Abstract
INTRODUCTION
Patellar instability can be considered as a rapidly increasing musculoskeletal subject of interest. It is now well accepted that multiple factors can produce this pathological condition, isolated, but more often in concert. One major static compound is found to be in trochlear dysplasia. It has been stated that the form of the trochlear surface is primary and genetically bilaterally determined already before use. According to these data, recurrent dislocation of the patella has been described as a hereditary disease with autosomal dominant transmission. Against this assumption, we hypothesize that subjects may devise a flattened trochlea when there is no significant biomechanical interplay and thus input between the patella and the distal femur during developmental growth; according to the assumption form follows function.
PRESENTATION OF CASE
In this context, we report the case of a 16-year old male who previously suffered from a traumatic patellar dislocation during sporting activity in his below-knee amputated lower extremity, which occured at age of 18 months. The patient was allocated with a high-grade trochlear dysplasia in his previously amputated limb, while presenting a normal trochlear shape at his healthy contralateral leg.
DISCUSSION
This rare case therefore reprents the history of an individuum with identic genetic predisposition and different biomechanical influences during childhood, which makes it of high clinical interest. In presence of trochlear dysplasia the patient suffered reluxation and concurrent subjective instability on the lower limb affected by the amputation which was treated with medial patellofemoral ligament (MPFL) plasty using an autologous gracilis graft.
CONCLUSION
One has to consider that a certain biomechanical input may be required for the development of a physiologic trochlear groove.
Keywords: Patella, MPFL, Trochlear dysplasia, Amputee, Patellar instability, Ligament
1. Introduction
Patellar instability can be considered as a rapidly increasing musculoskeletal subject of interest. It is now well accepted that multiple factors can produce this pathological condition, isolated, but more often in concert.1 Furthermore it is now an accepted precondition to develop patellofemoral arthritis. One major static compound is found in trochlear dysplasia. While there is strongly increasing literary information on how and when to treat patellofemoral incongruence, the body of literature exploring the etiology of trochlear dysplasia is surprisingly sparse and foremost not finally concluding. It has been stated that the form of the trochlear surface is primarily and genetically bilaterally determined already before use.4,5,8,9,12 According to these data, recurrent dislocation of the patella has been described as a hereditary disease with autosomal dominant transmission.7 Against this assumption, we hypothesize that subjects may devise a flattened trochlea when there is no significant biomechanical interplay and thus input between the patella and the distal femur during developmental growth, according to the assumption form follows function. In this context, we report the case of a 16-year-old male who previously suffered from a traumatic patellar dislocation during sporting activity in his below-knee amputated lower extremity, which occurred at the age of 18 months. The patient was allocated with a high-grade trochlear dysplasia in his previously amputated limb, while presenting a normal trochlear shape at his healthy contralateral leg. This rare case therefore represents the history of an individuum with identical genetic predisposition and different biomechanical influences during childhood, which makes it of high clinical interest. In the presence of trochlear dysplasia the patient suffered reluxation and concurrent subjective instability of the lower limb affected by the amputation which was treated with medial patellofemoral ligament (MPFL) plasty using an autologous gracilis graft.
2. Presentation of case
A 16-year-old male patient who previously underwent trauma-related below-knee amputation of the right leg as an 18-month old presented with the history of a first time acute patellar dislocation during skiing as a 15-year old. The patient was previously completely asymptomatic and highly active in competitive skiing and golf, well provided with a below-knee prosthesis. The patient, however, was without any significant mechanical load to his amputated limb between 18 and 36 months of age. Furthermore, application of the amputated extremity has always been much less, in particular during developing years, when compared to the other knee joint. Following conservative treatment a reluxation occurred while the patient was jumping from a wall with no significant trauma mechanism in generation. Both times the patella had to be relocated requiring medical attention. Hereon the patient described subjective instability during daily activity.
