Abstract
AIM: To assess the fecal immunochemical test (FIT) accuracy for colorectal cancer (CRC) and advanced neoplasia (AN) detection in CRC screening.
METHODS: We performed a multicentric, prospective, double blind study of diagnostic tests on asymptomatic average-risk individuals submitted to screening colonoscopy. Two stool samples were collected and the fecal hemoglobin concentration was determined in the first sample (FIT1) and the highest level of both samples (FITmax) using the OC-sensor™. Areas under the curve (AUC) for CRC and AN were calculated. The best FIT1 and FITmax cut-off values for CRC were determined. At this threshold, number needed to scope (NNS) to detect a CRC and an AN and the cost per lesion detected were calculated.
RESULTS: About 779 individuals were included. An AN was found in 97 (12.5%) individuals: a CRC in 5 (0.6%) and an advanced adenoma (≥ 10 mm, villous histology or high grade dysplasia) in 92 (11.9%) subjects. For CRC diagnosis, FIT1 AUC was 0.96 (95%CI: 0.95-0.98) and FITmax AUC was 0.95 (95%CI: 0.93-0.97). For AN, FIT1 and FITmax AUC were similar (0.72, 95%CI: 0.66-0.78 vs 0.73, 95%CI: 0.68-0.79, respectively, P = 0.34). Depending on the number of determinations and the positivity threshold cut-off used sensitivity for AN detection ranged between 28% and 42% and specificity between 91% and 97%. At the best cut-off point for CRC detection (115 ng/mL), the NNS to detect a CRC were 10.2 and 15.8; and the cost per CRC was 1814€ and 2985€ on FIT1 and FITmax strategies respectively. At this threshold the sensitivity, NNS and cost per AN detected were 30%, 1.76, and 306€, in FIT1 strategy, and 36%, 2.26€ and 426€, in FITmax strategy, respectively.
CONCLUSION: Performing two tests does not improve diagnostic accuracy, but increases cost and NNS to detect a lesion.
Keywords: Colorectal neoplasms, Early detection of cancer, Sensitivity and specificity, Adenoma, Occult blood, Cost-benefit analysis
Core tip: Our study has determined fecal immunochemical test (FIT) diagnostic accuracy, number needed to scope and cost per lesion detected in colorectal cancer (CRC) screening programs. FIT is highly sensitive for CRC detection, allowing a drastic reduction in the cost per lesion detected when compared with direct screening colonoscopy. These data are relevant to design CRC screening programs in this setting.
INTRODUCTION
Colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related death[1]. Evidence of effectiveness of CRC screening in average-risk population is available from randomized controlled trials for guaiac fecal occult blood tests[2,3] and sigmoidoscopy[4,5], and it has been shown that it is cost-effective or even cost-saving[6].
Although guaiac fecal occult blood tests are effective in CRC screening, several drawbacks have been described: low sensitivity for advanced colorrectal neoplasia (AN) and need of diet and medication restriction[7]. In contrast, fecal immunochemical tests (FIT) are highly specific for detecting human blood of colonic origin[7], some use an automated analysis for reading test results[7], and they have shown a higher sensitivity and specificity for CRC and AN[8-14]. Despite the superiority of FIT over guaiac based methods, its accuracy in average-risk population screening and the optimal number of stool samples or cut-off level has not been properly assessed. To our knowledge, only four studies (performed on three different cohorts of patients) have assessed the FIT accuracy in average-risk patients who were screened with colonoscopy[13-16].
The COLONPREV study (ClinicalTrials.gov, NCT00906997), designed to compare the efficacy of one-time colonoscopy and biennial FIT for reducing CRC-related mortality at 10 years in asymptomatic, average-risk individuals, offered an ideal framework to develop diagnostic tests studies, as a group of individuals were randomly assigned to colonoscopy screening[17]. So, we performed a prospective, nested study on individuals invited to the COLONPREV study to assess the accuracy of FIT to detect CRC and AN, as well as to establish the optimal number of FIT, the best cut-off value for CRC detection, and the resource consumption per lesion detected.
MATERIALS AND METHODS
Study design
A multicentre, prospective, blinded, cohort study of diagnostic test was performed in three tertiary hospitals in Spain between 1st January 2010 and 30th June 2011, aiming to assess the accuracy of FIT for AN and CRC detection in average-risk population.
Study population
Asymptomatic men and women aged 50 to 69 years, included in the COLONPREV study in Galicia and Euskadi were invited to participate in this diagnostic test study if they were offered a colonoscopy during the inclusion period. Exclusion criteria have been described elsewhere[17] and included personal history of CRC, adenoma or inflammatory bowel disease, family history of hereditary or familial CRC (i.e., > 2 first-degree relatives with CRC or one diagnosed before the age of 60 years), severe comorbidity, previous colectomy, FIT screening in the past 2 years, sigmoidoscopy or colonoscopy within the past 5 years, or symptoms requiring additional work-up. Individuals were also excluded if they did not accept the study or refused to undergo the colonoscopy.
Study interventions
All participants collected 2 stool samples from 2 consecutive days the week before the colonoscopy was scheduled. FIT was assessed using the automated OC-sensor™ (Eiken Chemical Co, Tokyo, Japan), without diet or medication restrictions. Samples were processed as previously described[18]. In each patient fecal hemoglobin (ng/mL of buffer), in the first sample (FIT1) and the highest level of the two samples (FITmax) was determined. Laboratory staff were blinded for the colonoscopy result, and endoscopists performing the colonoscopy were blinded for the FIT result.
Bowel cleansing, sedation and colonoscopy procedure was performed according to the Spanish Guidelines on Quality of Colonoscopy in CRC Screening[19]. Polyps were categorized as non-neoplastic or neoplastic (adenomas). Adenomas of 10 mm or more in size, or with villous architecture (> 25%), or with high-grade dysplasia or intramucosal carcinoma were classified as advanced adenomas. Invasive cancer was considered when malignant cells were observed beyond the muscularis mucosa. Advanced colorectal neoplasia was defined as advanced adenoma or invasive cancer. Tumor staging was performed according to the AJCC classification[20]. Patients were classified according to the most advanced lesion.
