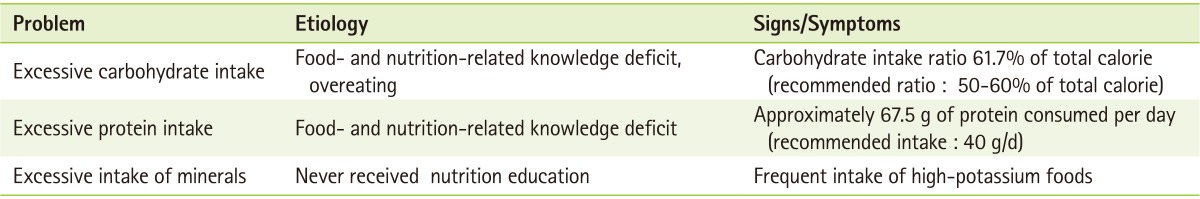
This patient revealed problematic dietary habits including excessive carbohydrate intake, excessive protein intake, and excessive potassium intake (Table 3). After analysing etiology, lack of knowledge and absence of education experience were selected as main causes. Therefore nutrition education for diabetic nephropathy was conducted.
Table 3.
Nutritional diagnosis of the patient
The nutritional problems of "excessive carbohydrate intake" and "excessive protein intake" were managed by establishing adequate nutrition through a diet comprising 1,600 kcal of energy, and below 60 percent of energy from carbohydrate and 40 g of protein per day. Food models and a food exchange list were configured to provide nutritional training for the proper dietary intake. Compliance issues were also discussed during the education period.
The association of carbohydrate intake and blood glucose control was discussed in relation to the nutritional problem of "excessive carbohydrate intake". Also, recommended amount of rice intake was 2/3-3/4 bowls (2.3 exchanges), which is reduced from one bowl (3 exchanges) a meal. Usually, it was necessary to take a proper amount of fat for preventing malnutrition and lack of caloric intake arise when protein and carbohydrates were restricted. However the patient had dyslipidemia and limited intake of animal fat was recommended. In addition, the patient was provided with information on the importance of eating the low-salt diet and tips for how to eat the low-salt diet easily. The tips for how to eat the low-salt diet are as follows. 1) Apply of spicy and sour flavor seasoning like pepper or vinegar, instead of salt or fermented soybean paste. 2) Limit the intake of high-salt-containing foods, such as kimchi, and other salted and pickled foods, 3) Consume side dishes during meals without the addition of salt, 4) Grilled food rather than boiled was recommended and use the food's own flavor effectively when cooking, 5) When salting, focus on one kind of food.
The patient was instructed to limit their intake of high potassium-containing foods (grains, potatoes, sweet potatoes, corn, soybean, green vegetables, nuts, tomatoes, kiwi, banana, melon etc.). To reduce potassium intake, the intake of raw vegetables was recommended. It was also recommended to remove the shell before cooking, to use leaves rather than stem and to boil vegetables in water 4-5 times of their volumes.
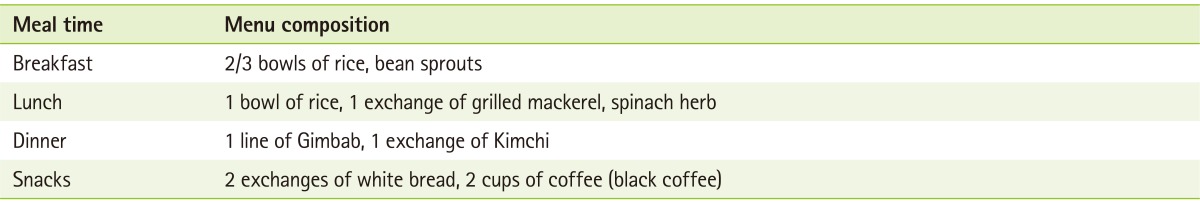
The results of nutrition education after 3 months are shown in Table 4-6. The patient's diet history during last 3 months was analyzed by the 24-hr recall method using Can Pro 3.0 software (The Korean Nutrition Society, Seoul, South Korea). The patient consumed approximately 1,300 kcal/d with a protein intake of 37.6 g, and the energy supply from carbohydrate, protein, and fat was 71.3%, 11.6%, and 17.1%, respectively.
Table 4.
Biochemical data of the patient after nutritional intervention
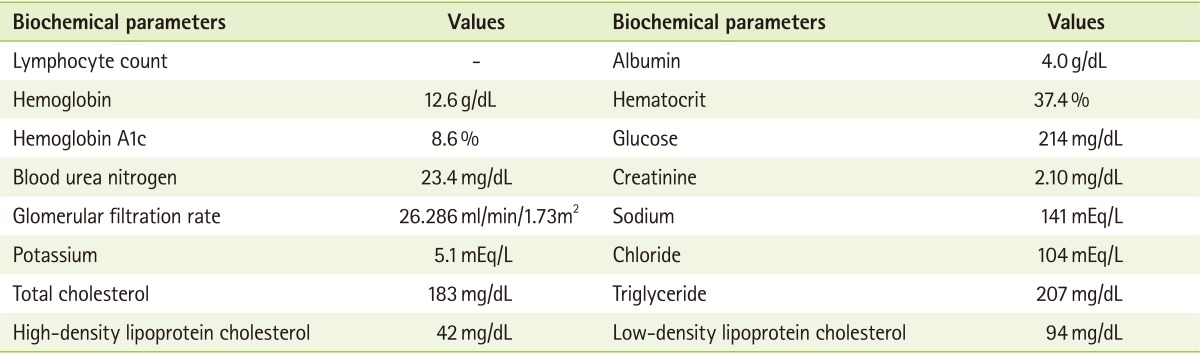
Table 6.
