Abstract
Introduction
Bladder exstrophy is the most common form of the exstrophy – epispadias complex. It is observed in 1:30 000 life births, about four times more often in boys than in girls. Iliac osteotomy is used to facilitate bringing together pubic bones and to minimize the tension of fused elements. To analyze complications after primary bladder exstrophy closure with a special consideration of the role of pelvic osteotomy.
Material and method
It is a retrospective study evaluating 100 patients (chosen by chance out of 356) with bladder exstrophy (65 boys and 35 girls), treated in Pediatric Urology Department of the Children's Memorial Health Institute in Warsaw, Poland between 1982 and 2006. All children underwent primary bladder exstrophy closure, among them 32 elsewhere. Primary bladder exstrophy closure with contemporary iliac osteotomy was done in 36 children. In the rest 64 patients bladder was closed without osteotomy, regardless child's age.
Results
Dehiscence after primary closure followed with bladder prolaps occurred in 31 patients, among them 13 out of 68 (19%) operated in our department and 18 out of 32 (56%) operated in another hospital. Primary bladder exstrophy closure with contemporary iliac osteotomy was done in 32 infants above 72 hours of life.
Conclusions
Osteotomy performed at primary bladder exstrophy closure diminishes the risk of wound dehiscence independently of patient's age. Posterior iliac osteotomy is sufficient and safe and could be repeated if necessary.
Keywords: bladder exstrophy, exstrophy epispadias complex, pelvic osteotomy
INTRODUCTION
Bladder exstrophy is the most common form of the exstrophy–epispadias complex. It is observed in one of every 30,000 live births, occurring about four times more often in boys than in girls. It is a complex defect that affects not only the urinary tract, but also the musculoskeletal, gastrointestinal, and genital systems. Developmental anomalies arise between the 6th and 10th week of gestation as a consequence of cloacal membrane hypertrophy, which prevents migration of the mesoderm between the ectoderm and endoderm [1]. This disrupts the development of the lower part of the abdominal wall with a consequent symphyseal diastasis and extension of the muscles and fascias of the anterior abdominal wall and pelvic diaphragm. Additionally, the anus and vagina are positioned more anteriorly. Extension and rotation of the pubic bones that are the attachment for the cavernosal bodies result in reduction and bending of the penis in boys and total cleft of the clitoris in girls (Fig. 1). Furthermore, the urogenital septum, in the form of two lateral bundles that attach the bladder neck region to the pubic bones, is also cleft. Total dissection of these bundles is necessary to position the bladder deep within the pelvis. The primary closure of bladder exstrophy is fundamental for further functional urethral, penile, and bladder neck reconstruction. It is therefore crucial not only to close the bladder, but also to place it properly in the pelvis. Fusion of the symphysis with reconstruction of all layers of the anterior abdominal wall is the basic element of the surgical procedure (Fig. 2). An iliac osteotomy is used to facilitate bringing together pubic bones and to minimize the tension of the fused elements. It is thought that osteotomy is not necessary in newborns up to 72 hours of life because the pubic bones are elastic enough to be brought together [2, 3]; however, is it the correct approach in such patients?
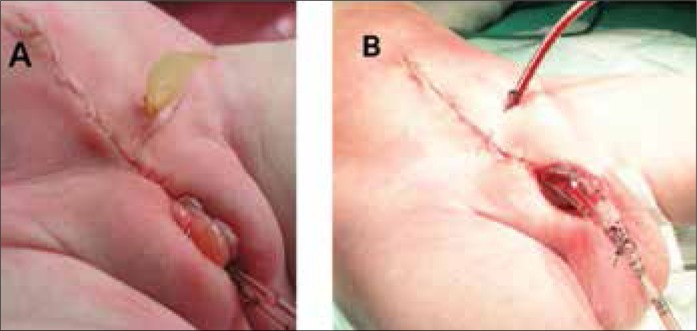
Figure 1.
A girl (a) and a boy (b) with bladder exstrophy before surgery.
Figure 2.
The same girl (a) and boy (b) in the end of primary bladder exstrophy closure with posterior iliac osteotomy.
This study aimed to analyze the complications after primary bladder exstrophy closure with special consideration for the role of pelvic osteotomy.
