Abstract
Milk of calcium (MOC) is a colloidal suspension of calcium salts occurring in calyceal cysts and diverticula. Although reported to be rare, in fact it seems to be more common than previously thought. It has characteristic appearances on plain x-rays, ultrasound, and CT imaging particularly in the prone and supine positions. Often entirely asymptomatic, its appearance may be mistaken for renal stones on radiography or angiomyolipomas on ultrasonography. In this paper, a series of cases is presented outlining its characteristic features and reviewing the relevant literature.
Keywords: milk of calcium, renal cysts, renal stone milk of calcium cysts
INTRODUCTION
Ludin and Howald first described milk of calcium (MOC) renal cysts in 1940 [1] while the first radiological description was made by Holm in 1948 and demonstrated layering in such a cyst [2]. Since then there have been sporadic reports of MOC cysts in the literature. With the advent of better imaging tools, such as real-time ultrasound (RTUS), computed tomography (CT), and magnetic resonance imaging (MRI) scanning, MOC cysts are being diagnosed more commonly than before [3]. We present a series of cases of MOC cysts and review the relevant literature.
CASE REPORT
Patient 1
A 38-year-old man presented with classic right renal colic symptoms, with tenderness elicited in his right loin. He was apyrexial with normal biochemical and hematological investigations. Intravenous urography (IVU) demonstrated delayed excretion on the right with appearances suggestive of a 4-5 mm stone at the lower end of the right ureter. Ureteroscopy was performed and two small stone fragments were successfully removed. Serum uric acid, calcium, oxalate, phosphate, and 24 hr. urine tests were normal. A follow-up IVU performed two months later was entirely normal.
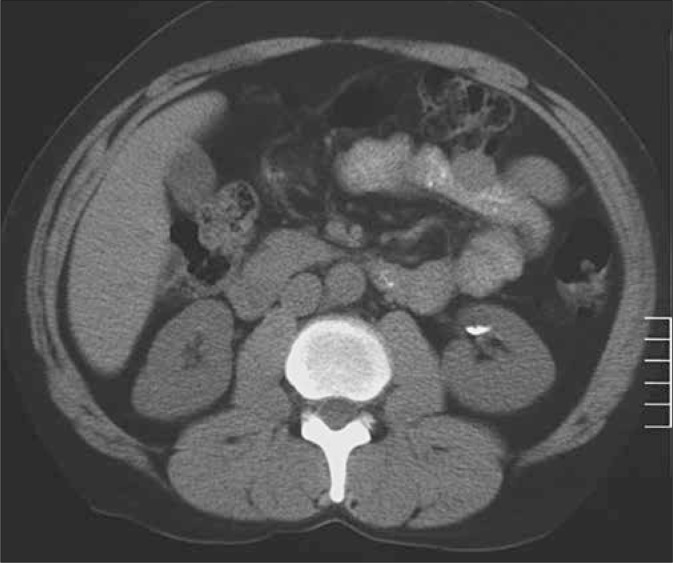
He presented eight months later with LUTS, but pain now in the left loin. KUB (kidneys, ureter, and bladder) and ultrasound (USG) imaging demonstrated three calcified densities in the upper and middle pole of the left kidney. He underwent ESWL treatment using the Storz SLK Lithotripter, but the post-treatment KUB revealed no fragmentation with only a change noted in the configuration of the densities. A critical review of the x-ray films resulted in a CT scan being performed which demonstrated a left renal cyst containing calcium layering out in a dependent fashion, apparent in both the supine and prone images (Fig. 1).
Fig. 1.
Supine non-contrast CT scan. Left Kidney: Milk of calcium (MOC) seen layering out in a left anterior renal cyst.
