Abstract
As a biologically-mediated pathway between adversity and declines in physical health, allostatic load has been frequently hypothesized as a potential contributor to racial disparities in birth outcomes, but empirical evidence is lacking. The purpose of this study was to examine the relationships between maternal preconception allostatic load, race, and adverse birth outcomes within the context of neighborhood-level poverty using data from the Bogalusa Heart Study. Allostatic load was quantified as a count of regulatory biomarkers falling in the highest risk quartile of the sample distribution as measured from a physical examination that took place prior to conception. Consistent with previous findings, African American women resided in more impoverished neighborhoods and had higher allostatic load scores compared to whites; however, allostatic load was not associated with preterm birth or low birthweight in fully adjusted models. These results underscore a need for further refinement of both biologic and contextual measures that capture holistically the way in which stressful conditions and experiences encountered across the life-course influence health potentials and engender inequities in reproductive health outcomes.
Keywords: allostatic load, stress, pregnancy, race, birth outcomes
Introduction
Decades of policy and public health intervention targeting reproductive health have done little to reduce the disproportionately high rates of adverse perinatal outcomes experienced by African American women compared to women of other racial and ethnic groups in the United States (Alexander, Wingate et al. 2008, Lu, Kotelchuck et al. 2010). Moving beyond individual and interpersonal-level risk factors, a growing body of research has examined social and structural determinants of reproductive health in an effort to explain the persistence of racial disparities (Kramer, Hogue 2009). Evidence indicates that characteristics of the physical and social environment in which women reside – crime rates (Messer, Kaufman et al. 2006, Masi, Hawkley et al. 2007), residential segregation (Kramer, Cooper et al. 2010, Bell, Zimmerman et al. 2006), neighborhood poverty and deprivation (Janevic, Stein et al. 2010, Metcalfe, Lail et al. 2011, Schempf, Kaufman et al. 2011, Giurgescu, Zenk et al. 2012), and income inequality (Olson, Diekema et al. 2010, Huynh, Parker et al. 2005), for example – negatively impact their health and that of their infant. Differential exposure to such stressors that may be more common in racially or socioeconomically disadvantaged groups may lead to gradients in health outcomes along racial or socioeconomic lines.
Less is known about the biological mechanisms by which exposure to such stressors affect health and functioning (Metcalfe, Lail et al. 2011). Allostatic load is a theoretical construct that represents dysregulation across the body's multiple physiological systems responsible for maintaining equilibrium when faced with physical or social challenges (McEwen 1998). It is the cumulative physiological wear and tear wrought on the body by over-activation of the physiologic stress response that places an individual at increased risk for onset of stress-related clinical diseases (McEwen, Seeman 1999, McEwen 2000). Measurements of allostatic load are typically derived from biomarkers representing multiple physiologic domains (e.g. cardiovascular, metabolic, immune, and endocrine) (Juster, McEwen et al. 2010). While studies vary considerably in their operationalization of allostatic load, including the constituent biomarkers used to measure it, results consistently implicate its role as a biologically-mediated pathway between adversity and negative health outcomes (Juster, McEwen et al. 2010, Carlson, Chamberlain 2005). Allostatic load has been shown to be higher among individuals of lower socioeconomic position (Crimmins, Kim et al. 2009), those living in impoverished or deprived neighborhoods (Merkin, Basurto-Davila et al. 2009, Bird, Seeman et al. 2010, Blair, Raver et al. 2011, Schulz, Mentz et al. 2012), non-whites (Geronimus, Hicken et al. 2006, Chyu, Upchurch 2011, Deuster, Kim-Dorner et al. 2011, Duru, Harawa et al. 2012), and those in situations of more directly observable daily, chronic stress (e.g. caregivers) (Roepke, Mausbach et al. 2011). Moreover, high allostatic load scores have been associated with increased risks for a number of stress-related chronic morbidities, declines in cognitive functioning, and all-cause mortality (Seeman, McEwen et al. 2001, Karlamangla, Singer et al. 2002, Gruenewald, Seeman et al. 2006, Karlamangla, Singer et al. 2006, Juster, McEwen et al. 2010, Beckie 2012).
As a model of biological risk patterned by chronic and repeated stressors over the life-course, it follows that allostatic load leading up to the time of pregnancy would be associated with negative birth outcomes (Lu, Halfon 2003). Dysregulation of the hypothalamic-pituitary axis – the primary mediator of allostatic load – may result in higher outputs of stress hormones during pregnancy leading to preterm labor (Hobel, Goldstein et al. 2008). Furthermore, excess glucocorticoids may result in immune-suppression, placing the woman at risk for infections and subsequently a heightened pro-inflammatory response associated with preterm labor or premature rupture of membranes (Goldenberg, Culhane 2003). Given the biologic plausibility of allostatic load as a biological mediator of the effect of class- or race-based stress on birth outcomes, it is frequently hypothesized as a contributor to disparities in reproductive health (Lu, Halfon 2003, Tiedje 2003, Hogue, Bremner 2005, Morello-Frosch, Shenassa 2006, Shannon, King et al. 2007, Latendresse 2009), but empirical evidence is sparse.
In a previous manuscript based on the same population analyzed in the current study, we examined associations with low birthweight, preterm birth, and small-for-gestational age and found no difference in risk by allostatic load level, race, or maternal education at time of birth (Wallace, Harville, et al. under review). In the follow-up analyses presented here, we sought to examine more closely the relationships between allostatic load, race, and adverse birth outcomes within the context of neighborhood-level poverty. With the availability of neighborhood-level socioeconomic indicators in the current study, applying a socioecological framework in this manner may provide valuable insight into the mechanisms behind stress and racial disparities in birth outcomes particularly given the historical and contextual factors unique to African American women in the south. The legacy and accumulation of race- and class-based discrimination and mistreatment experienced by these women as a socially-defined racial group in addition to may contribute to the persistence of reproductive health inequities.