MATERIAL AND METHOD
This retrospective study evaluated 100 patients (randomly chosen from a database of 356 patients) with bladder exstrophy (65 boys and 35 girls) who were treated in the Pediatric Urology Department of the Children's Memorial Health Institute in Warsaw, Poland between 1982 and 2006. All children underwent primary bladder exstrophy closure, among them 32 who underwent surgery at institutions other than our own. Age at the primary closure did not exceed 1–year in 91 cases, of which 51 were newborns in the first three days of life. In the six children who had been operated on in other hospitals, there was no data about the children's age at the time of primary closure (Table 1).
Table 1.
Age at the primary bladder closure
| Age | Operation in our department | Operation in another hospital | Total |
|---|---|---|---|
| 1st day | 13 | 7 | 20 |
| 2nd day | 19 | 7 | 26 |
| 3rd day | 4 | 1 | 5 |
| 4–30 days | 14 | 5 | 19 |
| 1–12 months | 15 | 6 | 21 |
| >12 months | 3 | – | 3 |
| No data available | – | 6 | 6 |
| Total | 68 | 32 | 100 |
Primary bladder exstrophy closure with contemporary iliac osteotomy was performed in 36 children. In the remaining 64 patients, the bladder was closed without osteotomy, regardless child's age (Table 2).
Table 2.
Age at the primary closure with or without osteotomy
| Age | Closure without osteotomy | Closure with osteotomy | Total |
|---|---|---|---|
| 1st day | 18 | 2 | 20 |
| 2nd day | 25 | 1 | 26 |
| 3rd day | 4 | 1 | 5 |
| 4–30 days | 8 | 11 | 19 |
| 1–12 months | 4 | 17 | 21 |
| >12 months | – | 3 | 3 |
| No data available | 5 | 1 | 6 |
| Total | 64 | 36 | 100 |
Four newborns that presented with symphyseal diastasis over 4 cm were operated in our department with primary closure performed together with posterior iliac osteotomy (Fig. 3). The same type of orthopedic procedure was performed in all other cases in which primary closure was accompanied by osteotomy. Postoperatively, the child was immobilized in a rigid plaster dressing in a chair position for three weeks (Fig. 4) and then discharged home with legs joined together with an elastic bandage for another three weeks. There is no data regarding the position and period of immobilization in case of children operated in other hospitals.
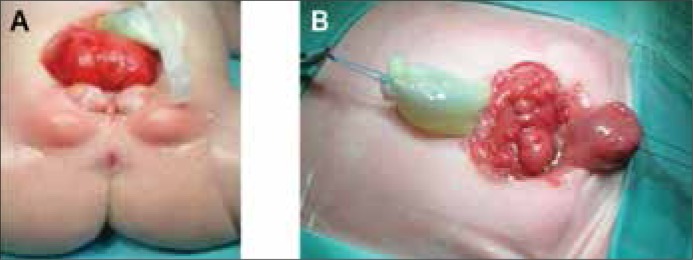
Figure 3.
Posterior iliac osteotomy in bladder exstrophy.
Figure 4.
Immobilization in chair position by using plaster dressing.
To analyze the results of the study on complications after primary bladder exstrophy closure with or without pelvic osteotomy, the chi–square test was used. The differences between the observed frequencies and expected ones were not significant (p = 0.099; χ2 = 2.72; with Yates correction).
Wound dehiscence according to age (up to 72 hrs. and above 72 hrs. of life) and primary closure with or without osteotomy were compared using the Fisher exact test.
RESULTS
Dehiscence after primary closure that was followed by bladder prolapse occurred in 31 patients, among them 13 out of 68 (19%) operated in our department and 18 out of 32 (56%) operated at another hospital. Among the 31 patients with wound dehiscence, only seven (19.4%) were primarily closed with osteotomy and the other 24 (37.5%) without (Table 3).
Table 3.
Wound dehiscence according to age and primary closure with or without osteotomy
| Age | Closure without osteotomy | Dehiscence | Closure with osteotomy | Dehiscence |
|---|---|---|---|---|
| 1st day | 18 | 7 | 2 | 1 |
| 2nd day | 25 | 3 | 1 | – |
| 3rd day | 4 | 3 | 1 | – |
| 4–30 days | 8 | 5 | 11 | 4 |
| 1–12 months | 4 | 4 | 17 | 1 |
| >1 year | – | – | 3 | – |
| No data available | 5 | 2 | 1 | 1 |
| Total | 64 | 24 | 36 | 7 |
The relationship between primary bladder exstrophy closure up to 72 hours of life with osteotomy and wound dehiscence after closure without osteotomy was not significant (P = 0.6996) [the Fisher exact test] (Table 4).