Sample size calculation
Reported FIT sensitivity and specificity for AN in asymptomatic individuals was, respectively, 27.1% and 96.1%[21], while in patients undergoing a colonoscopy for any reason, these figures were 50.9%-67% and 88%-91.4%[22,23]. The prevalence of AN in average-risk, asymptomatic individuals ranges from 6.3% to 10.5%[24-27]. Taking these parameters into account, a sample size ranging from 724 to 1350 individuals would provide a 10% accuracy at a 5% bilateral significance level.
Analysis of resources and cost-benefit analysis
For each positivity threshold and strategy, the number of subjects needed to scope (NNS) to detect an AN or a CRC and the direct cost per lesion detected were determined. The analysis costs were calculated on the basis of the published colonoscopy costs in Spain (colonoscopy, 70€; colonoscopy with biopsy, 140€)[28] and FIT determination cost (3.2€).
Other aspects
The study was approved by the Galician Clinical Research Ethics Committee, under resolution dated 28th May 2009 (Code 2009/153). Patients’ clinical histories were accessed for study purposes in accordance with the research protocols laid down by clinical documentation departments. All patients provided written informed consent.
Finally, to design the study and to write this original article the QADAS quality assessment tool for diagnostic tests, the STARD checklist and the STROBE checklist for cohort study were used[29-31].
Statistical analysis
The data were included in a specifically designed database (www.coloncruzer.es). Continuous variables were described using means and standard deviation, and categorical variables by the absolute number and percentage. Comparisons to identify differences in fecal hemoglobin concentrations between groups were performed using non-parametric tests (Mann-Whitney or Krukal-Wallis tests) in quantitative variables. To compare overall diagnostic accuracy for AN and CRC in both FIT1 and FITmax strategies the receiver operating characteristics (ROC) curve were drawn, and the χ2 test for homogeneity of the corresponding area under the curve (AUC) was used. The best cut-off value of FIT1 and FITmax for CRC detection was determined with the Youden index. For each FIT testing strategy, sensitivity, specificity, positive and negative predictive value (PPV, NPV), as well as positive and negative likelihood ratio for the best cut-off and for prestablished positivity thresholds (50, 75, 100, 150 and 200 ng/mL) were calculated. Sensitivity and specificity for AN at the best CRC detection cut-off point was compared with the rest of thresholds using McNemar test[32].
The EPIDAT 3.1 software (Dirección Xeral de Innovación e Xestión da Saúde Pública, Santiago de Compostela, Spain) was used to perform sample size calculation, ROC curves drawings and comparisons. Statistical analyzes were performed using the SPSS statistical software, version 15.0 (SPSS Inc., Chicago, IL, United States). A P value < 0.05 was considered statistically significant.
RESULTS
Baseline characteristics
Overall, 851 subjects enrolled in the COLONPREV study were included in this FIT accuracy study. Fifty-four individuals did not complete the colonoscopy and 18 did not returned the FIT kit, so the evaluable population was 779 individuals: 386 male/393 female, mean age 57.55 ± 4.55 years. Hemoglobin concentration was 58.3 ± 278.4 ng/mL of buffer in the first determination and 57.3 ± 308.5 ng/mL in the second determination.
Invasive carcinoma was detected in 5 (0.6%) individuals (3 TNM I; 1 TNM II, 1 TNM III), advanced adenomas in 92 (11.7%), and non advanced adenomas in 202 (25.9%). Therefore, AN was found in 97 (12.5%) patients. In 480 cases (61.6%) no neoplastic lesion was found; among them 124 had hiperplastic polyps, 6 had an inflammatory polyp, diverticula were found in 92 cases and an ulcerative colitis was detected in one patient.
Diagnostic accuracy of FIT
In patients with invasive CRC, FIT1 and FITmax (998 ± 1075.44, 1257.4 ± 1531.8) were significantly higher than in patients with advanced adenomas (233.14 ± 543.1 vs 325.3 ± 747.7, P = 0.05), non-advanced adenomas (42.4 ± 224.6 vs 76.7 ± 303.5, P < 0.001) or no neoplastic lesions (21.8 ± 150 vs 41.7 ± 216.5, P < 0.001). FIT1 and FITmax were similar in patients with non advanced adenomas and no neoplasms. Patients with CRC or AN had significantly higher FIT1 and FITmax than patients without these lesions (Figure 1).
Figure 1.
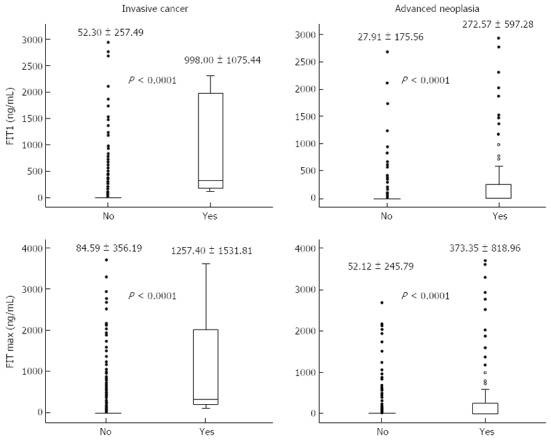
Fecal hemoglobin (ng/mL) according to the most advanced lesion. Values expressed as mean ± SD. Mann-Withney test. FIT: Fecal immunochemical test; FIT1: Fecal hemoglogin concentration in the first stool sample; FITmax: Highest fecal hemoglobin concentration of two stool samples.
Accuracy of FIT1 and FITmax was analyzed using ROC curves (Figure 2). For CRC diagnosis, the AUC of FIT1 was 0.97 (95%CI: 0.94-0.99) and that of FITmax was 0.95 (95%CI: 0.92-0.99). The best cut-off value for CRC diagnosis was 115 ng/mL for both FIT1 and FITmax. For AN diagnosis the AUC of FIT1 was similar to that of FITmax (0.72, 95%CI: 0.66-0.77 vs 0.73, 95%CI: 0.67-0.79, respectively; homogeneity area test P = 0.27). The best cut-off value for AN diagnosis was 8 ng/mL in the FIT1 strategy and 20 ng/mL in the FITmax strategy.
Figure 2.
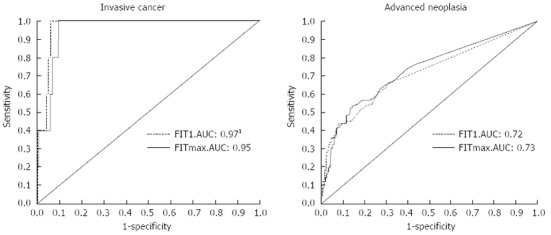
Receiver operating characteristics curves of fecal immunochemical test-1 and -max for advanced neoplasia and invasive cancer. FIT: Fecal immunochemical test; FIT1: Fecal hemoglogin concentration in the first stool sample; FITmax: Highest fecal hemoglobin concentration of two stool samples; AUC: Area under the curve. 1P = 0.034 with respect to FITmax in the homogeneity area test.
