Abstract
INTRODUCTION
Although there is no debate that patients with peritonitis or hemodynamic instability should undergo urgent laparotomy after penetrating abdominal injury, it is also clear that certain stable patients may be managed without operation. Controversy persists regarding use of laparoscopy.
PRESENTATION OF CASE
We report a case of gunshot wounds with bullet in left adrenal gland and perirenal subcapsular hematoma. The patients had no signs of peritonitis but in the observation period we noted a significative blood loss, so we performed an exploratory laparoscopy.
DISCUSSION
We found the bullet in adrenal parenchyma. The postoperative period was regular and the patient was discharged without any local or general complication.
CONCLUSION
Although the data are still controversial, the importance of the laparoscopic approach is rapidly increasing also in case of penetrating trauma of the abdomen. This technique assumes both a diagnostic and therapeutic role by reducing the number of negative laparotomies.
Keywords: Laparoscopy, Gunshot wounds, Penetrating abdominal trauma
1. Introduction
The proper treatment of penetrating abdominal wounds is still controversial. In the first half of the twentieth century, an exploratory laparotomy was performed in principle on all the patients with penetrating wounds of the abdomen. This approach was based on the assumption of an high incidence of intra-abdominal lesions (98%).1 Since the 1960s non-operative management (NOM) started to be considered an appropriate method to safety treat these patients. Nowadays the NOM has become the standard of care in case of stab wounds to the anterior abdomen, instead, gunshot wounds to the abdomen are still treated by mandatory exploration. Even if also in the latter case, the percentage of negative laparotomies is in the range of 15–27%.2 The hemodynamically stable patients without clinical signs of peritonitis are candidates for the NOM. At this time however, there is a little evidence to support this NOM strategy for gunshot injuries where there is a known solid organ injury.3 The clinical signs which suggest an intra-abdominal injuries are represented by tenderness, hemodynamic instability, hematuria, hematemesis, rectal bleeding, blood in the nasogastric tube. The diagnostic opportunities for hemodynamically stable patients includes roentgenography, FAST, CT scan, rigid sigmoidoscopy, contrast cystogram and diagnostic laparoscopy. Patients are transferred to the operating room in case of deterioration of hemodynamic status, worsening of abdominal exam or decrease in hemoglobin level. In our case report we had a gunshot wound in the back. Many authors believe that gunshot wounds in the back require routine exploration, in fact the retroperitoneal injuries may not manifest immediate clinical symptoms and lead to delayed diagnosis which may cause significant morbidity.4 In recent years laparoscopy has developed its therapeutic role in trauma with possibility to screen or the necessity of laparotomy.5
2. Case report
29-years-old man comes to the emergency room, in good general clinical condition (heart rate 78/min; blood pressure 120/65 mmHg), with a penetrating wound in left lumbar region without signs of peritonitis (Fig. 1). We perform routine blood tests (Hb 14.8 g/dl, WBC 11,000), chest X-ray and abdominal CT. The chest X-ray shows, in left subfrenic space, the presence of foreign metallic body (diameter 9 mm). The abdominal CT was performed with triphasic technique for the study of the urinary tract. The metallic bullet (diameter 1 cm) was found in retroperitoneum associated with cortical lesion of the upper pole of left kidney with perirenal subcapsular hematoma (transverse diameter 5.2 cm, sagittal 6.5 cm, coronal 11 cm). The excretory phase of both kidneys is regular and there are not lesions of the other abdominal organs (Fig. 2). Given the hemodynamic stability and the absence of hemoperitoneum we decide to take a NOM. Control blood test is repeated after 3 and 6 h with evidence of significant decline in hemoglobin (Hb 10.8 g/dl vs 14.8 g/dl); heart rate and blood pressure are normal. The rapid anemia and the CT report (renal cortical lesion with retroperitoneal hematoma) encourage us to carry out an exploratory diagnostic laparoscopy. The patient is placed in right lateral recumbency with an inclination of 50–60° relative to the operating table which is broken to extend the space between the last rib and the iliac crest.6–8 We used Veress needle to induce pneumoperitoneum and three trocars in the left subcostal region. In contrast to retroperitoneal approach, we chose a transperitoneal laparoscopic procedure because allows for a larger working space, adequate maneuverability and the presence of familiar anatomic landmarks.9 Careful exploration of the peritoneal cavity did not show lesions of the peritoneal organs. Considering CT results, the spleno-pancreatic block is medially mobilized to access the retroperitoneum and reach the adrenal and renal space. We opened Gerota on the upper pole of the kidney with identification of peri-renal hematoma, without any signs of active bleeding. We decide to carry out intraoperative radiological control using an image intensifier. Only a careful and accurate comparison of these X-ray images and laparoscopic vision allows us to identify and extract the bullet out of the adrenal parenchyma10 (Fig. 3a and b). Accurate hemostasis is made through a bipolar forceps and further application of fibrin glue in the renal and adrenal loggia for the purpose of a correct repositioning of the spleno-pancreatic block. We settle a tubular drainage in renal region. In postoperative period hemoglobin values were stable and were not required transfusion. The abdominal drain is removed during the fourth postoperative day and the patient is discharged without complications.
Fig. 1.

Penetrating wound in left lumbar region. Patient on surgical table.
Fig. 2.
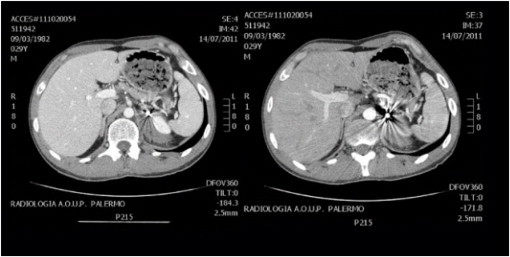
CT scan of abdomen: left renal space with metallic foreign body.
