Abstract
Peroral cholangioscopy is an important tool for diagnosis and treatment of various biliary disorders. Peroral cholangioscopy can be performed by using a dedicated cholangioscope that is advanced through the accessory channel of a duodenoscope, or by direct insertion of a small-diameter endoscope into the bile duct. Direct peroral cholangioscopy refers to insertion of an ultraslim endoscope directly into the bile duct for visualization of the biliary mucosa and lumen. This approach provides a valuable and economic solution for diagnostic and therapeutic applications in the biliary tree. Compared to ductoscopy using a dedicated cholangioscope, the direct approach has several advantages and disadvantages. In this editorial, I discuss the advantages, disadvantages, and possible future developments pertaining to direct peroral cholangioscopy.
Keywords: Cholangioscopy, Direct peroral cholangioscopy, Dedicated cholangioscopes
Core tip: Direct peroral cholangioscopy is a valuable and economic tool for diagnostic and therapeutic applications in the biliary tree. However, solutions are needed to make access to the biliary tree easier, and to improve the endoscope stability within the biliary tree for diagnostic and therapeutic maneuvers.
METHODS OF PERORAL CHOLANGIOSCOPY
Peroral cholangioscopy has numerous applications in diagnosis and treatment of various biliary disorders[1]. Currently, peroral cholangioscopy can be performed by two different methods: (1) by using a dedicated cholangioscope and (2) by direct insertion of a small-diameter upper endoscope into the biliary tree (the direct method).
Peroral cholangioscopy using a dedicated cholangioscope
In this approach, a dedicated cholangioscope is advanced through the accessory channel of a duodenoscope and directed into the bile duct (Figure 1). A biliary sphincterotomy is usually necessary for advancement of the cholangioscope through the biliary sphincter. Although biliary cannulation can be achieved directly with the tip of the cholangioscope, most endoscopists prefer cannulation over a guidewire[2]. Once the scope is advanced to the target location, the guidewire is removed to enhance visualization and to permit use of the working channel. The duct is irrigated with sterile saline solution through the accessory channel of the cholangioscope for adequate visualization, followed by slow withdrawal of the scope, allowing systematic inspection of the ductal mucosa and lumen.
Figure 1.
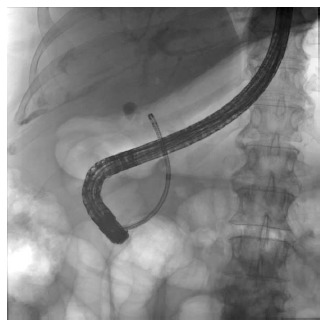
Cholangioscopy using a dedicated cholangioscope. In this approach, a dedicated cholangioscope is advanced through the accessory channel of a duodenoscope and directed into the bile duct.
Direct peroral cholangioscopy
In direct peroral cholangioscopy, an ultraslim upper endoscope is inserted through the mouth and advanced to the duodenum. It is subsequently maneuvered across the biliary sphincter and into the bile duct for observation of the mucosa and the lumen of the bile duct (Figure 2). Maneuvering of the endoscope across the biliary sphincter requires presence of a sphincterotomy and in most cases performance of a balloon sphincteroplasty. Presence of a guidewire in the bile duct often allows a more proximal access, to the common hepatic duct. The guidewire is subsequently removed to better visualize the lumen and mucosa, to allow more freedom of movement at the tip of the endoscope and to make the accessory channel available for therapeutic measures if needed. The bile duct is irrigated with sterile saline solution through the accessory channel of the ultraslim endoscope followed by slow withdrawal of the endoscope allowing systematic inspection of the biliary tree. Sterile saline irrigation can be substituted with carbon dioxide (CO2) insufflation. In a study involving 19 patients with suspected biliary disease, Ueki et al[3] reported superior image quality using CO2 insufflation compared to saline irrigation. Another study involving 36 patients, however, reported that although the median time required to obtain a clear endoscopic image using CO2 insufflation was significantly shorter than that required for saline irrigation, the quality of the endoscopic images obtained was similar in the majority of cases[4]. Air insufflation during direct cholangioscopy has been associated with serious adverse events and its use has been discouraged[5].
Figure 2.
