Abstract
The endoscopic injection of vesicoureteric orifices with synthetic or natural materials is a widely recognized method of treating vesicoureteral reflux (VUR). The aim of this study is to present two cases of clinically significant complications following the use of dextranomer/hyaluronic acid copolymer, which led to the progression of the reflux degree, permanent infection of the urinary tract, and the necessity to perform surgical treatment.
Keywords: vesicoureteral reflux, endoscopy, complication, Deflux®, UTI
INTRODUCTION
The endoscopic injection of the vesicoureteric orifices with synthetic or natural materials is a widely recognized method used in the treatment of vesicoureteral reflux (VUR). From among the synthetic materials available, the most frequently used one is Deflux®, a dextranomer/hyaluronic acid copolymer. As regards to complications following this method of therapy as described in the literature, only clinically insignificant transient infections of the urinary system and transient impotency of the upper urinary tract have been reported so far. In our study we describe far more serious complications following the use of Deflux® which may even lead to the progression of the reflux degree, permanent infection of the urinary tract, and/or the necessity for surgical intervention.
MATERIALS AND METHODS
Case 1
In 2005, a 3-year-old girl with recurrent infections of the urinary tract was diagnosed with a left-sided third-degree VUR. The child was qualified for endoscopic treatment and Deflux® injection into the vesical ostium of the left ureter was performed two months later. Following the procedure, the infection of the urinary tract still persisted. Three years later, the miction cystography performed in our health center revealed the presence of a left-sided fifth-degree VUR. As a result, the patient qualified for the re-implantation of the ureter.
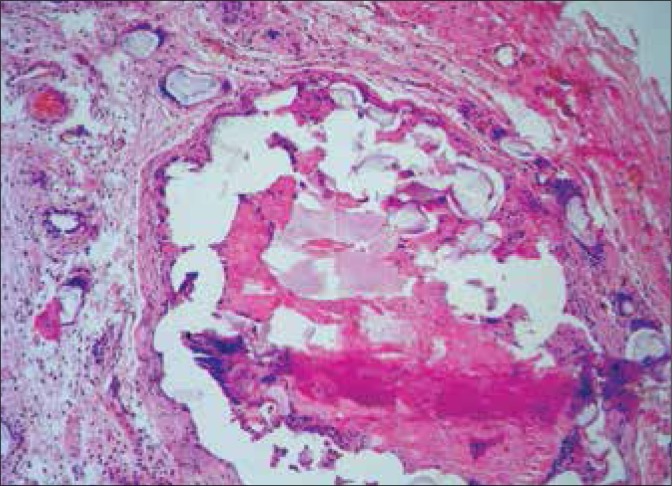
After the opening of the bladder, a hard inflammatory infiltrate in the area of the vesical ostium was found, which made the intravesical dissection impossible. The left ureter was transplanted using the Politano-Leadbetter method, having previously resected its intraparietal and paraureteral segments affected by the hard infiltrate. The excised 2-centimeter ureteral segment was then sent for histopathological examination, which revealed a significantly exfoliated transitional epithelium with a visible chronic inflammatory lymphocyte infiltrate beneath. Outside the muscular coat, a focus 2-milimeters in diameter was visible (Fig. 1). It was formed by droplets of iatrogenic origin and surrounded by polynucleic histiocytes.
Fig. 1.
Transverse section of the ureter in the external muscular layer. Droplets of the iatrogenic substance (Deflux®) surrounded by polynucleic histiocytes. Staining with hematoxylin-eosin. mag. 200x.
After surgery, the infections of the urinary tract remitted. A miction cystography performed six months later did not show any features of reflux. During the subsequent two-year observation period, the child did not require any pharmacological treatment.
Case 2
An 8-year-old girl with recurrent urinary tract infections that persisted three years after endoscopic treatment of 2nd degree bilateral VUR with Deflux® was subjected to a miction cystography, which revealed the presence of 2nd degree VUR on the right side and 3rd degree VUR on the left side. The patient was subsequently qualified for surgical treatment. A bilateral reimplantation of the ureters by Foure method was performed. Intraoperative findings included: hard inflammatory infiltrates around the paraureteral segments of both ureters, a palpable lump on the wall of the left ureter, and granulomas of the urinary bladder wall at the vesical ostia. The questionable lesions were removed and sent for histopathological investigation.
On microscopic examination, a chronic inflammatory lymphocytic infiltrate was found around both fragments of the resected ureters with a cluster of a substance of iatrogenic origin surrounded by polynucleic histiocytes located outside the muscular coat. The granulomas that were removed from the urinary bladder wall contained the muscular coat of the bladder with pseudocysts filled with a substance of iatrogenic origin, as well as amorphic calcifications, calcified eosinophilic necrotic masses, and clusters of histiocytes (Fig. 2). The lump from the wall of the left ureter was a similar pseudocyst with a band of polynucleic histiocytes visible on its internal layer and externally surrounded by a band of the fibrous connective tissue.
Fig. 2.
Ureter. Small calcification area in the transitional epithelium. Lymphocytic and plasmocytic infiltration of the subepithelial area.
The postoperative course was uncomplicated. The infections of the urinary tract remitted. Miction cystography performed six months after the surgery did not show the presence of VUR. The scintigraphic picture of both kidneys one year after the operation was normal.
DISCUSSION
The endoscopic treatment of VUR with Teflon was introduced into clinical practice in 1981 by Matouschek [1]. In subsequent years, this method was popularized by O'Donnell and Puri [2]. Since that time numerous articles on the effectiveness and safety of various materials used for the purpose of injecting the vesical ostia of the ureters have been published.
