Abstract
AIM: To assesse the rate of bile duct injuries (BDI) and overall biliary complications during single-port laparoscopic cholecystectomy (SPLC) compared to conventional laparoscopic cholecystectomy (CLC).
METHODS: SPLC has recently been proposed as an innovative surgical approach for gallbladder surgery. So far, its safety with respect to bile duct injuries has not been specifically evaluated. A systematic review of the literature published between January 1990 and November 2012 was performed. Randomized controlled trials (RCT) comparing SPLC versus CLC reporting BDI rate and overall biliary complications were included. The quality of RCT was assessed using the Jadad score. Analysis was made by performing a meta-analysis, using Review Manager 5.2. This study was based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. A retrospective study including all retrospective reports on SPLC was also performed alongside.
RESULTS: From 496 publications, 11 RCT including 898 patients were selected for meta-analysis. No studies were rated as high quality (Jadad score ≥ 4). Operative indications included benign gallbladder disease operated in an elective setting in all studies, excluding all emergency cases and acute cholecystitis. The median follow-up was 1 mo (range 0.03-18 mo). The incidence of BDI was 0.4% for SPLC and 0% for CLC; the difference was not statistically different (P = 0.36). The incidence of overall biliary complication was 1.6% for SPLC and 0.5% for CLC, the difference did not reached statistically significance (P = 0.21, 95%CI: 0.66-15). Sixty non-randomized trials including 3599 patients were also analysed. The incidence of BDI reported then was 0.7%.
CONCLUSION: The safety of SPLC cannot be assumed, based on the current evidence. Hence, this new technology cannot be recommended as standard technique for laparoscopic cholecystectomy.
Keywords: Bile ducts, Cholecystectomy, Single port, Single incision
Core tip: This study assessed the rate of Bile Duct Injuries and overall biliary complications during single port laparoscopic cholecystectomy. A systematic review of the literature was performed, including 11 randomized controlled trials (898 patients) and 60 non-randomized trials (3599 patients). No statistically significant differences were found. However, interpretation of the results was impaired by several limitations. Based on a retrospective analysis, an incidence of bile duct injuries up to 0.7% was found. The safety of single-port laparoscopic cholecystectomy cannot be assumed, based on the current evidence. Hence, this new technology cannot be recommended as standard technique for laparoscopic cholecystectomy so far.
INTRODUCTION
The recent decade has seen striking technical changes in gastrointestinal surgery. Surgeons’ interest and expectations were high while waiting for the next technical evolution after laparoscopy[1]. Some of these expectations were also fuelled by industry and by patients themselves.
Traditionally, many innovations in digestive surgery were first evaluated by using cholecystectomies in humans as an in vivo model. The large number of patients in good condition, the non-reconstructive nature of such an intervention, and the availability of a standardized operative technique for comparison are the main characteristics predisposing gallbladder surgery to assess new technologies. Complication rates are generally low, and the only real difficulty is to avoid bile duct injuries (BDI)[2]. Indeed, BDI represent the key criteria comparing a novel technique to the current standard laparoscopic approach. The widespread implementation of conventional laparoscopic cholecystectomy (CLC) in 1990’s was associated with an increased rate of bile duct injuries[3]. The lessons learnt by the clinical introduction of laparoscopy need to be re-considered since several novel techniques of minimal invasive surgery are on the point of being introduced as routine procedures in surgery without enough evidence on safety issues.
An increasingly voluminous literature on single port laparoscopic cholecystectomy (SPLC) has become available after five years of intense publications worldwide. In their meta-analysis, neither Sajid et al[4] nor Trastulli et al[5] found statistical significant differences between the two procedures in term of complications. However, BDI injuries were not analyzed specifically. On the other hand, Joseph et al[6] reported BDI rate as high as 0.72%, based on retrospective data.
The aim of this systematic review was to evaluate the current rate of BDI and overall biliary complication rate during single port laparoscopic cholecystectomy and to compare it with conventional laparoscopic cholecystectomy.
MATERIALS AND METHODS
Study selection
A systematic review of the literature published between January 1990 and November 2012 was performed by the first author from Medline, Embase and Web of Science databases. This search was then cross-checked by the senior author (Schäfer M). Following Medical Subject Heading (MeSH) and non-MeSH keywords were used: “cholecystectomy”, “laparoscopy”, “single trocar”, “single port”, “single incision”, “single site”, “single access”, “trans-umbilical”, “single incision laparoscopic surgery”, “laparoendoscopic single site”. The search was also enlarged using the “related articles” function and by manual cross-check of individual articles. A flowchart of the selection process, according to Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statements[7], is presented in Figure 1.
Figure 1.
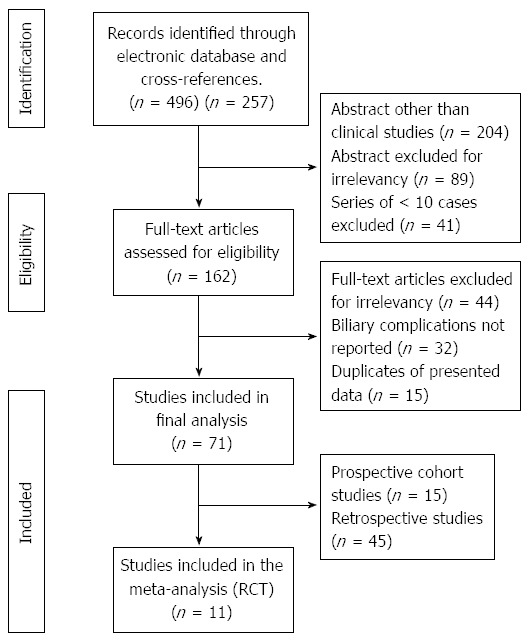
Flowchart diagram of the systematic review. RCT: Randomized controlled trials
Inclusion/exclusion criteria
Initially, all clinical trials conducted on humans and reporting clearly surgical complications were included. There were no language limitations. A second step of the analysis included only randomized controlled trials. We excluded all papers not related to the subject, all series that did not report surgical complications and all series including less than 10 patients.