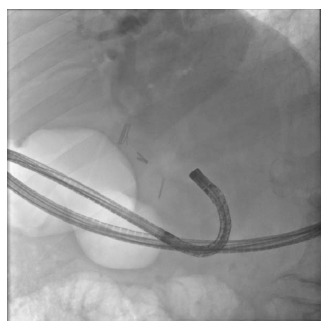
In direct peroral cholangioscopy, an ultraslim upper endoscope is inserted through the mouth and advanced to the duodenum. It is subsequently maneuvered across the biliary sphincter and into the bile duct for observation of the mucosa and the lumen of the bile duct.
With the introduction of high-definition ultraslim upper endoscopes with narrow band imaging capability, direct peroral cholangioscopy has become more popular. The ultraslim upper endoscopes currently used for direct peroral cholangioscopy have an outer diameter of approximately 5 mm and an instrument channel with an inner diameter of approximately 2 mm[5].
ADVANTAGES OF DIRECT PERORAL CHOLANGIOSCOPY
Commercial availability
In cholangioscopy, whether direct or using a dedicated cholangioscope, the quality of the image is of utmost importance. Among dedicated cholangioscopes, only high-definition video cholangioscopes can offer the same image quality as the ultraslim upper endoscopes used in direct cholangioscopy. Dedicated high-definition video cholangioscopes are currently produced only as prototypes and thus not available for commercial use. Ultraslim upper endoscopes used for direct cholangioscopy, on the other hand, are widely available on a commercial basis.
Image quality
Currently, none of the commercially available dedicated cholangioscopes can offer high-definition images. High definition, refers to an increase in pixels (dots) received by the endoscope and displayed on the monitor to increase the detail of the surface being seen, enabling detection of smaller and more obscure lesions[6]. It also may allow for more detailed examination of lesions that may already have been seen in standard definition, although, with less detail. The new-generation of ultraslim upper endoscopes offer high-definition images allowing detailed examination of biliary mucosa and ductal lumen with subsequent increase in their diagnostic capability (Figure 3).
Figure 3.
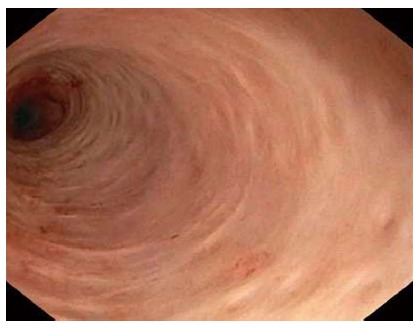
View of the bile duct lumen and mucosa by direct peroral cholangioscopy. Note the normal pit pattern.
Operating expense
Currently-available dedicated cholangioscopes are expensive to use. The single-operator cholangioscopy systems have single-use components that have to be discarded after each case while the dual-operator systems are fragile, break easily and are in need of frequent repairs[1,2]. The expenses associated with direct cholangioscopy are far less compared to use of dedicated cholangioscopes.
Narrow band imaging capability
At present, commercially available dedicated cholangioscopes do not have narrow band imaging capability. Described by Gono and colleagues for the first time in 2004, narrow band imaging uses electronic processing of light in order to highlight particular components of an image[7,8]. The principle behind narrow band imaging technology is that the bandwidths of blue and green light are narrowed while the contribution of red light is negated out of the emitted light[8]. The narrowed bandwidths of green and blue light lead to superficial penetration of the mucosa accentuating the microvasculature pattern as hemoglobin has a peak absorption spectrum towards both these wave lengths[8]. Narrow band imaging can therefore improve visualization of the vascular pattern and aid in the diagnosis of various biliary disorders particularly indeterminate biliary strictures[2].
Size of accessory channel
The currently available ultraslim upper endoscopes have an accessory channel with an inner diameter of 2 mm, which is much larger than the accessory channel of the dedicated cholangioscopes measuring approximately 1.2 mm[2,5]. The larger size of the accessory channel allows easier passage of equipment such as biopsy forceps for tissue sampling or lithotripsy probes for fragmentation of difficult to remove biliary stones.
Operating a single endoscope
Compared to dedicated cholangioscopy which requires simultaneous operation of two endoscopes (the duodenoscope and the dedicated cholangioscope), direct cholangioscopy involves only a single endoscope that is manipulated into the lumen of the bile duct by a single endoscopist. Dealing with only one endoscope, avoids problems associated with simultaneous operation of multiple endoscopes such as coordination of movements.
Simultaneous irrigation, suction and therapeutic maneuvers
The ultraslim upper endoscope allows simultaneous irrigation, suction and therapeutic maneuvers. None of the currently available dedicated cholangioscopes have this capability.