Methods
Identification of Study Population
Women included in these secondary analyses are participants of the Bogalusa Heart Study (BHS), a biracial (African American/white) study begun by researchers now at Tulane who have been rigorously researching cardiovascular health in children and young adults since 1973 (Berenson, McMahan et al. 1980). Surveys of all school children in the semi-rural town of Bogalusa, Louisiana were repeated approximately every two years through 1994, enrolling new children each time and re-examining those previously enrolled. Examinations continued as participants aged into adulthood, the most recent completed in 2009 (Chen, Srinivasan et al. 2010). Bogalusa Heart Study investigators provided access to the study data for the purposes of this investigation which was approved by the Tulane University Institutional Review Board.
Birth records for the 1,354,951 births that occurred in the state of Louisiana between the years 1990 and 2009, inclusive, were provided by the Louisiana Department of Health and Hospitals, Office of the State Registrar and Vital Records. A three-stage data linkage procedure was used to identify mother-infant pairs of women who had participated in at least one BHS examination prior to conception and her firstborn infant using LinkPro v3.0 (InfoSoft, Inc., Winnipeg, MB) (Figure 1). First, an exact match of social security number was sought for each woman with a non-missing SSN was categorized as follows: 1:1 match (women with only one birth), 1:N match (women with multiple births), and unmatched (including truly nulliparous women and women with missing or potentially typo-error SSN in the birth records). All SSN matches (1:1 and 1:N) were considered definite matches (total of 973 women matched to 1,730 infants).
Figure 1.
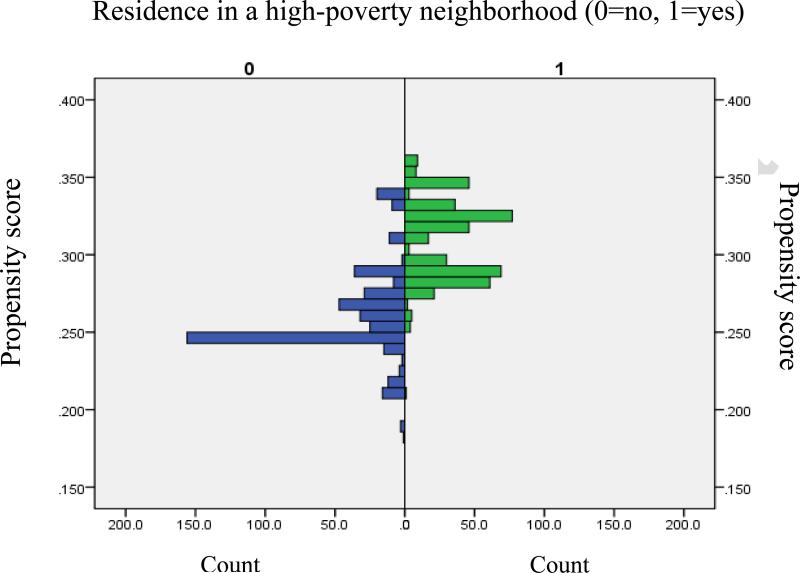
Propensity score matching. Propensity for living in a high-poverty neighborhood by actual residence in a high-poverty neighborhood (1) vs. a low-poverty neighborhood (0).
In the second stage, all women who remained unmatched to a birth record after Stage I (n=4,886) were included in a probabilistic linkage based on maternal date of birth (day, month, year), first name, last name, and Soundex codes for first and last names . Records with exact matches on all seven variables were classified as true-matches (814 women matched to 2,140 infants). Records that matched on four or fewer variables were excluded as non-matches. The remaining 335 records (those matched on five or six of the seven variables) were reviewed manually and classified as either true-matches or non-matches by comparison of matching variables with alternate values for names and date of birth, as well as maternal race and address variables not used in the matching strategy.
Finally, Stage III of the linkage repeated Stage II for all women who remained unmatched this time using the child's last name (and Soundex code) from the birth record and maternal last name from BHS. The same rules for minimum number of matching variables and manual review for classification of non-matches and true-matches were applied as in stage II.
Combining true matches from all three stages resulted in a single dataset of 2,773 women matched to 5,227 infants. Limiting the dataset to singleton first births resulted in 2,743 mother-infant pairs. Of these, 1,497 (54.6%) had a BHS examination that occurred prior to the date of conception, 1,467 (98.0%) had data from that examination on at least one of the 9 allostatic load biomarkers and 866 (final sample size) had complete data on all 9 biomarkers (352 African American, 514 white).
Individual-level measures
Preconception allostatic load was derived from the following nine biomarkers collected at a BHS examination that occurred prior to conception: systolic and diastolic blood pressure (SBP and DBP), total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides, glucose, insulin, and waist circumference. Where women were seen at more than one BHS examination prior to conception, biomarker values from the most recent visit were used. Allostatic load scores were quantified in each individual by summing the number of biomarkers falling within the highest risk quartile (bottom 25th percentile for HDL, top 25th percentile for all others) of the age-adjusted sample distribution. This is a frequently utilized operationalization of allostatic load, representing a multi-systemic index of physiologic dysregulation.(Juster, McEwen et al. 2010). Possible allostatic load scores in this sample therefore ranged from 0 (women with all 9 biomarkers of allostatic load falling within normal ranges) to 9(women for whom all 9 biomarkers were measured in the highest risk quartile, indicating the greatest degree of dysregulation).