2.1. Clinical assessment
Clinical examination uncovered a straight long leg axis without signs of malrotation or genu recurvatum, but slightly hypotrophic thigh musculature when compared to the healthy contralateral side (Fig. 1). Patellofemoral articulation was painless and centered between 0 and 130° of knee flexion. The apprehension sign was positive between 0 and 30° of knee flexion, while the pathologic patella could be manually lateralized. Adequate stability was provided at higher degrees of flexion. The remaining knee examination revealed no further detectable pathologies.
Fig. 1.

Pre – and intraoperative macroscopic image illustrating right-sided (left on image) amputation and reduced musculature at right knee joint with normal patellofemoral articulation.
2.2. Radiographic examinations
Radiographic examination identified a straight leg axis (Fig. 2), while the Patella skyline view at 30°, 60° and 90° of flexion revealed a flattened trochlea and a flattened patellar undersurface when compared with the left knee joint (Fig. 3). We made this observation even though being familiar with previous data presented on limitations of plain radiographic examination of the trochlea.10 Insall-Salvati was 1.42 in display of patella alta. Standard MRI clearly showed a high-grade trochlear dysplasia type C according to Dejour2 with a previously ruptured MPFL and no detectable cartilage damage (Fig. 4). The tibial tuberosity to trochlear groove (TTTG) distance was 10.1 mm. MR imaging of the contralateral knee illustrated normal patellofemoral articulation, normal MPFL and a TTTG of 4.7 mm with an Insall-Salvati of 1.35.
Fig. 2.
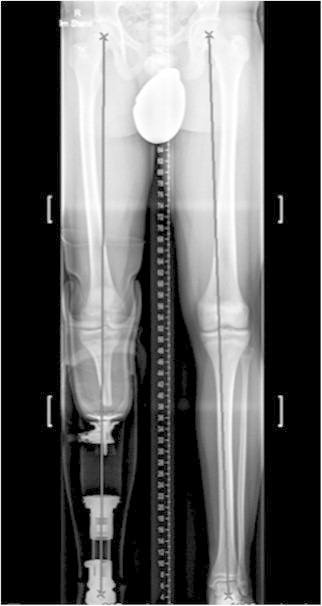
Preoperative conventional weight-bearing and AP hip-knee-ankle radiographs. Manually drawn Mikulicz line displaying the mechanical axis depicts minimal valgus at right leg (left on image) and slight varus deformity at left leg. Right lower extremity replaced by prosthesis.
Fig. 3.
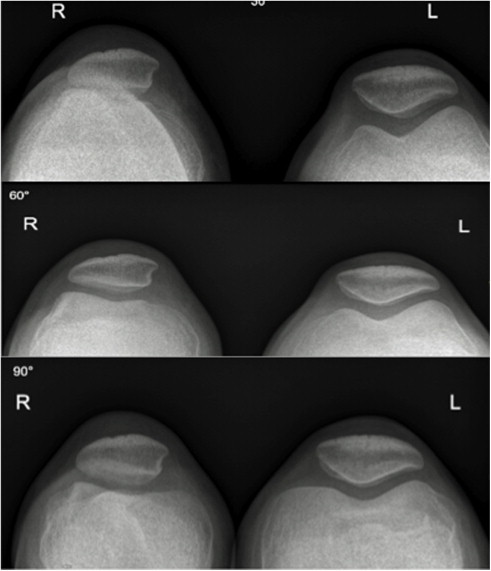
Conventional skyline view radiographs displaying right-sided trochlear dyplasia (left on image) without significant lateral displacement. Patellofemoral architecture and alignment are normal at the left-sided knee joint.
Fig. 4.
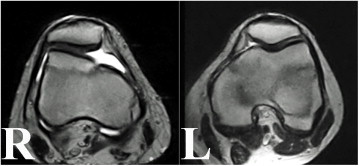
Axial MR imaging displaying high-grade trochlear dysplasia, insufficient MPFL, slightly tilting and shifting patella at right-sided knee joint (left on image). In comparison normal appearing patellofemoral condition at left knee joint. Cut-out depicting localizer on sagittal image, respectively.