DISADVANTAGES OF DIRECT PERORAL CHOLANGIOSCOPY
Larger outer diameter of the endoscope
The ultraslim upper endoscopes have an outer diameter of 5-6 mm, which is significantly larger than the diameter of most dedicated peroral cholangioscopes (3.0-3.5 mm). Direct cholangioscopy using the ultraslim upper endoscopes can therefore be performed only in patients with dilated bile ducts. In addition, the larger outer diameter requires generous sphincterotomy and sphincteroplasty for manipulation of the endoscope across the biliary sphincter.
Difficulty of insertion into the bile duct
The most profound disadvantage of direct peroral cholangioscopy is the difficulty associated with traversing the biliary sphincter to gain access to the bile duct. A high percentage of direct peroral cholangioscopy procedures, therefore, end up in failure. This difficulty of bile duct cannulation with an upper endoscope is mainly due to the looping of the ultraslim upper endoscope in the stomach or in the duodenum (Figure 4). There are therefore multiple published reports in the endoscopic literature with innovative suggestions on how to achieve this task. Introduction of the endoscope over a guidewire, through a regular overtube, or with the help of a double-balloon overtube are some of the suggestions[9-12]. However, despite use of these accessories, failure rate still remains high[13].
Figure 4.
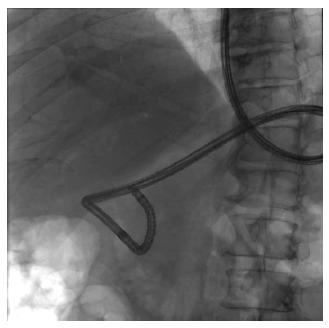
Fluoroscopic view of the ultraslim upper endoscope. Note looping of the endoscope in the stomach. Although the tip of the endoscope is well within the bile duct lumen, the endoscope cannot be further advanced to the more proximal ducts because of the looping.
Lack of stability inside the bile duct
Another disadvantage of direct cholangioscopy is the instability of the ultraslim upper endoscope once it is inside the bile duct. This instability makes it difficult to perform diagnostic or therapeutic procedures such as obtaining biopsies of lesions or lithotripsy of difficult to remove biliary stones. Endoscope instability can also lead to loss of access and prolongation of the procedure.
Lack of access to proximal ducts
In direct peroral cholangioscopy, access to the more proximal ducts is often not possible. Usually direct cholangioscopy can only visualize the ducts distal to the confluence of the right and left hepatic ducts. The right and left hepatic ducts and their branches are for the most part inaccessible for direct peroral cholangioscopy, limiting its use in only the most distal parts of the biliary tract[5].
FUTURE DIRECTIONS
Despite its many advantages, direct peroral cholangioscopy is rarely performed in nonacademic settings, mostly because of the difficult and time-consuming task of bile duct cannulation with an upper endoscope. Different variations of inflatable balloons used as an anchor within the biliary tree have been introduced for easier access[5,14]. Although these devices perform well for allowing access to the bile duct for assessment and therapy of disorders of the distal biliary system, it is often difficult to maneuver the endoscope and gain access to the ducts proximal to the bifurcation after deflation and removal of the anchoring balloon. Devices, such as overtubes, that can allow more proximal access while improving the stability of the endoscope are needed.
Currently, direct peroral cholangioscopy can only be performed in patients with dilated biliary tree. Ultraslim upper endoscopes with smaller outer diameter but preserved stiffness designed for direct peroral cholangioscopy will be a welcome addition to the existent array of endoscopes.
Finally, accessory equipment designed for use in direct peroral cholangioscopy can further improve the utility of this procedure.
CONCLUSION
Peroral cholangioscopy is an important tool for diagnosis and treatment of various biliary disorders. Peroral cholangioscopy can be performed by using a dedicated cholangioscope or by direct insertion of an ultraslim endoscope into the bile duct (direct peroral cholangioscopy). Compared to ductoscopy using a dedicated cholangioscope, the direct approach has several advantages and disadvantages (Table 1). The direct approach provides a valuable and economic solution for diagnostic and therapeutic applications in the biliary tree. However, solutions are needed to make access to the biliary tree easier, and to improve the endoscope stability within the biliary tree for diagnostic and therapeutic maneuvers.
Table 1.