Outcome of interest
The primary endpoint was the rate of BDI, as described by Strasberg et al[2]. Secondary endpoints were the rate of overall biliary complications, defined as any complication related to the biliary system that required the readmission of patients or additional interventions, such as endoscopic retrograde cholangiopancreatography or percutaneous drainage of bilioma. The time of follow-up, the realization of intraoperative cholangiography (IOC) and the report of a true critical view were also considered.
Study quality
The quality of randomized controlled trials (RCT) was assessed using the Jadad score[8]. Studies with a score of ≥ 4 were considered high quality studies. Two reviewers (Allemann P, Schäfer M) evaluated independently all RCT included in the analysis. Results were compared thereafter and consensus were established when discrepancies were found.
Statistical analysis
Meta-analysis was conducted according to the PRISMA guideline. Investigations were performed using Review Manager 5.2 (release November 8, 2012. Cochrane Information Management System). Evaluating dichotomous variables, OR were used in the statistical analysis and favored conventional laparoscopic cholecystectomy if < 1. A statistically significant result was considered if the P value was < 0.05, and if the confidence interval did not include the value 1. Heterogeneity was assed using χ2 and I2 statistics. High I2 and P value < 0.001 indicated significant heterogeneity between the studies. A power calculation was made using STATA 12.0 (Stata Corp., College Station, TX, United States), with an alpha-error of 0.05 (two sided) and a power of 80%.
RESULTS
After electronic research and manual cross match, 496 abstracts were collected. From these, 71 studies were included in the final analysis. Eleven studies were randomized controlled trials, including a total of 839 patients (438 SPLC, 401 CLC)[9-19]. Eight series were single center[9,12,14-19], whereas the three remaining trials were multicenter studies[10,11,13]. Four studies have been performed in Asia[9,12,15,18], four in Europe[11,14,16,19], one in North America[17], one in South America[10], and one in Europe and North America[13]. Conventional laparoscopic cholecystectomy was performed with four ports in nine series[9-11,13-15,17-19] and three ports in two[12,16]. Operative indications included benign gallbladder disease operated in an elective setting in all studies, excluding all emergency cases and acute cholecystitis. Body mass index > 30 kg/m2 was considered as a contra-indication in five studies[11-13,16,19], > 40 kg/m2 in one study[17] and previous upper-GI surgery in eight studies[9,11-13,15,16,18,19]. Repartition of the studies according to Jadad score is presented in Figure 2. No studies were rated as high quality (≥ 4 points). The median follow-up was 1 mo (range 0.03-18 mo).
Figure 2.
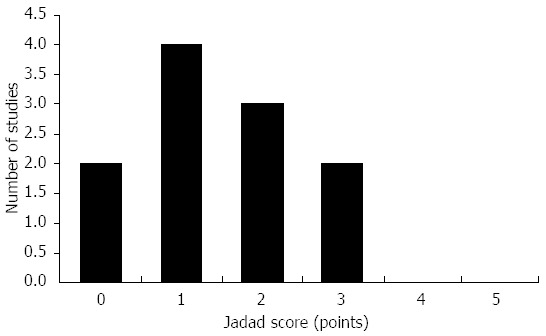
Repartition of the studies according to Jadad score.
The incidence of BDI was 0.4% for SPLC, compared to 0% for CLC (OR = 4.5), but the difference was not statistically different (P = 0.36, 95%CI: 0.22-96). The heterogeneity was zero (χ2 = 0.00, df = 1, P = 0.95; I2 = 0%). Of note, only two studies including 148 patients contributed to the analysis, while the remaining nine studies were not included because no events were observed in both groups. Forrest plots are presented in Figure 3A.
Figure 3.
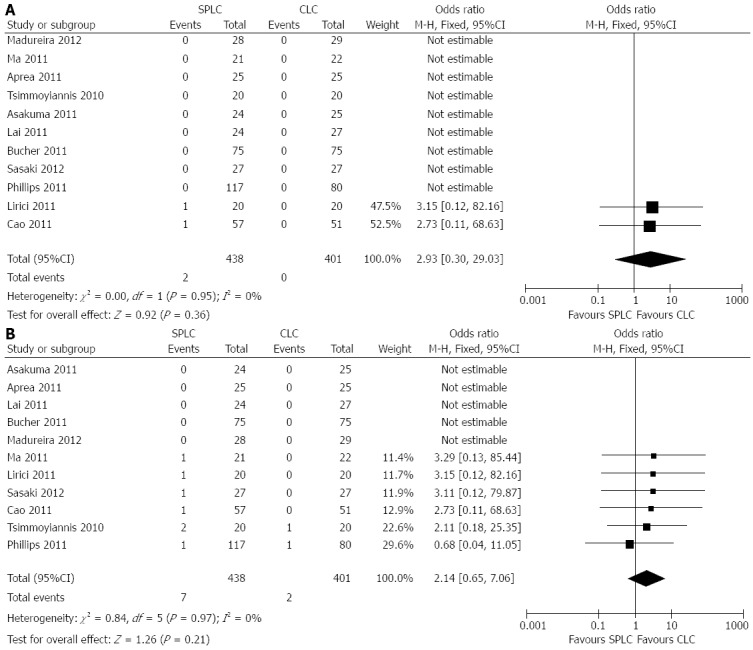
Forest plot. A: Outcome: BDI; B: Outcome: Overall biliary complication. SPLC: Single-port laparoscopic cholecystectomy; BDI: Bile duct injuries; CLC: Conventional laparoscopic cholecystectomy.
The incidence of overall biliary complication was also higher for SPLC compared to CLC with 1.6% vs 0.5% (OR = 3.2), but again, the difference did not reached statistically significance (P = 0.21, 95%CI: 0.66-15). The heterogeneity was zero (χ2 = 0.84; I2 = 0%). Six studies including 482 patients contributed to the analysis. Five studies were not included because no events were observed in both groups. Forrest plots are presented in Figure 3B.