Table 4.
Patients operated up to 72 hrs. of life
| Wound dehiscence | With osteotomy | Without osteotomy | Total |
|---|---|---|---|
| Yes No |
1 3 |
13 34 |
14 37 |
| 4 | 47 | 51 |
Fisher's exact test p = 0.6995798 NS
Primary bladder exstrophy closure with contemporary iliac osteotomy was performed in 32 infants above 72 hours of life. In these cases a significant difference was found by using the Fisher exact test in wound dehiscence after primary closure (P <0.002) (Table 5). A P value of less than 0.05 was considered as statistically significant and values between 0.06 and 0.1 were considered to show statistical tendency. Additionally, in one patient dehiscence was accompanied by peritonitis (treated conservatively) and in another patient with intestinal perforation (treated surgically). Heeling of the wounds in the sacral region was good in all cases.
Table 5.
Patient operated above 72 hrs. of life
| Wound dehiscence | With osteotomy | Without osteotomy | Total |
|---|---|---|---|
| Yes No |
6 26 |
11 6 |
17 32 |
| 32 | 17 | 49 |
Fisher's exact test p = 0.001931013 p <0.002 S
Secondary bladder closure was performed at least one year after first operation. In all cases, re–operation was accompanied by posterior iliac osteotomy with seven cases with re–osteotomy among them. The surgical technique and immobilization period were the same in secondary and primary closure. Among the re–operated, there were 24 children aged one to two years and seven children over two years of age, including one four year old boy. There were no complications of osteotomy observed in either group with primary or secondary closure (Figs. 5 & 6).
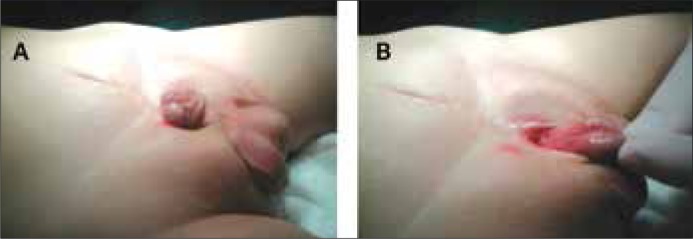
Figure 5.
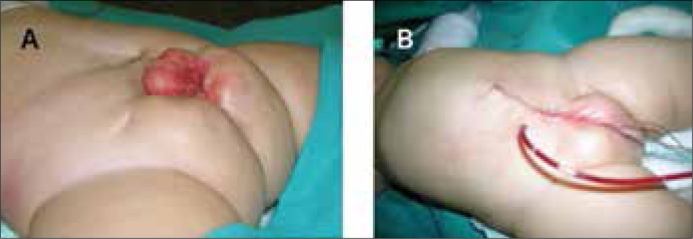
A girl with wound dehiscence after primary bladder exstrophy closure without osteotomy (a) and after secondary closure with posterior osteotomy (b).
Figure 6.
A boy with wound dehiscence after primary bladder exstrophy closure without osteotomy (a) and after secondary closure posterior osteotomy (b).
All children with closed bladder were followed up in the outpatient clinic. Urinalysis was performed once a month. Typically, the upper tract was checked by ultrasound examination about three months after the surgery and voiding cysturethrogram (VCUG) was performed one year later. Vesicoureteral reflux (VUR) was detected in 70 patients (70%) with 46 being bilateral VUR.
Upper urinary tract dilation was detected in 28 children (Table 6). In one patient with severe bilateral hydroureteronephrosis, a trans–uretero–ureterocutaneostomy was performed.
Table 6.
Upper urinary tract dilation and continence after bladder closure
| Upper tract | Dry >1 h | Incontinent | No data about dryness | Total |
|---|---|---|---|---|
| dilation | 14 | 1 | 13 | 28 |
| no dilation | 5 | 32 | 35 | 72 |
| Total | 19 | 33 | 48 | 100 |
Evaluation of dryness was not possible in 48 patients because of lack of data. Among the remaining 52 patients, 33 were totally incontinent or presented very short dry periods while 19 were dry for more than one hour. In the dry group, 14 (74%) had dilation of the upper urinary tract (Table 6).