Patient 2
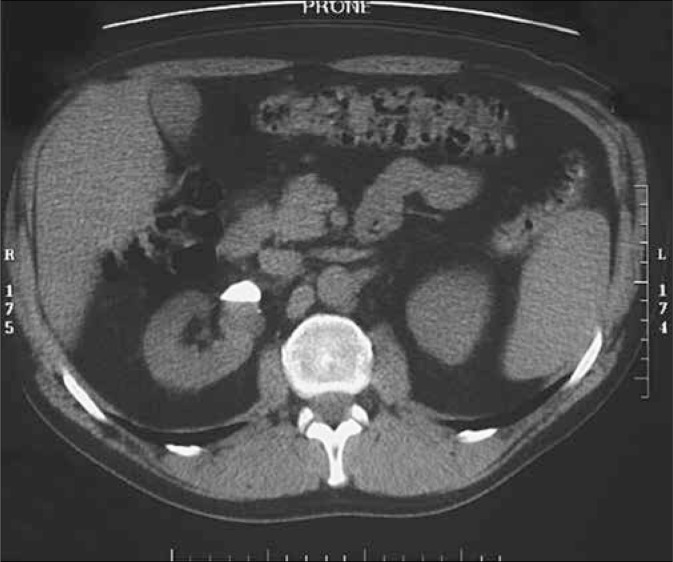
A 54-year-old man experienced bilateral loin pain and frank hematuria lasting for a few days. He had received ESWL to a left renal calculus 12 years prior to presentation. He was apyrexial with normal abdominal examination. Urinalysis revealed microscopic hematuria although with negative urine cultures. KUB revealed a right upper quadrant dense opacity possibly lying within the right kidney. USG of the kidney failed to detect a renal stone. A CT scan was performed and suggested the presence of bilateral renal cysts with a calcium fluid interface characteristic of MOC cysts (Fig. 2).
Fig. 2.
Prone non-contrast CT scan, section through the kidneys. Left kidney: Dense material (milk of calcium) layers out in a dependent fashion with a stark fluid-fluid level.
He had a normal cystoscopy; 24-hr urine collections demonstrated elevated levels of calcium and oxalates. He admitted to high calcium intake with regular daily intake of milk and cheese. He was commenced on bendrofluazide and given the necessary dietary information regarding renal stones.
Patient 3
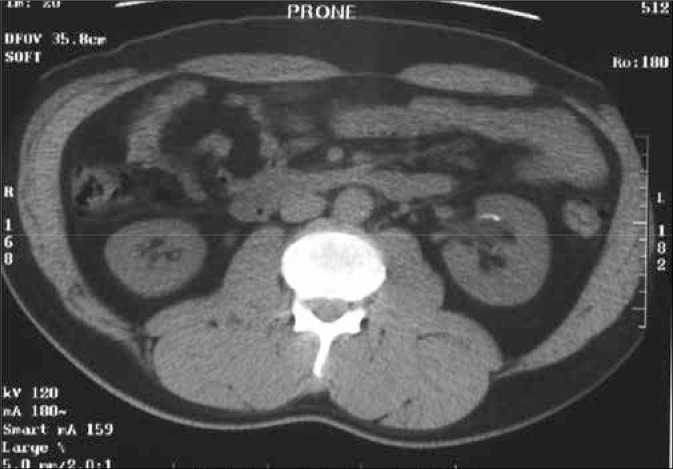
A 44-year-old man with a past history of renal stones presented with left loin pain of 24 hr. duration. MSU was normal with a trace of blood on dipstick testing. Excretory urography and USG demonstrated a left pelvicalyceal cyst with a 0.5 cm radiopaque calculus communicating with the collecting system. He received two treatments of ESWL to the left renal stone at an interval of four weeks, which led to successful fragmentation. Post-treatment KUB showed some stone fragments, but they were relatively small in size and did not require further treatment. His 2-year follow-up KUB demonstrated a significant increase in the size of the radiopaque density. Given that he was known to have a pelvicalyceal cyst, a CT scan was requested and confirmed the presence of calcium fluid interface with characteristic layering, in addition to a few small calculi with the cyst (Fig. 3). As he had remained asymptomatic, no further action was deemed necessary.
Fig. 3.
Prone non-contrast CT scan, section through the kidneys. Right kidney: Milk of calcium (MOC) layers out in the anterior renal cyst. It is impossible to determine whether the low attenuation lesion is a cyst or a diverticulum on these unenhanced scans.