Three of 11 studies reported a perioperative assessment of the critical view of safety, for a total of 119 patients. The use of intraoperative cholangiography was also described in three studies for a total of 77 patients. The procedure was performed in 100%, 70% and 5% of SPLC patients, respectively.
For the non-randomized reports, 60 studies were included with a total of 3599 patients[20-79]. Fifteen were prospective cohort studies and 45 were purely retrospective. From this survey, 25 BDI were reported. The BDI rate was 0.7% and the overall biliary complication rate was 2%. The distribution of BDI according to the Strasberg classification[2] is presented in Figure 4; 12/25 cases of BDI were type-A injuries, and 5/25 were reported, but not specified otherwise. The overall surgical complication rate was 5%. One third (62/180) of them were related to the surgical site (seroma, hematoma, infection, hernia). In particular, 18 postoperative hernias were reported (overall hernia rate of 0.5%). The median follow-up of patients was 2 mo (range 0.03-24 mo) (Table 1).
Figure 4.
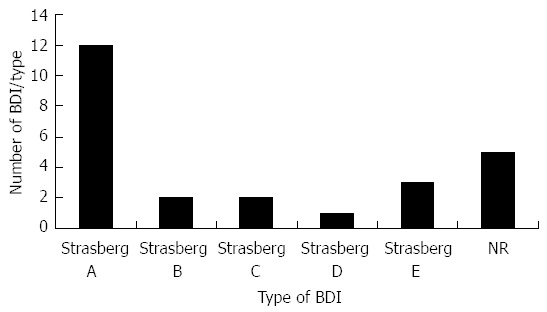
Repartition of the typeof bile duct injuries. BDI: Bile duct injuries.
Table 1.
Data of the non-randomized trials
| Serie | Year | n | BDI | Overall compl |
| Cuesta et al[20] | 2008 | 10 | 0 | 0 |
| Palanivelu et al[21] | 2008 | 10 | 1 | 2 |
| Rao et al[22] | 2008 | 20 | 0 | 0 |
| Hodgett et al[23] | 2009 | 29 | 0 | 3 |
| Hong et al[24] | 2009 | 15 | 0 | 0 |
| Kravetz et al[25] | 2009 | 20 | 0 | 0 |
| Kuon Lee et al[26] | 2009 | 37 | 1 | 2 |
| Langwieler et al[27] | 2009 | 14 | 0 | 0 |
| Merchant et al[28] | 2009 | 21 | 0 | 0 |
| Philipp et al[29] | 2009 | 29 | 0 | 6 |
| Podolsky et al[30] | 2009 | 15 | 0 | 3 |
| Tacchino et al[31] | 2009 | 12 | 0 | 2 |
| Vidal et al[32] | 2009 | 19 | 0 | 0 |
| Zhu et al[33] | 2009 | 10 | 0 | 0 |
| Garijo Alvarez et al[34] | 2010 | 30 | 1 | 3 |
| Brody et al[35] | 2010 | 56 | 0 | 2 |
| Carr et al[36] | 2010 | 60 | 0 | 4 |
| Chow et al[37] | 2010 | 41 | 1 | 1 |
| Curcillo et al[38] | 2010 | 297 | 1 | 26 |
| Edwards et al[39] | 2010 | 80 | 3 | 7 |
| Elsey et al[40] | 2010 | 238 | 0 | 5 |
| Erbella et al[41] | 2010 | 100 | 0 | 0 |
| Fronza et al[42] | 2010 | 25 | 0 | 3 |
| Fumagalli et al[43] | 2010 | 21 | 0 | 2 |
| Hu et al[44] | 2010 | 32 | 0 | 0 |
| Ito et al[45] | 2010 | 31 | 0 | 0 |
| Rawlings et al[46] | 2010 | 54 | 0 | 2 |
| Rivas et al[47] | 2010 | 100 | 1 | 1 |
| Roberts et al[48] | 2010 | 56 | 2 | 3 |
| Romanelli et al[49] | 2010 | 22 | 0 | 1 |
| Roy et al[50] | 2010 | 50 | 1 | 2 |
| Schlager et al[51] | 2010 | 20 | 1 | 1 |
| Kim et al[52] | 2010 | 56 | 1 | 2 |
| Yu et al[53] | 2010 | 33 | 0 | 0 |
| Duron et al[54] | 2011 | 43 | 0 | 0 |
| Han et al[55] | 2011 | 150 | 2 | 15 |
| Jacob et al[56] | 2011 | 36 | 1 | 2 |
| Khambaty et al[57] | 2011 | 81 | 0 | 0 |
| Kilian et al[58] | 2011 | 16 | 0 | 0 |
| Krajinovic et al[59] | 2011 | 50 | 0 | 5 |
| Kupcsulik et al[60] | 2011 | 30 | 0 | 1 |
| Li et al[61] | 2011 | 51 | 0 | 8 |
| Mesas Burgos et al[62] | 2011 | 10 | 0 | 0 |
| Mutter et al[63] | 2011 | 61 | 0 | 0 |
| Prasad et al[64] | 2011 | 100 | 0 | 0 |
| Qiu et al[65] | 2011 | 56 | 0 | 3 |
| Raakow et al[66] | 2011 | 200 | 2 | 11 |
| Rup et al[67] | 2011 | 101 | 0 | 5 |
| Vermulapalli et al[68] | 2011 | 205 | 3 | 9 |
| Vrzgula et al[69] | 2011 | 100 | 1 | 5 |
| Wen et al[70] | 2011 | 50 | 0 | 2 |
| Wu et al[71] | 2011 | 100 | 1 | 3 |
| El-geidie et al[72] | 2012 | 67 | 0 | 1 |
| Feinberg et al[73] | 2012 | 50 | 0 | 2 |
| Kehagias et al[74] | 2012 | 60 | 0 | 0 |
| Koo et al[75] | 2012 | 100 | 0 | 6 |
| Oruc et al[76] | 2012 | 25 | 0 | 1 |
| Sasaki et al[77] | 2012 | 114 | 1 | 10 |
| Wong et al[78] | 2012 | 20 | 0 | 1 |
| Yeo et al[79] | 2012 | 60 | 1 | 7 |
| Total | 3599 | 26 | 180 | |
| 0.7% | 5.0% |
BDI: Bile duct injuries.