Detailed descriptions of the BHS risk screening examinations at which these biomarkers were collected have been published in greater detail elsewhere (Berenson, McMahan et al. 1980). Briefly, the physical examination involved triplicate waist circumference measurement midway between the rib cage and the superior border of the iliac crest. Right arm blood pressure was measured in triplicate with mercury sphygmomanometers by each of 2 trained observers on subjects in a relaxed, seated position; means of 6 replicate blood pressure readings were used for both SBP and DBP. All subjects were instructed to fast for 12 hours prior to the examination and blood draw. Plasma glucose level was measured as part of a multiple chemistry profile (SMA20) with the multichannel Olympus Au-5000 analyzer (Olympus, Lake Success, NY). A radioimmunoassay kit was used to measure plasma insulin (Phadebas insulin kit, Pharmacia Diagnostics, Piscataway, NJ). Serum cholesterol and triglycerides levels were assayed enzymatically on the Hitachi 902 Automatic Analyzer (Roche Diagnostics, Indianapolis, Ind) (Srinivasan S.R., Berenson G.S. 1983). All laboratories responsible for processing BHS samples are rigorously monitored for quality control, precision and accuracy by independent institutions.
Additional individual-level variables studied included maternal race, age and education at time of first birth (less than high school, high school, greater than high school), smoking during pregnancy (yes/no), year of BHS examination at which allostatic load measure was derived, and years between that exam and date of last menstrual period (preconception years).
Neighborhood-level poverty
For the purposes of this study, “neighborhood” was defined as U.S .Census block group, based on the Census 2000 TIGER Line/Shapefiles. Where available, participant's address number, street, city, state, and zip of residence at the time of the BHS examination from which the allostatic load measure was derived were georeferenced into U. S. census block group using ESRI ArcGIS for Desktop Version 10.1 (Redlands, CA: Environmental Systems Research Institute). The final sample of 866 women resided in 55 census block groups, and the number of women-infant pairs per block group ranged from 1 to 151 (mean=6).
Neighborhood-level poverty was defined as the percentage of households living below the federal poverty level in a single block group. Block-group poverty levels were obtained from Census data and linked to participants’ georeferenced block group location. Given the broad range of years at which participant's preconception BHS examinations took place, data on neighborhood-level poverty were obtained from both Census 1990 and Census 2000. For women whose preconception BHS examination occurred between the years 1987-1993, block group poverty levels were obtained from Census 1990. For preconception examinations that occurred between 1998-2003, data were obtained from Census 2000. Finally, for women whose examination took place from 1994-1997, neighborhood poverty was estimated as the mean of Census 1990 and Census 2000 values. For the purposes of modeling, neighborhood poverty was dichotomized into high poverty (>27% of households below poverty level, top quartile of the sample distribution) or low poverty (≤27% of households below poverty level). Individuals were then categorized by their race and poverty level of the neighborhood in which they resided (white, low poverty neighborhood; white, high poverty neighborhood; African American, low poverty neighborhood African American, high poverty neighborhood).
Birth outcomes
Birth weight and gestational age of infants born to women participants of BHS were extracted from the birth records. Gestational age on the birth record is an estimation based on the date of last menstrual period. When the date is unknown or missing, gestational age is based on a clinical estimate (as estimated by attendant) for birth records from 1990-2002 and later replaced by an obstetric estimate (as estimated by attendant based on all perinatal factors including ultrasound) for records issued after 2003 (Wier, Pearl et al. 2007). Low birthweight was defined as a birth weight of less than 2,500 grams and births before 37 completed weeks gestation were classified as preterm.
Statistical Analyses
All individual-level variables, potential confounders, and birth outcomes were stratified by race to assess their bivariate distributions. Descriptive analyses also included a crude comparison of difference in neighborhood poverty by race as well as the cross-distribution of participants by allostatic load quartile and neighborhood poverty quartile among African American and whitewomen separately.
To address potential structural confounding, participants were frequency-matched based on their propensity for residing in a high-poverty neighborhood. Given the greater probability (propensity) for living in a high poverty neighborhood among women who did so (Figure 1), propensity-score matching should reduce potential unmeasured structural confounding between women across poverty levels. Generalized estimating equations (GEE) were used to estimate racial disparities in low birthweight and preterm birth associated with allostatic load, individual-level socioeconomic position (education), and a combined race-neighborhood poverty level variable.. Models accounted for propensity-score matched individuals and clustering within neighborhood and were adjusted for maternal, age, smoking during pregnancy, year of BHS examination and years between examination and conception.
Results
Allostatic load was derived from biomarkers measured at a BHS examination that occurred an average of 6.8 years prior to conception. African American women were significantly younger at the time of their first birth and had significantly higher mean preconception allostatic load score compared to whites (Table 1). African American women, on average, lived in neighborhoods with a greater proportion of households below the federal poverty level compared to white women (31.7% vs. 17.7%). Allostatic load scores were considered high if they fell in the top (4th) quartile of the distribution of scores, corresponding to a value of 3 or more in this sample. Twenty-two percent (n=76)of African American mothers had high allostatic load and lived in high poverty neighborhoods compared to only 3.3% (n= 17) of white women (Table 2).
Table 1.
