Abstract
Intratesticular epidermoid cysts are rare solid tumorlike lesions. They constitute 1% of all testicular tumors. Major advances have been achieved during the last decades, shifting the management of epidermoid cysts to a more conservative approach.
We present a case of a 20-year-old male who was referred to the urology department with a two-year history of a gradually increasing painless right-sided scrotal lump. We will discuss the diagnostic work up of intratesticular epidermoid cyst, with the operative management and literature review.
Keywords: epidermoid cyst, scrotal ultrasound, testicular mass
INTRODUCTION
Intratesticular epidermoid cyst is an uncommon clinical condition affecting mostly young men, presenting as a painless testicular mass. We report a 20-year-old male presenting with a two-year history of a painless right intratesticular epidermoid cyst, with the work up diagnosis and management. In addition, literature review with consensus of management is presented.
CASE REPORT
A 20-year-old male was referred to the urology outpatient clinic with a two-year history of a gradually increasing painless right-sided scrotal lump. He had no relevant history of trauma or infection. The mass has noticeably increased in size over the last six months, which raised a concern by his general practitioner.
Clinical examination confirmed a non-tender 1.5 cm hard mass involving the upper part of the right testis. The rest of the examination was normal.
All tumor markers were negative. In addition, a scrotal ultrasound showed a well-defined 1.5 cm intratesticular mass with a classical onion ring pattern, which is highly suggestive of an epidermoid cyst (Fig. 1). However, due to the fact of the recent increase in size the patient was counseled for inguinal exploration with frozen section and possible orchiectomy.
Fig. 1.
Ultrasound image of epidermoid cyst showing classic onion ring pattern.
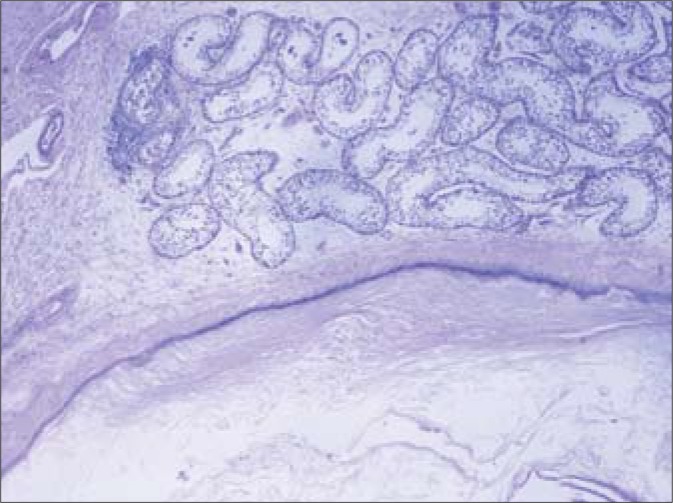
Inguinal exploration was performed and a frozen section confirmed epidermoid cyst adherent to the overlying tunica albuginea (Fig. 2). Hence, the testis was spared.
Fig. 2.
Histological image of the frozen section of epidermoid cyst.
The patient recovered well from the operation and was reviewed in the outpatient clinic at 6-weeks. The wound healed and the right testis was in a good condition.
DISCUSSION
Intratesticular epidermoid cysts are rare testicular tumor-like lesions. They constitute 1% of all testicular tumors [1]. Major advances have been achieved during the last decades, shifting the management of epidermoid cysts to a more conservative approach [2].
The usual presentation is an incidental finding of a painless testicular mass, with the right side presentation being the predominant side [3].
Intratesticular epidermoid cysts share a unique ultrasonographic characteristics mainly presenting in the form of a wellcircumscribed hypoechoic mass with a hyperechogenic rim and center. In addition, extensive keratinization inside the cyst makes a characteristic onion skin-like appearance, seen in ultrasound scan and magnetic resonance imaging (MRI) studies, which strongly supports the diagnosis [4]. However, recently it has been shown that mature teratomas might have a similar ultrasonic feature to the epidermoid cysts [5]. Therefore, though a triad of findings including the sonographic appearance of an onion ring, avascularity on Doppler sonography, and negative results of tumor marker studies-is highly suggestive of an epidermoid cyst, due to the above-mentioned it would be unsafe to completely rely on ultrasound [6].
Histologic sections of these tumors classically show a squamous epithelial layer lining the cyst and multiple concentric laminated layers of keratin. More importantly, they lack dermal components such as hair follicles and sebaceous glands, which differentiate them from mature teratoma [7].
CONCLUSION
Intratesticular epidermoid cysts are rare benign intratesticular growths with distinctive clinical and ultrasonographic characteristics. Clinical assessment and understanding the benign intrascrotal processes is the key to making a diagnosis. Ultrasound has an important role and adds essential information. Once clinical assessment and radiological findings support the diagnosis, a testis sparing procedure should be performed.
REFERENCES
- 1.Ross JH, Kay R, Elder J. Testis sparing surgery for pediatric epidermoid cysts of the testis [see comments] J Urol. 1993;149:353–356. doi: 10.1016/s0022-5347(17)36080-9. [DOI] [PubMed] [Google Scholar]
- 2.Dieckmann KP, Loy V. Epidermoid cyst of the testis: A review of clinical and histogenetic considerations. Br J Urol. 1994;73:436–441. doi: 10.1111/j.1464-410x.1994.tb07611.x. [DOI] [PubMed] [Google Scholar]
- 3.Heidenreich A, Engelmann UH, Vietsch HV, et al. Organ preserving surgery in testicular epidermoid cysts. J Urol. 1995;153:1147–1150. [PubMed] [Google Scholar]
- 4.Eustace S, Graham D, Behan M, et al. Ultrasonographic diagnosis and surgical enucleation of an epidermoid cyst of the testis. Br J Urol. 1994;74:518–519. doi: 10.1111/j.1464-410x.1994.tb00437.x. [DOI] [PubMed] [Google Scholar]
- 5.Maizlin ZV, Belenky A, Baniel J, et al. Epidermoid cyst and teratoma of the testis: sonographic and histologic similarities. J Ultrasound Med. 2005;24(10):1403–1409. doi: 10.7863/jum.2005.24.10.1403. quiz 1410-1411. [DOI] [PubMed] [Google Scholar]
- 6.Dogra VS, Gottlieb RH, Rubens DJ, et al. Testicular epidermoid cysts: sonographic features with histopathologic correlation. J Clin Ultrasound. 2001;29(3):192–196. doi: 10.1002/1097-0096(200103/04)29:3<192::aid-jcu1018>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 7.Garrett JE, Cartwright PC, Snow BW, et al. Cystic testicular lesions in the pediatric population. J Urol. 2000;163:928–936. [PubMed] [Google Scholar]