DISCUSSION
This meta-analysis assessed the risk of BDI and other biliary complications of single port access cholecystectomy; and compared it to conventional laparoscopic cholecystectomy. The analysis of the current literature revealed an increased rate for BDI of 0.4% and other biliary complications (1.6%) compared to conventional laparoscopic cholecystectomy (0%, 0.5% respectively). However, the differences found were not statistically significant.
Cautious interpretation is mandatory since many limitations impact on these results. Only two series contributed to the analysis of the BDI rate[11,12] and this is strictly not enough to build a statistically valid analysis. Moreover, the quality of these RCT was low, as Jadad scores were not above three, as illustrated in Figure 2. For example, still many investigators use envelope-based randomization technique, and/or blinding is not systematically performed. As stated by Baum[80], overcoming the ongoing allegation that research in surgery is not more than a “comic opera” requires that the surgical community has to make efforts to realize high quality trials. An important shortcoming of published series is the lack of a long-term follow-up, meaning that late occurring bile duct complications may be underreported. Only three studies reported a follow-up of ≥ 6 mo[10,13,18]. One third of the reports described follow-up of ≤ 2 wk. Of greatest relevance, even after pooled analysis, is that few patients could be satisfactorily included in the meta-analysis. This is probably the main limitation of our current review. Indeed, since the incidence of BDI is < 1%, large patient numbers are needed to detect the true incidences and its differences. A power calculation based on previous retrospective data[6] revealed a total of 14048 patients would be needed in order to detect a statistically significant difference in terms of BDI rate. This means that all RCT included in this review were clearly underpowered and sample sizes were too small to assess events with a low incidence. As seen with historical comparisons between laparoscopic and open cholecystectomy, RCT will possibly never answer this thorny issue and a larger international prospective database will be more appropriate in this setting.
Unable to assess clearly the safety issue of SPLC based on the meta-analysis, we decided to perform a second enquiry including larger non-randomized prospective and retrospective studies[20-79] in order to increase the sample size, accepting a lower grade of evidence and a higher risk of bias. The incidence of BDI was then found to be as high as 0.7%, three-times greater than the majority of recent large reviews concerning conventional laparoscopy[81-83]. This result was slightly lower than the rate reported by Joseph et al[6] in their analysis, probably due to a larger sample size and more recent included series. Ominously, one third (8/25) of the BDI reported in our retrospective review were Strasberg type-B or more, indicating a possible tendency for more complex injuries (Figure 4). This aspect could be underestimated, as 20% of BDI were not described or classified by the authors.
Being aware of a potentially increased rate of BDI, different strategies have been proposed to decrease this unacceptably high risk. Only three out of eleven studies used IOC, with suboptimal technical success rate (62%, 77/124 attempts)[14,16,18]. This may be explained by the need of precision and dexterity required to perform IOC, both lacking in SPLC setting. However, the true impact of this aspect remains unclear, as the discussion on the role of IOC during cholecystectomy is a never-ending story[84,85]. Although described for many years as a critical step to limit BDI during CLC, the use of the so-called “critical view of safety” was clearly reported as a sine qua non condition before clipping and dividing the cystic duct in three trials only[11,14,18]. Most often, this was done by the exchange of the dissecting tools for an extra-grasper, in order to gain the right exposure.
Finally, more attention should be paid by the surgeons in critically evaluating their experience with SPLC and in defining the criteria for safety. This aspect is still clearly inadequate in the current literature, as eight studies of the retrospective pool concluded that SPLC was safe, while reporting BDI or increased overall complication rates. Moreover, the hypothesis that the avoidance of 5 mm trocars as in SPLC is of significant clinical benefit was challenged by no-one.
In conclusion, the BDI rate during SPLC seems to be comparable to standard CLC at first sight, but the overall quality of RCT remains low, failing to present any convincing evidence thus far. Larger retrospective data confirm the doubt about the safety of these procedures. Based on the current evidence, SPLC cannot currently be recommended as standard technique for laparoscopic cholecystectomy.
ACKNOWLEDGMENTS
Dr Michael Cotton made a complete revision of our manuscript, looking at language accuracy.
COMMENTS
Background
Single port laparoscopic cholecystectomy (SPLC) is a new technical refinement of endoscopic surgery, which has emerged more than five years ago. The basic concept of laparoscopy remains intact, but all the instruments are introduced in the abdominal cavity through one single site (usually the umbilicus, but other locations have also been described). The goal of this modification is to decrease the surgical trauma on the abdominal wall, by decreasing the number of necessary ports. On the other hand, due to the loss of triangulation between the instruments, this technique appears technically more difficult to perform.
Research frontiers
Early in its use, this technique was used to perform cholecystectomy. After many years of practice, literature failed to shows important clinical advantages (in terms of pain reduction, length of hospital stay and cosmetic results), when compared to conventional laparoscopic cholecystectomy.
Innovations and breakthroughs
Inadvertent events after SPLC have already largely been covered in other meta-analyses. They concluded that the complication rate was similar between this approach, when compared to conventional laparoscopy. However, these studies were not specifically focused on bile duct injuries. Because this type of complication carries a much more significant potential of decreased quality of life and even mortality, authors considered that safety of SPLC should be evaluated in the light of bile duct injuries (BDI) rate, instead of overall complication rate.
Applications
As long as no stronger evidence concerning biliary safety is provided, SPLC cannot currently be recommended as standard technique for laparoscopic cholecystectomy. It appears mandatory that future studies should focus on longer follow-up of the patients. Owing to the relatively low incidence of complications, it seems evident that only large prospective nationwide cohort studies will be adequate to meet the endpoint of biliary safety. Randomized controlled trials will invariably fail to enroll enough patients to delineate such a small difference.