Descriptive Statistics of individual-level demographics, biological indicators and pregnancy outcomes and neighborhood-level poverty by race (N=866).
| African American (n=352) | White (n=514) | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Age at time of exama | 13.4 | 5.7 | 4 | 34 | 15.8 | 6.5 | 5 | 35 |
| Age at first birtha | 20.9 | 4.8 | 13 | 41 | 23.3 | 5.1 | 13.0 | 39.0 |
| Years between allostatic load measurement and conception (preconception years) | 6.7 | 4.3 | 0 | 16 | 6.9 | 4.3 | 0 | 16 |
| Allostatic load biomarkers | ||||||||
| SBP, mmHg | 103.7 | 9.7 | 83.0 | 134.6 | 103.8 | 9.1 | 78.0 | 145.7 |
| DBP, mmHg | 64.3 | 9.7 | 37.7 | 91.0 | 65.4 | 8.0 | 41.3 | 92.7 |
| Waist circumference, cm | 69.9 | 14.6 | 45.1 | 122.0 | 69.3 | 12.6 | 45.6 | 132.0 |
| Total cholesterol, mg/dL | 174.5 | 30.5 | 100.0 | 312.0 | 171.2 | 32.0 | 97.0 | 309.0 |
| High Density Lipoprotein, mg/dL a | 57.2 | 13.1 | 27.0 | 103.0 | 50.8 | 11.3 | 22.0 | 102.0 |
| Low Density Lipoprotein, mg/dL | 106.3 | 27.0 | 38.2 | 230.0 | 105.2 | 27.3 | 40.3 | 219.1 |
| Triglycerides, mg/dL a | 67.8 | 30.5 | 24.0 | 286.0 | 93.3 | 94.5 | 26.5 | 520.0 |
| Glucose, mg/dL | 79.9 | 15.0 | 43.0 | 317.0 | 80.4 | 17.9 | 59.0 | 365.0 |
| Insulin, uU/mL a | 13.9 | 9.5 | 3.6 | 80.0 | 11.5 | 7.0 | 3.2 | 68.0 |
| Allostatic load scorea | 2.6 | 1.7 | 0 | 8 | 2.1 | 1.9 | 0 | 8 |
| Neighborhood poverty, %a | 31.7 | 17.2 | 1.0 | 59.2 | 17.7 | 10.5 | 0 | 46.9 |
| N | % | N | % | |||||
|---|---|---|---|---|---|---|---|---|
| Low birthweighta | 49 | 13.9 | 37 | 7.2 | ||||
| Preterm birth | 44 | 12.5 | 47 | 9.1 | ||||
| Education (at time of first birth)a | ||||||||
| More than high school | 94 | 26.7 | 220 | 42.8 | ||||
| High school | 146 | 41.5 | 188 | 36.6 | ||||
| Less than high school | 112 | 31.8 | 106 | 20.6 | ||||
| Smoked during pregnancya | 11 | 3.1 | 92 | 17.9 |
P<0.01
Table 2.
Number Percentage of individuals by level of allostatic load and neighborhood poverty among White and African American study participants (N=866).
| Quartile of neighborhood povertyb | ||||
|---|---|---|---|---|
| Quartile of allostatic load score by racea | 1st | 2nd | 3rd | 4th |
| African American (n=352) | ||||
| 1st | 8 (2.3%) | 18 (5.1%) | 5 (1.4%) | 35 (9.9%) |
| 2nd | 5 (1.4%) | 17 (4.8%) | 14 (4.0 %) | 44 (12.5%) |
| 3rd | 6 (1.7%) | 26 (7.4%) | 15 (4.3%) | 29 (8.2%) |
| 4th | 10 (2.8%) | 28 (8.0%) | 16 (4.5%) | 76 (21.6%) |
| White (n=514) | ||||
| 1st | 28 (5.5%) | 60 (11.7%) | 39 (7.6%) | 10 (2.0%) |
| 2nd | 14 (2.7%) | 67 (13.0%) | 35 (6.8%) | 11 (2.1%) |
| 3rd | 14 (2.7%) | 37 (7.2%) | 24 (4.7%) | 10 (2.0%) |
| 4th | 25 (4.9%) | 64 (12.5%) | 59 (11.5%) | 17 (3.3%) |
Allostatic load score quartile values are as follows: 1st = 0, 2nd=1, 3rd=2, 4th≥3 or more.
Neighborhood poverty quartile values are as follows: 1st ≤ 10.2%, 2nd = from 10.3% to 20.6%, 3rd = from 20.7% to 29.4%, and 4th ≥ 29.5%
A racial disparity in low birthweight was apparent in this sample (13.9% among African Americans, 7.2% among whites, P<0.01), and although the rate of preterm birth appeared higher in African American women compared to whites (12.5% vs. 9.1%), this difference was not statistically significant.
In unadjusted models, allostatic load was not associated with either adverse birth outcome. Table 3 presents the odds ratios and 95% confidence intervals from fully-adjusted GEE models for associations with low birthweight and preterm birth. Allostatic load was not significantly associated with low birth weight or preterm birth for African American or white mothers controlling for race, neighborhood socioeconomic status, maternal education, maternal age at time of birth, smoking during pregnancy, year of BHS examination and years between examination and conception.
Table 3.