Patient 4
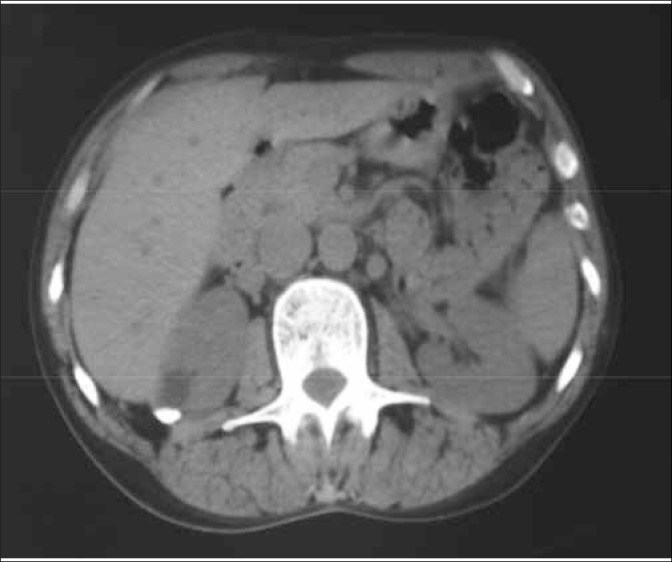
A 55-year-old man presented with right renal colic and macroscopic hematuria. He subsequently passed a small stone with resolution of his symptoms. An IVU was performed, the right kidney and ureter were normal but an incidental 1.0 cm radiopaque density was noted in the left renal pelvis. USG revealed a left parapelvic cystic structure measuring 2.4 cm in diameter, containing a 1.3cm focus of calcification within its lateral margins. CT demonstrated a 14 mm left parapelvic cyst showing no significant enhancement (-2 to -3 Hounsfield units) with characteristic layering in a dependent fashion, apparent in both the supine and prone images consistent with MOC cysts (Fig. 4).
Fig. 4.
Prone non-contrast CT scan. Left kidney: Low attenuation cyst in the anterior cortex of the left kidney demonstrating layering out of milk of calcium (MOC) in the prone position.
Serum biochemistry was normal but 24-hr urine collection demonstrated high urinary calcium (↑9.08 mmol/24hr normal 2.5-7.5 m.mol/hr.), oxalate (↑880 m.mol/hr. normal 80-490 m.mol/hr.), and phosphate (↑80.9 mmol/24hr normal 15-50 m.mol/hr.) levels. He was given the standard dietary advice and commenced on bendroflumethiazide.
Patient 5
A 46-year-old female presented with vague intermittent right upper quadrant and loin pain. She denied any urinary symptoms and the urinalysis was negative. IVU demonstrated a 13 mm calcific density in the upper pole of the right kidney with prompt bilateral excretion. USG revealed a 2.5 cm echogenic lesion in the liver with posterior acoustic enhancement consistent with a hemangioma. The appearances of the renal lesion were of mixed low and high attenuation with a fluid level. There were no solid elements within it. A non-contrast CT scan confirmed the presence of a 2.5 cm cyst in the right posterior superior renal cortex with a fluid interface and characteristic calcific layering posteriorly in the supine position (Fig. 5). A diagnosis of MOC cyst was made and the patient's symptoms were attributed to the possible hemangioma.
Fig. 5.
Supine non-contrast CT scan, axial section through the kidneys. Low attenuation cyst in the posterior cortex of the right kidney contains milk of calcium (MOC), layering out with fluid-fluid level.
DISCUSSION
Pyelocalyceal diverticula also referred to as pericalyceal cysts or calyceal diverticula are eventrations of the upper collecting system, which lie within the renal parenchyma and communicate via a narrow channel with the collecting system. They are smooth walled and are lined by transitional epithelium. Mostly they are asymptomatic, measuring <1 cm in diameter and discovered incidentally on an IVU. They are seen in 21- 45 of every 10,000 IVUs and found bilaterally in 3% of cases with equal incidence in both sexes [4, 5].
Pyelocalyceal diverticula are associated with urinary tract infections, renal calculi, flank pain, pyuria, micro and macroscopic hematuria, and hypertension. They can present as a renal mass and sometimes may contain MOC [4, 6].
MOC is a viscous colloidal suspension of calcium carbonate, calcium phosphate, calcium oxalate, and occasionally ammonium phosphate [4]. They are seen in two groups of patients, each with their own characteristic features. The first and the largest group of patients have MOC in a calyceal diverticulum, while the second group have multiple radiodense levels of MOC in the dilated calyces of a hydronephrotic kidney [7].