Peer review
Two peer reviewers contributed to the revision of this manuscript. They recognized that this serious complication should be carefully assessed, before considering a wide acceptation of this new surgical approach. If the conclusion of this manuscript is that literature failed to close the debate, this does not imply a rejection of this new technique. On the contrary, more efforts should be made to continue evaluating SPLC in the light of biliary complications. According to their comments, details on the type of BDI were added. In particular, the distribution of these complications, according to Strasberg classification, was detailed in the results and discussed in the conclusion. Moreover, more information was given concerning the distribution of overall complications.
Footnotes
P- Reviewers: Sandblom G, Wang DS S- Editor: Gou SX L- Editor: A E- Editor: Ma S
References
- 1.Greaves N, Nicholson J. Single incision laparoscopic surgery in general surgery: a review. Ann R Coll Surg Engl. 2011;93:437–440. doi: 10.1308/003588411X590358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–125. [PubMed] [Google Scholar]
- 3.McMahon AJ, Fullarton G, Baxter JN, O’Dwyer PJ. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg. 1995;82:307–313. doi: 10.1002/bjs.1800820308. [DOI] [PubMed] [Google Scholar]
- 4.Sajid MS, Ladwa N, Kalra L, Hutson KK, Singh KK, Sayegh M. Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: meta-analysis and systematic review of randomized controlled trials. World J Surg. 2012;36:2644–2653. doi: 10.1007/s00268-012-1719-5. [DOI] [PubMed] [Google Scholar]
- 5.Trastulli S, Cirocchi R, Desiderio J, Guarino S, Santoro A, Parisi A, Noya G, Boselli C. Systematic review and meta-analysis of randomized clinical trials comparing single-incision versus conventional laparoscopic cholecystectomy. Br J Surg. 2013;100:191–208. doi: 10.1002/bjs.8937. [DOI] [PubMed] [Google Scholar]
- 6.Joseph M, Phillips MR, Farrell TM, Rupp CC. Single incision laparoscopic cholecystectomy is associated with a higher bile duct injury rate: a review and a word of caution. Ann Surg. 2012;256:1–6. doi: 10.1097/SLA.0b013e3182583fde. [DOI] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 9.Sasaki A, Ogawa M, Tono C, Obara S, Hosoi N, Wakabayashi G. Single-port versus multiport laparoscopic cholecystectomy: a prospective randomized clinical trial. Surg Laparosc Endosc Percutan Tech. 2012;22:396–399. doi: 10.1097/SLE.0b013e3182631a9a. [DOI] [PubMed] [Google Scholar]
- 10.Madureira FA, Manso JE, Madureira Fo D, Iglesias AC. Randomized clinical study for assessment of incision characteristics and pain associated with LESS versus laparoscopic cholecystectomy. Surg Endosc. 2013;27:1009–1015. doi: 10.1007/s00464-012-2556-1. [DOI] [PubMed] [Google Scholar]
- 11.Lirici MM, Califano AD, Angelini P, Corcione F. Laparo-endoscopic single site cholecystectomy versus standard laparoscopic cholecystectomy: results of a pilot randomized trial. Am J Surg. 2011;202:45–52. doi: 10.1016/j.amjsurg.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 12.Cao ZG, Cai W, Qin MF, Zhao HZ, Yue P, Li Y. Randomized clinical trial of single-incision versus conventional laparoscopic cholecystectomy: short-term operative outcomes. Surg Laparosc Endosc Percutan Tech. 2011;21:311–313. doi: 10.1097/SLE.0b013e31822cfacd. [DOI] [PubMed] [Google Scholar]
- 13.Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, DeNoto G, Rivas H, Islam A, Soper N, Gecelter G, et al. Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc. 2012;26:1296–1303. doi: 10.1007/s00464-011-2028-z. [DOI] [PubMed] [Google Scholar]
- 14.Bucher P, Pugin F, Buchs NC, Ostermann S, Morel P. Randomized clinical trial of laparoendoscopic single-site versus conventional laparoscopic cholecystectomy. Br J Surg. 2011;98:1695–1702. doi: 10.1002/bjs.7689. [DOI] [PubMed] [Google Scholar]
- 15.Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK. Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg. 2011;202:254–258. doi: 10.1016/j.amjsurg.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 16.Aprea G, Coppola Bottazzi E, Guida F, Masone S, Persico G. Laparoendoscopic single site (LESS) versus classic video-laparoscopic cholecystectomy: a randomized prospective study. J Surg Res. 2011;166:e109–e112. doi: 10.1016/j.jss.2010.11.885. [DOI] [PubMed] [Google Scholar]
- 17.Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S. Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg. 2011;254:22–27. doi: 10.1097/SLA.0b013e3182192f89. [DOI] [PubMed] [Google Scholar]
- 18.Asakuma M, Hayashi M, Komeda K, Shimizu T, Hirokawa F, Miyamoto Y, Okuda J, Tanigawa N. Impact of single-port cholecystectomy on postoperative pain. Br J Surg. 2011;98:991–995. doi: 10.1002/bjs.7486. [DOI] [PubMed] [Google Scholar]
- 19.Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2010;24:1842–1848. doi: 10.1007/s00464-010-0887-3. [DOI] [PubMed] [Google Scholar]
- 20.Cuesta MA, Berends F, Veenhof AA. The “invisible cholecystectomy”: A transumbilical laparoscopic operation without a scar. Surg Endosc. 2008;22:1211–1213. doi: 10.1007/s00464-007-9588-y. [DOI] [PubMed] [Google Scholar]