DISCUSSION
The importance of a successful initial bladder exstrophy closure was emphasized by authors who had found that the ultimate continence rate was higher in those who underwent a successful initial closure [4]. Staged repair (bladder and abdominal wall closure, epispadias repair, bladder neck reconstruction) seems to be a good treatment option to achieve this success. However, from the Jeffs's [4] era, this procedure has been significantly modified as far as one–stage reconstruction initiated by Grady and Mitchell [5]. Independently of the concept, there is one principle that the exstrophied bladder together with posterior urethra should be detached from the symphysis and placed deep within the pelvic ring. In the past there was an idea to close the symphysis without osteotomy, especially in newborn up to 72 hours [6]. Recently, most authors agree that osteotomy is an essential step in the treatment of bladder exstrophy in order to achieve a tension–free closure of the bladder and abdominal wall [7–9]. Even advocators of the one–stage repair who performed the procedure without osteotomy are presently leaning to osteotomies in most patients [10]. In the newborn less than 72 hours of life, we also performed bladder closure without osteotomy but only if pubic bone diastasis was smaller than 4cm. In cases in which the diastasis was greater than 4cm, the closure was accompanied with posterior iliac osteotomy. After analysis of our material we have learned that osteotomy is very useful in all patients even with smaller diastasis. It reduces the tension of closed elements so that the occurrence of dehiscence is significantly decreased. Kantor et al. [8], however, concluded that pelvic osteotomy has no clear indication from an orthopedic point of view – but we found it to facilitate the abdominal wall closure and prevent postoperative wound dehiscence. We agree that osteotomy allows pelvic closure and proper abdominal wall reconstruction, which improves the cosmetic results of the operation [11]. An example of a good cosmetic result is shown in Figure 7. Putting together the pubic bones is essential for pelvic diaphragm closure, which prevents vaginal and anal prolapse [12, 13]. The pelvic diaphragm is also important for further functional reconstruction and the achievement of the continence [11, 14, 15]. However some authors question the role of osteotomy in ultimate orthopedic and urological outcomes, but the small number of patients being evaluated seems to be inadequate for such conclusions [7, 8].
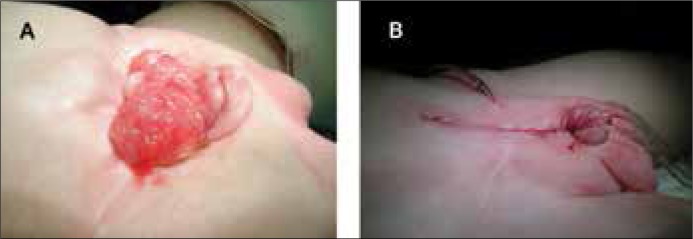
Figure 7.
A boy 2 years after primary bladder exstrophy closure with posterior iliac osteotomy in neonate period.
There are two types of iliac osteotomy mostly used: posterior and anterior [2, 7, 8, 12, 16]. However, a group from Baltimore has advocated performing these two procedures together as a combined transverse innominate and vertical iliac osteotomy [9]. We found posterior iliac osteotomy to be a simple and efficient procedure that does not cause as many difficulties with changing the position of the baby as were raised. Also, we never observed the femoral nerve palsies, bony non–unions or delayed unions, nor joint pains that were described by Okubadejo [17] nor did we observe any complications related to external stabilization and traction. Immobilization in the plaster dressing in the chair position is sufficient for pelvic bones stabilization and allows movements in the knee and ankle joints. The child can be placed on his back and can be turned to their right or left side. Neither deep nor superficial infections of the osteotomy wound were observed, which underlines the safety of the method. It is also important that this procedure could be repeated in primarily unsuccessful cases.
Whichever type of osteotomy is used, the pelvic ring closure could increase resistance to urinary outflow. Since VCUG detected VUR in 70% of children and upper tract dilation was observed in 74% of patients in the dry group, the risk of upper urinary tract deterioration should be considered if a one–stage reconstruction is performed without any complementary antireflux procedure.
CONCLUSIONS
Osteotomy performed at the time of primary bladder exstrophy closure diminishes the risk of wound dehiscence independently of patient's age.
Posterior iliac osteotomy is sufficient and safe and can be repeated if necessary.
Urinary outflow resistance after primary bladder closure may predispose to the upper urinary tract dilation that could be the cause of renal failure, especially because VUR is observed in the vast majority of cases.