The etiology of MOC is uncertain but obstruction and inflammation seem to be key factors [8, 9]. Obstruction and stagnation of urine possibly results in super-saturation of calcium salts resulting in the formation of calcium microliths. Due to a disturbance in stone forming and inhibiting factors a dynamic equilibrium probably results, preventing the aggregation of the microliths. Why the microliths do not increase in size and form a stone remains unexplained [7].
Fig. 6.
Case 3: 2-year follow-up KUB demonstrated a significant increase in the size of the radio – opaque density, proven on CT as MOC.
Fig. 7.
Case 4(a): Ultrasonography revealed a left parapelvic cystic structure measuring 2.4 cm in diameter, containing a 1.3 cm focus of calcification within its lateral margins.
Fig. 8.
Case 4(b): Control film showing 1 cm radio-opaque density in the left renal pelvis.
The importance of MOC cysts lies in its recognition as it may avoid unnecessary procedures like ESWL [10, 11] or PCNLs [12].
The diagnosis can be made with a supine film. An upright or lateral decubitus film may show the half moon shaped calcification changing with respect to the patient's position. However this is not always easy, as MOC cysts may opacify poorly or lack the classical appearance [12]. MOC cysts can be mistaken for a renal stone or a gallstone if they lie in the right upper quadrant region.
Their appearance in IVU depends on whether there is a patent communication with the collecting system as most calyceal diverticula tend to opacify better in delayed films [6].
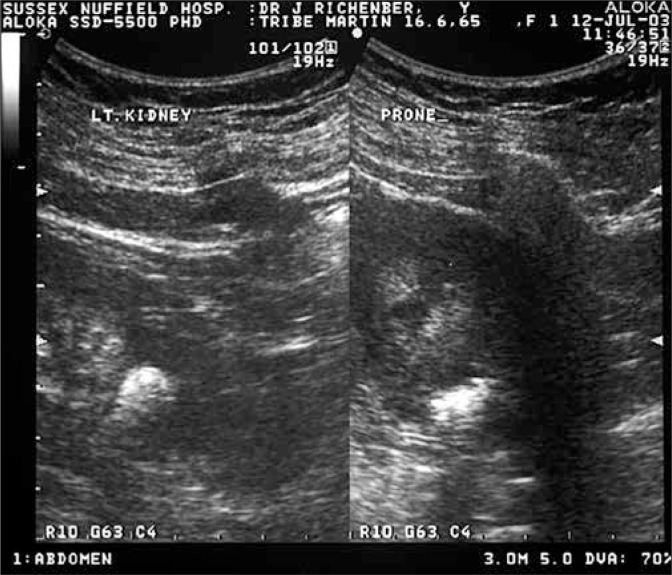
MOC cysts exhibit characteristic gravity-dependent, acoustic shadows on ultrasonography, which are helpful in differentiating it from either a renal stone or an angiomyolipomas [13].
A non-contrast CT scan is capable of demonstrating the layers of calcified material in the dependent portions of the cyst with the characteristic postural change on supine and prone positions [14]. These findings help differentiate it from renal calculi, tumor calcification, and AML. In our experience, CT has been more effective in the diagnosis as we have been able to demonstrate the characteristic layering effect in all of our patients.
Fig. 9.
Case 5: IVU: 13 mm calcific density in the upper pole of the right kidney with prompt bilateral excretion.
Kinard et al. has reported the use of MRI as extremely useful in the diagnosis of MOC cysts. Calcium emits a weak signal while the remainder of the fluid in the cyst gives an intense signal on the T1 and T2 weighted images, which can be used to demonstrate the characteristic layering of calcium. This appearance on MRI is virtually pathognomonic [5].
Pyelocalyceal cysts and diverticula are usually asymptomatic and require no further treatment, but they can become complicated or symptomatic requiring surgical treatment, which may involve a nephrectomy, hemi or partial nephrectomy, deroofing of the cyst [16] or endoscopic marsupialization with or without fulguration [9, 17].
In summary, MOC cysts should be considered as a possible differential diagnosis when dealing with vague opacities in the kidney and before further treatment is instituted. Investigations such as USG and CT imaging should be performed, thereby avoiding unwarranted intervention.