- 21.Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Praveenraj P. Transumbilical flexible endoscopic cholecystectomy in humans: first feasibility study using a hybrid technique. Endoscopy. 2008;40:428–431. doi: 10.1055/s-2007-995742. [DOI] [PubMed] [Google Scholar]
- 22.Rao PP, Bhagwat SM, Rane A, Rao PP. The feasibility of single port laparoscopic cholecystectomy: a pilot study of 20 cases. HPB (Oxford) 2008;10:336–340. doi: 10.1080/13651820802276622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS. Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg. 2009;13:188–192. doi: 10.1007/s11605-008-0735-0. [DOI] [PubMed] [Google Scholar]
- 24.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy : scarless cholecystectomy. Surg Endosc. 2009;23:1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 25.Kravetz AJ, Iddings D, Basson MD, Kia MA. The learning curve with single-port cholecystectomy. JSLS. 2009;13:332–336. [PMC free article] [PubMed] [Google Scholar]
- 26.Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech A. 2009;19:495–499. doi: 10.1089/lap.2008.0424. [DOI] [PubMed] [Google Scholar]
- 27.Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009;23:1138–1141. doi: 10.1007/s00464-009-0389-3. [DOI] [PubMed] [Google Scholar]
- 28.Merchant AM, Cook MW, White BC, Davis SS, Sweeney JF, Lin E. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS) J Gastrointest Surg. 2009;13:159–162. doi: 10.1007/s11605-008-0737-y. [DOI] [PubMed] [Google Scholar]
- 29.Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009;209:632–637. doi: 10.1016/j.jamcollsurg.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 30.Podolsky ER, Rottman SJ, Curcillo PG. Single port access (SPA) cholecystectomy: two year follow-up. JSLS. 2009;13:528–535. doi: 10.4293/108680809X12589998404245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009;23:896–899. doi: 10.1007/s00464-008-0147-y. [DOI] [PubMed] [Google Scholar]
- 32.Vidal O, Valentini M, Espert JJ, Ginesta C, Jimeno J, Martinez A, Benarroch G, Garcia-Valdecasas JC. Laparoendoscopic single-site cholecystectomy: a safe and reproducible alternative. J Laparoendosc Adv Surg Tech A. 2009;19:599–602. doi: 10.1089/lap.2009.0205. [DOI] [PubMed] [Google Scholar]
- 33.Zhu JF, Hu H, Ma YZ, Xu MZ. Totally transumbilical endoscopic cholecystectomy without visible abdominal scar using improved instruments. Surg Endosc. 2009;23:1781–1784. doi: 10.1007/s00464-008-0228-y. [DOI] [PubMed] [Google Scholar]
- 34.Garijo Alvarez J, Sánchez López JD, González Elosua T, Gascón Hove M, García-Sancho Téllez L, Del Castillo Diez F, Torres Jiménez J. [Laparoscopic transumbilical cholecystectomy. Results with the gel device and literature review] Cir Esp. 2010;87:293–298. doi: 10.1016/j.ciresp.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 35.Brody F, Vaziri K, Kasza J, Edwards C. Single incision laparoscopic cholecystectomy. J Am Coll Surg. 2010;210:e9–e13. doi: 10.1016/j.jamcollsurg.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 36.Carr A, Bhavaraju A, Goza J, Wilson R. Initial experience with single-incision laparoscopic cholecystectomy. Am Surg. 2010;76:703–707. [PubMed] [Google Scholar]
- 37.Chow A, Purkayastha S, Aziz O, Pefanis D, Paraskeva P. Single-incision laparoscopic surgery for cholecystectomy: a retrospective comparison with 4-port laparoscopic cholecystectomy. Arch Surg. 2010;145:1187–1191. doi: 10.1001/archsurg.2010.267. [DOI] [PubMed] [Google Scholar]
- 38.Curcillo PG, Wu AS, Podolsky ER, Graybeal C, Katkhouda N, Saenz A, Dunham R, Fendley S, Neff M, Copper C, et al. Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc. 2010;24:1854–1860. doi: 10.1007/s00464-009-0856-x. [DOI] [PubMed] [Google Scholar]
- 39.Edwards C, Bradshaw A, Ahearne P, Dematos P, Humble T, Johnson R, Mauterer D, Soosaar P. Single-incision laparoscopic cholecystectomy is feasible: initial experience with 80 cases. Surg Endosc. 2010;24:2241–2247. doi: 10.1007/s00464-010-0943-z. [DOI] [PubMed] [Google Scholar]
- 40.Elsey JK, Feliciano DV. Initial experience with single-incision laparoscopic cholecystectomy. J Am Coll Surg. 2010;210:620–64, 620-64. doi: 10.1016/j.jamcollsurg.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 41.Erbella J, Bunch GM. Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc. 2010;24:1958–1961. doi: 10.1007/s00464-010-0886-4. [DOI] [PubMed] [Google Scholar]
- 42.Fronza JS, Linn JG, Nagle AP, Soper NJ. A single institution’s experience with single incision cholecystectomy compared to standard laparoscopic cholecystectomy. Surgery. 2010;148:731–734; discussion 734-736. doi: 10.1016/j.surg.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 43.Fumagalli U, Verrusio C, Elmore U, Massaron S, Rosati R. Preliminary results of transumbilical single-port laparoscopic cholecystectomy. Updates Surg. 2010;62:105–109. doi: 10.1007/s13304-010-0024-9. [DOI] [PubMed] [Google Scholar]
- 44.Hu H, Zhu J, Wang W, Huang A. Optimized transumbilical endoscopic cholecystectomy: a randomized comparison of two procedures. Surg Endosc. 2010;24:1080–1084. doi: 10.1007/s00464-009-0730-x. [DOI] [PubMed] [Google Scholar]