Comparison of direct and dedicated cholangioscopy
| Direct cholangioscopy | Dedicated high-definition cholangioscopy | |
| Commercial availability of the endoscope | Yes | No (prototypes) |
| Operating expense | Low | High |
| Image quality | Excellent | Excellent |
| Narrow band imaging capability | Yes | Yes |
| Required number of operators | One | Two |
| Irrigation capability | Yes | Limited |
| Suctioning capability | Yes | Limited |
| Fragility | No | Yes |
| Size of accessory channel | 2 mm | 1.2 mm |
| Insertion into the bile duct | Difficult | Easy |
| Stability inside the bile duct | Unstable | Stable |
| Access to proximal ducts | No | Yes |
Footnotes
P- Reviewers: Lin CH, Kara M, Nimura Y S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
References
- 1.Parsi MA. Peroral cholangioscopy in the new millennium. World J Gastroenterol. 2011;17:1–6. doi: 10.3748/wjg.v17.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parsi MA, Stevens T, Collins J, Vargo JJ. Utility of a prototype peroral video cholangioscopy system with narrow-band imaging for evaluation of biliary disorders (with videos) Gastrointest Endosc. 2011;74:1148–1151. doi: 10.1016/j.gie.2011.07.050. [DOI] [PubMed] [Google Scholar]
- 3.Ueki T, Mizuno M, Ota S, Ogawa T, Matsushita H, Uchida D, Numata N, Ueda A, Morimoto Y, Kominami Y, et al. Carbon dioxide insufflation is useful for obtaining clear images of the bile duct during peroral cholangioscopy (with video) Gastrointest Endosc. 2010;71:1046–1051. doi: 10.1016/j.gie.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Doi S, Yasuda I, Nakashima M, Iwashita T, Toda K, Mukai T, Iwata K, Itoi T, Moriwaki H. Carbon dioxide insufflation vs. conventional saline irrigation for peroral video cholangioscopy. Endoscopy. 2011;43:1070–1075. doi: 10.1055/s-0030-1256764. [DOI] [PubMed] [Google Scholar]
- 5.Parsi MA, Stevens T, Vargo JJ. Diagnostic and therapeutic direct peroral cholangioscopy using an intraductal anchoring balloon. World J Gastroenterol. 2012;18:3992–3996. doi: 10.3748/wjg.v18.i30.3992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Overhiser AJ, Sharma P. Advances in endoscopic imaging: narrow band imaging. Rev Gastroenterol Disord. 2008;8:186–193. [PubMed] [Google Scholar]
- 7.Gono K, Obi T, Yamaguchi M, Ohyama N, Machida H, Sano Y, Yoshida S, Hamamoto Y, Endo T. Appearance of enhanced tissue features in narrow-band endoscopic imaging. J Biomed Opt. 2004;9:568–577. doi: 10.1117/1.1695563. [DOI] [PubMed] [Google Scholar]
- 8.Singh R, Mei SC, Sethi S. Advanced endoscopic imaging in Barrett’s oesophagus: a review on current practice. World J Gastroenterol. 2011;17:4271–4276. doi: 10.3748/wjg.v17.i38.4271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larghi A, Waxman I. Endoscopic direct cholangioscopy by using an ultra-slim upper endoscope: a feasibility study. Gastrointest Endosc. 2006;63:853–857. doi: 10.1016/j.gie.2005.07.050. [DOI] [PubMed] [Google Scholar]
- 10.Bohle W. A simple and rapid technique of direct cholangioscopy. Gastrointest Endosc. 2007;65:559. doi: 10.1016/j.gie.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 11.Choi HJ, Moon JH, Ko BM, Hong SJ, Koo HC, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Overtube-balloon-assisted direct peroral cholangioscopy by using an ultra-slim upper endoscope (with videos) Gastrointest Endosc. 2009;69:935–940. doi: 10.1016/j.gie.2008.08.043. [DOI] [PubMed] [Google Scholar]
- 12.Moon JH, Ko BM, Choi HJ, Koo HC, Hong SJ, Cheon YK, Cho YD, Lee MS, Shim CS. Direct peroral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol. 2009;104:2729–2733. doi: 10.1038/ajg.2009.435. [DOI] [PubMed] [Google Scholar]
- 13.Terheggen G, Neuhaus H. New options of cholangioscopy. Gastroenterol Clin North Am. 2010;39:827–844. doi: 10.1016/j.gtc.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 14.Moon JH, Ko BM, Choi HJ, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. Intraductal balloon-guided direct peroral cholangioscopy with an ultraslim upper endoscope (with videos) Gastrointest Endosc. 2009;70:297–302. doi: 10.1016/j.gie.2008.11.019. [DOI] [PubMed] [Google Scholar]