References
- 1.Muecke EC. The role of the cloacal membrane in exstrophy. The first successful experimental study. J Urol. 1964;92:659. doi: 10.1016/S0022-5347(17)64028-X. [DOI] [PubMed] [Google Scholar]
- 2.Gearhart JP. Exstrophy, epispadias and other bladder anomalies. Campbell's Urology Eighth Edition. 2002;61:2136–2196. [Google Scholar]
- 3.Schultz WG. Plastic repair of exstrophy of the bladder combined with bilateral osteotomy of the ilia. J Urol. 1958;79:453. doi: 10.1016/S0022-5347(17)66294-3. [DOI] [PubMed] [Google Scholar]
- 4.Oesterling JE, Jeffs RD. The importance of a successful initial bladder closure in the surgical management of classical bladder exstrophy: Analysis of 144 patients treated at the Johns Hopkins Hospital between 1975 and 1985. J Urol. 1987;137:258. doi: 10.1016/s0022-5347(17)43972-3. [DOI] [PubMed] [Google Scholar]
- 5.Grady RW, Mitchell ME. Complete primary repair of exstrophy. J. Urol. 1999;162:1415–1420. [PubMed] [Google Scholar]
- 6.Baker LA, Gearhart JP. The staged approach to bladder exstrophy closure and role of osteotomies. World J Urol. 1998;16:205. doi: 10.1007/s003450050054. [DOI] [PubMed] [Google Scholar]
- 7.Castagnetti M, Gigante C, Perrone G, Rigamonti W. Comparison of musculoskeletal and urological functional outcomes in patients with bladder exstrophy undergoing repair with and without osteotomy. Pediatr Surg Int. 2008;24:689–693. doi: 10.1007/s00383-008-2132-x. [DOI] [PubMed] [Google Scholar]
- 8.Kantor R, Salai M, Ganel A. Orthopaedic long term aspects of bladder exstrophy. Clin Orthop Relat Res. 1997;335:240–245. [PubMed] [Google Scholar]
- 9.Sponseller P, Jani MM, Jeffs RD, Gearhart JP. Anterior innominate osteotomy in repair of bladder exstrophy. J Bone Joint Surg. 2001;83A:184–193. doi: 10.2106/00004623-200102000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Grady RW, Mitchell ME. Complete primary repair of exstrophy. J Urol. 1999;162:1415–1420. [PubMed] [Google Scholar]
- 11.Chan DY, Jeffs RD, Gearhart JP. Determinants of continence in the bladder exstrophy population: predictors of success? Urology. 2001;57:774–777. doi: 10.1016/s0090-4295(00)01102-x. [DOI] [PubMed] [Google Scholar]
- 12.Mathews R, Sponseller PD, Jeffs RD, Gearhert JP. Bladder neck reconstruction in classic bladder exstrophy: the role of osteotomy in the development of continence. BJU Int. 2000;85:498–500. doi: 10.1046/j.1464-410x.2000.00517.x. [DOI] [PubMed] [Google Scholar]
- 13.Ebert AK, Falkert A, Brandl R, Hirschfelder H, Koller M, Rösch WH. Pelvic floor imaging using three–dimensional ultrasonography and magnetic resonance imaging in the long term follow–up of the bladder – exstrophy – epispadias complex. BJU Int. doi: 10.1111/j.1464-410X.2009.08736.x. [DOI] [PubMed] [Google Scholar]
- 14.Frimberger D, Gearhart JP, Mathews R. Female exstrophy: failure of initial reconstruction and its implications for continence. J Urol. 2003;170:2428–2431. doi: 10.1097/01.ju.0000090195.72919.f5. [DOI] [PubMed] [Google Scholar]
- 15.Surer I, Baker LA, Jeffs RD, Gearhart JP. Modified Young – Dees – Leadbetter bladder neck reconstruction in patients with successful primary bladder closure elsewhere: a single institution experience. J Urol. 2001;165:2438–2440. doi: 10.1016/S0022-5347(05)66224-6. [DOI] [PubMed] [Google Scholar]
- 16.Lottmann H, Melin Y, Lombrail P, Cendron J. Reconstruction of bladder exstrophy: retrospective study of 57 patients with evaluation of criteria in favor of the acquisition of continence. Ann Urol. 1998;32:233–239. [PubMed] [Google Scholar]
- 17.Okubadejo G, Sponseller P, Gearhart JP. Complications in orthopedic management of exstrophy. J Ped Orthop. 2003;23:522–528. [PubMed] [Google Scholar]