- 45.Ito M, Asano Y, Horiguchi A, Shimizu T, Yamamoto T, Uyama I, Miyakawa S. Cholecystectomy using single-incision laparoscopic surgery with a new SILS port. J Hepatobiliary Pancreat Sci. 2010;17:688–691. doi: 10.1007/s00534-010-0266-4. [DOI] [PubMed] [Google Scholar]
- 46.Rawlings A, Hodgett SE, Matthews BD, Strasberg SM, Quasebarth M, Brunt LM. Single-incision laparoscopic cholecystectomy: initial experience with critical view of safety dissection and routine intraoperative cholangiography. J Am Coll Surg. 2010;211:1–7. doi: 10.1016/j.jamcollsurg.2010.02.038. [DOI] [PubMed] [Google Scholar]
- 47.Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010;24:1403–1412. doi: 10.1007/s00464-009-0786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roberts KE, Solomon D, Duffy AJ, Bell RL. Single-incision laparoscopic cholecystectomy: a surgeon’s initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg. 2010;14:506–510. doi: 10.1007/s11605-009-1116-z. [DOI] [PubMed] [Google Scholar]
- 49.Romanelli JR, Roshek TB, Lynn DC, Earle DB. Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc. 2010;24:1374–1379. doi: 10.1007/s00464-009-0781-z. [DOI] [PubMed] [Google Scholar]
- 50.Roy P, De A. Transumbilical multiple-port laparoscopic cholecystectomy (TUMP-LC): a prospective analysis of 50 initial patients. J Laparoendosc Adv Surg Tech A. 2010;20:211–217. doi: 10.1089/lap.2009.0395. [DOI] [PubMed] [Google Scholar]
- 51.Schlager A, Khalaileh A, Shussman N, Elazary R, Keidar A, Pikarsky AJ, Ben-Shushan A, Shibolet O, Horgan S, Talamini M, et al. Providing more through less: current methods of retraction in SIMIS and NOTES cholecystectomy. Surg Endosc. 2010;24:1542–1546. doi: 10.1007/s00464-009-0807-6. [DOI] [PubMed] [Google Scholar]
- 52.Kim JH, You YK, Hong TH, Lee SK, Park JH, Yoon YC, Kim JG. Single-port laparoscopic cholecystectomy: A comparative study in 106 initial cases. Asian J Endosc Surg. 2010;3:101–152. [Google Scholar]
- 53.Yu WB, Zhang GY, Li F, Yang QY, Hu SY. Transumbilical single port laparoscopic cholecystectomy with a simple technique: initial experience of 33 cases. Minim Invasive Ther Allied Technol. 2010;19:340–344. doi: 10.3109/13645706.2010.527772. [DOI] [PubMed] [Google Scholar]
- 54.Duron VP, Nicastri GR, Gill PS. Novel technique for a single-incision laparoscopic surgery (SILS) approach to cholecystectomy: single-institution case series. Surg Endosc. 2011;25:1666–1671. doi: 10.1007/s00464-010-1374-6. [DOI] [PubMed] [Google Scholar]
- 55.Han HJ, Choi SB, Kim WB, Choi SY. Single-incision multiport laparoscopic cholecystectomy: things to overcome. Arch Surg. 2011;146:68–73. doi: 10.1001/archsurg.2010.287. [DOI] [PubMed] [Google Scholar]
- 56.Jacob D, Raakow R. Single-port versus multi-port cholecystectomy for patients with acute cholecystitis: a retrospective comparative analysis. Hepatobiliary Pancreat Dis Int. 2011;10:521–525. doi: 10.1016/s1499-3872(11)60088-x. [DOI] [PubMed] [Google Scholar]
- 57.Khambaty F, Brody F, Vaziri K, Edwards C. Laparoscopic versus single-incision cholecystectomy. World J Surg. 2011;35:967–972. doi: 10.1007/s00268-011-0998-6. [DOI] [PubMed] [Google Scholar]
- 58.Kilian M, Raue W, Menenakos C, Wassersleben B, Hartmann J. Transvaginal-hybrid vs. single-port-access vs. ‘conventional’ laparoscopic cholecystectomy: a prospective observational study. Langenbecks Arch Surg. 2011;396:709–715. doi: 10.1007/s00423-011-0769-8. [DOI] [PubMed] [Google Scholar]
- 59.Krajinovic K, Ickrath P, Germer CT, Reibetanz J. Trocar-site hernia after single-port cholecystectomy: not an exceptional complication? J Laparoendosc Adv Surg Tech A. 2011;21:919–921. doi: 10.1089/lap.2011.0292. [DOI] [PubMed] [Google Scholar]
- 60.Kupcsulik P, Szlávik R, Nehéz L, Lukovich P. [Single port transumbilical cholecystectomy [SILS] -- 30 non-selected cases] Magy Seb. 2011;64:69–73. doi: 10.1556/MaSeb.64.2011.2.3. [DOI] [PubMed] [Google Scholar]
- 61.Lill S, Karvonen J, Hämäläinen M, Falenius V, Rantala A, Grönroos JM, Ovaska J. Adoption of single incision laparoscopic cholecystectomy in small-volume hospitals: initial experiences of 51 consecutive procedures. Scand J Surg. 2011;100:164–168. doi: 10.1177/145749691110000305. [DOI] [PubMed] [Google Scholar]
- 62.Mesas Burgos C, Ghaffarpour N, Almström M. Single-site incision laparoscopic cholecystectomy in children: a single-center initial experience. J Pediatr Surg. 2011;46:2421–2425. doi: 10.1016/j.jpedsurg.2011.09.052. [DOI] [PubMed] [Google Scholar]
- 63.Mutter D, Callari C, Diana M, Dallemagne B, Leroy J, Marescaux J. Single port laparoscopic cholecystectomy: which technique, which surgeon, for which patient? A study of the implementation in a teaching hospital. J Hepatobiliary Pancreat Sci. 2011;18:453–457. doi: 10.1007/s00534-010-0348-3. [DOI] [PubMed] [Google Scholar]
- 64.Prasad A, Mukherjee KA, Kaul S, Kaur M. Postoperative pain after cholecystectomy: Conventional laparoscopy versus single-incision laparoscopic surgery. J Minim Access Surg. 2011;7:24–27. doi: 10.4103/0972-9941.72370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Qiu Z, Sun J, Pu Y, Jiang T, Cao J, Wu W. Learning curve of transumbilical single incision laparoscopic cholecystectomy (SILS): a preliminary study of 80 selected patients with benign gallbladder diseases. World J Surg. 2011;35:2092–2101. doi: 10.1007/s00268-011-1144-1. [DOI] [PubMed] [Google Scholar]