2.3. Surgical treatment
According to current guidelines and with respect to the reported specific patient history, the patient was skeletally mature at the time of operative intervention. Therefore we decided to proceed with an isolated MPFL replacement following gracilis tendon harvest from the uninjured knee. We felt against ipsilateral tendon harvest since the amputee stump had been revised several times due to wound considerations following amputation, and on MRI the hamstring complex appeared highly hypoplastic.
In supine decubitus initial diagnostic arthroscopy revealed a clearly flattened trochlea presenting with no identifiable sulcus and a medial-sided cliff appearing pattern as within trochlea dysplasia type D. This information contradicted previous collected MRI data. The patella was strongly lateralized in extension and tended to dip physiologically not before 30–50° of knee flexion. Patellofemoral cartilage and the remaining joint appeared normal. Following contralateral tendon harvest we performed standard MPFL surgery as previously described.11 Final arthroscopy showed normal patellofemoral articulation already in full extension with full range of free motion and no signs of increased patellofemoral pressure (Fig. 5).
Fig. 5.
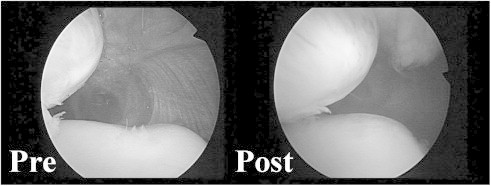
Arthroscopic view, right-sided knee joint, from anterolateral portal. Snapshot of medial-sided patellofemoral articluation before MPFL (Pre, left-sided image) and after MPFL (Post, right-sided image) replacement in full knee extension. While the patella is clearly laterally displaced before ligament substitution (Pre), normal appearing patellofemoral articulation postoperatively (Post).
3. Discussion and conclusion
We present the case of a patient affected by one-sided trochlear dysplasia type C according to Dejour in a previously below-knee amputated knee joint at the age of 18 months. The contralateral knee joint was without pathologic abnormalities and in particular without trochlear dysplasia. Even though the patient was provided with a below-knee prosthesis approximately 18 months following the traumatic incident (at the age of 3 years), biomechanical input to the knee joint has never been comparable to that of the contralateral knee joint. Furthermore, there was no weight-bearing for 1.5 years during the crucial years in which infants start to walk. The patient was well reported that application of the amputated extremity has always been much less, in particular during developing years, when compared to the other knee joint. We assume that the patient's right leg was rather used as a static bearing in full extension, with no or little weight applied during flexion moments. Thus, pressure of the patella on the trochlea as an articular counterpart was significantly reduced. However the patient managed to clearly increase deployment to get involved in semi-professional athletic activity in later moments of life.
With regard to these facts, the present case seems interesting to study a possible influence of abnormal biomechanics during childhood on the incidence of trochlear dysplasia and the anatomical shape of the anterior knee compartment. It is particularly interesting since normally and potentially genetically determined dysplasia has been reported to be both-sided.4
Until today there remains controversy regarding the development of the final patellofemoral joint, in particular when trochlear shape is considered. In the evolutionary history the configuration of the trochlea with deepened groove and lateral elevation followed the obliquity of the femur. Articular surface shape among mammals depends on type of locomotion. Among human adults the femoral diaphysis has a valgus obliquity angle of 8–10 degrees. Thus, the trochlea has an elevated lip on the lateral side with a deepened sulcus in order to avoid lateral displacement during early degrees of flexion. Findings of Doskocil3 and Garron5 point out that the joint surface morphology of the knee is determined very early during in utero life. In contrast to this, Tardieu pointed out that femoral obliquity is acquired through the process of learning to walk, being an epigenetic feature, and not by genetic determinism.12 In the human newborn, the femoral diaphysis is vertical. As a child starts to walk, the femoral obliquity angle develops between 1 and 7 years of age, inducing a secondary valgus of the extensor apparatus. Among non-walking children, as in the case presented here, this obliquity does not develop.8 Embryology has shown that the patellar anlage can be discovered within the quadriceps condensation in the 20 mm embryo or at 7.5 weeks of gestation. According to Walmsley, the patella acquires an articular surface in common with the distal femora after initial conformation. Further patella mechanical behavior results in determination, to an undescribed extent, of the final shape of the articulating trochlea.13 Post-partum, emergence of the complex patellofemoral articulation undergoes a constant development during growth. Nietosvaara9 has shown that the cartilaginous trochlear angle is already shaped at birth, but that the osseous trochlea gains depth during adolescence. We hypothesize that in this particular case the load of the leg in extension has contributed to the valgisation of the femur, but the absence of normal load and function of the femoropatellar joint favored the trochlear dysplasia.