Performance characteristics of FIT1 and FITmax
Table 1 describes sensitivity, specificity, PPV, NPV, LLR + and - to detect a CRC at different FIT1 and FITmax positivity thresholds. As shown, both strategies show a high sensitivity and specificity for CRC, although FITmax decreases specificity and PPV, without increasing the sensitivity or NPV. Table 2 describes sensitivity, specificity, PPV, NPV, LLR positive and negative to detect an AN at different FIT1 and FITmax cut-off points. Depending on the number of determinations and the positivity threshold cut-off used sensitivity for AN detection ranged between 28% and 42% and specificity between 91% and 97%. In only one determination strategy, statistically significant differences in specificity between 115 ng/mL, 50 ng/mL (P = 0.001) and 75 ng/mL (P = 0.01) were detected. In FITmax strategy, statistically significant differences in specificity were found between 115 ng/mL, 50 ng/mL (P < 0.001), 75 ng/mL (P = 0.03) and 200 ng/mL (P < 0.001). Finally, in FITmax strategy, we found statistically significant differences in sensitivity between 115 ng/mL, 50 ng/mL (P = 0.03) and 200 ng/mL (P = 0.008).
Table 1.
Performance characteristics of fecal immunochemical test-1 and -max for colorectal cancer detection at different positive thresholds n (%)
| Hemoglobin concentration (ng/mL) | FIT strategy | Individuals with a positive result1 | Sensitivity2 | Specificity2 | Positive predictive value2 | Negative predictive value2 | Positive likelihood ratio2 | Negative likelihood ratio2 |
| 50 | FIT13 | 67 (8.6) | 100 (90-100) | 92 (90-94) | 7 (0-15) | 100 (100-100) | 12.48 (9.83-15.85) | - |
| FITmax4 | 101 (13.0) | 100 (90-100) | 88.60 (85-90) | 5 (0-10) | 100 (100-100) | 8.06 (6.69-9.72) | - | |
| 75 | FIT13 | 61 (7.8) | 100 (90-100) | 93 (91-95) | 8 (0-16) | 100 (100-100) | 13.82 (10.74-17) | - |
| FITmax4 | 89 (11.4) | 100 (90-100) | 89 (87-91) | 6 (0-11) | 100 (100-100) | 9.21 (7.53-11.28) | - | |
| 100 | FIT13 | 55 (7.1) | 100 (90-100) | 94 (92-95) | 9 (1-18) | 100 (100-100) | 15.48 (11.84-20.24) | - |
| FITmax4 | 82 (10.5) | 100 (90-100) | 90 (88-92) | 6 (0-12) | 100 (100-100) | 10.05 (8.13-12.43) | - | |
| 115 | FIT13 | 51 (6.5) | 100 (90-100) | 94 (92-96) | 10 (1-19) | 100 (100-100) | 16.83 (12.71-22.7) | - |
| FITmax4 | 79 (10.1) | 100 (90-100) | 90 (88-93) | 6 (0-12) | 100 (100-100) | 10.46 (8.42-12.99) | - | |
| 150 | FIT13 | 48 (6.2) | 80 (35-100) | 94 (93-96) | 8 (0-17) | 100 (100-100) | 14.07 (8.33-23.76) | 0.21 (0.04-1.22) |
| FITmax4 | 70 (9.0) | 80 (35-100) | 91 (89-94) | 6 (0-12) | 100 (100-100) | 9.38 (5.72-15.40) | 0.22 (0.04-1.26) | |
| 200 | FIT13 | 45 (5.8) | 80 (35-100) | 95 (93-96) | 9 (0-18) | 100 (100-100) | 15.10 (8.89-25.66) | 0.21 (0.04-1.22) |
| FITmax4 | 59 (7.6) | 80 (35-100) | 93 (91-95) | 7 (0-14) | 100 (100-100) | 11.26 (6.78-18.69) | 0.22 (0.04-1.24) |
Values are expressed as absolute numbers and percentage;
Values are expressed as percentage and its 95%CI;
Fecal hemoglobin concentration in the first sample;
Higher fecal hemoglobin concentration of the two samples. FIT: Fecal immunochemical test.
Table 2.