Odds Ratios of low birthweight and preterm birth associated with maternal race and neighborhood poverty level and allostatic load.a
| Low birthweight |
Preterm Birth |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Allostatic load | 1.10 | 0.93 | 1.31 | 1.01 | 0.85 | 1.19 |
| Race and Neighborhood Poverty Levelb | ||||||
| White, low poverty | Referent | Referent | ||||
| White, higher poverty | 3.39d | 1.42 | 8.11 | 2.11 | 0.98 | 4.52 |
| African American, low poverty | 5.23d | 2.26 | 12.10 | 2.56c | 1.19 | 5.49 |
| African American, higher poverty | 3.51c | 1.01 | 12.19 | 2.37 | 0.80 | 7.05 |
| Education | ||||||
| More than high school | Referent | Referent | ||||
| High school | 1.52 | 0.63 | 3.67 | 0.77 | 0.35 | 1.72 |
| Less than high school | 1.07 | 0.34 | 3.31 | 0.82 | 0.30 | 2.29 |
Model controlled for maternal age at time of birth, smoking during pregnancy, year of BHS examination and years between examination and conception
High poverty defined as top quartile of neighborhood poverty distribution (>27.0% of families below federal poverty level)
<0.05
<0.001
White women living in a high poverty neighborhood and African American women in either a low or high poverty neighborhood were more likely to have a low birthweight infant compared to white women living in a low poverty neighborhood. The association was strongest for African American women living in neighborhoods of lowpoverty, who were more than 5 times as likely to have a low birthweight infant than white women in lowpoverty (OR: 5.23, 95% CI: 2.26, 12.10). Likewise, women in this group – African Americans in low poverty – were more likely to have given birth preterm compared to white women in the same low poverty neighborhoods. There was no statistical difference in the likelihood of preterm birth for African American women in high poverty or white women in high poverty compared to white women in low poverty. Finally, maternal education, as an indicator of individual-level socioeconomic position, was not associated with either preterm birth or low birth weight in the fully adjusted models that included allostatic load and the grouped race/neighborhood poverty variable.
Discussion
Our aim in the present analysis was to examine a potential mechanism by which chronic stress accumulates in the body over time with implications for preconception health and racial disparities in adverse birth outcomes. Consistent with previous literature, we found that mean allostatic load score was higher among African American women compared to whites, and that African American women were more likely to reside in a higher-poverty neighborhood.(Merkin, Basurto-Davila et al. 2009, Seeman, Gruenewald et al. 2010, Chyu, Upchurch 2011) . We also found a higher percentage of low birthweight infants and a higher albeit nonsignificant rate of preterm birth among African American women compared to white, trends supported by our state and national birth outcomes data (Martin, Hamilton et al. 2011, Marian F. MacDorman, T.J. Mathews 2011).
Contrary to our hypothesis, however, we did not find that allostatic load predicted low birthweight or preterm birth in the models that included race and neighborhood poverty level. Nor was there a significant association between neighborhood poverty level and allostatic load in this sample with adjustment for race (data not shown). In a study based in Detroit, Schulz, et al. (Schulz, Mentz et al. 2012) reported a positive association between neighborhood poverty and allostatic load with residents of higher-poverty neighborhoods (> 20% of households below the poverty line) had an average 10% higher allostatic load score. Moreover, they found that the relationship between neighborhood poverty and allostatic load was mediated through perceived psychosocial stress and not by health-related behaviors (Schulz, Mentz et al. 2012). It may be that in the absence of psychosocial stress measures we were unable to tease out and disentangle the pathways through which poverty and allostatic load together impact women's health and pregnancy outcomes. Furthermore, tests of potential mediating pathways between poverty, allostatic load, and birth outcomes may require additional structural and psychosocial indicators given the unique cultural context of this sample of young, semi-rural women in the southern US (Janevic, Stein et al. 2010).
An additional finding from these analyses is that among the groupings that considered both the individual's race and the level of poverty in the neighborhood in which they resided, African American women in areas of lower poverty appeared to fare worst relative to whites in the same low-poverty neighborhoods, compared with both white and African American women from impoverished neighborhoods, independent of individual socioeconomic position. Messer et al.(Messer, Vinikoor et al. 2008) found that compared to a low-poverty neighborhood, living in a higher poverty neighborhood increased the odds of preterm birth among white women, but the association was non-significant for black women with adjustment for maternal age and education. Similarly, O'Campo et al.,(O'Campo, Burke et al. 2008) reported greater effect estimates of the relationship between neighborhood poverty and preterm birth among white women compared to those estimated among non-Hispanic Black women in race-stratified models, a difference that may be partially explained by the narrower range of depravation distribution among the Black women in their sample. Conversely, the distribution of neighborhood poverty percentage was broader among African American women in our sample compared to whites.
Taken together, this evidence suggests that while poverty has deleterious effects on reproductive health for all women regardless of race, higher neighborhood socioeconomic position does not necessarily eliminate the disproportionate burden of adverse outcomes among African American women compared to whites, and in this instance, appears to exacerbate the disparity. Reasons for our finding are unclear, but suggest additional factors such as racial segregation,(Kramer, Cooper et al. 2010, Bell, Zimmerman et al. 2006) institutionalized racism,(Mendez, Hogan et al. 2012) or perceived discrimination (Giurgescu, Zenk et al. 2012) may be influencing the relationship between neighborhood environment and adverse birth outcomes among African American women in areas of lower poverty. It may be that responses to racial discrimination – which vary by socioeconomic position in the degree of socialization parents impart on families – may be more protective in neighborhoods characterized by high levels of poverty disorder (Caughy, O'Campo et al. 2004).