REFERENCES
- 1.Lüdin M, Howald R. Eine eigenartige intrarenale Zyste. Schwiezerisches medizinisches Wochenschrift. 1940;70:230–232. [Google Scholar]
- 2.Holm H. On pyelogenic renal cyst. ACTA. 1948;29:87–89. [Google Scholar]
- 3.Yeh HC, Mitty HA, Halton K, et al. Milk of calcium in renal cysts: new sonographic features. J Ultrasound Med. 1992;11(5):195–203. doi: 10.7863/jum.1992.11.5.195. [DOI] [PubMed] [Google Scholar]
- 4.Wulfsohn Mendley A. Pyelocalyceal diverticula. J Urol. 1980;123(1):1–8. doi: 10.1016/s0022-5347(17)55748-1. [DOI] [PubMed] [Google Scholar]
- 5.Timmons JW, Jr, Malek RS, Hattery RR, Deweerd JH. Calyceal diverticulum. J Urol. 1975;114(1):6–9. doi: 10.1016/s0022-5347(17)66930-1. [DOI] [PubMed] [Google Scholar]
- 6.Gayer G, Apter S, Heyman Z, Morag B. Pyelocalyceal diverticula containing milk of calcium--CT diagnosis. Clinical Radiology. 1998;53(5):369–371. doi: 10.1016/s0009-9260(98)80011-1. [DOI] [PubMed] [Google Scholar]
- 7.McCorkell SJ, Hefty TR, Dowling AD. Bilateral milk-of-calcium urine and hydronephrosis. J Urol. 1985;133(1):77–78. doi: 10.1016/s0022-5347(17)48793-3. [DOI] [PubMed] [Google Scholar]
- 8.Melekos MD, Kosti PN, et al. Milk of calcium cysts masquerading as renal calculi. Eur J Radiol. 1998;28(1):62–66. doi: 10.1016/s0720-048x(97)00106-x. [DOI] [PubMed] [Google Scholar]
- 9.Kikuchi E, Sumitomo M, Hatakeyama N, et al. Percutaneous endoscopic marsupialization of a pyelocalyceal diverticulum with milk of calcium stones. Urol Int. 1998;60(1):62–65. doi: 10.1159/000030206. [DOI] [PubMed] [Google Scholar]
- 10.Biyani CS, Bhatia V. Renal milk of calcium--a new contraindication to extracorporeal shock wave lithotripsy? Br J Urol. 1992;70(4):447–448. doi: 10.1111/j.1464-410x.1992.tb15809.x. [DOI] [PubMed] [Google Scholar]
- 11.Vandeursen H, Baert L. An intrarenal opacity resisting extracorporeal shock wave lithotripsy. J Urol. 1990;144(4):961–962. doi: 10.1016/s0022-5347(17)39632-5. [DOI] [PubMed] [Google Scholar]
- 12.Langer W, Theiss M, Hofmockel G, Frohmuller H. Atypical findings in a patient with a renal milk-of-calcium cyst. Urology. 1996;48(1):135–138. doi: 10.1016/s0090-4295(96)00105-7. [DOI] [PubMed] [Google Scholar]
- 13.Patriquin H, Lafortune M, Filiatrault D. Urinary milk of calcium in children and adults: use of gravity-dependent sonography. Am J Roentgenol. 1985;144(2):407–413. doi: 10.2214/ajr.144.2.407. [DOI] [PubMed] [Google Scholar]
- 14.Bude RO, Korobkin MT. Milk of calcium renal cyst: CT findings. Urology. 1992;40(2):149–151. doi: 10.1016/0090-4295(92)90515-x. [DOI] [PubMed] [Google Scholar]
- 15.Kinard RE, Orrison WW, Brogdon BG, Kaude JV. MR imaging of milk of calcium renal cyst. J Comput Assist Tomogr. 1986;10(6):1057–1059. doi: 10.1097/00004728-198611000-00036. [DOI] [PubMed] [Google Scholar]
- 16.Williams G, Blandy JP, Tresidder GC. Communicating cysts and diverticula of the renal pelvis. Br J Urol. 1969;41(2):163–170. doi: 10.1111/j.1464-410x.1969.tb09918.x. [DOI] [PubMed] [Google Scholar]
- 17.Hulbert JC, Reddy PK, Hunter DW, et al. Percutaneous techniques for the management of calyceal diverticula containing calculi. J Urol. 1986;135(2):225–227. doi: 10.1016/s0022-5347(17)45590-x. [DOI] [PubMed] [Google Scholar]