Performance characteristics of fecal immunochemical test-1 and -max for advanced neoplasia1 detection at different thresholds
| Hemoglobin concentration (ng/mL) | FIT strategy | Individuals with a positive result2 | Sensitivity3 | P4 | Specificity3 | P5 | Positive predictive value3 | Negative predictive value3 | Positive likelihood ratio3 | Negative likelihood ratio3 |
| 50 | FIT16 | 67 (8.6) | 35 (25-45) | 0.06 | 95 (93-97) | 0.001 | 51 (38-63) | 91 (89-93) | 7.24 (4.72-11.13) | 0.68 (0.59-0.79) |
| FITmax7 | 101 (13.0) | 42 (32-53) | 0.03 | 91 (89-93) | < 0.001 | 41 (31-51) | 92 (90-94) | 4.98 (3.44-6.72) | 0.63 (0.53-0.75) | |
| 75 | FIT16 | 61 (7.8) | 33 (23-43) | 0.2 | 96 (94-97) | 0.01 | 52 (39-66) | 91 (89-93) | 7.76 (4.92-12.23) | 0.70 (0.61-081) |
| FITmax7 | 89 (11.4) | 40 (30-51) | 0.1 | 93 (91-95) | 0.03 | 44 (33-55) | 92 (89-94) | 5.48 (3.82-7.87) | 0.65 (0.55-0.76) | |
| 100 | FIT16 | 55 (7.1) | 32 (22-42) | 0.5 | 96 (95-98) | 0.5 | 56 (42-70) | 91 (89-93) | 9.08 (5.57-14.80) | 0.71 (0.61-0.81) |
| FITmax7 | 82 (10.5) | 37 (27-47) | 1 | 93 (91-95) | 0.5 | 44 (33-55) | 91 (89-93) | 5.50 (3.76-8.05) | 0.67 (0.58-0.79) | |
| 115 | FIT16 | 51 (6.5) | 30 (20-40) | 97 (95-98) | 57 (42-71) | 91 (88-93) | 9.27 (5.56-15.46) | 0.72 (0.64-0.83) | ||
| FITmax7 | 79 (10.1) | 36 (26-46) | 94 (92-95) | 44 (33-56) | 91 (89-93) | 5.59 (3.79-8.26) | 0.68 (0.59-0.79) | |||
| 150 | FIT16 | 48 (6.2) | 28 (18-37) | 0.5 | 97 (96-98) | 1 | 56 (41-71) | 90 (88-93) | 9.04 (5.33-15.34) | 0.74 (0.66-0.84) |
| FITmax7 | 70 (9.0) | 32 (22-42) | 0.1 | 94 (92-96) | 0.06 | 44 (32-57) | 91 (88-93) | 5.59 (3.67-8.51) | 0.72 (0.63-0.83) | |
| 200 | FIT16 | 45 (5.8) | 28 (18-37) | 0.5 | 97 (96-99) | 0.1 | 60 (44-75) | 90 (88-93) | 10.55 (6.04-18.41) | 0.74 (0.65-0.84) |
| FITmax7 | 59 (7.6) | 28 (18-37) | 0.08 | 95 (94-97) | < 0.001 | 46 (32-59) | 90 (88-93) | 5.93 (3.72-9.45) | 0.76 (0.67-0.86) |
1Advanced neoplasia: advanced adenomas (adenoma > 1 cm in size, with high-grade dysplasia, or with villous component > 25) or colorectal cancer;
Values are expressed as absolute numbers and percentage;
Values are expressed as percentage and its 95%CI; 4Significance of the sensitivity differences when compared with the optimal cut-off point in McNemar test. Differences with P < 0.05 are considered statistically significant; 5Significance of the specificity differences when compared with the optimal cut-off point in McNemar test. Differences with P < 0.05 are considered statistically significant;
Fecal hemoglobin concentration in the first sample;
Higher fecal hemoglobin concentration of the two samples. FIT: Fecal immunochemical test.
Cost-benefit analysis
When direct colonoscopy screening was analyzed, the NNS to detect a CRC and an AN were 155.8 and 8.2, respectively. The NNS to detect a CRC or an AN decreased from the lowest positivity threshold to the best cut-off value, and then rose again. At 115 ng/mL, in the FIT1 strategy, the NNS to detect a CRC and an AN were 10.2 and 1.76. At the same cut-off point, in FITmax strategy, the NNS to detect a CRC and an AN increased to 15.8 and 2.26 respectively, as shown in Table 3.
Table 3.
Number of colonoscopies needed to detect one lesion and cost per lesion (€) according to positivity threshold and fecal immunochemical test testing strategy
| Lesion | Positivity threshold (ng/mL) |
No. need to scope |
Cost per lesion detected (€) |
Cost increment (€) | ||
| FIT1 | FITmax | FIT1 | FITmax | |||
| CRC | 0 | 155.80 | 16898 | |||
| 50 | 13.40 | 20.20 | 2206 | 3489 | 58.16 | |
| 75 | 12.20 | 17.80 | 2038 | 3223 | 58.15 | |
| 100 | 11.00 | 16.40 | 1912 | 3055 | 59.78 | |
| 115 | 10.20 | 15.80 | 1814 | 2985 | 64.55 | |
| 150 | 12.00 | 17.50 | 2163 | 3451 | 59.55 | |
| 200 | 11.25 | 14.75 | 2075 | 3083 | 48.58 | |
| Advanced neoplasia1 | 0 | 8.20 | 889 | |||
| 50 | 1.97 | 2.46 | 317 | 425 | 34.07 | |
| 75 | 1.91 | 2.28 | 312 | 413 | 32.37 | |
| 100 | 1.77 | 2.28 | 302 | 424 | 40.40 | |
| 115 | 1.76 | 2.26 | 306 | 426 | 39.22 | |
| 150 | 1.78 | 2.26 | 312 | 445 | 42.63 | |
| 200 | 1.67 | 2.19 | 311 | 456 | 46.62 | |
Advanced neoplasia: advanced adenomas (adenoma > 1 cm in size with high-grade dysplasia or with villous component > 25) or colorectal cancer. FIT: Fecal immunochemical test; CRC: Colorectal cancer.
Cost-benefit analysis is displayed in Table 3. The cost per CRC and AN detected in the direct colonoscopy screening strategy was 16898€ and 889€. In contrast in the optimal cut-off point, cost per CRC detected was reduced between 89.2% and 82.3% and cost per AN detected was reduced between 65.6% and 52.1%, depending on the number of FIT determinations. Finally, using two FIT determinations increased cost per CRC detected between 48.58 and 64.55%, and cost per AN detected between 32.37% and 46.62% when compared with only one FIT determination.
DISCUSSION
In this diagnostic tests study we have assessed the accuracy of FIT to detect AN and CRC in an average-risk cohort, and have compared the performance characteristics, endoscopic resources needed and cost-benefit of two FIT testing strategies (one-day vs two-day sampling). FIT only detected 30%-36% of AN, although its accuracy to detect CRC was very high (100% sensitivity and 90%-94% specificity). Furthermore, two-day sampling strategy did not enhance FIT accuracy and increased resource consumption compared to one-day sampling.
Our study has several strengths. First, it was performed on average-risk individuals participating in a pragmatic, population-based CRC screening study[17], with all participants undergoing a colonoscopy. Second, it includes an estimation of direct costs, allowing us to perform a cost-benefit analysis.
Studies addressed to assess FIT accuracy by performing FIT and colonoscopy to all the participants are scant[13-16,21-23,33-37]; some were performed on patients scheduled for colonoscopy because of symptoms or increased risk of CRC[22,23,33,34], others were performed on asymptomatic patients but included subjects with family risk or younger than 50 years[21,35-37]. To our knowledge only four studies (performed on three different cohorts)[13-16] have assessed the accuracy of FIT in average-risk individuals who were offered colonoscopy as CRC screening strategy. A Korean study[13] and two German studies[14,15] were carried out in the setting of oportunistic screening. Recently, a Dutch study has assessed FIT accuracy in a cohort of individuals participating in a population-based screening study[16]. Our study was also carried out on asymptomatic average-risk individuals, participating in a population-based screening study[17], which would allow us to obtain relevant information for CRC screening programs. At the best cut-off value, with one-day FIT, we found that diagnostic accuracy for AN detection is similar to that found in the studies performed on average-risk individuals with a quantitative FIT[13-16]. With respect to CRC, we found a higher sensitivity when compared to previous studies[13,16], but this could be explained by the low number of CRC detected in our cohort.