There are limitations to these analyses for consideration. First, our definition of “neighborhood” as census block group undoubtedly mischaracterized neighborhood or community as would be perceived by the individuals living within them. This problem of neighborhood definition is not new to social epidemiology (Messer, Vinikoor et al. 2008), and it both limits comparison across studies and prohibits causal inference regarding neighborhood-level effects. Ideally, future studies can incorporate more carefully considered groupings of individuals within salient, community-based geographical areas that capture the stressors and stress buffers experienced by residents on a daily basis. Further, we had no information on the amount of time these women lived in the neighborhood prior to the time of allostatic load measurement or for the period of time between the allostatic load measurement and conception of their first born child. However, given the relatively young age of this sample and the school-based nature of recruitment for the Bogalusa Heart Study, it is reasonable to assume that most if not all of these women had spent a majority a of their young lives in the neighborhood in which we classified them. Our measure of allostatic load therefore should have captured the physiologic effects of cumulative exposure to the neighborhood environment occurring though childhood and into adolescence (Theall, Drury et al. 2012).
Despite its limitations, this analysis does contribute to the literature by being one of the first to empirically measure the effect of allostatic load on adverse birth outcomes, taking into account individual- and neighborhood-level stressors. In prior work we estimated the effect of allostatic load on African American and white women in New Orleans, a very different cultural, structural, and social context from that of Bogalusa (Wallace, Harville 2012). In that study, which was limited in sample size and number of allostatic load biomarkers, we found a small positive association between allostatic load and gestational age, such that higher maternal allostatic load decreased gestational age at birth. We found no racial difference in the magnitude of effect of allostatic load on gestational age or birth weight. In addition to a larger sample size and a greater number of allostatic load biomarkers, data available for the current study allowed us to examine a measure allostatic load prior to pregnancy, an important improvement given the known physiologic changes that occur during pregnancy independent of preexisting physiologic dysregulation (Shannon, King et al. 2007). Further, the life-course perspective suggests that birth outcomes are not only the result of exposures that occur during the weeks of gestation, but are influenced by the accumulation of exposures leading up to the time of pregnancy (Lu, Halfon 2003). As such, we examined maternal allostatic load an index of stress accumulation in the years leading up to pregnancy.
The persistence of racial disparities in perinatal outcomes implicates the profoundly pervasive nature of the political, economic, and social processes that drive health inequity above and beyond the effects of demographics, health behaviors, and individual-level resources. Describing the biologic pathways by which theses process get “under the skin” to affect the health of women and their children will require a great deal of future work and research that is both relevant to social policy and amenable to individual-level intervention.
Research Highlights.
Provides initial empirical test of the effect of allostatic load on birth outcomes.
Considers the contextual effects of race within neighborhood-level poverty.
African American women more likely to have higher allostatic load levels.
Allostatic load does not predict preterm birth or low birthweight.
Acknowledgements
This study was supported by grants ES-021724 from National Institute of Environmental Health Science, and AG-16592 from the National Institute on Aging and the Eunice Kennedy Shriver National Institute of Child Health And Human Development (T32HD057780 to MEW). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- ALEXANDER GR, WINGATE MS, BADER D, KOGAN MD. The increasing racial disparity in infant mortality rates: composition and contributors to recent US trends. American Journal of Obstetrics and Gynecology. 2008;198(1):51, e1–51, e9. doi: 10.1016/j.ajog.2007.06.006. [DOI] [PubMed] [Google Scholar]
- BECKIE TM. A systematic review of allostatic load, health, and health disparities. Biological research for nursing. 2012;14(4):311–346. doi: 10.1177/1099800412455688. [DOI] [PubMed] [Google Scholar]
- BELL JF, ZIMMERMAN FJ, ALMGREN GR, MAYER JD, HUEBNER CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Social science & medicine. 2006;1982;63(12):3030–3045. doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- BERENSON GS, MCMAHAN CA, VOORS AW, WEBBER LS, SRINIVASAN SR, FRANK GC, FOSTER TA, BLONDE CV. Cardiovascular risk factors in children: the early natural history of atherosclerosis and essential hypertension. Oxford University Press; New York: 1980. [Google Scholar]
- BIRD CE, SEEMAN T, ESCARCE JJ, BASURTO-DAVILA R, FINCH BK, DUBOWITZ T, HERON M, HALE L, MERKIN SS, WEDEN M, LURIE N. Neighbourhood socioeconomic status and biological ‘wear and tear’ in a nationally representative sample of US adults. Journal of epidemiology and community health. 2010;64(10):860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BLAIR C, RAVER CC, GRANGER D, MILLS-KOONCE R, HIBEL L, FAMILY LIFE PROJECT KEY INVESTIGATORS Allostasis and allostatic load in the context of poverty in early childhood. Development and psychopathology. 2011;23(3):845–857. doi: 10.1017/S0954579411000344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARLSON ED, CHAMBERLAIN RM. Allostatic load and health disparities: a theoretical orientation. Research in nursing & health. 2005;28(4):306–315. doi: 10.1002/nur.20084. [DOI] [PubMed] [Google Scholar]