The most extensive study on Teflon was published in 1998. Based on the analysis of 12,251 injections of refluxing ureters from 41 various centers, a 95.5% effectiveness of the Teflon method was demonstrated and no side-effects reported [3]. Also, researchers from Lyon, based on the results of 650 injections performed from 1986 to 1993, did not observe any early or late complications, including those related to remote Teflon migration [4].
Very good results with the use of silicone (Macroplastique) were presented by Oswald et al., who did not observe any local or remote complications [5]. Also, bovine collagen (Zynplast) and autologic chondrocytes were used with success.
The most recent discovery with regard to synthetic materials used in the endoscopic treatment of VUR, i.e. Deflux®, has also received enthusiastic opinions. A detailed analysis of the remote results of the endoscopic treatment of VUR showed, however, that there is no ideal synthetic material to be used for that purpose.
As early as in 1991, Bonnet et al. described the appearance of two granulomas as a side-effect reaction against the foreign matter of Teflon that was previously injected [6]. In1996, Italian pediatricians from a neuropsychiatric ward described the case of a 6-year-old girl who had sustained on ischemic brain stroke as a result of Teflon migration, and they also reported the resulting damage to the microcirculation [7]. One year later, urologists from Padova confirmed their observations of both the formation of huge granulomas around the clusters of Teflon, as an inflammatory reaction against the foreign matter, and the tendency of Teflon to migrate to distant areas [8]. Far less serious complications, such as urinary tract infection, hemorrhagic cystitis, obstruction of the injected ureter leading to hydronephrosis, epididymitis and edema of the urinary bladder, have been reported in the comparative studies on the effectiveness and safety of the use of different materials. Additionally, it turned out that the use of autologic chondrocytes was not absolutely safe, as the remaining calcifications were almost identical with the deposits at the vesicular ostium of the ureter, causing a colicky pain and erythrocyturia or hematuria [9].
In the light of the facts presented here, Deflux® has appeared to be the safest material so far. The only drawbacks reported following the use of this material for the treatment of VUR were the occurrence of transient infections of the urinary tract and transient obstructions of the ureter [10]. Nevertheless, the cases described above demonstrate that the use of Deflux® also involves the risk of appearance of serious and persistent complications, which not only resulted in the failure to correct VUR, but they also caused its high clinical advancement and the necessity to re-implant the ureters. In those cases, the use of Deflux® considerably delayed the performance of effective anti-reflux surgery; moreover, it made it far more risky and technically difficult because of the resulting dysfunction of the anatomical relations at the vesicoureteric junction.
CONCLUSIONS
The use of Deflux®, as in the case of other synthetic materials, involves the risk of serious complications.
In the two cases described above, even after the use of Deflux®, the reflux persisted and advanced clinically and was accompanied by persistent UTI, which was resistant to pharmocotherapy.
The histopathological examination of the abnormal masses removed from the area of the VUJ confirmed the presence of a long-lasting inflammation, the formation of granulomas, and pseudocysts around the Deflux® injection site.
REFERENCES
- 1.Matouschek E. Die Behandlung des vesicorenalen refluxes durch transuretherale (Einspritzung von polytetrafluoroethylenepaste) Urologe. 1981;20:263. [PubMed] [Google Scholar]
- 2.A'Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J. 1984;289:5–9. doi: 10.1136/bmj.289.6436.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puri P, Granata C. Multicenter survey of endoscopic treatment of vesicoureteral reflux using polytetrafluoroethylene. J Urol. 1998;160(3 Pt 2):1007–1011. doi: 10.1097/00005392-199809020-00011. [DOI] [PubMed] [Google Scholar]
- 4.Chaffange P, Dubois R, Bouhafs A, et al. Endoscopic treatment of vesicorenal reflux in children: short- and long-term results of polytetrafluoroethylene (Teflon) injections. Prog Urol. 2001;11:546–551. [PubMed] [Google Scholar]
- 5.Oswald J, Riccabona M, Lusuardi L, et al. Prospective comparison and 1-year follow-up of a single endoscopic subureteral polydimethylsiloxane versus dextranomer/hyaluronic acid copolymer injection for treatment of vesicoureteric reflux in children. Urology. 2002;60:894–897. doi: 10.1016/s0090-4295(02)01903-9. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet A, Grandcoin P, Sibert L, et al. Peri-ureteral granulomas after Teflon injection for vesicoureteral reflux. Prog Urol. 1991;1:1046–1050. [PubMed] [Google Scholar]
- 7.Borgatti R, Tettamanti A, Piccinelli P. Brain injury in a healthy child one year after periureteral injection of Teflon. Pediatrics. 1996;98(2 Pt 1):290–291. [PubMed] [Google Scholar]
- 8.Aragona F, D'Urso L, Scremin E, et al. Polytetrafluoroethylene giant granuloma and adenopathy: long-term complications following subureteral polytetrafluoroethylene injection for the treatment of vesicoureteral reflux in children. J Urol. 1997;158(4):1539–1542. doi: 10.1016/s0022-5347(01)64275-7. [DOI] [PubMed] [Google Scholar]
- 9.Gargollo PC, Paltiel H, Rosoklija I, Diamond DA. Mound calcification after endoscopic treatment of vesicoureteral reflux with autologous chondrocytes - a normal variant of mound appearance? J Urol. 2009;181:2702–2707. doi: 10.1016/j.juro.2009.02.053. [DOI] [PubMed] [Google Scholar]
- 10.Chi A, Gupta A, Snodgrass W. Urinary tract infection following successful dextranomer/hyaluronic acid injection for vesicoureteral reflux. J UroI. 2008;179:1966–1969. doi: 10.1016/j.juro.2008.01.054. [DOI] [PubMed] [Google Scholar]