The performance characteristics of FIT can be adapted to screening variables (prevalence of CRC, participation rates, endoscopic resources), by modifying positivity threshold or by analyzing several stool samples[13,15,33-37]. However, only three studies[13,15,16] have assessed the accuracy of FIT at several cut-off points in an average-risk screening study. Moreover, the study by Park et al[13] is the one that also analyzed more than one stool sample per patient. As previously reported, we found that sensitivity was higher at the lower positivity threshold and, conversely, specificity increased when increasing the positivity threshold. With respect to the number of FIT performed, we decided to analyze only two stool samples per patient, as the ongoing regional screening programs in our country test for one or two stool samples[38]. When comparing 1-d FIT with 2- or 3-d FIT, no clear benefit of several-day sampling has been described, except in a Japanese study in which a qualitative FIT was used[35]. Two studies conducted on referral cohorts (with symptomatic or high risk patients), in which FIT and colonoscopy was performed in all the participants, did not find superiority of 2- or 3-d sampling over single sampling[33,34]. Studies performed in screened average-risk population (that underwent colonoscopy only if FIT was positive), have shown that 2-d sampling could be superior to 1-sampling in different characteristics (depending on the criteria to consider a result as positive) at a particular cut-off level, but they also found that 1-d testing could perform as well as 2-d strategy by changing the threshold of positivity[39-43]. In the study by Park et al[13], AUC for CRC was better with three or two test than with only the first day FIT. In our cohort, however, the AUC for CRC was similar for FIT1 and FITmax, and this could be explained by the fact that all CRC in our cohort were detected with the FIT1 best cut-off.
Modifying the positivity threshold or the number of stool samples to be analyzed not only affect the FIT accuracy, but it also has a great impact on the colonoscopy workload and on the efficiency of the screening, as it influences the rate of patients with a positive test and the PPV. In our study we found that the positivity rate was higher (13%) with the FITmax strategy at the lowest positivity threshold. The same results are found in studies that compared one-day FIT with 2 or 3-d FITmax strategy[33,34,39-41,43]. Finally, as the colonoscopy workload accounts for about 40% to 50% of total screening costs[44,45] modifying the positivity rate and the PPV has relevant consequences. Several studies have assessed this issue with controversial results. We decided to assess the cost benefit analysis by calculating the cost per detected lesion, and as in previous studies[37,46], intermediate thresholds were the most cost-effective for one-day and two-day sampling, being the most cost-effective strategy one-day sampling with a positivity threshold of 115 ng/mL. Our study does not pretend to compare cost-effectiveness among different screening strategies. In fact, we have only made a cost-benefit analysis inside a diagnostic test study. In fact, when cost-effectiveness is assessed by simulation models[47-49], in which screening and treatment costs are related to life-years gained, the most cost-effective strategies are those that allow to detect the greatest number of lesions (lowest positivity threshold and 2-d sampling), provided there is unlimited colonoscopy capacity[47].
As commented previously, FIT sensitivity for AN ranges between 28% and 42% according to the number of determinations and the cut-off point used. Although this is a limitation in the context of a diagnostic test we must be aware of two conditions that favours FIT as a screening test for CRC. First, this effect is diminished by the lower participation rate in the colonoscopy group than in the FIT group. Moreover, in a recently randomized controlled study, the first round of FIT screening detected about half the number of advanced adenomas that were detected by colonoscopy in the first round[17]. Besides, the recurrent nature of FIT screening may reduce the apparent advantage of colonoscopy. In a recently published studies after 4 rounds of CRC screening with FIT, the positive predictive value of the FIT for AN was 40% at the first round, and approximately 33% in the subsequent rounds[50].
Our study has several limitations. First, our sample size was near the lowest range to assess the true accuracy of FIT with a 10% accuracy. However, the prevalence of AN in our series was higher than previously reported, and with that prevalence, our sample size and the previously reported sensitivity and specificity[21], the accuracy achieved in this study was estimated in 8.82%. Second, the number of invasive cancer was low and all of them were detected by FIT1, and this could bias our results. Despite this, the accuracy for AN is similar to that reported previously in average-risk screening[13,15], which makes us consider our results reliable in this setting.
In conclusion, our study shows a low sensitivity of FIT to detect AN, but a high specificity. Its accuracy for CRC detection is high in the setting of average-risk CRC population. With respect to the number of samples, 2-d sampling does not improve the accuracy for CRC, but increases the sensitivity for AN detection, at the expense of increasing the direct costs per lesion detected.
ACKNOWLEDGMENTS
Clinical investigators: Galicia: Mª Belén Aguado, Ana Alonso, M Teresa Alves, Celia Cabalerio, Ana Belén Fernández, Javier Fernandez-Seara, Ana Cruz González, Mª Dolores González, Simoneta González, Pilar Iglesias, Ángeles López-Martinez, Carmen Méndez, Isabel Pérez, Carmen Portasany, Mar Rionda, Rosa Rodríguez, Manuel Rubio, Miriam Vázquez, José Ángel Vázquez, Pablo Vega, Mª Carmen Vidal. Basque Country: María E Alkiza, Jone Altzibar, Pilar Amiano, Juan Arenas, Edurne Artiñano, Ángel Cosme, Isabel Egitegi, Kepa Elorriaga, José L Elósegui, José M Enriquez-Navascués, Cristina Erce, Inés Gil, María A Gutiérrez-Stampa, Mariluz Jaúregui, Eva Laredo, Roberto Martínez, Maria J Mitxelena, Isabel Montalvo, Carlos Placer, Isabel Portillo, Cristina Sarasqueta. We acknowledge Dr. Enrique Quintero and Dr. Antoni Castells, national coordinators of the COLONPREV study, their support and valuable comments on the manuscript.
COMMENTS
Background
Colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related death. Evidence of effectiveness of CRC screening in average-risk population is available from randomized controlled trials for guaiac fecal occult blood tests and sigmoidoscopy, and it has been shown that it is cost-effective or even cost-saving.