- CAUGHY MO, O'CAMPO PJ, MUNTANER C. Experiences of racism among African American parents and the mental health of their preschool-aged children. American Journal of Public Health. 2004;94(12):2118–2124. doi: 10.2105/ajph.94.12.2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHEN W, SRINIVASAN SR, BERENSON GS. Amplification of the association between birthweight and blood pressure with age: the Bogalusa Heart Study. Journal of hypertension. 2010;28(10):2046–2052. doi: 10.1097/HJH.0b013e32833cd31f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHYU L, UPCHURCH DM. Racial and ethnic patterns of allostatic load among adult women in the United States: findings from the National Health and Nutrition Examination Survey 1999-2004. Journal of women's health (2002) 2011;20(4):575–583. doi: 10.1089/jwh.2010.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CRIMMINS EM, KIM JK, SEEMAN TE. Poverty and biological risk: the earlier “aging” of the poor. The journals of gerontology.Series A, Biological sciences and medical sciences. 2009;64(2):286–292. doi: 10.1093/gerona/gln010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DEUSTER PA, KIM-DORNER SJ, REMALEY AT, POTH M. Allostatic load and health status of African Americans and whites. American Journal of Health Behavior. 2011;35(6):641–653. doi: 10.5993/ajhb.35.6.1. [DOI] [PubMed] [Google Scholar]
- DURU OK, HARAWA NT, KERMAH D, NORRIS KC. Allostatic load burden and racial disparities in mortality. Journal of the National Medical Association. 2012;104(1-2):89–95. doi: 10.1016/s0027-9684(15)30120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GERONIMUS AT, HICKEN M, KEENE D, BOUND J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GIURGESCU C, ZENK SN, DANCY BL, PARK CG, DIEBER W, BLOCK R. Relationships among neighborhood environment, racial discrimination, psychological distress, and preterm birth in African American women. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN / NAACOG. 2012;41(6):E51–61. doi: 10.1111/j.1552-6909.2012.01409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOLDENBERG RL, CULHANE JF. Infection as a cause of preterm birth. Clinics in perinatology. 2003;30(4):677–700. doi: 10.1016/s0095-5108(03)00110-6. [DOI] [PubMed] [Google Scholar]
- GRUENEWALD TL, SEEMAN TE, RYFF CD, KARLAMANGLA AS, SINGER BH. Combinations of biomarkers predictive of later life mortality. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(38):14158–14163. doi: 10.1073/pnas.0606215103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOBEL CJ, GOLDSTEIN A, BARRETT ES. Psychosocial stress and pregnancy outcome. Clinical obstetrics and gynecology. 2008;51(2):333–348. doi: 10.1097/GRF.0b013e31816f2709. [DOI] [PubMed] [Google Scholar]
- HOGUE CJ, BREMNER JD. Stress model for research into preterm delivery among black women. American Journal of Obstetrics and Gynecology. 2005;192(5 Suppl):S47–55. doi: 10.1016/j.ajog.2005.01.073. [DOI] [PubMed] [Google Scholar]
- HUYNH M, PARKER JD, HARPER S, PAMUK E, SCHOENDORF KC. Contextual effect of income inequality on birth outcomes. International journal of epidemiology. 2005;34(4):888–895. doi: 10.1093/ije/dyi092. [DOI] [PubMed] [Google Scholar]
- JANEVIC T, STEIN CR, SAVITZ DA, KAUFMAN JS, MASON SM, HERRING AH. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Annals of Epidemiology. 2010;20(6):445–451. doi: 10.1016/j.annepidem.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JUSTER R, MCEWEN BS, LUPIEN SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- KARLAMANGLA AS, SINGER BH, MCEWEN BS, ROWE JW, SEEMAN TE. Allostatic load as a predictor of functional decline. MacArthur studies of successful aging. Journal of clinical epidemiology. 2002;55(7):696–710. doi: 10.1016/s0895-4356(02)00399-2. [DOI] [PubMed] [Google Scholar]
- KARLAMANGLA AS, SINGER BH, SEEMAN TE. Reduction in allostatic load in older adults is associated with lower all-cause mortality risk: MacArthur studies of successful aging. Psychosomatic medicine. 2006;68(3):500–507. doi: 10.1097/01.psy.0000221270.93985.82. [DOI] [PubMed] [Google Scholar]
- KRAMER MR, COOPER HL, DREWS-BOTSCH CD, WALLER LA, HOGUE CR. Metropolitan isolation segregation and Black-White disparities in very preterm birth: a test of mediating pathways and variance explained. Social science & medicine (1982) 2010;71(12):2108–2116. doi: 10.1016/j.socscimed.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KRAMER MR, HOGUE CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiologic reviews. 2009;31:84–98. doi: 10.1093/ajerev/mxp003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LATENDRESSE G. The interaction between chronic stress and pregnancy: preterm birth from a biobehavioral perspective. Journal of midwifery & women's health. 2009;54(1):8–17. doi: 10.1016/j.jmwh.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LU MC, HALFON N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Maternal and child health journal. 2003;7(1):13–30. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- LU MC, KOTELCHUCK M, HOGAN V, JONES L, WRIGHT K, HALFON N. Closing the Black-White gap in birth outcomes: a life-course approach. Ethnicity & disease. 2010;20(1 Suppl 2):S2–62-76. [PMC free article] [PubMed] [Google Scholar]
- MARIAN F, MACDORMAN TJ, MATHEWS . Understanding Racial and Ethnic Disparities in U.S. Infant Mortality Rates. National Center for Health Statistics; Hyattsville, MD: 2011. [PubMed] [Google Scholar]