While it has been previously reported that the final shape of the patella and trochlea is mostly genetically determined, we consider that trochlear deepening could also be strongly dependent on biomechanical input during growth. This hypothesis is underlined by the present case report. This consideration has been recently underlined by a rabbit animal model in which an artificially malpositioned patella during growth constrained physiological trochlear sulcus development in terms of depth when compared to control.6
Conflict of interest
None declared.
Footnotes
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1.Colvin A.C., West R.V. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751–2762. doi: 10.2106/JBJS.H.00211. [DOI] [PubMed] [Google Scholar]
- 2.Dejour H., Walch G., Neyret P., Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76(1):45–54. [PubMed] [Google Scholar]
- 3.Doskocil M. Formation of the femoropatellar part of the human knee joint. Folia Morphol (Praha) 1985;33(1):38–47. [PubMed] [Google Scholar]
- 4.Dupont J.Y. Patellar subluxation: where are we in 1995? Acta Orthop Belg. 1995;61(3):155–168. [PubMed] [Google Scholar]
- 5.Garron E., Jouve J.L., Tardieu C., Panuel M., Dutour O., Bollini G. Anatomic study of the anterior patellar groove in the fetal period. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(5):407–412. [PubMed] [Google Scholar]
- 6.Kaymaz B., Atay O.A., Ergen F.B., Mermerkaya M.U., Olgun Z.D., Atesok K., Doral M.N. Development of the femoral trochlear groove in rabbits with patellar malposition. Knee Surg Sports Traumatol Arthrosc. 2013;21(8 (Aug)):1841–1848. doi: 10.1007/s00167-012-2163-7. [DOI] [PubMed] [Google Scholar]
- 7.Miller G.F. Familial recurrent dislocation of the patella. J Bone Joint Surg Br. 1978;60-B(2):203–204. doi: 10.1302/0301-620X.60B2.659465. [DOI] [PubMed] [Google Scholar]
- 8.Nietosvaara Y. The femoral sulcus in children. An ultrasonographic study. J Bone Joint Surg Br. 1994;76(5):807–809. [PubMed] [Google Scholar]
- 9.Nietosvaara Y., Aalto K. The cartilaginous femoral sulcus in children with patellar dislocation: an ultrasonographic study. J Pediatr Orthop. 1997;17(1):50–53. [PubMed] [Google Scholar]
- 10.Salzmann G.M., Weber T.S., Spang J.T., Imhoff A.B., Schottle P.B. Comparison of native axial radiographs with axial MR imaging for determination of the trochlear morphology in patients with trochlear dysplasia. Arch Orthop Trauma Surg. 2010;130(3):335–340. doi: 10.1007/s00402-009-0912-y. [DOI] [PubMed] [Google Scholar]
- 11.Schottle P.B., Hensler D., Imhoff A.B. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):147–151. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]
- 12.Tardieu C., Dupont J.Y. The origin of femoral trochlear dysplasia: comparative anatomy, evolution, and growth of the patellofemoral joint. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(4):373–383. [PubMed] [Google Scholar]
- 13.Walmsley R. The development of the patella. J Anat. 1940;74(Pt 3):360–368. 363. [PMC free article] [PubMed] [Google Scholar]