Research frontiers
Despite the superiority of fecal immunochemical tests (FIT) over guaiac based methods, its accuracy in average-risk population screening and the optimal number of stool samples or cut-off level and the resource consumption per lesion detected has not been properly assessed.
Innovations and breakthroughs
In this diagnostic tests study authors have assessed the accuracy of FIT to detect advanced colorectal neoplasia and CRC in an average-risk cohort, and have compared the performance characteristics, endoscopic resources needed and cost-benefit of two FIT testing strategies (one-day vs two-day sampling). FIT only detected 30%-36% of advanced neoplasia (AN), although its accuracy to detect CRC was very high (100% sensitivity and 90%-94% specificity). Furthermore, two-day sampling strategy did not enhance FIT accuracy and increased resource consumption compared to one-day sampling.
Applications
Authors analyzed in this population different FIT strategies: 1 or 2 tests and different positive thresholds; not only to evaluate diagnostic accuracy but also endoscopic resources required and cost per lesion detected. Thus, analyzing two samples does not improve diagnostic accuracy and, instead, increases the costs by augmenting the number of colonoscopies needed to detect a CRC or an AN. Their cost-benefit analysis may allow health authorities to define the recommended strategy according to endoscopic resources.
Terminology
Average-risk population: Asymptomatic individuals aged 50-69 years with no familial history of CRC. Fecal immunochemical tests are based on the reaction of monoclonal or polyclonal antibodies specific for human hemoglobin, albumin or other fecal blood components.
Peer review
This is a multicentric study aimed at assessing accuracy of FIT in the detection of CRC and AN in patients undergoing CRC screening. The authors have compared specificity and sensitivity of two measures, one in the first sample and the other on the highest level of both samples. The authors showed a low sensitivity of FIT to detect AN, but a high specificity, which reach the highest level in the setting of average-risk CRC population. Two days sampling does not improve the accuracy for CRC, but increases the sensitivity for AN detection even though is more expensive. The study is well designed and well written and the results are interesting.
Footnotes
Supported by Grants from the Conselleria de Sanidade of Xunta de Galicia, No. PS09/74; Asociación Española contra el Cáncer (Fundación Científica), Instituto de Salud Carlos III, No. PI08/90717; Obra Social de Kutxa, Diputación Foral de Gipuzkoa, No. DFG 07/5; Departamento de Sanidad del Gobierno Vasco, EITB-Maratoia, No. BIO 07/CA/19; Acción Transversal contra el Cáncer del CIBERehd (2008); CIBERehd funded by the Instituto de Salud Carlos III; and Dirección Xeral de Innovación e Xestión da Saúde Pública, Conselleria de Sanidade, Xunta de Galicia
P- Reviewers: Franceschi F, Hsiao KCW, Hardt PD, Kita H, Maurel J, Triantafyllou K S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Hewitson P, Glasziou P, Watson E, Towler B, Irwig L. Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update. Am J Gastroenterol. 2008;103:1541–1549. doi: 10.1111/j.1572-0241.2008.01875.x. [DOI] [PubMed] [Google Scholar]
- 3.Shaukat A, Mongin SJ, Geisser MS, Lederle FA, Bond JH, Mandel JS, Church TR. Long-term mortality after screening for colorectal cancer. N Engl J Med. 2013;369:1106–1114. doi: 10.1056/NEJMoa1300720. [DOI] [PubMed] [Google Scholar]
- 4.Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, Parkin DM, Wardle J, Duffy SW, Cuzick J; UK Flexible Sigmoidoscopy Trial Investigators. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375:1624–1633. doi: 10.1016/S0140-6736(10)60551-X. [DOI] [PubMed] [Google Scholar]
- 5.Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, Bresalier R, Andriole GL, Buys SS, Crawford ED, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366:2345–2357. doi: 10.1056/NEJMoa1114635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lansdorp-Vogelaar I, Knudsen AB, Brenner H. Cost-effectiveness of colorectal cancer screening. Epidemiol Rev. 2011;33:88–100. doi: 10.1093/epirev/mxr004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quintero E. Chemical or immunological tests for the detection of fecal occult blood in colorectal cancer screening? Gastroenterol Hepatol. 2009;32:565–576. doi: 10.1016/j.gastrohep.2009.01.179. [DOI] [PubMed] [Google Scholar]
- 8.Smith A, Young GP, Cole SR, Bampton P. Comparison of a brush-sampling fecal immunochemical test for hemoglobin with a sensitive guaiac-based fecal occult blood test in detection of colorectal neoplasia. Cancer. 2006;107:2152–2159. doi: 10.1002/cncr.22230. [DOI] [PubMed] [Google Scholar]
- 9.Guittet L, Bouvier V, Mariotte N, Vallee JP, Arsène D, Boutreux S, Tichet J, Launoy G. Comparison of a guaiac based and an immunochemical faecal occult blood test in screening for colorectal cancer in a general average risk population. Gut. 2007;56:210–214. doi: 10.1136/gut.2006.101428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allison JE, Sakoda LC, Levin TR, Tucker JP, Tekawa IS, Cuff T, Pauly MP, Shlager L, Palitz AM, Zhao WK, et al. Screening for colorectal neoplasms with new fecal occult blood tests: update on performance characteristics. J Natl Cancer Inst. 2007;99:1462–1470. doi: 10.1093/jnci/djm150. [DOI] [PubMed] [Google Scholar]
- 11.Rozen P, Levi Z, Hazazi R, Waked A, Vilkin A, Maoz E, Birkenfeld S, Niv Y. Quantitative colonoscopic evaluation of relative efficiencies of an immunochemical faecal occult blood test and a sensitive guaiac test for detecting significant colorectal neoplasms. Aliment Pharmacol Ther. 2009;29:450–457. doi: 10.1111/j.1365-2036.2008.03898.x. [DOI] [PubMed] [Google Scholar]
- 12.Parra-Blanco A, Gimeno-García AZ, Quintero E, Nicolás D, Moreno SG, Jiménez A, Hernández-Guerra M, Carrillo-Palau M, Eishi Y, López-Bastida J. Diagnostic accuracy of immunochemical versus guaiac faecal occult blood tests for colorectal cancer screening. J Gastroenterol. 2010;45:703–712. doi: 10.1007/s00535-010-0214-8. [DOI] [PubMed] [Google Scholar]
- 13.Park DI, Ryu S, Kim YH, Lee SH, Lee CK, Eun CS, Han DS. Comparison of guaiac-based and quantitative immunochemical fecal occult blood testing in a population at average risk undergoing colorectal cancer screening. Am J Gastroenterol. 2010;105:2017–2025. doi: 10.1038/ajg.2010.179. [DOI] [PubMed] [Google Scholar]