- MARTIN JA, HAMILTON BE, VENTURA SJ, OSTERMAN MJ, KIRMEYER S, MATHEWS TJ, WILSON EC. Births: final data for 2009. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2011;60(1):1–70. [PubMed] [Google Scholar]
- MASI CM, HAWKLEY LC, PIOTROWSKI ZH, PICKETT KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Social science & medicine (1982) 2007;65(12):2440–2457. doi: 10.1016/j.socscimed.2007.07.014. [DOI] [PubMed] [Google Scholar]
- MCEWEN BS. The neurobiology of stress: from serendipity to clinical relevance. Brain research. 2000;886(1-2):172–189. doi: 10.1016/s0006-8993(00)02950-4. [DOI] [PubMed] [Google Scholar]
- MCEWEN BS. Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- MCEWEN BS, SEEMAN T. Protective and damaging effects of mediators of stress. Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- MENDEZ DD, HOGAN VK, CULHANE JF. Stress during Pregnancy: The Role of Institutional Racism. Stress and health : journal of the International Society for the Investigation of Stress. 2012 doi: 10.1002/smi.2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MERKIN SS, BASURTO-DAVILA R, KARLAMANGLA A, BIRD CE, LURIE N, ESCARCE J, SEEMAN T. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Annals of Epidemiology. 2009;19(3):194–201. doi: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MESSER LC, KAUFMAN JS, DOLE N, SAVITZ DA, LARAIA BA. Neighborhood crime, deprivation, and preterm birth. Annals of Epidemiology. 2006;16(6):455–462. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- MESSER LC, VINIKOOR LC, LARAIA BA, KAUFMAN JS, EYSTER J, HOLZMAN C, CULHANE J, ELO I, BURKE JG, O'CAMPO P. Socioeconomic domains and associations with preterm birth. Social science & medicine (1982) 2008;67(8):1247–1257. doi: 10.1016/j.socscimed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- METCALFE A, LAIL P, GHALI WA, SAUVE RS. The association between neighbourhoods and adverse birth outcomes: a systematic review and meta-analysis of multi level studies. Paediatric and perinatal epidemiology. 2011;25(3):236–245. doi: 10.1111/j.1365-3016.2011.01192.x. [DOI] [PubMed] [Google Scholar]
- MORELLO-FROSCH R, SHENASSA ED. The environmental “riskscape” and social inequality: implications for explaining maternal and child health disparities. Environmental health perspectives. 2006;114(8):1150–1153. doi: 10.1289/ehp.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'CAMPO P, BURKE JG, CULHANE J, ELO IT, EYSTER J, HOLZMAN C, MESSER LC, KAUFMAN JS, LARAIA BA. Neighborhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. American Journal of Epidemiology. 2008;167(2):155–163. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- OLSON ME, DIEKEMA D, ELLIOTT BA, RENIER CM. Impact of income and income inequality on infant health outcomes in the United States. Pediatrics. 2010;126(6):1165–1173. doi: 10.1542/peds.2009-3378. [DOI] [PubMed] [Google Scholar]
- ROEPKE SK, MAUSBACH BT, PATTERSON TL, VON KANEL R, ANCOLI- ISRAEL S, HARMELL AL, DIMSDALE JE, ASCHBACHER K, MILLS PJ, ZIEGLER MG, ALLISON M, GRANT I. Effects of Alzheimer caregiving on allostatic load. Journal of health psychology. 2011;16(1):58–69. doi: 10.1177/1359105310369188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCHEMPF AH, KAUFMAN JS, MESSER LC, MENDOLA P. The neighborhood contribution to black-white perinatal disparities: an example from two north Carolina counties, 1999-2001. American Journal of Epidemiology. 2011;174(6):744–752. doi: 10.1093/aje/kwr128. [DOI] [PubMed] [Google Scholar]
- SCHULZ AJ, MENTZ G, LACHANCE L, JOHNSON J, GAINES C, ISRAEL BA. Associations between socioeconomic status and allostatic load: effects of neighborhood poverty and tests of mediating pathways. American Journal of Public Health. 2012;102(9):1706–1714. doi: 10.2105/AJPH.2011.300412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEEMAN T, GRUENEWALD T, KARLAMANGLA A, SIDNEY S, LIU K, MCEWEN B, SCHWARTZ J. Modeling multisystem biological risk in young adults: The Coronary Artery Risk Development in Young Adults Study. American Journal of Human Biology : The Official Journal of the Human Biology Council. 2010;22(4):463–472. doi: 10.1002/ajhb.21018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEEMAN TE, MCEWEN BS, ROWE JW, SINGER BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHANNON M, KING TL, KENNEDY HP. Allostasis: a theoretical framework for understanding and evaluating perinatal health outcomes. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN / NAACOG. 2007;36(2):125–134. doi: 10.1111/j.1552-6909.2007.00126.x. [DOI] [PubMed] [Google Scholar]
- SRINIVASAN SR, BERENSON GS. Serum lipoproteins in children and methods for study. Handbook of Electrophoresis edn. CRC Press; Boca Raton, FL: 1983. pp. 185–204. [Google Scholar]
- THEALL KP, DRURY SS, SHIRTCLIFF EA. Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. American Journal of Epidemiology. 2012;176(Suppl 7):S164–74. doi: 10.1093/aje/kws185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TIEDJE LB. Psychosocial pathways to prematurity: changing our thinking toward a lifecourse and community approach. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN / NAACOG. 2003;32(5):650–658. doi: 10.1177/0884217503257529. [DOI] [PubMed] [Google Scholar]
- WALLACE ME, HARVILLE EW. Allostatic Load and Birth Outcomes Among White and Black Women in New Orleans. Maternal and child health journal. 2012 doi: 10.1007/s10995-012-1083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WIER ML, PEARL M, KHARRAZI M. Gestational age estimation on United States livebirth certificates: a historical overview. Paediatric and perinatal epidemiology. 2007;21(Suppl 2):4–12. doi: 10.1111/j.1365-3016.2007.00856.x. [DOI] [PubMed] [Google Scholar]