- 66.Raakow R, Jacob DA. Single-Incision Cholecystectomy in about 200 Patients. Minim Invasive Surg. 2011;2011:915735. doi: 10.1155/2011/915735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rupp CC, Farrell TM, Meyer AA. Single incision laparoscopic cholecystectomy using a “two-port” technique is safe and feasible: experience in 101 consecutive patients. Am Surg. 2011;77:916–921. [PubMed] [Google Scholar]
- 68.Vemulapalli P, Agaba EA, Camacho D. Single incision laparoscopic cholecystectomy: a single center experience. Int J Surg. 2011;9:410–413. doi: 10.1016/j.ijsu.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 69.Vrzgula A, Pribula V, Krajnicák R, Müdry M, Vasilenko T. [SILS cholecystectomy--analysis of the first 100 patients] Rozhl Chir. 2011;90:440–445. [PubMed] [Google Scholar]
- 70.Wen KC, Lin KY, Chen Y, Lin YF, Wen KS, Uen YH. Feasibility of single-port laparoscopic cholecystectomy using a homemade laparoscopic port: a clinical report of 50 cases. Surg Endosc. 2011;25:879–882. doi: 10.1007/s00464-010-1287-4. [DOI] [PubMed] [Google Scholar]
- 71.Wu SD, Han JY, Tian Y. Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: a retrospective comparative study. J Laparoendosc Adv Surg Tech A. 2011;21:25–28. doi: 10.1089/lap.2010.0377. [DOI] [PubMed] [Google Scholar]
- 72.El-Geidie AA. Single-incision laparoscopic cholecystectomy (SILC) using harmonic scalpel. J Surg Res. 2012;176:50–54. doi: 10.1016/j.jss.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 73.Feinberg EJ, Agaba E, Feinberg ML, Camacho D, Vemulapalli P. Single-incision laparoscopic cholecystectomy learning curve experience seen in a single institution. Surg Laparosc Endosc Percutan Tech. 2012;22:114–117. doi: 10.1097/SLE.0b013e31824799ef. [DOI] [PubMed] [Google Scholar]
- 74.Kehagias I, Karamanakos SN, Markopoulos GA, Kalfarentzos F. Benefits and drawbacks of SILS cholecystectomy: a report of 60 SILS cholecystectomies with conventional instrumentation from an academic center. Surg Innov. 2012;19:438–445. doi: 10.1177/1553350612438411. [DOI] [PubMed] [Google Scholar]
- 75.Koo EJ, Youn SH, Baek YH, Roh YH, Choi HJ, Kim YH, Jung GJ. Review of 100 cases of single port laparoscopic cholecystectomy. J Korean Surg Soc. 2012;82:179–184. doi: 10.4174/jkss.2012.82.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oruc MT, Ugurlu MU, Boyacioglu Z. Transumbilical multiple-port laparoscopic cholecystectomy using standard laparoscopic instruments. Minim Invasive Ther Allied Technol. 2012;21:423–428. doi: 10.3109/13645706.2011.649039. [DOI] [PubMed] [Google Scholar]
- 77.Sasaki K, Watanabe G, Matsuda M, Hashimoto M. Single-incision laparoscopic cholecystectomy: comparison analysis of feasibility and safety. Surg Laparosc Endosc Percutan Tech. 2012;22:108–113. doi: 10.1097/SLE.0b013e3182456e3b. [DOI] [PubMed] [Google Scholar]
- 78.Wong JS, Cheung YS, Fong KW, Chong CC, Lee KF, Wong J, Lai PB. Comparison of postoperative pain between single-incision laparoscopic cholecystectomy and conventional laparoscopic cholecystectomy: prospective case-control study. Surg Laparosc Endosc Percutan Tech. 2012;22:25–28. doi: 10.1097/SLE.0b013e318242ea44. [DOI] [PubMed] [Google Scholar]
- 79.Yeo D, Mackay S, Martin D. Single-incision laparoscopic cholecystectomy with routine intraoperative cholangiography and common bile duct exploration via the umbilical port. Surg Endosc. 2012;26:1122–1127. doi: 10.1007/s00464-011-2009-2. [DOI] [PubMed] [Google Scholar]
- 80.Baum M. Reflections on randomised controlled trials in surgery. Lancet. 1999;353 Suppl 1:SI6–SI8. doi: 10.1016/s0140-6736(99)90220-9. [DOI] [PubMed] [Google Scholar]
- 81.Chuang KI, Corley D, Postlethwaite DA, Merchant M, Harris HW. Does increased experience with laparoscopic cholecystectomy yield more complex bile duct injuries? Am J Surg. 2012;203:480–487. doi: 10.1016/j.amjsurg.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 82.Dolan JP, Diggs BS, Sheppard BC, Hunter JG. Ten-year trend in the national volume of bile duct injuries requiring operative repair. Surg Endosc. 2005;19:967–973. doi: 10.1007/s00464-004-8942-6. [DOI] [PubMed] [Google Scholar]
- 83.Giger U, Ouaissi M, Schmitz SF, Krähenbühl S, Krähenbühl L. Bile duct injury and use of cholangiography during laparoscopic cholecystectomy. Br J Surg. 2011;98:391–396. doi: 10.1002/bjs.7335. [DOI] [PubMed] [Google Scholar]
- 84.Flum DR, Flowers C, Veenstra DL. A cost-effectiveness analysis of intraoperative cholangiography in the prevention of bile duct injury during laparoscopic cholecystectomy. J Am Coll Surg. 2003;196:385–393. doi: 10.1016/S1072-7515(02)01806-9. [DOI] [PubMed] [Google Scholar]
- 85.Ausania F, Holmes LR, Ausania F, Iype S, Ricci P, White SA. Intraoperative cholangiography in the laparoscopic cholecystectomy era: why are we still debating? Surg Endosc. 2012;26:1193–1200. doi: 10.1007/s00464-012-2241-4. [DOI] [PubMed] [Google Scholar]