- 14.Hundt S, Haug U, Brenner H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann Intern Med. 2009;150:162–169. doi: 10.7326/0003-4819-150-3-200902030-00005. [DOI] [PubMed] [Google Scholar]
- 15.Haug U, Hundt S, Brenner H. Quantitative immunochemical fecal occult blood testing for colorectal adenoma detection: evaluation in the target population of screening and comparison with qualitative tests. Am J Gastroenterol. 2010;105:682–690. doi: 10.1038/ajg.2009.668. [DOI] [PubMed] [Google Scholar]
- 16.de Wijkerslooth TR, Stoop EM, Bossuyt PM, Meijer GA, van Ballegooijen M, van Roon AH, Stegeman I, Kraaijenhagen RA, Fockens P, van Leerdam ME, et al. Immunochemical fecal occult blood testing is equally sensitive for proximal and distal advanced neoplasia. Am J Gastroenterol. 2012;107:1570–1578. doi: 10.1038/ajg.2012.249. [DOI] [PubMed] [Google Scholar]
- 17.Quintero E, Castells A, Bujanda L, Cubiella J, Salas D, Lanas Á, Andreu M, Carballo F, Morillas JD, Hernández C, et al. Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. N Engl J Med. 2012;366:697–706. doi: 10.1056/NEJMoa1108895. [DOI] [PubMed] [Google Scholar]
- 18.Vilkin A, Rozen P, Levi Z, Waked A, Maoz E, Birkenfeld S, Niv Y. Performance characteristics and evaluation of an automated-developed and quantitative, immunochemical, fecal occult blood screening test. Am J Gastroenterol. 2005;100:2519–2525. doi: 10.1111/j.1572-0241.2005.00231.x. [DOI] [PubMed] [Google Scholar]
- 19.Jover R, Herráiz M, Alarcón O, Brullet E, Bujanda L, Bustamante M, Campo R, Carreño R, Castells A, Cubiella J, et al. Clinical practice guidelines: quality of colonoscopy in colorectal cancer screening. Endoscopy. 2012;44:444–451. doi: 10.1055/s-0032-1306690. [DOI] [PubMed] [Google Scholar]
- 20.O‘Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with the new American Joint Committee on Cancer sixth edition staging. J Natl Cancer Inst. 2004;96:1420–1425. doi: 10.1093/jnci/djh275. [DOI] [PubMed] [Google Scholar]
- 21.Morikawa T, Kato J, Yamaji Y, Wada R, Mitsushima T, Shiratori Y. A comparison of the immunochemical fecal occult blood test and total colonoscopy in the asymptomatic population. Gastroenterology. 2005;129:422–428. doi: 10.1016/j.gastro.2005.05.056. [DOI] [PubMed] [Google Scholar]
- 22.Levi Z, Rozen P, Hazazi R, Vilkin A, Waked A, Maoz E, Birkenfeld S, Leshno M, Niv Y. A quantitative immunochemical fecal occult blood test for colorectal neoplasia. Ann Intern Med. 2007;146:244–255. doi: 10.7326/0003-4819-146-4-200702200-00003. [DOI] [PubMed] [Google Scholar]
- 23.Greenberg PD, Bertario L, Gnauck R, Kronborg O, Hardcastle JD, Epstein MS, Sadowski D, Sudduth R, Zuckerman GR, Rockey DC. A prospective multicenter evaluation of new fecal occult blood tests in patients undergoing colonoscopy. Am J Gastroenterol. 2000;95:1331–1338. doi: 10.1111/j.1572-0241.2000.02032.x. [DOI] [PubMed] [Google Scholar]
- 24.Strul H, Kariv R, Leshno M, Halak A, Jakubowicz M, Santo M, Umansky M, Shirin H, Degani Y, Revivo M, et al. The prevalence rate and anatomic location of colorectal adenoma and cancer detected by colonoscopy in average-risk individuals aged 40-80 years. Am J Gastroenterol. 2006;101:255–262. doi: 10.1111/j.1572-0241.2006.00430.x. [DOI] [PubMed] [Google Scholar]
- 25.Terhaar Sive Droste JS, Craanen ME, van der Hulst RW, Bartelsman JF, Bezemer DP, Cappendijk KR, Meijer GA, Morsink LM, Snel P, Tuynman HA, et al. Colonoscopic yield of colorectal neoplasia in daily clinical practice. World J Gastroenterol. 2009;15:1085–1092. doi: 10.3748/wjg.15.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Betés Ibáñez M, Muñoz-Navas MA, Duque JM, Angós R, Macías E, Súbtil JC, Herraiz M, de la Riva S, Delgado-Rodríguez M, Martínez-Gonzélez MA. Diagnostic value of distal colonic polyps for prediction of advanced proximal neoplasia in an average-risk population undergoing screening colonoscopy. Gastrointest Endosc. 2004;59:634–641. doi: 10.1016/s0016-5107(04)00155-5. [DOI] [PubMed] [Google Scholar]
- 27.Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med. 2000;343:162–168. doi: 10.1056/NEJM200007203430301. [DOI] [PubMed] [Google Scholar]
- 28.Ladabaum U, Ferrandez A, Lanas A. Cost-effectiveness of colorectal cancer screening in high-risk Spanish patients: use of a validated model to inform public policy. Cancer Epidemiol Biomarkers Prev. 2010;19:2765–2776. doi: 10.1158/1055-9965.EPI-10-0530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J. Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol Assess. 2004;8:iii, 1–234. doi: 10.3310/hta8250. [DOI] [PubMed] [Google Scholar]
- 30.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ. 2003;326:41–44. doi: 10.1136/bmj.326.7379.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 32.Trajman A, Luiz RR. McNemar chi2 test revisited: comparing sensitivity and specificity of diagnostic examinations. Scand J Clin Lab Invest. 2008;68:77–80. doi: 10.1080/00365510701666031. [DOI] [PubMed] [Google Scholar]
- 33.Rozen P, Comaneshter D, Levi Z, Hazazi R, Vilkin A, Maoz E, Birkenfeld S, Niv Y. Cumulative evaluation of a quantitative immunochemical fecal occult blood test to determine its optimal clinical use. Cancer. 2010;116:2115–2125. doi: 10.1002/cncr.25012. [DOI] [PubMed] [Google Scholar]
- 34.Oort FA, van Turenhout ST, Coupé VM, van der Hulst RW, Wesdorp EI, Terhaar sive Droste JS, Larbi IB, Kanis SL, van Hengel E, Bouman AA, et al. Double sampling of a faecal immunochemical test is not superior to single sampling for detection of colorectal neoplasia: a colonoscopy controlled prospective cohort study. BMC Cancer. 2011;11:434. doi: 10.1186/1471-2407-11-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakama H, Yamamoto M, Kamijo N, Li T, Wei N, Fattah AS, Zhang B. Colonoscopic evaluation of immunochemical fecal occult blood test for detection of colorectal neoplasia. Hepatogastroenterology. 1995;46:228–231. [PubMed] [Google Scholar]
- 36.Nakama H, Zhang B, Fattah AS. A cost-effective analysis of the optimum number of stool specimens collected for immunochemical occult blood screening for colorectal cancer. Eur J Cancer. 2000;36:647–650. doi: 10.1016/s0959-8049(00)00020-4. [DOI] [PubMed] [Google Scholar]
- 37.Nakama H, Zhang B, Zhang X. Evaluation of the optimum cut-off point in immunochemical occult blood testing in screening for colorectal cancer. Eur J Cancer. 2001;37:398–401. doi: 10.1016/s0959-8049(00)00387-7. [DOI] [PubMed] [Google Scholar]
- 38.Salas D. Situacion de los programas de cribado de cáncer colorrectal en España - 2012. Available from: http://www.programascancerdemama.org/index.php/situacion-de-los-programas-de-cribado-de-cancer-colorrectal-en-espana-ano-2012. Accessed March 25, 2013.