Fig. 3.
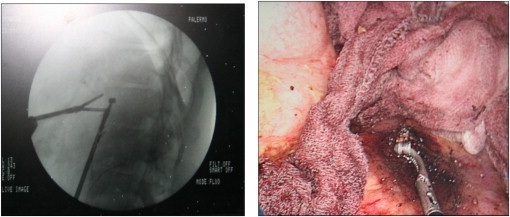
(a) Intraoperative radiological control with an image intensifier. (b) Laparoscopic vision with extraction of the bullet out of the adrenal parenchyma.
3. Discussion
The laparoscopic approach allows us to identify a bleeding or the presence of visceral lesions combining the minimally invasive treatment of the possible injury. Moreover this approach reduces the incidence of negative laparotomies.5 Over the years, various authors have formulated several algorithms for treatment of these patients, nevertheless the role of laparoscopy in such situations is still controversial.11 In our case report we had a penetrating retroperitoneal hematoma: firstly we attempted the NOM with strict clinical-laboratory control of the patient. Potential candidates for NOM after penetrating abdominal injury must be hemodynamically stable without signs of peritonitis. The treatment of retroperitoneal bleeding varies depending on the hemodynamic status of the patient. In this case CT scan confirmed a renal injury with entrance wound only and the presence of the bullet in the renal space. The rapid drop in hemoglobin and the evidence of on-going bleeding with hemodynamic stability have led us to perform a laparoscopic surgical treatment.12
4. Conclusion
Although the data are still controversial, the importance of the laparoscopic approach is rapidly increasing also in case of penetrating trauma of the abdomen. This technique assumes both a diagnostic and therapeutic role by reducing the number of negative laparotomies. The advantages of laparoscopy are: the reduction of blood loss, the low risk of contamination, the early functional recovery, the reduction of postoperative pain and the better cosmetic result. This procedure, however, can only be performed by experienced surgeons on properly selected patients.
Author contributions
Agrusa Antonino: study design and writing, Romano Giorgio: study design, De Vita Giovanni: data collections, Frazzetta Giuseppe: data collections and data analysis, Chianetta Daniela: data collections and data analysis, Di Buono Giuseppe: data collections and data analysis, Gulotta Gaspare: study design.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Moore E., Moore J.B., Van-Duzer-Moore S., Thompson J.S. Mandatory laparotomy for gunshot wounds penetrating the abdomen. Am J Surg. 1980;140:847–851. doi: 10.1016/0002-9610(80)90130-0. [DOI] [PubMed] [Google Scholar]
- 2.Salim A., Velmahos G. When to operate on abdominal gunshot wounds. Scand J Surg. 2002;91:62–66. doi: 10.1177/145749690209100110. [DOI] [PubMed] [Google Scholar]
- 3.DuBose J., Inaba K., Teixeira P.G.R., Pepe A., Dunham M.B., McKenney M. Selective non-operative management of solid organ injury following abdominal gunshot wound. Injury. 2007;38(9):1084–1090. doi: 10.1016/j.injury.2007.02.030. [DOI] [PubMed] [Google Scholar]
- 4.Butt M.U., Zacharias N., Velmahos G.C. Penetrating abdominal injuries: management controversies. Scand J Trauma Resusc Emerg Med. 2009;17(April (17)):19. doi: 10.1186/1757-7241-17-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Malley E., Boyle E., O’Callaghan A., Coffey J.C., Walsh S.R. Role of laparoscopy in penetrating abdominal trauma: a systematic review. World J Surg. 2013;37:113–122. doi: 10.1007/s00268-012-1790-y. [DOI] [PubMed] [Google Scholar]
- 6.Agrusa A., Romano G., Di Buono G., Dafnomili A., Gulotta G. Laparoscopic approach in abdominal emergencies: a 5-year experience at a single center. G Chir. 2012;33(November–December (11–12)):400–403. [PubMed] [Google Scholar]
- 7.Tuveri M., Calò P.G., Medas F., Tuveri A., Nicolosi A. Limits and advantages of fundus-first laparoscopic cholecystectomy: lessons learned. J Laparoendosc Adv Surg Tech A. 2008;18(1):69–75. doi: 10.1089/lap.2006.0194. [DOI] [PubMed] [Google Scholar]
- 8.Conzo G., Musella M., Corcione F., De Palma M., Avenia N., Milone M. Laparoscopic treatment of pheochromocytomas smaller or larger than 6 cm. A clinical retrospective study on 44 patients. Laparoscopic adrenalectomy for pheochromocytoma. Ann Ital Chir. 2013;84:417–422. [PubMed] [Google Scholar]
- 9.Allaf M.E., Bhayani S.B., Kavoussi L.R. Taking the side of transperitoneal access for surgery in upper urinary tract. Curr Urol Rep. 2004;5(April (2)):87–92. doi: 10.1007/s11934-004-0019-5. [DOI] [PubMed] [Google Scholar]
- 10.Biondi A., Motta S., Di Giunta M., Crisafi R.M., Zappalà S., Rapisarda D. The use of laparoscopy for diagnosis and stadiation of the lymphomas. Ann Ital Chir. 2009;80(November–December (6)):445–447. [PubMed] [Google Scholar]
- 11.Miles E.J., Dunn E., Howard D., Mangram A. The role of laparoscopy in penetrating abdominal trauma. JSLS. 2004;8:304–309. [PMC free article] [PubMed] [Google Scholar]
- 12.Chamisa I. Civilian abdominal gunshot wounds in Durban, South Africa: a prospective study of 78 cases. Ann R Coll Surg Engl. 2008;90:581–586. doi: 10.1308/003588408X301118. [DOI] [PMC free article] [PubMed] [Google Scholar]