Achievement results of nutritional interventions
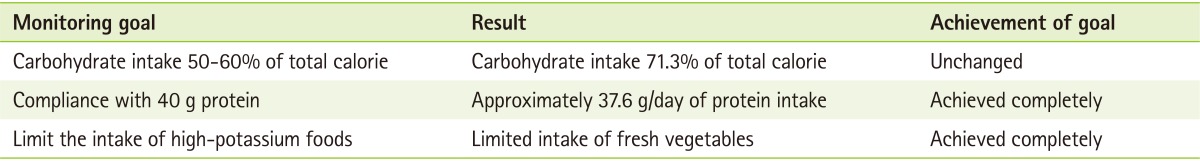
After receiving the nutrition education for three months, the patient's energy intake was reduced by 500 kcal compared to three months ago. Protein intake was about 30 g less compared to three months ago. Limited intake of high-potassium foods was relatively well kept.
Discussion
This article is a case report of a patient with chronic kidney disease caused by diabetic nephropathy. Because this patient had never received any nutrition education, the patient's food and nutrition related knowledges was poor. As a result, the patient had problems including excessive intakes of carbohydrate, protein, and potassium, which was problematic for disease management. To solve this problem, nutrition education was performed. Three months after the education, the patient's blood profile data was collected from electronic medical records (EMR), and the patient's dietary intake data was collected through direct interviews. Effects of nutrition education intervention were analyzed.
After intervention, carbohydrate intake did not conform exactly to recommendation, but protein intake and limitation of high-potassium foods were fairly well complied. The recommended carbohydrate intake is 50-60% of the total calories consumed [4]. Excessive carbohydrate intake should be avoided as far as possible owing to its blood glucose control issues. To slow the progression of kidney complications, protein intake should be limited to 0.8-1 g/kg IBW/d for those with microalbuminuria, and should be limited to 0.8 g/kg IBW/d for those with macroalbuminuria, and should be limited to 0.6-0.8 g/kg IBW/d for those with end-stage renal disease [7]. Adequate fat intake is necessary to prevent malnutrition, because a lack of caloric intake can induce the restricted protein and carbohydrate intake [4]. This patient also had dyslipidemia. Dyslipidemia is one of the most common complication in patients with diabetic nephropathy and is correlated with disease progression [8]. This patient needs to be screened for microalbuminuria to prevent the progression of diabetic nephropathy, and dyslipidemia should be treated to reduce cardiovascular mortality [9]. The consumption of oils with saturated fatty acids and meat should be limited, and stir-fried vegetables and vegetable oil should be consumed in moderation [4].
For strict blood pressure control, sodium intake is limited to 2,000 mg/d [7]. Potassium is involved in the contraction and relaxation of muscles in the human body and is an essential electrolyte. However, when kidney function decreases, excess potassium cannot be easily excreted and is accumulated in the body, creating a burden. Therefore, potassium intake should be limited in chronic kidney disease or in the case of hyperkalemia [4,7]. Potassium is mainly found in vegetables and fruits. Therefore, the intake of coarse grains and vegetables should be limited, and should be soaked in water for more than 2 hours, and then blanched in boiling water before cooking [4,7]. Phosphorus in combination with calcium is found in bones and teeth. In reduced renal function, the amount of phosphorus that is emitted through the kidneys decreases and the blood levels of phosphorus increase. As the blood levels increase, skeletal calcium levels decrease causing debilitating bone disease. Therefore, drug therapy is required in chronic kidney disease stages and the intake of foods that contain high levels of phosphorus should be reduced [7].
A diabetic diet entails consumption of a healthy and balanced diet. Whereas a chronic kidney disease or diabetic nephropathy diet should be designed to delay the progression of kidney disease, uremia due to renal dysfunction, hypertension, edema, hyperkalemia, hyperlipidemia and to control blood glucose along with the regulation of sodium, protein, and potassium levels. Thus compared to the diabetic diet, the diabetic nephropathy diet is a little more complicated and restrictive. However, a personalized diet plan and continuous monitoring are required in diabetic nephropathy patien according to the patient's stage of disease.
Table 5.
Daily diet composition consumed by the patient after nutritional intervention
Footnotes
We declare that we have no conflict of interest.
References
- 1.Park SA. Social welfare approach for the patient with diabetic nephropathy. J Korean Diabetes. 2013;14:42–45. [Google Scholar]
- 2.Kim MK. Pathophysiology of diabetic nephropathy. J Korean Diabetes. 2013;14:15–18. [Google Scholar]
- 3.Kim JH. The epidemiology of diabetic nephropathy. J Korean Diabetes. 2013;14:11–14. [Google Scholar]
- 4.Kim JY. Diet therapy in patients of diabetic nephropathy. J Korean Diabetes. 2013;14:27–31. [Google Scholar]
- 5.American Diabetes Association. Standards of medical care in diabetes-2013. Diabetes Care. 2013;36(Suppl 1):S11–S66. doi: 10.2337/dc13-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho JW. Diet therapy for diabetic nephropathy. Korean Clin Diabetes. 2009;10:45–50. [Google Scholar]
- 7.Korean Diabetes Association. Medical treatment manual for diabetes - practice of dietetic therapy doctor need to know. Seoul: Korean Diabetes Association; 2011. pp. 27–31. [Google Scholar]
- 8.Gall MA, Hougaard P, Borch-Johnsen K, Parving HH. Risk factors for development of incipient and overt diabetic nephropathy in patients with non-insulin dependent diabetes mellitus: prospective, observational study. BMJ. 1997;314:783–788. doi: 10.1136/bmj.314.7083.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28:164–176. doi: 10.2337/diacare.28.1.164. [DOI] [PubMed] [Google Scholar]