- 39.Guittet L, Bouvier V, Mariotte N, Vallee JP, Levillain R, Tichet J, Launoy G. Performance of immunochemical faecal occult blood test in colorectal cancer screening in average-risk population according to positivity threshold and number of samples. Int J Cancer. 2009;125:1127–1133. doi: 10.1002/ijc.24407. [DOI] [PubMed] [Google Scholar]
- 40.Grazzini G, Visioli CB, Zorzi M, Ciatto S, Banovich F, Bonanomi AG, Bortoli A, Castiglione G, Cazzola L, Confortini M, et al. Immunochemical faecal occult blood test: number of samples and positivity cutoff. What is the best strategy for colorectal cancer screening? Br J Cancer. 2009;100:259–265. doi: 10.1038/sj.bjc.6604864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van Roon AH, Wilschut JA, Hol L, van Ballegooijen M, Reijerink JC, ‘t Mannetje H, Kranenburg LJ, Biermann K, van Vuuren AJ, Francke J, et al. Diagnostic yield improves with collection of 2 samples in fecal immunochemical test screening without affecting attendance. Clin Gastroenterol Hepatol. 2011;9:333–339. doi: 10.1016/j.cgh.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 42.Guittet L, Bouvier V, Guillaume E, Levillain R, Ruiz A, Lantieri O, Launoy G. Colorectal cancer screening: why immunochemical faecal occult blood test performs as well with either one or two samples. Dig Liver Dis. 2012;44:694–699. doi: 10.1016/j.dld.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 43.Faivre J, Dancourt V, Manfredi S, Denis B, Durand G, Gendre I, Bidan JM, Jard C, Levillain R, Jung S, et al. Positivity rates and performances of immunochemical faecal occult blood tests at different cut-off levels within a colorectal cancer screening programme. Dig Liver Dis. 2012;44:700–704. doi: 10.1016/j.dld.2012.03.015. [DOI] [PubMed] [Google Scholar]
- 44.Castiglione G, Zappa M, Grazzini G, Sani C, Mazzotta A, Mantellini P, Ciatto S. Cost analysis in a population based screening programme for colorectal cancer: comparison of immunochemical and guaiac faecal occult blood testing. J Med Screen. 1997;4:142–146. doi: 10.1177/096914139700400306. [DOI] [PubMed] [Google Scholar]
- 45.Grazzini G, Ciatto S, Cislaghi C, Castiglione G, Falcone M, Mantellini P, Zappa M. Cost evaluation in a colorectal cancer screening programme by faecal occult blood test in the District of Florence. J Med Screen. 2008;15:175–181. doi: 10.1258/jms.2008.008032. [DOI] [PubMed] [Google Scholar]
- 46.Berchi C, Guittet L, Bouvier V, Launoy G. Cost-effectiveness analysis of the optimal threshold of an automated immunochemical test for colorectal cancer screening: performances of immunochemical colorectal cancer screening. Int J Technol Assess Health Care. 2010;26:48–53. doi: 10.1017/S0266462309990808. [DOI] [PubMed] [Google Scholar]
- 47.Wilschut JA, Habbema JD, van Leerdam ME, Hol L, Lansdorp-Vogelaar I, Kuipers EJ, van Ballegooijen M. Fecal occult blood testing when colonoscopy capacity is limited. J Natl Cancer Inst. 2011;103:1741–1751. doi: 10.1093/jnci/djr385. [DOI] [PubMed] [Google Scholar]
- 48.Wilschut JA, Hol L, Dekker E, Jansen JB, Van Leerdam ME, Lansdorp-Vogelaar I, Kuipers EJ, Habbema JD, Van Ballegooijen M. Cost-effectiveness analysis of a quantitative immunochemical test for colorectal cancer screening. Gastroenterology. 2011;141:1648–1655.e1. doi: 10.1053/j.gastro.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 49.Goede SL, van Roon AH, Reijerink JC, van Vuuren AJ, Lansdorp-Vogelaar I, Habbema JD, Kuipers EJ, van Leerdam ME, van Ballegooijen M. Cost-effectiveness of one versus two sample faecal immunochemical testing for colorectal cancer screening. Gut. 2013;62:727–734. doi: 10.1136/gutjnl-2011-301917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crotta S, Segnan N, Paganin S, Dagnes B, Rosset R, Senore C. High rate of advanced adenoma detection in 4 rounds of colorectal cancer screening with the fecal immunochemical test. Clin Gastroenterol Hepatol. 2012;10:633–638. doi: 10.1016/j.cgh.2012.02.030. [DOI] [PubMed] [Google Scholar]


